Abstract
Objective
Fetal ventriculomegaly may occur in isolation or as part of a broader syndrome. We aimed to determine the added value of magnetic resonance imaging (MRI) for informing the pre-natal and postnatal care of pregnancies complicated by ventriculomegaly (VM).
Study design
Retrospective analysis of all cases of prenatally diagnosed VM referred to the fetal center at Lucile Packard Children’s Hospital Stanford 1/1/2009–6/1/2014 were reviewed. Ultrasound (US) and MRI findings were reviewed, and the added yield of MRI evaluated.
Results
A total of 91 cases of fetal VM were identified and 74 (81%) underwent MRI. In 62/74 (84%) cases, additional CNS or non-CNS findings, not seen on US, were discovered on MRI, of which 58 were CNS-related. Forty-six (62%) of the additional findings were considered clinically relevant, of which 45 were CNS-related.
Conclusion
Fetal MRI identifies additional, clinically relevant CNS and non-CNS findings in a majority of cases of VM following initial US.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Ventriculomegaly (VM), or enlargement of the lateral ventricles, is the most common central nervous system (CNS) anomaly identified using prenatal imaging techniques [1]. Fetal VM affects approximately 1 in 1000 live births and prognosis varies widely depending on the severity, associated brain malformations, and presence of other congenital anomalies. Fetuses classified as having mild, isolated VM (10 to 12 mm in diameter) have more favorable outcomes than those with severe ventricular dilation or additional CNS abnormalities [2]. Therefore, it is important that the diagnosis of all associated anomalies be accurate and complete.
VM is typically diagnosed during a routine second trimester anatomy ultrasound (US). However, the rate of associated malformations, both CNS and non-CNS, may be underestimated at the time of US diagnosis [3, 4]. Fetal magnetic resonance imaging (MRI) is the recommended modality to further characterize CNS anomalies detected on US, which may inform prognosis. Estimates of rates of additional findings identified by fetal MRI range widely from 5 [5] to 50% [6]. Because MRI provides high resolution imaging of the entire fetus, it may also assist with detecting non-CNS abnormalities. The importance of these additional MRI findings in directing prenatal and delivery planning, counseling, and postnatal care arrangements is not well described in the literature.
We describe the range of associated anomalies in prenatally diagnosed VM in a single, quaternary care center. We also evaluate the added value of fetal MRI for identifying additional CNS and non-CNS findings informing prenatal and postnatal clinical management planning in fetal VM cases, including utilizing reassuring findings to allow for local delivery with prospective postnatal planning.
Material and methods
Study population
All cases of prenatally diagnosed VM referred to The Fetal and Pregnancy Health Program at Lucile Packard Children’s Hospital Stanford (LPCHS) between 1/1/2009 and 6/1/2014 were reviewed. The fetal center database was established prospectively in 2009, was approved by the Stanford University Institutional Review Board under an expedited review process, and has been renewed annually. A search was carried out to identify all cases referred for or identified with VM of any severity. In our institution, VM is defined as any enlargement of the lateral ventricle greater than or equal to 10 mm.
Upon diagnosis of fetal VM by US, patients are offered genetic counseling, genetic testing if not already done (including amniocentesis for karyotype or microarray, and non-invasive prenatal testing when it became available during the study period), evaluation for congenital viral infections based on maternal serum serology, and fetal MRI. Patients may have declined any or all offers of or recommendations for genetic or other testing. Additional multidisciplinary prenatal consultations, including with pediatric neurology, are offered to patients and families based on fetal findings.
Data collection and definitions
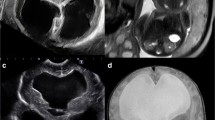
A retrospective chart review and analysis of fetal US and MRI findings were performed. All cases underwent a detailed anatomical US survey at LPCHS or an affiliated LPCHS satellite, all of which have common standardized protocols based on the American Institute of Ultrasound in Medicine guidelines [7]. Images of the lateral ventricles were obtained in an axial transventricular plane. Measurements of the atrium of the lateral ventricles were performed at the level of the glomus of the choroid plexus, positioning the calipers inside the echoes generated by the lateral walls at the widest part of the ventricle opposite the internal parieto-occipital sulcus. The US reports were reviewed and ventricle measurements and laterality of VM were recorded [8, 9]. For the purpose of this study, the width of the larger of the two ventricles was recorded if the process was asymmetric. The VM was classified as mild (10–12 mm), moderate (13–15 mm), or severe (>15 mm) [3, 10] based on the initial US at diagnosis at our institution. US images were reviewed in some cases for clarification of measurements by a single investigator with prenatal US expertise (YJB) masked to the other findings and outcomes. Based in part on the findings of the initial US, subsequent US exams were obtained as per provider clinical recommendations and gestational age. If more than one US was performed, the maximum ventricle measurement of all US exams was also recorded. For patients who received only one US, the initial US and maximum US measurements were the same. MRI scans were obtained on either a 1.5 Tesla (GE MR 450 W) or 3.0 Tesla (GE 750) scanner (General Electric Healthcare, Chicago, IL). Single shot fast spin echo images of the fetal brain were obtained in three planes. Brain findings on MRIs were read by experienced neuroradiologists and body findings were read by pediatric radiologists with expertize in fetal MRI (RB, ER, PB). The classifications were based on the interpretations of these experts. New findings and clarifications provided by MRI, as well as clinically relevant added value of MRI findings, were assessed. Potential “clinical relevance” of MRI findings was assessed by chart review of provider notes, and was defined as findings assisting in any of the following: (1) directing consultations, (2) recommendation of delivery venue, (3) need for postnatal imaging, (4) other follow up recommendations, or (5) providing clarifying information that influenced patient decision for continuation of pregnancy. Importantly, not all findings deemed clinically relevant were of equivalent severity, and some findings were deemed relevant in that they provided reassurance. To allow for applicable analyses, the level of clinical relevance with regard to postnatal concern, whether reassuring or concerning, was ranked using a Likert scale (1–5, in increasing order of relevance) by three investigators (ASD, VYC, SRH), who were masked to patient identifiers and neonatal outcomes. If, based on the scoring of the investigators, the finding had an average Likert scale ranking of ≥3, it was considered clinically relevant. Findings were ranked independently and discrepancies were adjudicated collectively.
Analysis
Descriptive analyses of the cohort findings were performed to determine the added benefit of fetal MRI compared to initial prenatal US alone in differentiating cases of fetal VM (Microsoft Excel, Redmond, WA). Logistic regression using SAS version 9.3 (Cary, NC) was performed to determine the association between the severity of VM by initial US and the clinical relevance of MRI findings without adjustment for covariates.
Results
Ninety-one cases of VM were referred to our fetal center from approximately 1300 total referrals to the LPCHS fetal center during the study period (7%), and all received at least one US. The median gestational age at the time of initial US exam at our center was 26 weeks (IQR 22–31 weeks) (Table 1). Based on this initial US at diagnosis, 37 cases were classified as mild (10–12 mm), 19 cases as moderate (13–15 mm), and 28 as severe (>15 mm). The remaining seven cases were referred for VM due to a finding of VM at an outside institution, but ventricles were determined to be < 10 mm bilaterally on initial US at LPCHS.
Among the cases in which genetic counseling and testing were pursued, results were available in the medical record in 36 cases: four cases of aneuploidy were detected, including two cases of trisomy 21, one case of trisomy 13, and one case of trisomy 8. In 36 cases, maternal viral serology results were available in the medical record; none of the results were consistent with recent infection.
Of the 91 patients referred for suspected fetal VM, 88 (97%) were offered fetal MRI and 74 (81%) had MRIs performed. Of the three cases where a fetal MRI was not offered, two were classified as severe and one as mild by US measurements. In the two cases of severe VM where an MRI was not offered, one patient presented at 36 weeks, and MRI was deferred until after delivery; in another case, a fetal MRI had been performed at an outside institution. The majority of MRIs were performed using a 1.5 Tesla scanner during this period. In one case the 3.0 Tesla scanner was used.
Among the 74 MRIs performed, the median gestational age at MRI was 28 weeks. There were 30 cases in which MRI altered the level of severity of VM compared to US. In 21 of these cases, MRI found the ventricles to be more enlarged than was seen on US (nine cases changed from mild on US to moderate on MRI, seven cases from moderate on US to severe on MRI, four cases from no VM on US to mild on MRI, and one case from no VM on US to severe on MRI). In nine cases, MRI found the ventricles to be less enlarged than was seen on US (six cases changed from moderate on US to mild on MRI, one case from mild on US to no VM on MRI, one case from severe on US to moderate on MRI, and one case from severe on US to mild on MRI). In 62/74 (84%) cases, additional CNS or non-CNS findings were seen on MRI that were not detected by prenatal US. In 20 of these cases, non-CNS findings were seen, which included obstetric, craniofacial, pulmonary, gastrointestinal, and renal/urogenital anomalies. In 58/74 (78%) cases, additional CNS findings were seen on MRI. These additional findings included cortical, posterior fossa, and midline anomalies, as well as additional ventricular anomalies (Table 2).
Additional CNS findings detected by MRI were assessed as clinically relevant in 45/74 (61%) cases. Additional clinically relevant non-CNS findings were seen in 14/74 cases (19%). When assessing both CNS and non-CNS findings together, the additional findings detected by MRI were determined to be clinically relevant in 46/74 (62%) cases. These clinically relevant additional CNS and non-CNS findings were seen across all levels of VM severity; however, they were most frequently observed in cases that were classified as severe on the initial US measurement (Table 3a and b). Among the cases receiving an MRI, 21 of the 21 (100%) cases which had been classified as severe, 12 of 19 cases (63%) which had been classified as moderate, and 11 of 28 cases (39%) which had been classified as mild on initial US had clinically relevant additional CNS or non-CNS findings seen on MRI. There were six cases which were referred for, and received, fetal MRI for primary concern of VM, but the US at our institution did not confirm VM. However, in two of these six cases (33%), clinically relevant additional findings were seen on MRI. These additional clinically relevant findings in the cases where VM was not confirmed included a small inferior vermis, a cleft lip/palate, findings concerning for a bronchopulmonary anomaly, and findings concerning for Hirschsprung’s disease. There was a significant association between moderate or severe VM by US and the clinical significance of MRI findings (OR 7.6 [95% CI 2.6–22], p = 0.0002) compared to none or mild VM. While non-CNS findings were less frequently seen, they were present across all levels of VM severity.
Among the 46 cases in which additional findings by fetal MRI were deemed to be clinically relevant: 42 directed prenatal consults, 22 directed postnatal consults, four altered the delivery location to a tertiary care center, 29 resulted in recommendations for postnatal imaging, 23 directed counseling or postnatal follow up recommendations, and ten provided information affecting the patient’s decision to terminate the pregnancy (Supplemental Table 1). Within each category of clinical relevance, cases ranged from no VM to severe VM seen on initial US (Table 4).
In the 42 cases where MRI findings helped to direct the recommendation for prenatal consults, neurology consults were most frequently recommended (26), followed by neonatology (23), genetics (20), and neurosurgery (15), respectively. In the 22 cases where MRI findings helped to direct the recommendation for postnatal consults, neurology consults were the most frequently recommended (15), followed by neurosurgery (14), genetics (9), and ophthalmology (4). The need for these more specific consultation services were guided by MRI findings, particularly in those cases with moderate or severe initial US findings.
Prenatal MRI altered delivery location to a tertiary center in only four cases (Supplemental Table 2). In all four cases, review of initial US findings by a multidisciplinary team had suggested that local delivery was an appropriate option; however, additional findings on MRI indicated that immediate intensive care or intervention may be required postnatally, necessitating delivery at a tertiary care institution. In contrast, MRI provided reassuring information to permit local delivery in 41 cases if VM was mild, isolated, and if feasible for appropriate prenatal consultations, communication to primary providers, and planning for postnatal neonatal management and follow up.
Discussion
In this study, we examined the value added by MRI to identify additional findings in prenatally diagnosed VM, and to inform prenatal and postnatal clinical decisions. Our results show that MRI provides valuable information regarding clinically relevant CNS and non-CNS findings in approximately two-thirds of the cases. Although these additional findings were seen most frequently among severe VM cases, they were encountered across all levels of VM severity, and served to direct prenatal consultation, postnatal imaging, and follow up recommendations. MRI may also be helpful as an adjuvant to US: in the case where VM was not detected on US, the MRI permitted enhanced visualization of a ventricle to clarify that severe, unilateral VM was indeed present. Importantly, we demonstrate that not all additional findings necessarily require delivery at a tertiary center; only four of the 46 cases in which fetal MRI provided additional clinically relevant information resulted in change of delivery venue to a tertiary center, while the vast majority provided information to confidently allow for local delivery, often after prenatal consultations and creation of a postnatal management and follow up plan.Footnotes b in Table 3a and a in Table 3b is not linked to anything in the body of Tables. Please indicate where “a,b” should be inserted or delete the footnote.Thank you for noting this oversite. I have inserted "a" and "b" as requested in the tables - they appear at end of the titles.
Our study is unique in its focus on the ways in which MRI affects decisions about prenatal care and consultation, direction of delivery venue, and postnatal recommendations and follow up among those with prenatally diagnosed VM. Previous studies have primarily focused on describing additional findings detected by fetal MRI [2, 11,12,13] or neurodevelopmental outcomes for apparently isolated severe [14] or mild VM [15] identified prenatally. The inclusion of broader prenatal and perinatal consultation and management decisions as part of our analysis is a different approach and may explain why we report greater percentage of findings deemed clinically significant on MRI as compared with previous studies. Parazzini et al. [16] analyzed 179 cases of fetal VM and reported that MRI provided additional important information in only two cases (1.1%). One fetus had bilateral frontal schizencephaly and agenesis of the septum pellucidum and the other had isolated agenesis of the septum pellucidum. Kandula et al. [17] reported 40 cases of mild fetal VM and similarly found clinically relevant additional findings in only three cases (7.5%). However, these studies defined additional information of importance or relevance as altering the clinical prognosis of the pregnancy or with the potential to negatively influence prenatal counseling offered to the parents. Findings that were reassuring or which helped to guide the short-term management of the pregnancy or immediate postnatal period were not included in these definitions, and thus the importance of these findings in guiding clinical decision-making may be underestimated.
Based on our analyses, only rarely did MRI findings lead to a change in delivery venue to a tertiary center; rather, in the majority of cases MRI provided reassuring information to allow prospective planning for local delivery. However, decisions about delivery venue may be influenced by regional resources and capabilities. A study conducted by Irwin et al. [18] similarly described the ability of MRI to alter prognosis in both positive and negative ways. This study included 57 pregnancies prenatally diagnosed with a CNS anomaly by US, where MRI altered the diagnosis in 31 (54%) cases. Among these 31 cases, in 17 (55%), MRI findings served to worsen the prognosis; however, in 14 cases (45%), MRI findings actually improved the prognosis [18].
Our results suggest that MRI may be useful in providing reassuring information, permitting the local delivery of infants with prenatally diagnosed VM, even if additional information was gained by fetal MRI not seen by US. A goal for referral centers, including ours, and consistent with the tenets of family-centered care, is to allow mothers to deliver their infants at their local hospital if the infant does not require immediate higher level of care or intervention. By utilizing the additional information gained by fetal MRI, physicians may be able to more accurately predict which infants will need intensive evaluations or interventions soon after birth. This may lead to more confident prenatal predictions of postnatal needs, and providers may be more secure in recommending that infants be born at their local hospital after appropriate prenatal consultations, and with planned outpatient follow up. Postnatal MRI capabilities may not always be available at the local delivery venue, and as such a fetal MRI might obviate the perceived need for a neonatal brain MRI scan in the immediate postnatal period.
The critical importance of a multidisciplinary approach to fetal care and planning cannot be underestimated. The precepts of comprehensive involvement of maternal-fetal medicine specialists, neonatologists and other appropriate pediatric subspecialists presented by ACOG and AAP should not be applied only to cases in which fetal intervention is anticipated [19]. In one study, anxiety and depression scores and symptoms were reduced in women whose pregnancies were affected by fetal anomalies by comprehensive prenatal counseling [20]. Our study underscores the importance of fetal MRI in providing a comprehensive assessment of the fetus for prognostic counseling.
Our study is limited by its retrospective, descriptive design in a single center. Referral bias may also be an issue given that more severe or complex cases are likely to be referred to our fetal center. There were also cases in which the interval of time between the initial US and MRI was prolonged. The median gestational age at US was 26 weeks versus a median gestational age of 28 weeks at MRI. In these cases, it is possible that the additional findings seen on MRI were not due to the imaging modality itself, but rather, because findings may have been more easily detected later in gestation, or even that new findings emerged during this time period. However, Griffiths et al. described 570 cases with a fetal brain abnormality detected by US at a gestational age of ≥ 18 weeks. Prenatal US alone provided a correct diagnosis in 68% of cases when compared with postnatal assessment. However, MRI, when performed within two weeks of the US, was accurate in 93% of cases [21]. We were also unable to assess technical factors, which may have limited the diagnostic ability of the US exams including maternal BMI, prior abdominal surgery, etc. The Likert scale utilized to determine potential clinical relevance of MRI findings is not a validated tool and may be limited by subjectiveness, but provided a quantitative method for data analysis across independent reviewers. Additionally, congenital viral testing and genetic testing results were available in only some of our cases. Previous work by Tugçu et al. [22] described chromosome abnormalities in approximately 11% of the VM cases who underwent karyotype analysis and congenital infection in 2.5% of cases. More complete data in these areas may have enhanced understanding of the etiology of VM in our cohort.
Directions for future research include evaluation of neonatal and later infancy neuroimaging findings and other outcomes after prenatally diagnosed VM. Such analyses will allow for evaluation of the capabilities of fetal US and MRI, alone and in combination, to predict postnatal findings. In addition, evaluating postnatal neurodevelopmental and functional outcomes with regard to fetal imaging findings will allow for a more complete understanding of the impact of fetal VM with or without additional findings seen by MRI.
In summary, fetal MRI was able to identify clinically relevant CNS and non-CNS findings in nearly two-thirds of fetal VM following initial US evaluation. Not only did MRI add value to the prenatal assessment of VM, both in terms of identifying additional CNS and non-CNS findings, but MRI also directed appropriate use of expanded consulting services and approaches, diagnostic testing, and ultimate recommendations for delivery location and follow up. The focus of this study on the ability of MRI to provide complementary data and often reassurance, supply information important to accurate counseling, and clarify postnatal care needs, is a differentiator from previous analyses.
References
Garel C, Luton RJ. Ventricular dilatations. Childs Nerv Syst. 2003;19:301–8.
Benacerraf BR, Shipp TD, Bromley B, Levine D. What does magnetic resonance imaging add to the prenatal sonographic diagnosis of ventriculomegaly? J Ultrasound Med. 2007;26:1513–22.
Gaglioti P, Oberto M, Todros T. The significance of fetal ventriculomegaly: etiology, short- and long-term outcomes. Prenat Diagn. 2009;29:381–8.
Pilu G, Falco P, Gabrielli S, Perolo A, Sandri F, Bovicelli L. The clinical significance of fetal isolated cerebral borderline ventriculomegaly: report of 31 cases and review of the literature. Ultrasound Obstet Gynecol. 1999;14:320–6.
Salomon LJ, Ouahba J, Delzoide AL, Vuillard E, Oury JF, Sebag G, et al. Third trimester fetal MRI in isolated 10 to 12 mm ventriculomegaly: is it worth it? BJOG. 2006;113:942–7.
Morris JE, Rickard S, Paley MN, Griffiths PD, Rigby A, Whitby EH. The value of in-utero magnetic resonance imaging in ultrasound diagnosed foetal isolated cerebral ventriculomegaly. Clin Radiol. 2007;62:140–4.
American Institute of Ultrasound in Medicine. AIUM practice guideline for the performance of obstetric ultrasound examinations. J Ultrasound Med. 2013;32:1083–101.
International Society of Ultrasound in Obstetrics & Gynecology Education Committee. Sonographic examination of the fetal central nervous system: guidelines for performing the ‘basic examination’ and the ‘fetal neurosonogram’. Ultrasound Obstet Gynecol. 2007;29:109–16.
Guibaud L, Lacalm A. Etiological diagnostic tools to elucidate ‘isolated’ ventriculomegaly. Ultrasound Obstet Gynecol. 2015;46:1–11.
Manganaro L, Savelli S, Francioso S, DiMaurizio M, Coratella F, Vilella G, et al. Role of fetal MRI in the diagnosis of cerebral ventriculomegaly assessed by ultrasonography. Radiol Med. 2009;114:1013–23.
Garcia-Flores J, Recio M, Uriel M, Cañamares M, Cruceyra M, Tamarit I, et al. Fetal magnetic resonance imaging and neurosonography in congenital neurological anomalies: supplementary diagnostic and postnatal prognostic value. J Matern Fetal Neonatal Med. 2013;26:1517–23.
Kul S, Korkmaz HA, Cansu A, Dinc H, Ahmetoglu A, Guven S, et al. Contribution of MRI to ultrasound in the diagnosis of fetal anomalies. J Magn Reson Imaging. 2012;35:882–90.
Yin S, Na Q, Chen J, Li-Ling J, Liu C. Contribution of MRI to detect further anomalies in fetal ventriculomegaly. Fetal Diagn Ther. 2010;27:20–4.
Kennelly MM, Cooley SM, McParland PJ. Natural history of apparently isolated severe fetal ventriculomegaly: perinatal survival and neurodevelopmental outcome. Prenat Diagn. 2009;29:1135–40.
Pagani G, Thilaganathan B, Prefumo F. Neurodevelopmental outcome in isolated mild fetal ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2014;44:254–60.
Parazzini C, Righini A, Doneda C, Arrigoni F, Rustico M, Lanna M, et al. Is fetal magnetic resonance imaging indicated when ultrasound isolated mild ventriculomegaly is present in pregnancies with no risk factors? Prenat Diagn. 2012;32:752–7.
Kandula T, Fahey M, Chalmers R, Edwards A, Shekleton P, Teoh M, et al. Isolated ventriculomegaly on prenatal ultrasound: what does fetal MRI add? J Med Imaging Radiat Oncol. 2015;59:154–62.
Irwin K, Henry A, Gopikrishna S, Taylor J, Welch AW. Utility of fetal MRI for workup of fetal central nervous system anomalies in an Australian maternal-fetal medicine cohort. Aust N Z J Obstet Gynaecol. 2016;56:267–73.
American College of Obstetricians and Gynecologists. Committee on Ethics; American Academy of Pediatrics. Committee on Bioethics. Committee opinion no. 501: maternal-fetal intervention and fetal care centers. Obstet Gynecol. 2011;118(2 Pt 1):405–10.
Gorayeb RP, Gorayeb R, Berezowski AT, Duarte G. Effectiveness of psychological intervention for treating symptoms of anxiety and depression among pregnant women diagnosed with fetal malformation. Int J Gynaecol Obstet. 2013;121:123–6.
Griffiths PD, Bradburn M, Campbell MJ, Cooper CL, Graham R, Jarvis D, et al. Use of MRI in the diagnosis of fetal brain abnormalities in utero (MERIDIAN): a multicentre, prospective cohort study. Lancet. 2017;389:538–46.
Tugçu AU, Gulumser C, Ecevit A, Abbasoglu A, Uysal NS, Kupana ES, et al. Prenatal evaluation and postnatal early outcomes of fetal ventriculomegaly. Eur J Paediatr Neurol. 2014;18:736–40.
Acknowledgements
This study was funded by a Medical Scholars Research Program grant from Stanford University School of Medicine (JAK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Katz, J.A., Chock, V.Y., Davis, A.S. et al. Utility of prenatal MRI in the evaluation and management of fetal ventriculomegaly. J Perinatol 38, 1444–1452 (2018). https://doi.org/10.1038/s41372-018-0208-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0208-6
- Springer Nature America, Inc.
This article is cited by
-
Role of fetal MRI to diagnose abnormal cerebral ventricular system and associated fetal brain anomalies
Egyptian Journal of Radiology and Nuclear Medicine (2022)
-
Fetal therapy for congenital hydrocephalus—where we came from and where we are going
Child's Nervous System (2020)