Abstract
Objective
To describe variation in mortality and morbidity effects of high-level, high-volume delivery hospital between racial/ethnic groups and insurance groups.
Study Design
Retrospective cohort including infants born at 24–32 weeks gestation or birth weights ≤2500 g in California, Missouri, and Pennsylvania between 1995 and 2009 (n = 636,764). Multivariable logistic random-effects models determined differential effects of birth hospital level/volume on mortality and morbidity through an interaction term between delivery hospital level/volume and either maternal race or insurance status.
Result
Compared to non-Hispanic white neonates, odds of complications of prematurity were 14–25% lower for minority infants in all gestational age and birth weight cohorts delivering at high-level, high-volume centers (odds ratio (ORs) 0.75–0.86, p < 0.001–0.005). Effect size was greatest for Hispanic infants. No difference was noted by insurance status.
Conclusions
Neonates of minority racial/ethnic status derive greater morbidity benefits than non-Hispanic white neonates from delivery at hospitals with high-level, high-volume neonatal intensive care units.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In the United States, approximately 2–3% of infants born annually are <34 weeks gestation and 1–2% weigh <1500 g [1]. These premature and very low birth weight (VLBW) infants experience significant complications of prematurity, resulting in extended hospital stays and life-long medical challenges. VLBW infants represent 54.8% of deaths in the first year after birth and, in 2005, cost the health care system US$26.2 billion between neonatal intensive care unit (NICU) care expenses, delivery costs, early intervention services, and loss of household productivity [2, 3].
Since the 1960s, efforts have been made to consolidate neonatal intensive care services to improve quality and access to care, also known as “regionalization of perinatal care.” [4] Numerous studies demonstrating significantly improved survival for premature and low birth weight infants born at hospitals with high-level and high-volume intensive care nurseries underscore the regionalization movement [5,6,7,8]. Further, associations have been demonstrated between delivery hospital NICU level, delivery hospital volume, and complications of preterm birth. These relationships vary by state and by the improvement in mortality associated with delivery at a high-level, high-volume hospital, which may reflect the fact that improved survival allows infants who otherwise would die to survive and develop complications [9].
While considerable evidence supports the mortality benefits of delivering VLBW and preterm infants at hospitals with high-level NICUs, limited data exist on the differential impact of delivery hospital level on individuals of varying races and socioeconomic statuses. Prematurity rates for minority and publicly insured infants are consistently higher than those for non-Hispanic white and privately insured neonates [1, 10, 11]. Additionally, differential delivery hospital quality explains up to 40% of racial disparities in outcomes for these premature infants, and black infants are cared for at lower quality hospitals than their non-Hispanic white, Asian, or Hispanic counterparts [12,13,14]. However, no study has examined the effect of delivery hospital level on patients of different racial or socioeconomic status. Given these prior findings, our study aims to identify those racial and socioeconomic groups who benefit most from high-level neonatal intensive care services and who should be targeted for delivery at hospitals with high-level NICU facilities.
Methods
Study design
Data population
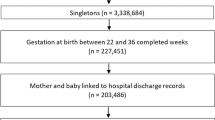
A retrospective cohort was constructed from birth and death certificates linked to hospital records of all infants born at gestational ages of 24–32 weeks or birth weights <2500 g in California, Missouri, and Pennsylvania between 1995 and 2009. Infants were excluded for gestational age <24 weeks (11,005 infants) or birth weight <500 g (3,332 infants) given inconsistent resuscitation and treatment standards applied in these cohorts. Infants were also excluded for the presence of congenital anomalies (41,565 infants, Supplemental Material A); for birth weight >5 SDs from the mean birth weight for gestational age (391 infants)—because of concern that either birth weight or gestational age may have been incorrectly entered into the birth certificate; and for missing gestational age, birth weight, birth hospital, birth year, race, payment status, or death status (80,402 infants) [9]. From a total of 773,450 births at 24–32 weeks or birth weights ≤2500 g, our final cohort included 636,764 neonates. This study was approved by the IRBs of California, Missouri, Pennsylvania, and The Children’s Hospital of Philadelphia.
NICU level definitions
According to American Academy of Pediatrics guidelines, level 1 NICUs offer only well newborn care and post-delivery stabilization of sicker infants. Level 2 NICUs have the ability to care for neonates at or beyond 32 weeks gestation and may provide mechanical ventilation for <24 h. Level 3 NICUs provide care for very ill and premature infants, whereas level 4 NICUs offer pediatric cardiothoracic surgery and cardiopulmonary bypass services [15]. For each hospital and year, neonatal intensive care unit levels were hand-verified based on American Academy of Pediatrics guidelines and characteristics of the patients delivering at each hospital during the given year. As in prior work, specific characteristics that determined the assigned level included the number of extremely low birth weight (ELBW) and VLBW infants cared for annually, the frequency of mechanical ventilation, number of infants mechanically ventilated for longer than 96 h, the presence of patients receiving extracorporeal membrane oxygenation and cardiac surgery services, and each hospital’s self-identified NICU level [5, 9].
A high-level, high-volume hospital was defined as a facility with a level 3 or level 4 NICU that cares for more than 50 VLBW neonates annually based on prior work [5, 9]. As in prior work, infants were assigned to their initial birth hospital to account for the effects of resuscitation and initial delivery room management on both short-term and long-term outcomes of care [5, 9].
Study outcome definitions
The primary outcomes for our analysis were pre-discharge mortality and composite morbidity. Pre-discharge mortality did not include deaths after transfer out of the birth hospital. In keeping with prior studies, pre-discharge mortality included fetal deaths given the possibility for variable interpartum management to convert some fetal deaths to neonatal deaths [5, 9]. Composite morbidity included infants with any of necrotizing enterocolitis, retinopathy of prematurity, bronchopulmonary dysplasia, and grades 3 and 4 intraventricular hemorrhage, which were identified using ICD-9-CM codes (Supplemental Material B). These specific complications of prematurity were selected as they are among the most common morbidities, are consistently represented in similar studies, and are strong predictors of future death and neurocognitive delay [5, 9, 16, 17].
Covariate variable definitions
Maternal chronic medical conditions, pregnancy complications, gestational age, and birth weight were included as covariate variables given their known associations with study outcomes (Supplemental Material C) [5, 9, 18,19,20,21,22,23,24,25]. Maternal race and insurance status were analyzed through interaction terms with birth hospital NICU level. Maternal race was categorized as either non-Hispanic white or minority racial/ethnic group in the primary analysis and subsequently subdivided by racial and ethnic group. Racial and ethnic subgroups included non-Hispanic white, non-Hispanic Black, Hispanic, Asian/Pacific Islander, and Other. Insurance status was categorized as either privately insured or publicly insured/uninsured and was used as a proxy for patient income. Private insurance included health maintenance organizations and fee-for-service plans, while public insurance included federal plans and Medicaid plans. Uninsured individuals were those whose insurance status was coded as self-pay or none.
Data analysis
We used χ2 tests or t tests to determine univariate associations between factors. Multivariable logistic random-effects models determined the differential effect of high-level, high-volume birth hospital on mortality and complications of prematurity through an interaction term between delivery hospital level and maternal race or insurance status after adjusting for the covariates described above and listed in Supplemental Material C. Models adjusted for clustering at the hospital level by the calculation of standard errors using the methods of Huber and White.
Code availability
Stata 15.1 code for this analysis is available in Supplemental Material G or by contacting the authors.
Results
Population Demographics
Sixty nine percent of non-Hispanic white neonates delivered at high-level, high-volume hospitals vs. 76% of minority neonates (p < 0.001). Seventy percent of publicly insured and uninsured neonates delivered at high-level, high-volume centers vs. 75% of privately insured neonates (p < 0.001) (Table 1). Minority neonates were disproportionately publicly insured or uninsured. While 50% of infants overall were publicly insured or uninsured, 61% of minority neonates were publicly insured or uninsured (p < 0.001). Sixty seven percent of non-Hispanic black neonates and 69% of Hispanic neonates were publicly insured or uninsured, while 35% of non-Hispanic white, 29% of Asian, and 41% of other race neonates were publicly insured or uninsured (p < 0.001) (Supplemental Material D).
Population outcomes
Our cohort had an overall pre-discharge mortality rate of 1.29% with mortality rates in the gestational age and birth weight subgroups ranging from 1.37% in the LBW cohort to 18.80% in the ELBW cohort (Supplemental Material E). There was a 26–38% reduction in odds of mortality for all neonates born at high-level, high-volume centers across gestational age and birth weight categories (p < 0.001) (Supplemental Material F). Meanwhile, the overall rate of composite morbidity was 5.23% with subgroup morbidities ranging from 5.55% in the LBW cohort to 54.41% in the ELBW cohort (Supplemental Material E). There was a 42–64% increase in odds of composite morbidity for infants born at high-level, high-volume centers across gestational age and birth weight cohorts (p < 0.001) (Supplemental Material F). There were increased odds of necrotizing enterocolitis, retinopathy of prematurity, and bronchopulmonary dysplasia for infants born at high-level, high-volume hospitals, but decreased odds of high grade intraventricular hemorrhage (Supplemental Material F).
Interaction between maternal race and hospital level
Minority neonates demonstrated less of an increase in odds of morbidity when delivered at high-level, high-volume centers compared to non-Hispanic white neonates delivering at high-level, high-volume centers. This reduction in odds of morbidity ranged between 14 and 25% and spanned all gestational age and birth weight cohorts (Fig. 1). There was no such statistically significant difference noted for pre-discharge mortality (Fig. 1).
When further subdivided by racial/ethnic group, Hispanic infants were notable for a composite morbidity reduction of 19–30% (odds ratio (OR) 0.70–0.81, p < 0.001–0.003) compared to non-Hispanic white neonates when delivering at high-level, high-volume centers (Fig. 2). There was no statistically significant difference in delivery hospital effect on composite morbidity for infants of black, Asian, or other races compared to non-Hispanic white infants. However, all of these groups demonstrated trends toward a reduction in odds of composite morbidity compared to non-Hispanic white neonates.
Meanwhile, subgroup analysis by complication of prematurity highlights the differential benefit for minority neonates born at high-level, high-volume centers is driven by reductions in odds of necrotizing enterocolitis, retinopathy of prematurity, and bronchopulmonary dysplasia (Table 2). The same differential benefit was not demonstrated for grade 3 and 4 intraventricular hemorrhage.
Interaction between maternal payment status and hospital level
There was no statistically significant interaction between insurance status and birth hospital NICU level/volume in predicting neonatal mortality or morbidity (Fig. 3).
Discussion
Past research has consistently demonstrated improved mortality outcomes for premature and low birth weight neonates born at high-level, high-volume centers [5,6,7,8]. Our study reaffirms this finding. Consistent with past studies, our analysis also highlights increased odds of developing common complications of prematurity among infants born at high-level, high-volume centers, likely resulting from this improvement in survival [9]. Compared to non-Hispanic white neonates, infants of minority race delivered at high-level, high-volume hospitals had a 14–25% lower rate of common complications of preterm birth, such as necrotizing enterocolitis, retinopathy of prematurity, and bronchopulmonary dysplasia, across all gestational age and birth weight cohorts. Among racial and ethnic subgroups, this effect was statistically significant for Hispanic infants. In contrast to these findings, we found no differential effect by delivery hospital for infants of mothers with different insurance coverage.
The three outcomes that drove the improved morbidity effect for delivery at a high-level, high-volume center for minority racial/ethnic groups—necrotizing enterocolitis, retinopathy of prematurity, and bronchopulmonary dysplasia—are identified later in an infant’s hospital course after preterm birth and may be more heavily influenced by ongoing medical interventions [26,27,28,29,30,31]. In contrast, intraventricular hemorrhage is an acute event that often occurs very early in neonatal life and can be more heavily influenced by interpartum factors—such as antenatal glucocorticoid administration, delivery room intubation, and use of vasoactive medications—than by long-term NICU management [32,33,34]. These dynamics could explain why hospital volume and experience in caring for low birth weight and preterm infants may protect against acute outcomes like severe intraventricular hemorrhage while also increasing survival of very premature or ill infants who go on to develop more chronic complications [9]. It also may reflect ongoing lower quality care for minority patients at lower-volume, lower-level hospitals compared to non-Hispanic white patients [35, 36].
The observed reduction in complications of prematurity for Hispanic neonates born at high-level, high-volume hospitals is likely due to disparities in baseline birth hospital quality between these infants and non-Hispanic white infants. Howell et al.’s [12] study demonstrates that hospital quality contributes 29.5% of Hispanic–white neonatal outcome disparities and 39.9% of black–white neonatal outcome disparities in New York City. Meanwhile, Horbar, et al.’s [13, 14] analysis found significant segregation and inequality in NICU care. Black infants were clustered at NICUs with lower quality scores than non-Hispanic white infants, while Hispanic and Asian infants were clustered at NICUs with higher quality scores. This study also highlights significant geographic variation, with high NICU quality in the Pacific region explaining much of the differential in delivery hospital quality for Hispanic infants. Given that a large portion of our study population is comprised of Hispanic infants from California, it is likely that differential outcomes between high-quality, regionalized California NICUs and the lower-volume and lower quality NICUs at which Hispanic women deliver elsewhere explains the morbidity benefit we found for Hispanic neonates at high-level, high-volume NICUs. Future research should analyze the interaction between race and NICU level for different geographic areas to clarify whether regional trends in NICU structure and quality explain racial differences in birth hospital effects.
The differential effect of high-level, high-volume delivery hospital demonstrated for racial and ethnic groups was not seen for insurance groups, despite significant overlap between minority racial or ethnic identity and lower socioeconomic status. Hispanic neonates were more likely to be publicly insured or uninsured and demonstrated a morbidity benefit from high-level, high-volume delivery hospital across all cohorts. Meanwhile, Asian infants were among the least likely to be publicly insured, but demonstrated a trend toward benefit from high-level, high-volume delivery hospital that was similar to the trend noted for Hispanic neonates. This suggests that the morbidity effect may be truly associated with race/ethnicity rather than a confounding payment status effect. The absence of a significant interaction between payment status and delivery hospital may reflect a smaller difference in baseline delivery hospital quality between privately insured and publicly insured neonates than the difference that has been previously described between racial/ethnic groups [12,13,14]. Regional variation between states with different health care payment structures could also minimize the overall payment status effect size. Finally, it is also important to acknowledge that our study was not powered to detect differences in morbidity effect between insurance subgroups and our insurance categorizations may therefore not ideally reflect socioeconomic status. Further analyses should seek to describe and explain this discrepancy between racial/ethnic and payment status effects.
There are some limitations when assessing our data. First, we did not specifically consider how social and economic factors impact delivery hospital choice. In our cohort, a higher percentage of minority and privately insured neonates were born at hospitals with high-level, high-volume NICUs. If the factors prompting these differences in birth hospital choice also altered infants’ baseline risks for mortality and morbidity, they could have confounded our interaction terms. There are limited to no data on the factors influencing choice of delivery hospitals for patients, particularly those with public insurance or of minority racial/ethnic status. These factors could also vary between states with different health care funding and delivery structures. Future studies should consider factors such as hospital demographics and distance between residence and birth hospital to account for factors underlying birth hospital choice [9].
Further, we relied on self-identified racial and ethnic categories in our data analysis. There is widespread uncertainty about the utility of racial and ethnic grouping in predicting outcomes for individual patients given heterogeneity within groups and variable self-identification [37,38,39,40]. The categories in our dataset also preclude potentially important distinctions by subgroup, such as Middle Eastern and North African individuals or Hispanic individuals of variable geographic origin. Finally, we relied on International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes to identify neonatal complications. Variability in birth hospital coding methods could therefore have affected accuracy in enumerating our outcome measures, although this has not been demonstrated in other work.
Ultimately, our results suggest that minority premature infants—Hispanic infants in particular—show a reduction in the odds of common morbidities of preterm birth compared to non-Hispanic white neonates when they deliver at hospitals with high-level and high-volume neonatal intensive care units. Neonatal intensive care unit regionalization efforts should continue and special efforts should be made to ensure that minority women can access these high-level services. To reduce disparities between hospitals serving primarily minority versus primarily non-Hispanic white patients, efforts should be made to equalize the quality of standard obstetric and neonatal services.
References
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1–54.
Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013;131:855–60. https://doi.org/10.1542/peds.2012-2471.
Institute of Medicine. Preterm birth: causes, consequences, and prevention. Washington, DC: The National Academic Press; 2007.
Yu VYH, Doyle LW. Regionalized long-term follow-up. Semin Neonatol. 2004;9:135–44. https://doi.org/10.1016/j.siny.2003.08.008.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–75. https://doi.org/10.1056/NEJMsa065029.
Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109:745–51.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304:992–1000. https://doi.org/10.1001/jama.2010.1226.
Chung JH, Phibbs CS, Boscardin WJ, Kominski GF, Ortega AN, Needleman J. The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care. 2010;48:635–44. https://doi.org/10.1097/MLR.0b013e3181dbe887.
Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8. https://doi.org/10.1542/peds.2011-2820.
Markus AR, Krohe S, Garro N, Gerstein M, Pellegrini C. Examining the association between Medicaid coverage and preterm births using 2010–2013 National Vital Statistics Birth Data. J Child Poverty. 2016;23:79–94. https://doi.org/10.1080/10796126.2016.1254601.
Durbin DR, Giardino AP, Shaw KN, Harris MC, Silber JH. The effect of insurance status on likelihood of neonatal interhospital transfer. Pediatrics. 1997;100:E8.
Howell EA, Janevic T, Herbert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172:269–77. https://doi.org/10.1001/jamapediatrics.2017.4402.
Horbar JD, Edwards EM, Greenberg LT, Profit J, Draper D, Helkey D, et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 2019. https://doi.org/10.1001/jamapediatrics.2019.0241.
Howell EA, Hebert PL, Zeitlin J. Racial segregation and inequality of care in neonatal intensive care units is unacceptable. JAMA Pediatr. 2019. https://doi.org/10.1001/jamapediatrics.2019.0240.
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97. https://doi.org/10.1542/peds.2012-199.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely pretern infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56. https://doi.org/10.1542/peds.2009-2959.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months. JAMA. 2003;289:1124–9. https://doi.org/10.1001/jama.289.9.1124.
Ananth C, Basso O. Impact of pregnancy-induced hypertension on stillbirth and neonatal mortality in first and higher order births: a population-based study. Epidemiology. 2010;21:118–23. https://doi.org/10.1097/EDE.0b013e3181c297af.
Perger L, Mukhopadhyay D, Komidar L, Wiggins-Dohlvik K, Uddin MN, Beeram M. Maternal pre-eclampsia as a risk factor for necrotizing enterocolitis. J Matern-Fetal Neonatal Med. 2016;29:2098–103. https://doi.org/10.3109/14767058.2015.1076386.
Leary P, Leary SE, Stout K, Schwartz S, Easterling TR. Maternal, perinatal, and postnatal outcomes in women with chronic heart disease in Washington State. Obstet Gynecol. 2012;120:1283–90. https://doi.org/10.1097/AOG.0b013e3182733d56.
Kendrick J, Sharma S, Holmen J, Palit S, Nuccio E, Chonchol M. Kidney disease and maternal and fetal outcomes in pregnancy. Am J Kidney Dis. 2015;66:55–59. https://doi.org/10.1053/j.ajkd.2014.11.019.
Nevis I, Reitsma, Dominic A, McDonald S, Thabane L, Aki E, et al. Pregnancy outcomes in women with chronic kidney disease: a systematic review. Clin J Am Soc Nephrol. 2011;6:2587–98. https://doi.org/10.2215/CJN.10841210.
Persson M, Shah PS, Rusconi F, Reichman B, Modi N, Kusuda S, et al. Association of maternal diabetes with neonatal outcomes of very preterm and very low-birth-weight infants: an International Cohort Study. JAMA Pediatr. 2018;172:867–75. https://doi.org/10.1001/jamapediatrics.2018.1811.
Grandi C, Tapia JL, Cardoso VC. Impact of maternal diabetes mellitus on mortality and morbidity of very low birth weight infants: a multicenter Latin America study. J Pediatr. 2015;91:234–41. https://doi.org/10.1016/j.jped.2014.08.007.
Shapiro-Mendoza C, Tomashek K, Kotelchuck M, Barfield W, Nannini JW, Declercq E. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics. 2008;121:e223–32. https://doi.org/10.1542/peds.2006-3629.
Yee W, Soraisham A, Shah V, Aziz K, Yoon W, Lee SK. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–304. https://doi.org/10.1542/peds.2011-2022.
Samuels N, van de Graaf R, de Jonge R, Reiss IK, Vermeulen M. Risk factors for necrotizing enterocolitis in neonates: a systematic review of prognostic studies. BMC Pediatr. 2017;17:105 https://doi.org/10.1186/s12887-017-0847-3.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sanchez PJ, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66. https://doi.org/10.1542/peds.2007-3423.
Fang JL, Sorita A, Carey WA, Colby CE, Murad MH, Alahdab F, et al. Interventions to prevent retinopathy of prematurity: a meta-analysis. Pediatrics. 2016;137 https://doi.org/10.1542/peds.2015-3387.
Trembath A, Laughon M. Predictors of bronchopulmonary dysplasia. Clin Perinatol. 2012;39:585–601. https://doi.org/10.1016/j.clp.2012.06.014.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3. https://doi.org/10.1002/14651858.CD004454.pub2.
Linder N, Haskin O, Levit O, Klinger G, Prince T, Naor N, et al. Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case–control study. Pediatrics. 2003;111(5 Part 1):e590–5.
Chevallier M, Debillon T, Pierrat V, Delorme P, Kayem G, Durox M, et al. Leading causes of preterm delivery as risk factors for intraventricular hemorrhage in very preterm infants: results of the EPIPAGE 2 cohort study. Am J Obstet Gynecol. 2017;216:518.el–518.e12. https://doi.org/10.1016/j.ajog.2017.01.002.
Handley SC, Passarella M, Lee HC, Lorch SA. Incidence trends and risk factor variation in severe intraventricular hemorrhage across a population based cohort. J Pediatr. 2018;200:24–29.e3. https://doi.org/10.1016/j.jpeds.2018.04.020.
Profit J, Gould J, Bennett M, Goldstein BA, Draper D, Phibbs C, et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics. 2017;140. https://doi.org/10.1542/peds.2017-0918.
Jha AK, Orav EJ, Epstein AM. Low-quality, high-cost hospitals, mainly in South, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Aff. 2011;30:1904–11. https://doi.org/10.1377/hlthaff.2011.0027.
Comstock R, Castillo E, Lindsay S. Four-year review of the use of race and ethnicity in epidemiologic and public health research. Am J Epidemiol. 2004;159:611–9.
Burchard EG, Ziv E, Coyle N, Gomez SL, Tang H, Karter AJ. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348:1170–5. https://doi.org/10.1056/NEJMsb025007.
Baker LC, Afendulis CC, McConville S, Phibbs CS, Fuentes-Afflick E. Differences in neonatal motality among whites and Asian American subgroups: evidence from California. Arch Pediatr Adolesc Med. 2007;161:69–76. https://doi.org/10.1001/archpedi.161.1.69.
Rice WS, Goldfarb SS, Brisendine AE, Burrows S, Wingate MS. Disparities in infant mortality by race among Hispanic and non-Hispanic infants. Matern Child Health J. 2017;21:1581–8. https://doi.org/10.1007/s10995-017-2290-3.
Funding
This work was supported by a grant R01 HD084819.
Author information
Authors and Affiliations
Contributions
SL obtained data for the project. GY and SL both contributed to idea development, project design, data analysis, and manuscript writing and editing. MP prepared data and assisted with data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yannekis, G., Passarella, M. & Lorch, S. Differential effects of delivery hospital on mortality and morbidity in minority premature and low birth weight neonates. J Perinatol 40, 404–411 (2020). https://doi.org/10.1038/s41372-019-0423-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0423-9
- Springer Nature America, Inc.
This article is cited by
-
The impact of volume and neonatal level of care on outcomes of moderate and late preterm infants
Journal of Perinatology (2024)