Abstract
Objectives
To examine risk factors for mortality among preterm infants during newborn and subsequent hospitalizations, and whether they differ by race/ethnicity.
Study design
We conducted a cross-sectional analysis using the 2016 Kids Inpatient Database. Hospitalizations of preterm infants were categorized as “newborn” for birth admissions, and “post-newborn” for all others. Multivariate logistic regression was performed to calculate associations of mortality with sociodemographic factors.
Results
Of 285915 hospitalizations, there were 7827 (2.7%) deaths. During newborn hospitalizations, adjusted OR (aOR) of death equaled 1.14 (95% CI 1.09–1.20) for males, 68.73 (61.91–76.30) for <29 weeks GA, and 0.81 (0.71–0.92) for transfer. Stratified by race/ethnicity, aOR was 0.69 (0.61–0.71) for Medicaid only among black infants. During post-newborn hospitalizations, death was associated with transfer (aOR 5.02, 3.31–7.61).
Conclusions
Risk factors for death differ by hospitalization types and race/ethnicity. Analysis by hospitalization types may identify risk factors that inform public health interventions for reducing infant mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Infant mortality in the U.S. is a major public health concern, at 5.79 per 1000 live births in 2017 [1]. The mortality rate declined in 2007 through 2011, but in recent years it has remained essentially unchanged [2], higher than most other developed countries [3]. Within this high U.S. infant mortality rate is a striking racial disparity: non-Hispanic black infants have the highest mortality rate at 11.21 deaths per 1000 births, compared to 4.87 among non-Hispanic white infants [4]. This disparity has been attributed to the high rates of preterm birth among non-Hispanic black women, and preterm birth itself is a major risk factor for infant death. Overall, preterm birth contributed to 66% of infant mortality in 2013 [4], and compared to white preterm infants, black preterm infants had a 1.7-fold higher rate of death in the first year of life [4].
Research efforts to identify risks and reduce infant mortality among preterm births face several challenges. First, estimation of mortality risk is difficult in this population whose complex birth circumstances are followed by prolonged length of stay in the hospital, of whom survivors are discharged to home with multiple medical and surgical morbidities. Second, from an epidemiological perspective, infant mortality rate is routinely reported in two periods within the first year: neonatal (0–27 days) and post-neonatal (28–364 days). However, for preterm infants today who often remain hospitalized well beyond 28 days of life, this temporal categorization does not provide relevant knowledge on risks of death that could inform intervention efforts. Finally, among preterm infants, death beyond the neonatal intensive care unit (NICU) remains poorly characterized, as most neonatal research data collection ends at hospital discharge. Given the shift in medical and social environment after NICU discharge, it is plausible that risk factors for death differ in the community, but this remains largely unknown.
Therefore, our objective for this study was to examine risk factors associated with death during newborn hospitalization and subsequent hospitalizations, and identify racial/ethnic disparities in risk factors, using a nationally representative dataset of infant hospitalizations in the U.S. We hypothesized that risk factors will vary between birth and subsequent hospitalizations, and vary between races/ethnicities.
Methods
Study sample
This was a secondary data analysis using the 2016 Kids’ Inpatient Database (KID), a data subset from the National Inpatient Sample (NIS) developed by the Agency for Healthcare Research and Quality (AHRQ), as part of the Healthcare Cost and Utilization Project (HCUP). This Federal-State-Industry partnership consists of collaboration of data from 4121 hospitals in 44 states, compiled every 3 years, and includes children younger than 20. Included on each discharge record are patient and hospital demographics, codes for International Classification of Diseases (ICD), Diagnosis Related Groups (DRG), and Major Diagnostic Category (MDC) assigned by the Medicare grouper during HCUP processing.
For the current study, the sample included preterm infants admitted at age 0 to 11 months in the 2016 KID. Preterm birth was defined as gestational age less than 37 weeks, identified by International Classification of Diseases, 10th Revision, (ICD-10) codes for “Disorders of newborn related to short gestation” (P07.2 and P0.73), which specified completed gestational weeks. A total of 288,834 preterm infant admissions were identified in the 2016 KID. Of these, 304 patients without death outcome data were excluded. Also excluded were 157 admissions whose sex information was missing, 2173 admissions whose exact gestational age was missing, and 285 admissions whose insurance information was missing.
To examine the risk factors separately for newborn and post-newborn hospitalizations, we defined “newborn” hospitalizations based on major diagnostic category (MDC). Admissions with MDC code of 15 (“newborn and other neonates”) were considered as newborn. The remaining hospitalizations were defined as “post-newborn”.
The exposures of interest included infant sex, gestational age, race/ethnicity, income level, insurance type, and hospital transfer status. Gestational age was categorized into extreme (<29 weeks), moderate (29 to <34 weeks), and late prematurity (34 to <37 weeks). Race/ethnicity was categorized as white, black, Hispanic, other (Asian or Pacific Islander, Native American, Other), or missing. The “missing” category was added because a substantial proportion of the sample (>10%) had missing data for race/ethnicity. Income level was categorized into four quartile groups based on median household income for patient’s ZIP code: <$43,000, $43,000–54,000, $54,000–<71,000, or >=$71,000. Patients with missing data for median household income (1% of the sample) was treated as <$43,000. Insurance type was categorized as Medicaid, private insurance, and other, which included Medicare, self-pay, and no charge. Hospital transfer was categorized as transferred in from a different acute care hospital or other type of health facility, or not transferred. Patients with missing data for transfer status (<0.2% of the sample) was treated as not transferred.
The 2016 KID dataset did not include birth weight, which had been included in 2006 and 2009 datasets. In an attempt to validate our methods for using the 2016 dataset without birth weight, we repeated all analyses with 2006 and 2009 datasets using gestational ages and birth weights.
The main outcome was death during hospitalization or survival, identified based on discharge disposition records.
Statistical analyses
Statistical analyses included bivariate comparisons of sociodemographic characteristics and death. For each admission type (newborn and post-newborn), we performed population-weighted multivariate logistic regression to characterize associations of mortality with sociodemographic and clinical factors available in the dataset.
All analyses were conducted using SAS 9.4 (Cary, NC). The complex sampling design was accounted for using PROC SURVEYFREQ and PROC SURVEYLOGISTIC. Descriptive analyses, including frequency analyses, were conducted for the selected study variables. Chi-square tests were used to examine the association between each of the potential risk factors and death. Multivariable logistic regression models were fitted separately for newborn and post-newborn admissions, including all potential risk factors of interest. We also tested the interactions between the risk factors. We repeated the logistic regression analyses separately for three racial/ethnic groups: white, black, and Hispanic, and calculated odds ratios of death for each potential risk factor with 95% confidence intervals.
To examine the consistency of results across the years, we separately analyzed 2009 and 2012 KID data. We conducted logistic regression analysis including birth weight (<1500 g vs. 1500–2500 g) as a predictor, to confirm that the main findings in these samples were consistent with those after accounting for birth weight. To further explore whether the main findings were consistent across gestational age groups, we conducted the logistic regression analysis separately by race/ethnicity and by gestational age categories.
For subjects missing data on median household income and transfer status, we conducted a sensitivity analyses, since we treated those with missing household income data as “<$43,000”, and missing transfer status as “no transfer”.
The study was exempt from human subjects review as analysis of de-identified secondary data.
Results
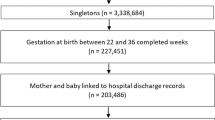
The 2016 HCUP sample represented 3,117,413 hospital discharges. Of these, 1,657,897 were admitted at less than 1 year of age, and 285,915 were preterm infants. There were 278,309 newborn hospitalizations and 7606 post-newborn hospitalizations.
Distributions of infant characteristics for newborn and post-newborn hospitalizations are shown in Table 1. Mortality rates during newborn and post-newborn hospitalizations were 2.7%, and 3.3%, respectively. Among newborn hospitalizations compared to post-newborn hospitalizations, there were higher proportions of transferred infants and late preterm (34–<37 weeks) births. The distribution of other characteristics were largely similar.
Table 2 shows the results of multivariable logistic regression of the associations between death and risk factors for all infants in the study sample. Factors significantly associated with increased odds of death were male sex with aOR 1.12 (95% CI 1.07–1.18) compared to female sex, extreme (<29 weeks) with aOR 62.19 (55.67–69.47) and 3.80 (3.45–4.18), respectively, compared to moderate (29–<34 weeks) and late prematurity (34–<37 weeks), and insurance types under “other” (Medicare, self-pay, no charge) with aOR 1.78 (1.55–2.04), compared to private insurance. There was a stepwise trend of increasing odds of death with decreasing neighborhood median income. Transfer was associated with decreased odds of death, with aOR 0.84 (0.73–0.96) compared to no transfer, as well as Medicaid with aOR 0.83 (0.77–0.89) compared to private insurance. Using white infants as reference, both black race and Hispanic ethnicity had slightly increased odds of death but without statistical significance, and races identified as “other” had higher odds of death at aOR 1.23 (1.11–1.38).
Separate results of newborn hospitalizations, stratified by race/ethnicity for white, black, and Hispanic infants, are shown in Table 3. During newborn hospitalization, risk factors associated with increased odds of death were identical to those in Table 2, with higher odds of death for male sex, extreme and moderate prematurity, “other” insurance type, and lower neighborhood median income. Transfer status was associated with decreased odds of death. Similar patterns of association were seen within each race/ethnicity, except Medicaid, which was associated with decreased odds of death only among black infants with aOR 0.69 (0.61–0.79) compared to private insurance. Only the lowest median income quartile was associated with increased odds of death among black infants, whereas a stepwise trend with decreasing income was present among white infants, and no association with income was seen among Hispanic infants.
During post-newborn hospitalizations (Table 4), the only risk factor associated with death was transfer status, with aOR 5.02 (3.31–7.61) compared to those not transferred. Among the post-newborn hospitalizations, frequencies of death were too small to permit stratification by race/ethnicity, with relative standard errors that were excessively high for reporting.
Sensitivity analyses, run without subjects missing data on household income and transfer status, found no differences in the results (data not shown).
Discussion
Our study provides new information that risk factors for death differ between newborn and subsequent hospitalizations among preterm infants, and differ by race/ethnicity. During newborn hospitalizations, risk factors for death mirrored those traditionally associated with preterm delivery and infant mortality: male sex, low gestational age, and low neighborhood income. Notably, Medicaid was associated with decreased risk of death, but only among black infants. Thereafter, during post-newborn hospitalizations, only transfer status was associated with increased risk of death.
Our results showed select sociodemographic risk factors for death in the newborn hospitalization period. Although individual-level risk factors have been associated with preterm birth [5,6,7,8], these risk factors – young maternal age, low education attainment, low income, unmarried marital status, short interpregnancy interval – have not been consistently associated with first-year mortality [5, 9, 10]. Other speculated factors contributing to racial disparity in infant mortality include prenatal care utilization [11], participation in prenatal Women, Infants, and Children (WIC) program [12], paternal involvement in child-rearing [13], and hospital-level mortality [14].
Less well known are predictors of infant death that occur after NICU discharge. One challenge is in identification of these deaths; death certificates do not provide complete information that delineate birth vs. subsequent hospitalizations. Although most infant deaths do occur in the hospital, and place of death is reported, there is no other entry in death certificates that specifies whether an infant ever went home from the birth hospitalization. In addition, most neonatal research databases end data collection at NICU discharge. In fact, surprisingly little is known regarding health outcomes of preterm infants after NICU discharge, except for few studies that have examined health care utilization data such as re-admissions [15], emergency room visits [16], and use of prescription medications [17] among preterm infants.
Due to this research gap, we formulated our approach to study infant deaths by hospitalization types, rather than chronological ages. The neonatal and post-neonatal classification is the current standard epidemiological method of reporting infant mortality rates, but today, with improvement in overall survival of preterm infants, it is less relevant in the preterm population. For preterm infants whose length of hospitalization can last for months, the risks of death before and after the cut-off of 28 days are likely unchanged while they remain hospitalized. Instead, by classification based on hospitalization types, we hoped to identify risk factors that differ between the hospital and the community to which they were discharged, which could inform public health efforts towards reducing infant mortality.
Of the risk factors we identified, one modifiable risk factor may be transfer status. Our results showed that during initial birth hospitalization, transfer status was associated with decreased risk of death. This finding seems to agree with existing literature that describe better outcomes among preterm infants delivered at higher-level facilities [18] with larger volume of high-risk deliveries [19]. Additionally, the benefits of antenatal transfer of women at risk of preterm delivery are well described [20], and likely reflect the success of perinatal regionalization efforts [21] to ensure that very low birth weight infants are delivered in level III or IV facilities equipped to handle high-risk neonates. However, comparisons of outcomes between outborn versus inborn infants are difficult, given inherent selection bias and in handling potential confounders in analyses. For example, we may have underestimated the mortality risk of outborn, transferred neonates, since some neonates are selectively retained at birth hospitals – those considered non-viable and died despite resuscitation or electively withdrawn life support, while others may have died during transport itself. Other relevant unknowns in our study population that could have varied between transferred and non-transferred infants, are maternal and neonatal illness severity, prenatal and obstetric care, level of resuscitation required at delivery, neonatal care availability, hospital demographics, and time spent at the preceding hospital. To address this problem, Fang et al. [22] used propensity scoring matching, to create inborn and outborn (transferred) cohorts with similar characteristics. They found that when matched on illness severity, outborn infants were less likely to die compared with inborns, although they had higher rates of comorbidities of prematurity, while without the matched analysis, outborns had higher risk of mortality. Additional research is warranted to accurately discern the groups of comparison, and analyses that take into account the medical complexities in maternal/neonatal illness, may be necessary to understand the contribution of transfer in infant mortality.
For post-newborn hospitalizations, we found that transfer was associated with high risk of death. The explanations for this finding remain unclear. Interhospital transfers are common in everyday neonatal practice, but there is clearly a knowledge gap regarding the outcomes of neonates who undergo transfer [23]. We speculate that the reason for the poor survival may have been the gravity of illness that required transfer to higher level of care. This reinforces the findings in the Nationwide Inpatient Sample (NIS) by Caskey et al. [24], which showed that pediatric patients transferred between hospitals had significantly greater mortality rate compared with patients admitted directly. In adults, transferred patients have more comorbid conditions, greater severity of illness, and 1.4-fold to 2.5-fold higher hospital mortality rates compared to direct admissions [25]. In our study population, due to lack of clinically relevant information, we could not identify and control for such comorbidities. Highlighting elevated severity of disease prior to transfer, Odetola et al. [23] have found that children transferred from referral hospital wards had the highest rates of undergoing CPR on the date of interhospital transfer, compared to transfers from emergency departments or intensive care units. While we did not have this level of clinical information in our study, it is possible that, beyond pre-existing comorbidities alone, timing of transfer played a role in mortality. It has been shown that timely provision of definitive care for acute life-threatening disease is associated with good clinical outcomes [26, 27]. Regionalization in the post-newborn period, similar to perinatal network regionalization, may be warranted to facilitate timely, appropriate transfer prior to deterioration. It will be important to identify barriers to timely transfer, such as insurance status or interhospital communication, and address them by collaboratively building measures including telemedicine capabilities and triage systems between hospitals.
Another potentially modifiable risk factor in our results was insurance status. We found that Medicaid had a protective effect from death compared to private insurance, but only among black infants, and only during newborn hospitalization. Although the reason for this finding is unclear, different patterns of clinical care and neonatal outcomes by insurance status have been described [28], and Medicaid has been associated with increased likelihood of neonatal transfer, compared to those with private insurance [29]. It is also possible that the prenatal benefits of Medicaid contributed partly to decreased mortality. The Medicaid program has an excellent record of financing coverage for pregnant women in low-income populations; approximately 45% of U.S. births are covered by Medicaid [30] and it has made substantial investments in prenatal and postnatal programs to improve maternal and infant health that often serve low-income families. Essential health benefits for low-income women of childbearing age include treatment of chronic disease, substance abuse screening, and increased access to prescribed contraceptives. In Michigan, participation in the program has been associated with decreased neonatal and post-neonatal mortality [31], with decreased odds of death among black infants (OR 0.71, 95% CI 0.58–0.87) and infants of other races (OR 0.74, 95% CI 0.61–0.91) compared to non-participants. The impact has continued with the Affordable Care Act Medicaid expansion, which dramatically increased the number of women eligible for Medicaid coverage by extending eligibility to non-pregnant women with household income up to 138% of federal poverty level. Bhatt et al. have shown that mean infant mortality rate in non-Medicaid expansion states rose (6.4 to 6.5) from 2014 to 2016, but declined in expansion states (5.9 to 5.6) [32]. Declines in infant mortality rates by Medicaid expansion were greatest in African American infants. Although our study could not identify which features of Medicaid account for reduced risk of infant mortality, our finding may be a reflection of quality health care utilization from preconception, prenatal and maternal chronic disease, to mental health management, made possible to minority, low-income, at-risk families through Medicaid.
Our data has important public health implications. To inform policies to improve infant survival, a thorough understanding of risk factors is necessary [21]. The majority of risk factors in our results during the newborn hospitalization were similar to risk factors commonly associated with preterm birth itself. Efforts to decrease infant mortality in premature infants, then, should focus on preventing or delaying preterm birth and optimizing therapies that may decrease complications of prematurity [33]. Ensuring good access to prenatal care, promoting delivery of low birth weight infants at centers with appropriate neonatal care, and consulting high-risk maternal–fetal specialists could reduce mortality in prematurely born infants. It should be recognized that efforts to reduce preterm birth alone will have less impact on the post-newborn aspect of infant mortality. Reducing deaths after birth hospitalization, and the racial disparity in these post-newborn deaths, will require further investigation of medical and social risk factors specific to the home and neighborhood environments, that were not feasible in our analysis, with frequencies of death that were too low to report when stratified by race/ethnicity.
Our study has several other limitations. First is the possible inaccuracy of hospital discharge data, which may have influenced our outcomes. In particular, identification of birth vs. non-birth hospitalization could only be achieved by either MDC or ICD-10 codes. While the MDC code “newborn and other neonates” should have been a match for the ICD-10 code “disorders of newborn related to short gestation”, they did not always align. This may have led to misclassifications of types of hospitalizations, though the differences between identification methods by MDC vs ICD-10 were relatively small (<100). In addition, although the KID is the largest dataset available on pediatric hospitalization data in the U.S., not all states participate in the KID. Although the data are weighted to be nationally representative, it is possible that the participating states may have differed in systematic ways from non-participating states. Similarly, since the database collects data on a hospitalization level, health care utilization on an individual patient level, such as repeated hospitalizations, was not possible. Notably, other variables known to be associated with mortality, such as medical or surgical comorbidities or cause of death were not available. Also unavailable were maternal characteristics known to be associated with infant deaths, and known to differ between race and ethnicity, such as age, prenatal care utilization, educational attainment, marital status, and exposure to smoking.
Despite these limitations, our findings provide new information to the field of infant mortality. With a large population-level data, we confirmed that the well-established risk factors for preterm birth are also risk factors for death, but diminish to transfer status alone after birth hospitalization, without association with gestational age. Medicaid was associated with decreased odds of death only among black race. These findings should lead to further examination of medical and social contributors to infant mortality, and analyses by hospitalization types may offer novel strategies for understanding racial disparities in infant mortality.
In summary, risk factors for death differ between birth and subsequent hospitalizations, and differ by race/ethnicity.
Data availability
Datasets utilized in the paper are publicly available through the Agency for Healthcare Research and Quality at https://www.hcup-us.ahrq.gov/kidoverview.jsp
References
Kochanek KDM, Xu SL, Arias J, Deaths E. Final data for 2017. Natl Vital- Stat Rep. 2019;68:1–76.
Mathews TJ, Driscoll AK. Trends in infant mortality in the United States, 2005-2014. NCHS. Data Brief. 2017;279:1–8.
Health status. 2016. https://www.oecd-ilibrary.org/content/data/data-00540-en.
Xu J, Murphy SL, Kochanek KD, Bastian B, Arias E. Deaths: final data for 2016. Natl Vital- Stat Rep. 2018;67:1–76.
Collins JW Jr, David RJ. The differential effect of traditional risk factors on infant birthweight among blacks and whites in Chicago. Am J Public Health. 1990;80:679–81.
Collins JW Jr, Wall SN, David RJ. Adequacy of prenatal care utilization, maternal ethnicity, and infant birthweight in Chicago. J Natl Med Assoc. 1997;89:198–203.
Berg CJ, Wilcox LS, d’Almada PJ. The prevalence of socioeconomic and behavioral characteristics and their impact on very low birth weight in black and white infants in Georgia. Matern Child Health J. 2001;5:75–84.
Kleinman JC, Kessel SS. Racial differences in low birth weight. Trends and risk factors. N. Engl J Med. 1987;317:749–53.
El-Sayed AM, Tracy M, Galea S. Life course variation in the relation between maternal marital status and preterm birth. Ann Epidemiol. 2012;22:168–74.
Cooperstock MS, Bakewell J, Herman A, Schramm WF. Association of sociodemographic variables with risk for very preterm birth in twins. Obstet Gynecol. 1998;92:53–6.
Byrd DR, Katcher ML, Peppard P, Durkin M, Remington PL. Infant mortality: explaining black/white disparities in Wisconsin. Matern Child Health J. 2007;11:319–26.
Khanani I, Elam J, Hearn R, Jones C, Maseru N. The impact of prenatal WIC participation on infant mortality and racial disparities. Am J Public Health. 2010;100:S204–9.
Ngui EM, Cortright AL, Michalski K. Relationship of paternity status, welfare reform period, and racial/ethnic disparities in infant mortality. Am J Mens Health. 2015;9:350–9.
Howell EA. Racial disparities in infant mortality: a quality of care perspective. Mt Sinai J Med. 2008;75:31–5.
Underwood MA, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalization of preterm infants. J Perinatol. 2007;27:614–9.
Kuzniewicz MW, Parker SJ, Schnake-Mahl A, Escobar GJ. Hospital readmissions and emergency department visits in moderate preterm, late preterm, and early term infants. Clin Perinatol. 2013;40:753–75.
Wade KC, Lorch SA, Bakewell-Sachs S, Medoff-Cooper B, Silber JH, Escobar GJ. Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol. 2008;28:696–701.
Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109:745–51.
Jensen EA, Lorch SA, Association between off-peak hour birth and neonatal morbidity and mortality among very low birth weight infants. J Pediatr. 2017;186:41–48.e4.
Shah KP, deRegnier RO, Grobman WA, Bennett AC. Neonatal mortality after interhospital transfer of pregnant women for imminent very preterm birth in Illinois. JAMA Pediatr. 2020;174:358–65.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304:992–1000.
Fang JL, Mara KC, Weaver AL, Clark RH, Carey WA. Outcomes of outborn extremely preterm neonates admitted to a NICU with respiratory distress. Arch Dis Child Fetal Neonatal Ed. 2020;105:33–40.
Odetola FO, Davis MM, Cohn LM, Clark SJ. Interhospital transfer of critically ill and injured children: an evaluation of transfer patterns, resource utilization, and clinical outcomes. J Hosp Med. 2009;4:164–70.
Caskey RN, Davis MM. Differences associated with age, transfer status, and insurance coverage in end-of-life hospital care for children. J Hosp Med. 2008;3:376–83.
Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA. Accepting critically ill transfer patients: adverse effect on a referral center’s outcome and benchmark measures. Ann Intern Med. 2003;138:882–90.
Sampalis JS, Denis R, Frechette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997;43:288–95. discussion 95-6.
Rapoport J, Teres D, Lemeshow S, Harris D. Timing of intensive care unit admission in relation to ICU outcome. Crit Care Med. 1990;18:1231–5.
Brandon GD, Adeniyi-Jones S, Kirkby S, Webb D, Culhane JF, Greenspan JS. Are outcomes and care processes for preterm neonates influenced by health insurance status?. Pediatrics. 2009;124:122–7.
Durbin DR, Giardino AP, Shaw KN, Harris MC, Silber JH. The effect of insurance status on likelihood of neonatal interhospital transfer. Pediatrics. 1997;100:E8
Gifford K, Walls J, Ranji U, Salganicoff A, Gomez I. Medicaid coverage of pregnancy and perinatal benefits: results from a state survey. April 2017, https://files.kff.org/attachment/Report-Medicaid-Coverage-of-Pregnancy-and-Perinatal-Benefits [accessed March 2022].
Meghea CI, You Z, Raffo J, Leach RE, Roman LA. Statewide medicaid enhanced prenatal care programs and infant mortality. Pediatrics. 2015;136:334–42.
Bhatt CB, Beck-Sague CM. Medicaid expansion and infant mortality in the United States. Am J Public Health. 2018;108:565–7.
Jacob J, Kamitsuka M, Clark RH, Kelleher AS, Spitzer AR. Etiologies of NICU deaths. Pediatrics 2015;135:e59–65.
Author information
Authors and Affiliations
Contributions
Drs. Matoba and Davis conceptualized and designed the study and drafted the initial manuscript. Dr. Kwon carried out the statistical analyses, reviewed and revised the manuscript. Drs. Collins and Davis critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matoba, N., Kwon, S., Collins, J.W. et al. Risk factors for death during newborn and post-newborn hospitalizations among preterm infants. J Perinatol 42, 1288–1293 (2022). https://doi.org/10.1038/s41372-022-01363-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01363-z
- Springer Nature America, Inc.
This article is cited by
-
End of life care in a level IV outborn neonatal intensive care unit
Journal of Perinatology (2024)