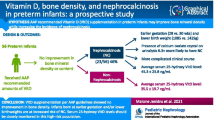
Abstract
Objective
To identify the vitamin D status to optimize calcium and bone health in preterm infants.
Study design
Very low birth weight infants had measurement of 25-hydroxyvitamin D status and markers of calcium and bone health from birth to term age. Piecewise linear regression modeling was performed to identify a 25-hydroxyvitamin D threshold associated with stable parathyroid hormone concentration and bone mineralization.
Results
In a cohort of 89 infants at term age, femur BMC and density increased linearly with 25-hydroxyvitamin D status until reaching a threshold of 48 ng/mL and 46 ng/mL, respectively. Parathyroid hormone status decreased as vitamin D status increased until reaching a plateau at 25-hydroxyvitamin D of 42 ng/mL.
Conclusion
Preterm infant vitamin D status was significantly associated with PTH status and femur mineralization with suggestion that achieving a specific 25-hydroxyvitamin concentration is associated with optimal calcium homeostasis and femur bone mineralization.
Similar content being viewed by others
Introduction
Emphasis on vitamin D health has grown through the past two decades with resurgence in rickets, revised definitions of vitamin D deficiency, and recognition of vitamin D’s importance in health beyond calcium homeostasis. For infants, historically, vitamin D deficiency was defined as the low vitamin D status measured in infants with rickets. If rickets was not apparent, then vitamin D health was assumed. More recent work has focused on the vitamin D status or circulating 25-hydroxyvitamin D [25(OH)D] concentration associated with optimal physiologic function of vitamin D-dependent processes. These contemporary studies disregard previous definitions of vitamin D status and, instead, aim to identify whether a specific 25(OH)D threshold is associated with achieving peak system function [1, 2].
For preterm infants, studies of calcium homeostasis and bone mineralization have demonstrated a muted role of vitamin D in these processes [3,4,5,6]. Yet, these studies are limited by predetermined definitions of ‘normal’ vitamin D and parathyroid hormone concentrations and by inadequacies in bone mineralization measurement techniques. Consequently, the objective of this study was to identify whether vitamin D status, as indicated by circulating 25(OH)D concentration, is associated with calcium equilibrium and bone mineralization in very low birth weight infants, and, if so, whether a specific threshold of 25(OH)D status is related to optimizing these processes.
Methods
Subjects
The Institutional Review Board of the Medical University of South Carolina approved this study. This was a single-center, prospective, observational study of very low birth weight infants born at less than 34 weeks’ postmenstrual age. Only infants with birth weight parameter defined as appropriate-for-gestational age (AGA) by Fenton growth chart were included in the study [7]. Infants with major congenital anomalies or born to mothers with history of parathyroid disease were not eligible for the study. Written informed consent was obtained from the parents either prior to or within three days of infant birth.
Measurements
Enrolled participants had daily measurement of vitamin D, calcium, and phosphorus intake while inpatient. If the participant was discharged prior to term age, parent provided feeding type and volume at study visit. Intake was calculated as the average of the day of discharge and parental report. Subjects had measurements of total body circulating 25(OH)D, calcium, and phosphorus homeostasis indicators assessed within three days of birth, one-month postnatal age, and at term-age equivalent. Term age was defined as 37–40 weeks’ postmenstrual age. At the term age visit, femur and lumbar spine bone mineralization were measured. Calcium and phosphorus homeostasis indicators measured were total calcium, inorganic phosphorus, alkaline phosphatase, and parathyroid hormone (PTH) in serum. Calcium and inorganic phosphorus were measured in the urine at one month and at term age, but not at the birth time point. Patient demographic and outcome data were collected.
Both urinary calcium and phosphorus measurements were standardized as a ratio to urinary creatinine and are presented as urinary calcium excretion and urinary phosphorus excretion. Serum 25(OH)D was measured by radioimmunoassay and serum intact PTH by immunoradiometric assay (Diasorin Corporation, Stillwater, MN). The 25(OH)D radioimmunoassay does not measure 25(OH)D epimers. Other serum and urinary measurements were performed in the Hospital Clinical Chemistry Laboratory using standard methodology. At term age, infant bone mineral content (BMC) and bone mineral density (BMD) were measured specifically at two regions—the left whole femur and the lumbar spine (vertebrae 1–4) by dual energy X-ray absorptiometry (DEXA) scan [Hologic Discovery A infant whole-body software (Malborough, MA)]. A single technician performed all evaluations.
Data analysis
Median and interquartile values for each indicator at each of the three time points were estimated. Association between the indicators and 25(OH)D was assessed by Spearman’s correlation coefficients. For each indicator at each time point, scatter plots were generated to graphically display the nature of monotonic associations with 25(OH)D status.
The primary outcome of this study was to identify if an association existed between serum 25(OH)D and PTH at term age and to examine whether a threshold of 25(OH)D status was associated with a leveling (plateau) of PTH concentration. To achieve this, piecewise linear regression models were used to estimate the parameters describing the association and the level of 25(OH)D at which the threshold occurred. This piecewise regression model, in addition to estimating the threshold, could also produce the estimates of association between 25(OH)D and PTH prior to and post that threshold. Similar piecewise models were also considered for the indicators of bone mineralization. If the estimated threshold and its corresponding 95% confidence interval (CI) were not in the range of the observed data, then it was determined that a piecewise linear regression model was not appropriate, and a simple linear regression model (monotonic relationship) was deemed adequate to evaluate the association. For models where the threshold could be estimated, the results were tabulated, and the fitted models were graphed.
The mathematical form of the piecewise regression model with two linear components is,
where y is the outcome (i.e., PTH at term age), x is 25(OH)D status, λ is the unknown threshold of the 25(OH)D level at which the trajectory potentially plateaus, α and α′ are the y-intercepts for the model prior and post the threshold, and β1 and (β1 + γ) are the slopes prior and post threshold, respectively. In this model, it was anticipated that the slope after the threshold, namely, (β1 + γ) would be zero if the outcome reached a plateau after the 25(OH)D concentrations reached λ. This model is more informative than quadratic or other non-linear models because it identifies a concentration of 25(OH)D with potential for clinical use to define sufficient 25(OH)D status. The estimation of the parameters was performed using a non-linear model fitting approach using a SAS macro with PROC NLIN (SAS Institute Inc. Cary, NC). The thresholds are presented as the 25(OH)D status with the corresponding 95% CI.
Results
Between 5 June 2008, and 16 December 2010, 97 infants were enrolled in the study. Eighty-nine infants were included in the analysis with infants excluded for being small-for-gestational age (n = 3), and, therefore, not meeting the inclusion criteria of birth AGA status; exiting the study by maternal request or by death in the first postnatal week (n = 3); and for fetal drug exposures (immunosuppressant and antiviral medication) with known severe bone effect (n = 2).
The 89 infants included in the analysis had median (interquartile range) birth weight of 1105 (900, 1280) grams and postmenstrual age of 28 (26, 29) weeks with 62% identified as African American. The median (interquartile range) intake through the study were vitamin D 609 (519,678) IU/day, calcium 182 (141, 244) mg/kg/day, and phosphorus 122 (85, 165) mg/kg/day. In this cohort, common birth-hospitalization preterm infant diagnoses (percent with diagnosis) included bronchopulmonary dysplasia (48%), culture-proven sepsis (20%), necrotizing enterocolitis stage ≥ 2a (8%), renal disease (12%), patent ductal arteriosus (28%), intraventricular hemorrhage (26%), and retinopathy of prematurity (28%). Hospital length of stay was a median (interquartile range) of 48 (36, 64) days. Two infants died after the first postnatal week and prior to term age. The term age visit occurred at a median [interquartile range (IQR)] of 69 (57,82) postnatal days and gestational age at 37.6 [36.6, 38.7] weeks. The occurrence of term age visits at 36 weeks’ gestation was due to coordination of outpatient term age visits with routine ophthalmology visits for subjects with transportation difficulties.
At each of the three study visits, subjects had their measurement of serum 25(OH)D and indicators of calcium, phosphorus, and bone health taken. The median (IQR) for each indicator at each time point is shown in Table 1. Median serum 25(OH)D, calcium, phosphorus, and alkaline phosphatase increased over time while median PTH decreased. Urinary excretion of calcium and phosphorus were both relatively stable between one month and term age. Bone mineralization measurements were only performed at term age.
Evaluation of whether an association of vitamin D status and these indicators exists began with assessment for a monotonic relationship. Scatter plots of each indicator and 25(OH)D status at birth (Fig. 1), one month (Fig. 2), and term age (Fig. 3) are presented. Weak, but statistically significant, positive rank order correlations were observed between 25(OH)D status and serum calcium at birth and at one postnatal month but not at term age. For serum phosphorus and 25(OH)D status, a significant positive correlation was only seen at one month. For PTH and 25(OH)D, significant negative correlations were observed at both one month and term age but not at birth. Serum alkaline phosphatase and 25(OH)D were positive correlated at birth and then negatively correlated at term age, with no significant correlation at one month. For urinary excretion of calcium and phosphorus, 25(OH)D had a significant positive correlation with urinary calcium excretion and a significant negative correlation with urinary phosphorus excretion at term age only. For the bone mineralization evaluation at term age, 25(OH)D status was significantly, positively correlated with both femur BMC and BMD but not with spine mineralization measurements.
Monotonic relationships between plasma 25(OH)D status and calcium, phosphorus, and bone health marker at birth. Spearman correlation coefficients (r) and associated p-value for 25(OH)D and specific factors were: serum calcium r = +0.25 (p = 0.02); serum phosphorus r = −0.1 (p = NS); PTH r = −0.17 (p = NS); alkaline phosphatase r = 0.23 (p = 0.04). NS denotes ‘not statistically significant’ for p-values > 0.05
Monotonic relationships between plasma 25(OH)D status and calcium, phosphorus, and bone health markers at 1 postnatal month. Spearman correlation coefficients (r) and associated p-value for 25(OH)D and specific factors were: serum calcium r = +0.31 (p < 0.01); serum phosphorus r = +0.28 (p = 0.02); PTH r = −0.4 (p < 0.01); alkaline phosphatase r = −0.0009 (p = NS); urine calcium excretion r = −0.002 (p = NS); urine phosphorus excretion r = −0.16 (p = NS). NS denotes ‘not statistically significant’ for p-values > 0.05
Monotonic relationships between plasma 25(OH)D status and calcium, phosphorus, and bone health markers at term age. Spearman correlation coefficients (r) and associated p-value for 25(OH)D and specific factors were serum calcium r = +0.0005 (p = NS); serum phosphorus r = −0.25 (p = NS); PTH r = −0.41 (p = 0.003); alkaline phosphatase r = −0.39 (p = 0.006); urine calcium excretion r = +0.36 (p = 0.005); urine phosphorus excretion r = −0.38 (p = 0.004); lumbar spine BMC r = −0.2 (p = NS); lumbar spine BMD r = +0.12 (p = NS); femur BMC r = +0.29 (p = 0.01); femur BMD r = +0.26 (p = 0.02). NS denotes ‘not statistically significant’ for p-values > 0.05
Piecewise regression models for estimating a threshold of 25(OH)D for the various indicators—PTH, femur BMC, and femur BMD—measured at term age produced the results along with 95% CI shown in Table 2. The slope describing the strength of association (with 95% CI) preceding the threshold are also shown in Table 2. For 25(OH)D status and PTH, PTH decreased as 25(OH)D increased until the PTH plateaued when 25(OH)D reached 42.9 (95% CI 32.2, 53.6) ng/mL. Similar thresholds are shown for femur BMC and BMD, but for these indicators, the slope before the threshold is slightly positive demonstrating an increase in femur BMC and BMD until a threshold of 25(OH)D at which point femur BMC and BMD measurements plateau. With respect to the slope line before the threshold, PTH was shown to decrease by 1.4 pg/mL for every increase in 1 ng/mL of 25(OH)D. The increase in femur BMC and BMD before the thresholds is small with 0.02 g and 0.0008 g/m2 increase respectively for every 1 ng/mL increase in 25(OH)D.
Discussion
In this study, as vitamin D status improved from birth to term age, PTH concentrations fell with a significant inverse correlation between 25(OH)D and PTH at one-month postnatal age and term age. This inverse correlation is similar to that found in adults, children, and in late preterm infants through the first three postnatal months [8,9,10,11]. The piecewise linear regression performed at term age demonstrated an inverse linear association between 25(OH)D and PTH until a threshold of 25(OH)D status of 42 (95% CI 32.3, 53.6) ng/mL where PTH plateaued. Due to the tight control of calcium by PTH, PTH often serves as an indicator of body calcium balance. If body calcium is adequate, then PTH expression is muted. When circulating calcium falls below a threshold, the parathyroid gland secretes PTH to activate intestinal calcium absorption, renal calcium reabsorption, and demineralization of bone to increase circulating calcium [2, 12]. Of note, because calcium and phosphorus are reabsorbed from bone proportionally, PTH also leads to phosphorus removal from bone but then increases renal excretion of phosphorus to avoid hyperphosphatemia. Urinary phosphorus excretion was negatively associated with 25(OH)D at term age, which may reflect a decrease in the PTH signaling of urinary phosphorus excretion with increased 25(OH)D.
In regards to bone health, femur BMC and BMD were significantly associated with vitamin D status. A threshold of vitamin D status demonstrating the concentration above which bone mineralization no longer increased was identified for both content and density [48.2 (95% CI 35.4, 61) ng/mL and 46.6 (95% CI 33.4, 59.7) ng/mL, respectively], but the change in slope was minimal and the confidence intervals fairly wide. Unlike the femur, lumbar spine mineralization did not demonstrate a significant association with vitamin D status. The difference between femur and lumbar spine mineralization in association with vitamin D status may reflect a difference in the role of vitamin D for mineralization of cortical versus trabecular bone. Vitamin D status in children is more commonly associated with differences in cortical bone (radial or femoral) mineralization [13, 14]. Studies performed in preterm infants with sensitive techniques, such as DEXA scan or qualitative CT scan are limited. Backstrom et al compared bone mineralization by DEXA scan for infants receiving either 200 IU/kg body weight up to 400 IU/day or a dose of 960 IU/day vitamin D and found no significant difference in forearm BMC or BMD with comparison groups achieving 25(OH)D status of 32 and 45 ng/mL, respectively [6].
This study is the first to show an association between 25(OH)D status and preterm infant femur bone mineralization. It is also the first study to identify a 25(OH)D threshold for PTH equilibrium. The results of the current study are not conclusive but, instead, identify a path for further study into the preterm infant vitamin D status. Of note, the piecewise linear regression model allows adjustment for confounding variables which can be quite numerous in preterm infant clinical study. Further study should prepare for these adjustments. In addition, the 25(OH)D radioimmunoassay used did not measure 25(OH)D epimers. Vitamin D metabolite epimers historically were considered to be inert, but recent data demonstrates that they may have some amount of bioactivity and are present in preterm infant blood [15, 16]. Therefore, further investigation of vitamin D function may require measurement of epimers to be included in the equations.
This study is limited to the nutritional and clinical practices of one institution. Since nutritional intervention of calcium, phosphorus, and vitamin D are inter-related, improvements in vitamin D delivery are associated with improvements in calcium and phosphorus delivery. This complementary increase in delivery complicates identification of causality. This comprehensive assessment of preterm infants from birth to term age is a foundation for evaluation including methods of vitamin D supplementation to ensure calcium and phosphorus homeostasis with optimal bone mineralization. Validation studies are required, as well as further exploration of the complex role of vitamin D in calcium, phosphorus, and bone in the growing, developing preterm infant.
References
Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–52.
Pludowski P, Holick MF, Pilz S, Wagner CL, Hollis BW, Grant WB, et al. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-a review of recent evidence. Autoimmun Rev. 2013;12:976–89.
Salle BL, David L, Glorieux FH, Delvin E, Senterre J, Renaud H. Early oral administration of vitamin D and its metabolites in premature neonates. Effect on mineral homeostasis. Pediatr Res. 1982;16:75–8.
Koo WW, Krug-Wispe S, Neylan M, Succop P, Oestreich AE, Tsang RC. Effect of three levels of vitamin D intake in preterm infants receiving high mineral-containing milk. J Pediatr Gastroenterol Nutr. 1995;21:182–9.
Natarajan CK, Sankar MJ, Agarwal R, Pratap OT, Jain V, Gupta N, et al. Trial of daily vitamin D supplementation in preterm infants. Pediatrics. 2014;133:e628–34.
Backstrom MC, Maki R, Kuusela AL, Sievanen H, Koivisto AM, Ikonen RS, et al. Randomised controlled trial of vitamin D supplementation on bone density and biochemical indices in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1999;80:F161–6.
Fenton TR. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003;3:13.
Harkness L, Cromer B. Low levels of 25-hydroxy vitamin D are associated with elevated parathyroid hormone in healthy adolescent females. Osteoporos Int. 2005;16:109–13.
Chapuy MC, Schott AM, Garnero P, Hans D, Delmas PD, Meunier PJ. Healthy elderly French women living at home have secondary hyperparathyroidism and high bone turnover in winter. EPIDOS Study Group. J Clin Endocrinol Metab. 1996;81:1129–33.
Giapros VI, Schiza V, Challa AS, Cholevas VK, Theocharis PD, Kolios G, et al. Vitamin D and parathormone levels of late-preterm formula fed infants during the first year of life. Eur J Clin Nutr. 2012;66:224–30.
Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, et al. Prevalence of vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90:3215–24.
Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R, Kifor O, et al. Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Nature. 1993;366:575–80.
Zamora SA, Rizzoli R, Belli DC, Slosman DO, Bonjour JP. Vitamin D supplementation during infancy is associated with higher bone mineral mass in prepubertal girls. J Clin Endocrinol Metab. 1999;84:4541–4.
Rigo J, Pieltain C, Salle B, Senterre J. Enteral calcium, phosphate and vitamin D requirements and bone mineralization in preterm infants. Acta Paediatr. 2007;96:969–74.
Hanson C, Jones G, Lyden E, Kaufmann M, Armas L, Anderson-Berry A. Vitamin D metabolism in the premature newborn: a randomized trial. Clin Nutr. 2016;35:835–41.
Aghajafari F, Field CJ, Rabi D, Kaplan BJ, Maggiore JA, O’Beirne M. et al. Plasma 3-Epi-25-Hydroxycholecalciferol can alter the assessment of vitamin D status using the current reference ranges for pregnant women and their newborns. J Nutr. 2016;146:70–5.
Funding
NIH/NCRR (K23 RR021891) and National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant (UL1TR001450).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Taylor, S.N., Wahlquist, A., Wagner, C.L. et al. Functional indicators of vitamin D adequacy for very low birth weight infants. J Perinatol 38, 550–556 (2018). https://doi.org/10.1038/s41372-018-0098-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0098-7
- Springer Nature America, Inc.