Abstract
Respirator face masks (RFMs) as a personal-level intervention is increasingly being utilized to reduce ambient particulate matter (PM) exposure, globally. We tested the effectiveness of 50 commercially available ones in reducing the exposure of ambient particle number concentrations (PNC), PM10, PM2.5, and PM1 (PM ≤ 10, 2.5, and 1 μm in diameter, respectively) in a traffic-affected urban site in Tehran. To examine the efficiency of RFMs, we applied a specific experimental setup including vacuum pumps, dummy heads, connecting tubes, glass chambers, and GRIMM Aerosol Spectrometer to measure all metrics after dummy heads. The average effectiveness of RFMs was in the range of 0.7–83.5%, 3.5–68.1%, 0.8–46.1%, and 0.4–32.2% in reducing ambient PNC, PM10, PM2.5, and PM1, respectively. Considering all metrics, the highest effectiveness was observed always for Biomask, followed by 3 M 9332, due to their well-designed physical characteristics (e.g., adjustable nose clip for any face/nose shape, and size, soft inner material in the nose panel to provide a secure seal against leakage, adjustable or elasticated straps/ear loops to better adjust on any face). Biomask reduced ambient PM10 with a mean value of 94.6 μg m−3 (minimum–maximum: 51.7–100.3 μg m−3), whereas it filtered on average just 29.0 μg m−3 (25.7–43.5 μg m−3) of ambient PM2.5 and 18.2 μg m−3 (14.7–21.8 μg m−3) of PM1. A fuzzy analytical hierarchy process to find the most important design-related factors of RFMs affecting their effectiveness, which showed the exhalation valve and its diaphragm (20.4%), nose clip (19.7%), and cheek flaps (18.6%) are ranked as the main design-related variables. The fuzzy technique for order preference by similarity to ideal solution indicated that Biomask and 3M 9332 had scores of 1 and 0.97, the highest scores compared with other RFMs. This study provides crucial evidence-based results to elucidate the effectiveness and design-related factors of RFMs in real-environmental circumstances.
Similar content being viewed by others
Introduction
More than 3 million of cardiovascular (CV) disease deaths were attributed to traffic-related PM2.5 exposure in 2016, globally [1,2,3,4,5,6]. The majority of premature deaths from exposure to PM2.5, as the most notable marker of ambient air pollution, have occurred in developing countries [3, 4, 7,8,9,10,11,12]. Given this sobering reality, there are two main approaches to reduce chronic and acute exposures to this global leading risk factor; ambient PM; firstly implementing population-level interventions such as shifting to clean fuels, transportation reform, reduce traffic emission(s), and secondly using personal-level interventions such as respirator FMs (RFMs) and air purifiers [3, 5, 13,14,15,16,17,18,19,20,21,22,23,24]. Wearing RFMs has been increasingly becoming as one of the most common individual-level interventions to protect against ambient PM exposure because it is impossible to implement population-level interventions in a short-time or even long-time, especially in highly polluted megacities of developing countries [1, 3, 17, 19, 25,26,27,28,29,30,31,32,33]. We reported that the annual concentrations of ambient PM2.5 far exceeding the World Health Organization Air Quality Guideline (10 μg m−3), U.S. EPA and national standard levels (12 μg m−3) during the period 2006–2017 [34,35,36,37]. Extreme air pollution episodes, particularly in the autumn and winter months, are becoming all too routine in Tehran [34, 38]. During this period, it is common to see people wearing various commercial brands of RFMs in outdoor to protect themselves against ambient PM exposure.
RFMs are used in occupational and non-occupational settings [20, 32, 39]. For occupational settings, the use of professional RFMs is supported by legal enforcement, and their manufacturers/producers are required to meet the national and international standards/guidelines (e.g., 42 CFR 84 in the US or EN 149:2001+A1:2009 in the EU) [19, 21, 40, 41]. Commercially available RFMs, used by people are not mainly supported by the national and international regulations compared with professional ones. Therefore, their producers mostly follow market laws related to the trends of fashion rather than human health [19, 32, 42]. Consequently, people particularly in developing countries wear mainly the non-certified commercial RFMs [42]. Given the aforementioned concerns, the stricter inspections are being recommended to produce, distribute, and sell the commercially available RFMs in developing countries [19,20,21]. To date, numerous studies have been published on the investigation of RFMs’ effectiveness against particles/aerosols [17, 19,20,21, 27, 29, 32, 40, 43,44,45,46,47,48]. Nevertheless, largely all investigations, with the exception of two studies [32, 44], have investigated their effectiveness under laboratory conditions against lab-generated and non-exhaust particles, including sodium chloride [17,18,19, 21, 43, 45, 46, 48, 49], dioctyl phthalate [17], biological aerosols [47, 50, 51], polystyrene latex [17, 46], aluminum oxide and volcano ash [20, 21], titanium dioxide, iron oxides, and silicon dioxide [28, 49], yellow dust [20, 21], and paraffin oil [40]. Since nearly all individuals in urban areas of developing countries are exposed to high levels of traffic-derived PM in the various size fractions [1, 11], which its physiochemical and toxicological properties are greatly differ from lab-generated and non-exhaust particles [52]. As such, addressing the following question is extremely urgent [17, 32, 44, 53]. How much is the effectiveness of commercially available RFMs against ambient PM under real-environmental conditions [17, 32, 44]?
In this challenging context, we conducted this study to investigate the effectiveness of (1) 50 RFMs based on ambient PNC in a traffic-affected urban site in Tehran; (2) all RFMs against ambient PM10, PM2.5, and PM1 (PMX) mass concentrations; (3) the most effective RFMs against above-mentioned metrics over the time (about 6 h); (4) the most effective RFM (one out of 50 RFMs) in terms of ambient PNC and PM mass concentrations in twenty-three various size fractions from 0.25–10 μm; and (5) the effect of the design-related factors of RFMs on their effectiveness using two-step methodology (the fuzzy analytical hierarchy process (AHP) and technique for order preference by similarity to ideal solution (TOPSIS)).
Materials and methods
Identification of RFMs
We assessed the effectiveness of 50 various commercial brands of RFMs (Fig. S1 from Supplementary material) against ambient PNC and PMX mass concentrations under a real-environmental condition. To identify a variety of utilized RFMs by Tehran citizens, we selected 225 pharmacies across different districts of Tehran megacity, mainly densely populated and highly polluted areas (Fig. S2) [35, 37, 54], and identified 40 various commercial brands. Moreover, we examined 27 medical equipment and supplies in Tehran, as well as a national e-commerce company in Iran (www.digikala.com), and then identified eight other ones. We also investigated the effectiveness of two international RFMs; namely 3M™ AuraTM 9332+ Disposable Face Mask, FFP3, Valved (3M 9332), and 3M™ Particulate Respirator 8210V, N95 (3M 8210V); purchased from an e-commerce website (www.amazon.com).
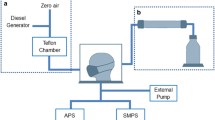
Experimental setup to evaluate the effectiveness of RFMs
A specific experimental setup was developed to monitor ambient PNC and PMX mass concentrations after dummy heads with and without RFMs (Fig. S3). The setup consists of two dummy heads (a) similar to adult human’s head which were connected to the vacuum pumps (b) (SPARMAX TC-501-V, Taiwan) through anti-electrostatic connecting tubes (c), with a flow rate equal to 16 L min−1. The outdoor air was pumped into two glass chambers (d) (90 (length) × 30 (width) × 30 (height) cm) and two internal baffles were used inside the chambers in order to better distribution of the air flow. Two real-time instruments (e) (GRIMM Aerosol Spectrometer, model 1.108 and 11E, Grimm Aerosol Technik GmbH, Ainring, Germany) were used to monitor the ambient PNC and PMX mass concentrations after dummy heads (with and without the RFMs) at a flow rate of 1.2 L min−1 [55,56,57]. The experimental setup was located on the balcony (<3 m above the ground) of the Exceptional Talents Development Center at Tehran University of Medical Sciences.
Instrumentation
Prior to each sampling campaign, two real-time devices and the experimental setup were run in parallel and ambient PNC measured by two portable instruments to normalize data across instruments, minimizing any possible measuring differences [32]. For this goal, both dummy heads were not wearing any RFM over the first 30-min of a 60-min test. As shown in Fig. S4, a high correlation was observed between two instruments with an R2 value of 0.98 and a slope of 0.94. Table S1 (from Supplementary material) illustrates the correction factors (on average 0.96) used for effectiveness-related test of RFMs and their R2 (0.86) based on ambient PNC. Furthermore, a simple linear regression was used to compare 24-hourly averaged ambient PM10 and PM2.5 measured by the portable instruments with the 24-hourly filter samples measured using Tisch Environmental high-volume air samplers to modify ambient PM10 and PM2.5 mass concentration data measured by the portable instruments [56]. There were high correlations between real-time instruments and high-volume air samplers’ data, with an R2 value of 0.92 and 0.94 for ambient PM10 and 0.90 and 0.93 for ambient PM2.5 (Figs. S5 and S6). Since the lack of PM1 high-volume air sampler, we corrected ambient PM1 mass concentration data from the real-time instruments based on our previous studies in Tehran [56, 58, 59].
Evaluating the effectiveness of RFMs
A total of 108 effectiveness-related tests of RFMs were conducted: 54 tests were conducted for evaluating the effectiveness of RFMs against ambient PNC, whereas the rest of tests were carried out for PMX mass concentrations. All tests were conducted during the autumn and winter months based on the Iranian calendar (from December 15, 2018 to March 10, 2019). The effectiveness-related test of each of RFMs lasted 60 min in time intervals of 1-min. To evaluate the effectiveness of RFMs, over the first 30 min, both dummy heads were not worn any RFM, and then the selected RFM was worn on the face of one of dummy head during the second 30-min. In fact, to assess the efficiency of each RFM, we had 30 1-min records for before and 30 1-min records after RFM. To evaluate the effectiveness of the most efficient RFMs (3 out of 50 ones) against all experimental metrics under investigation, we evaluated their effectiveness during ~6 h (380 min); 40 min for inter-comparing and correcting data measured by two real-time instruments and 340 min for evaluating their effectiveness in time intervals of 1-min. The effectiveness of the most effective RFM against ambient PM size fractions was determined during seven consecutive 30-min test of wearing and removing/doffing RFM using the glass chamber with GRIMM model 11E. We considered the average of all PM data throughout the period of wearing and removing/doffing RFMs as PM after and before them, respectively. To better avoid face-seal leakage and simulate the real situation, we attempted that RFMs were fitted well on dummy head according to the standard fitting instruction of one of 3M RFMs (https://multimedia.3m.com/mws/media/1546533O/3m-aura-9300plusgen3-technical-data-sheet-english-uk.pdf). We used a flow rate equivalent to 16 L min−1 and 11 L min−1 to simulate adults and children inhalation rates. The applied air flow rates were considered based on the 95th percentile inhalation rate recommended by EPA’s Exposure Factors Handbook for adults and children aged 21-<61 and 6-<11 years old, respectively [60, 61]. Air flow was regularly checked before and after each performance-related test of RFMs using rotameter (3–30 L min−1, SKC company) (Fig. S7). The effectiveness of RFMs was calculated as following [32]:
Quantifying the effect of the design-related factors of RFMs on their effectiveness
The fuzzy AHP and TOPSIS were used to quantify the effect of the design-related factors of RFMs on their effectiveness and to rank RFMs based on their scores, respectively [62, 63]. We conducted the levels of two-step methodology exactly similar to the previously conducted studies (Fig. 1) [62,63,64] and eight criteria were considered (Table S2) as the most important factors affecting the efficiency of RFMs. These factors include exhalation valve and its diaphragm, nose clip, chin tab, cheek flap, soft inner material in the nose panel or bridge, adjustable or elasticated straps/ear loops, how to connect the straps/ear loops with the body of RFM and how to design of the RFM edges. Linguistic scales and their numbers for the rating of each design-related factor were presented in Table S3. Data on weighting sector criteria of RFMs were collected using a weighting form according to point of view of five scientific experts on environmental health/epidemiology (Table S2). Finally, we computed a score for each of RFMs and then, the correlation between the score of RFMs and their effectiveness against PNC as well as PMX was investigated using the Pearson correlation.
Results
Effectiveness of RFMs
Figure 2 compares the average effectiveness of RFMs against ambient PNC (a), PM10 (b), PM2.5 (c), and PM1 (d) mass concentrations. Figure 2a and Table S4 reveal that the average effectiveness of all RFMs, with the exception of K300, 3M 9332, and Biomask, was lower than 50% in terms of ambient PNC. For ambient PNC, the average effectiveness of RFMs ranged from 0.73 to 83.5%. Moreover, the highest effectiveness for ambient PNC was found for K300, 3M 9332, and Biomask with a mean value of 67.6%, 71.1% and 83.5%, respectively. The effectiveness of children’s RFM in the matter of PNC ranged from 36.95% to 42.03%, with a mean value of 40.42%.
With reference to ambient PM10, PM2.5, and PM1 mass concentrations, the average effectiveness of RFMs was in the range of 3.5–68.1%, 0.8–46.1% and 0.4–32.2%, respectively (Fig. 2b–d and Tables S5–S7). Except for Biomask, the average effectiveness of all RFMs against ambient PM10, PM2.5, and PM1 was lower than 50%, 45% and 30%, respectively. Regarding PM10, the highest effectiveness was found for Biomask with values in the range of 64.9–71.6% and average equal to 68.1%, followed by 3M 9332 with the effectiveness in the range of 40.7–49.9% and average equal to 46.2%. Furthermore, during 30-min effectiveness-related tests for Biomask, ambient PM10 was in the range of 124.0–154.8 μg m−3, with a mean value of ~139.0 μg m−3, whereas ambient PM10 after Biomask (unfiltered PM10) ranged from 41.2 to 51.7 μg m−3, with a mean value of 44.3 μg m−3. In fact, Biomask reduced ambient PM10 in the range of 51.7–100.3 μg m−3, with a mean value of 94.6 μg m−3. The results of children’s RFM showed that the effectiveness in terms of PM10 was between 15.3 and 23.0%, with a mean value of 19.4%. On the other word, children’s RFM decreased ambient PM10 between 10.7 and 16.9 μg m−3, with a mean of 13.8 μg m−3. Detailed information regarding all RFMs’ effectiveness-related tests for ambient PM10 is presented in the Fig. 2b and Table S5.
Similar two previous metrics mentioned above; ambient PNC and PM10; the highest effectiveness in terms of ambient PM2.5 and PM1 was observed for Biomask with the average effectiveness equal to 46.1% (43.5–50.6%) and 32.2% (28.7–35.4%), followed by 3M 9332 with the average effectiveness equal to 38.0% (34.4–41.6%) and 24.0% (22.1–25.8%) (Fig. 2c, d). In terms of ambient mass concentrations, the average concentrations of ambient PM2.5 before and after Biomask were 62.9 μg m−3 (58.8–67.1 μg m−3) and 33.9 μg m−3 (32.6–36.8 μg m−3) (Table S6), while ambient PM1 before and after Biomask ranged from 51.1 to 62.1 μg m−3 and 36.3 to 41.8 μg m−3, with the mean value of 56.2 and 38.0 μg m−3 (Table S7). Besides, Biomask filtered just on average 29.0 μg m−3 (25.7–43.5 μg m−3) of ambient PM2.5 and 18.2 μg m−3 (14.7–21.8 μg m−3) of PM1. As can be seen from Fig. 2c, d, Tables S6 and S7, the children’s RFM exhibited an average effectiveness of 9.5 and 7.1% in the range of 7.6–11.4 and 6.1–7.9% in terms of ambient PM2.5 and PM1. Descriptive statistics of ambient PM2.5 and PM1 before and after RFMs, as well as ambient PM2.5 and PM1 reduced by all RFMs and their effectiveness are shown in Tables S6 and S7 in detail.
Temporal variability of effectiveness of the most effective RFMs
The top three of RFMs with the highest effectiveness in terms of ambient PNC was selected to see the temporal variation of their effectiveness (Biomask, 3M 9332 and K300) against all experimental metrics for ~6 h. For instance, Fig. 3 illustrates the effectiveness of Biomask against ambient PNC (Fig. 3a) and PMX mass concentrations over the time (Fig. 3b–d). In addition, Fig. S8 indicates the effectiveness of other RFMs (3M 9332 and K300) against preceding metrics over the time. At the beginning of the effectiveness-related tests during the first 40-min, with both dummy heads without RFMs, we observed a similar trend for all metrics under investigation (Figs. 3 and S8). However, ambient PNC and PMX mass concentrations decreased immediately after wearing RFMs. For ambient PNC, the effectiveness of Biomask, 3M 9332 and K300 showed a fluctuating trend in the range of 78.5–83.4%, 71.6–78.3%, and 62.4–70.2% during a 340-min investigation, respectively. Regarding ambient PM2.5 and PM1, their effectiveness was always <50% and 40%. Furthermore, the effectiveness of 3M 9332 and K300 in terms of ambient PM10 was in the range of 37.1–57.7% and 36.5–54.9%, respectively. We observed an interesting results regarding the effectiveness of Biomask against ambient PMX mass concentrations (Fig. 3b-d) compared with other RFMs. The effectiveness of Biomask that was in the range of 29.0–64.1% revealed a considerable rising together with the increase of ambient PMX mass concentrations, possibly related to higher contribution of larger-sized particles in the increase of ambient PMX compared with the smaller-sized particles. The significant increase of ambient PM10 was mainly related to the larger-sized fraction of PM10; PM10–2.5 (PM with an aerodynamic diameter between 2.5 and 10 μm); compared with another fraction; PM2.5 (Fig. S9a). In addition, PM2.5 was mainly made up of submicron particles; PM1; when the ambient PM2.5 remarkably increased 70 min after the start of investigating the effectiveness of Biomask; approximately at 110th minute (Fig. S9b). Besides, unfiltered PM10, PM2.5, and PM1 by Biomask had approximately a steady trend in the range of 37.0–46.0, 32.0–35.0, and 27.0–29.0 μg m−3 during a 340-min investigation. On the other hand, these concentrations that not filtered by Biomask are more likely related to the smaller-sized fractions of particles (Fig. S9a, b).
Effectiveness of the most effective RFM against ambient PM size fractions
Figure 4 illustrates the effectiveness of Biomask against 23 ambient PM size fractions between 0.25 and 10 μm. The effectiveness of Biomask in terms of various size fractions of ambient PNC and PM mass concentrations gradually increases with rising size fractions of ambient PM. This size-dependent effectiveness may be due to the larger-sized particles being more likely to capture/deposit by particle collection processes such as electrostatic attraction, impaction, and interception as compared with the submicron particles [17]. Regarding ambient PNC, the effectiveness of Biomask ranged from 78.82% (0.25–0.28 μm, PM0.25–0.28) to 92.75% (8.5–10.0 μm, PM8.5–10), while its effectiveness in terms of ambient PM mass concentrations in various size fractions was in the range of 34.0% (for PM0.25–0.28)–80.1% (for PM8.5–10). Tables S8 and S9 report detailed information on ambient PNC and PM mass concentrations in various size fractions before and after Biomask, as well as the amount of ambient PNC and PM mass concentrations filtered by Biomask.
The effect of design-related factors of RFMs on their effectiveness
We also quantified the effect of eight design-related factors of RFMs on their effectiveness based on the fuzzy AHP method and ranked the RFMs using the fuzzy TOPSIS approach (Figs. 5 and S10). The priority of the design-related factors of RFMs followed in the order of exhalation valve and its diaphragm (20.4%) > nose clip (19.7%) > cheek flaps (18.6%) > soft inner material in the nose panel or bridge (16.9%) > chin tab (14.8%) > how to design of the RFM edges (4.7%) > adjustable or elasticated straps/ear loops (2.4%) > how to connect the straps/ear loops with the body of RFM (2.4%). In addition, Fig. 6 shows the scatter-matrix, histogram, and Pearson rank correlation-matrix for the score of RFMs and their effectiveness against PNC, PM10, PM2.5, and PM1. Interestingly, there were the high statistically significant correlations between the score of RFMs and their effectiveness against PNC (Pearson’s correlation = 0.8), PM10 (0.7), PM2.5 (0.8), and PM1 (0.7). Detailed information on the score of all RFMs is presented in Fig. S10.
Discussion
Among all RFMs under investigation, the average effectiveness of three of RFMs, namely K300, 3M 9332, and Biomask, in terms of ambient PNC was more than 65%, and Biomask with an average effectiveness of 83.5% was the RFM with the highest effectiveness. Compared with other RFMs, Biomask had the highest effectiveness to decrease ambient PMX mass concentrations and reduced on average 94.6 μg m−3 (51.7–100.3 μg m−3), 29.0 μg m−3 (25.7–43.5 μg m−3), and 18.2 μg m−3 (14.7–21.8 μg m−3) of ambient PM10, PM2.5, and PM1, respectively. Because of the paucity of studies regarding evaluating the effectiveness of commercial RFMs against ambient PM under real-environmental conditions, we only compared our results with two studies [32, 44]. It should be highlighted that our study is differ with the mentioned studies in several parameters such as applied flow rate, investigated metrics and their concentrations, as well as type of RFMs. A study conducted by Pacitto et al. [32] demonstrated that the effectiveness of nine RFMs in terms of ambient PM2.5 under three breathing rates was in the range of 14–96%, whereas the effectiveness of our RFMs against PM2.5 was in the range of 0.8–46.1%. Furthermore, they indicated that the price of RFMs was not an indicator of their effectiveness, because the RFM with the best performance in terms of all metrics under investigation was not more expensive and the one with the lowest effectiveness was not the cheapest RFM [32]. Similar to the study of Pacitto et al. [32], no cost-effectiveness relationship was observed in our study because Biomask as the most effective RFM was cheaper compared with nearly all RFMs. Guan et al. [44] evaluated the effectiveness of six types of RFMs in terms of ambient PM size fraction of 5.6–560 nm in diameter and the effectiveness of them was in the range of 48–75% [44].
The effectiveness of RFMs is affected by multiple factors: almost importantly, the design-related factors of RFMs (adjustable nose clip/ear loops/straps to adjust RFMs based on the physical characteristics of wearers’ nose, head, and face; proper design of exhalation valve and its diaphragm, extendable chin tab and cheek flaps; proper connection of ear loops/straps with the body of RFM; type of materials used in all parts of them; the configuration and size of them; number of layers applied; thickness and pore size of layers); the second affected is the wearers-related factors such as the style of wearing/donning of RFM, the wearer facial characteristics, the type of wearer's activity, the pattern of inhalation flow rate and time-term use of RFM; finally, the environmental-related factors such as the mass and number concentrations of various size fractions of PM [17, 19,20,21, 32, 41, 46, 65]. Hereunder, we discussed on the main reasons for low effectiveness of nearly all RFMs under investigation in the present study, as well as for higher effectiveness of Biomask and 3M 9332 as compared with other RFMs in detail.
In this field study, we observed and experienced the weak design-related factors of RFMs that may be significantly reduced the effectiveness of them against ambient PM. As illustrated in Fig. S11 (detailed information regarding the weak design of various parts of RFMs), low effectiveness of nearly all RFMs may be due to: (1) the weak design of exhalation valve and its diaphragm; (2) the lack/weak design of soft inner material in the nose panel or bridge to provide a secure seal against leakage; (3) the application of unsuitable material in the external part of nose panel or bridge; (4) the weak design of RFMs’ edges; (5) non-adjustable or non-elasticated straps/ear loops; (6) the lack/weak design of chin tab and cheek flaps; and (7) improper connection of straps/ear loops with the body of RFMs that leads to not secure seal against leakage. We computed the importance weights of the above-mentioned criteria and ranked them using the fuzzy AHP approach. Regarding the weights representing the importance of the criteria, the highest weight was estimated for exhalation valve and its diaphragm (20.4%), followed by nose clip (19.7%), cheek flaps (18.6%), soft inner material in the nose panel or bridge (16.9%), and chin tab (14.8%), whereas the lowest weights were observed for how to connect the straps/ear loops with the body of RFMs (2.4%), adjustable or elasticated straps/ear loops (2.4%), and how to design of the RFM edges (4.7%).
Compared with other RFMs, higher effectiveness of Biomask and 3M 9332 might be attributed to the combination of different well-designed physical characteristics of these RFMs (Fig. S12) including adjustable nose clip that make it adaptable for any face or nose shape and size, cheek flaps, and chin tab, soft inner material in the nose panel or bridge to provide a secure seal against leakage, well-constructed exhalation valve and its diaphragm, elasticated or adjustable straps/ear loops. These well-designed characteristics lead to decrease ambient PM leakage because of adequate face-fit of them compared with other RFMs. Considering the results of ranking of RFMs using the fuzzy AHP-TOPSIS method, Biomask with the score of 1 had the highest rank, followed by 3M 9332 with the score of ~0.97. Though these RFMs were much better in comparison to others, none of them were significantly able to reduce ambient PM2.5 and PM1, more likely due to type of material used in filters, number of layers applied, thickness, and pore size of layers. Fig. S12f shows three different filter layers of Biomask as the most effective RFM in terms of all metrics under investigation in this study.
Collectively, our study clearly revealed that the effectiveness of RFMs was significantly less than the values mentioned and claimed by their manufacturers and sellers. We observed that RFMs throughout national market in Tehran were non-certified because there was no regulation on the certification of the RFMs in our country. Given the results of this study, we hope the appropriate guidelines/regulations will be introduced after our study and convince national agencies to put stricter inspection on the producers, importers, sellers, and distributors of RFMs.
Strengths and limitations
The strength of our study is that we tested the effectiveness of large number of RFMs from national and international market using PM air pollution in real-world condition. Our study can inform consumers and stakeholders on the most common personal-intervention product in developing countries against ambient PM air pollution. However, the experimental setup used to investigate the effectiveness of RFMs has several limitations. Importantly, it considered breathing only as inhalation of ambient air without the exhalation part. Because a positive pressure is generated during exhalation, the face-fit of RFMs might be compromised and unfiltered ambient PM could enter in the breathing zone, this is particularly true for RFMs without exhalation valve and RFMs with the weak design of exhalation valve and its diaphragm. Therefore, an overestimation of the measured effectiveness might have occurred [32]. In addition, Mahdavi et al. indicated that the differences between the penetration values, as a function of effectiveness, for “inhalation-only” setup and “inhalation-and-exhalation” setup were not statistically significant [66]. Flow rate used may not be representative of actual human breath rate within different situations (deep breathing, light exercise, etc.), though Pacitto et al. stated that no clear relationship between the change in breathing rate (32, 42, and 52 L min−1) and the effectiveness of RFMs was observed [32]. Finally, the dummy head is not similar to human face tissue affecting face-fit of RFMs and underestimation of the measured effectiveness might have occurred.
Conclusion
To the best of our knowledge, the present study is a comprehensive field and practical survey of the effectiveness of RFMs used by Tehran citizens against ambient traffic-related PM which provides notable scientific results. In terms of ambient PNC, PM10, PM2.5, and PM1, Biomask had the highest effectiveness compared with others. Compared with more RFMs under study, Biomask as the most effective RFM was cheaper. Therefore, no cost-effectiveness relationship was observed for RFMs in the present study. Given the wide range of effectiveness obtained, it is clear that consumers more attention must be given to the choice of the most effective RFM based on its design characteristics. In reality, our results indicated that prior to buying and using the RFMs, the consumers of these individual-level intervention products have to consider the design-related factors of RFMs, particularly exhalation valve and its diaphragm, nose clip, cheek flaps, soft inner material in the nose panel or bridge. In addition, it is recommended to the producers of these products that to be focus more on design-related factors discussed earlier in detail and also present the standard fitting instruction and fit-checking procedure.
References
Brook RD, Newby DE, Rajagopalan S. The global threat of outdoor ambient air pollution to cardiovascular health: time for intervention. JAMA Cardiol. 2017;2:353–4.
Lelieveld J, Evans JS, Fnais M, Giannadaki D, Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367.
Hadley MB, Vedanthan R, Fuster V. Air pollution and cardiovascular disease: a window of opportunity. Nat Rev Cardiol. 2018;15:193.
Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA, et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci USA. 2018;115:9592–7.
Rajagopalan S, Al-Kindi SG, Brook RD. Air pollution and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2054–70.
Hadley MB, Baumgartner J, Vedanthan R. Developing a clinical approach to air pollution and cardiovascular health. Circulation. 2018;137:725–42.
Landrigan PJ, Fuller R, Acosta NJ, Adeyi O, Arnold R, Baldé AB, et al. The Lancet Commission on pollution and health. Lancet. 2018;391:462–512.
Apte JS, Brauer M, Cohen AJ, Ezzati M, Pope III CA. Ambient PM2. 5 reduces global and regional life expectancy. Environ Sci Technol Lett. 2018;5:546–51.
Fantke P, McKone TE, Tainio M, Jolliet O, Apte JS, Stylianou K, et al. Global effect factors for exposure to fine particulate matter. Environ Sci Technol. 2019;53:6855–68.
West JJ, Cohen A, Dentener F, Brunekreef B, Zhu T, Armstrong B, et al. What we breathe impacts our health: improving understanding of the link between air pollution and health. Environ Sci Technol. 2016:50:4895–904.
Barzeghar V, Sarbakhsh P, Hassanvand MS, Faridi S, Gholampour A. Long-term trend of ambient air PM10, PM2.5, and O3 and their health effects in Tabriz city, Iran, during 2006–17. Sustain Cities Soc. 2020;54:101988.
Shamsipour M, Hassanvand MS, Gohari K, Yunesian M, Fotouhi A, Naddafi K, et al. National and sub-national exposure to ambient fine particulate matter (PM2. 5) and its attributable burden of disease in Iran from 1990 to 2016. Environ Pollut. 2019;255:113173.
Laumbach R, Meng Q, Kipen H. What can individuals do to reduce personal health risks from air pollution? J Thorac Dis. 2015;7:96.
Langrish JP, Li X, Wang S, Lee MM, Barnes GD, Miller MR, et al. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ Health Perspect. 2012;120:367.
Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, et al. Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation. 2017;136:618–27.
Zhang S, Li L, Gao W, Wang Y, Yao X. Interventions to reduce individual exposure of elderly individuals and children to haze: a review. J Thorac Dis. 2016;8:E62.
Shakya KM, Noyes A, Kallin R, Peltier RE. Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J Expo Sci Environ Epidemiol. 2017;27:352.
Peck R, Grinshpun S, Yermakov M, Rao M, Kim J, Reponen T. Efficiency of portable HEPA air purifiers against traffic related combustion particles. Build Environ. 2016;98:21–29.
Cherrie JW, Apsley A, Cowie H, Steinle S, Mueller W, Lin C, et al. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup Environ Med. 2018;75:446–52.
Steinle S, Sleeuwenhoek A, Mueller W, Horwell CJ, Apsley A, Davis A, et al. The effectiveness of respiratory protection worn by communities to protect from volcanic ash inhalation. Part II: Total inward leakage tests. Int J Hyg Environ Health. 2018;221:977–84.
Mueller W, Horwell CJ, Apsley A, Steinle S, McPherson S, Cherrie JW, et al. The effectiveness of respiratory protection worn by communities to protect from volcanic ash inhalation. Part I: Filtration efficiency tests. Int J Hyg Environ Health. 2018;221:967–76.
Chen R, Zhao A, Chen H, Zhao Z, Cai J, Wang C, et al. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: a randomized, double-blind crossover trial of air purifiers. J Am Coll Cardiol. 2015;65:2279–87.
Giles LV, Barn P, Künzli N, Romieu I, Mittleman MA, van Eeden S, et al. From good intentions to proven interventions: effectiveness of actions to reduce the health impacts of air pollution. Environ Health Perspect. 2010;119:29–36.
Morishita M, Adar SD, D’Souza J, Ziemba RA, Bard RL, Spino C, et al. Effect of portable air filtration systems on personal exposure to fine particulate matter and blood pressure among residents in a low-income senior facility: a randomized clinical trial. JAMA Intern Med. 2018;178:1350–7.
Barrett JR. Air pollution intervention: study links use of face masks to improved cardiovascular outcomes. Natl Inst Environ Health Sci. 2012;120:a122.
Langrish JP, Mills NL, Chan JK, Leseman DL, Aitken RJ, Fokkens PH, et al. Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol. 2009;6:8.
Zhang J, Mu Q. Air pollution and defensive expenditures: evidence from particulate-filtering facemasks. J Environ Econ Manag. 2017;92:517–36.
Shi J, Lin Z, Chen R, Wang C, Yang C, Cai J, et al. Cardiovascular benefits of wearing particulate-filtering respirators: a randomized crossover trial. Environ Health Perspect. 2016;125:175–80.
Patel D, Shibata T, Wilson J, Maidin A. Challenges in evaluating PM concentration levels, commuting exposure, and mask efficacy in reducing PM exposure in growing, urban communities in a developing country. Sci Total Environ. 2016;543:416–24.
van Dorn A. Clearing the air: do facemasks protect health? Lancet Respir Med. 2017;5:555–6.
Cheng Z, Luo L, Wang S, Wang Y, Sharma S, Shimadera H, et al. Status and characteristics of ambient PM2. 5 pollution in global megacities. Environ Int. 2016;89:212–21.
Pacitto A, Amato F, Salmatonidis A, Moreno T, Alastuey A, Reche C, et al. Effectiveness of commercial face masks to reduce personal PM exposure. Sci Total Environ. 2019;650:1582–90.
Morishita M, Wang L, Speth K, Zhou N, Bard RL, Li F, et al. Acute blood pressure and cardiovascular effects of near-roadway exposures with and without N95 respirators. Am J Hypertens. 2019;32:1054–65.
Faridi S, Shamsipour M, Krzyzanowski M, Künzli N, Amini H, Azimi F, et al. Long-term trends and health impact of PM 2.5 and O3 in Tehran, Iran, 2006–2015. Environ Int. 2018;114:37–49.
Faridi S, Niazi S, Yousefian F, Azimi F, Pasalari H, Momeniha F, et al. Spatial homogeneity and heterogeneity of ambient air pollutants in Tehran. Sci Total Environ. 2019;697:123–34.
Faridi S, Niazi S, Shamsipour M, Hassanvand MS. Comments on:” Meteorological correlates and AirQ+ health risk assessment of ambient fine particulate matter in Tehran, Iran”. Environ Res. 2019;174:122.
Bayat R, Ashrafi K, Motlagh MS, Hassanvand MS, Daroudi R, Fink G, et al. Health impact and related cost of ambient air pollution in Tehran. Environ Res. 2019;176:108547.
Yousefian F, Faridi S, Azimi F, Aghaei M, Shamsipour M, Yaghmaeian K, et al. Temporal variations of ambient air pollutants and meteorological influences on their concentrations in Tehran during 2012–2017. Sci Rep. 2020;10:1–11.
Huang W, Morawska L. Face masks could raise pollution risks. Nature. 2019;574:29–30.
Jung H, Kim J, Lee S, Lee J, Kim J, Tsai P, et al. Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual Res. 2014;14:991–1002.
Bard RL, Ijaz MK, Zhang JJ, Li Y, Bai C, Yang Y, et al. Interventions to reduce personal exposures to air pollution: a primer for health care providers. Glob heart. 2019;14:47.
Horwell C, Ferdiwijaya D, Wahyudi T, Dominelli L. Use of respiratory protection in Yogyakarta during the 2014 eruption of Kelud, Indonesia: community and agency perspectives. J Volcanol Geotherm Res. 2017;382:92–102.
Rengasamy S, Zhuang Z, Niezgoda G, Walbert G, Lawrence R, Boutin B, et al. A comparison of total inward leakage measured using sodium chloride (NaCl) and corn oil aerosol methods for air-purifying respirators. J Occup Environ Hyg. 2018;15:616–27.
Guan T, Hu S, Han Y, Wang R, Zhu Q, Hu Y, et al. The effects of facemasks on airway inflammation and endothelial dysfunction in healthy young adults: a double-blind, randomized, controlled crossover study. Part Fibre Toxicol. 2018;15:30.
Rengasamy S, Walbert GF, Newcomb WE, Faulkner K, Rengasamy MM, Brannen JJ, et al. Total inward leakage measurement of particulates for N95 filtering facepiece respirators—a comparison study. Ann Occup Hyg. 2013;58:206–16.
Rengasamy S, Eimer BC. Total inward leakage of nanoparticles through filtering facepiece respirators. Ann Occup Hyg. 2011;55:253–63.
Kelkar U, Gogate B, Kurpad S, Gogate P, Deshpande M. How effective are face masks in operation theatre? A time frame analysis and recommendations. Int J Infect Control 2013;9.
Shaffer RE, Rengasamy S. Respiratory protection against airborne nanoparticles: a review. J Nanopart Res. 2009;11:1661.
Kang M. Assessment of NIOSH-approved N95 filter performance against varying conditions. 2011. https://ir.uiowa.edu/etd/2722/.
Rengasamy S, Shaffer R, Williams B, Smit S. A comparison of facemask and respirator filtration test methods. J Occup Environ Hyg. 2017;14:92–103.
Lai A, Poon C, Cheung A. Effectiveness of facemasks to reduce exposure hazards for airborne infections among general populations. J R Soc Interface. 2011;9:938–48.
Li J, Chen H, Li X, Wang M, Zhang X, Cao J, et al. Differing toxicity of ambient particulate matter (PM) in global cities. Atmos Environ. 2019;212:305–15.
Amato F. Non-exhaust emissions: an urban air quality problem for public health; impact and mitigation measures. (Academic Press; 2018).
Yousefian F, Mahvi AH, Yunesian M, Hassanvand MS, Kashani H, Amini H. Long-term exposure to ambient air pollution and autism spectrum disorder in children: a case-control study in Tehran, Iran. Sci total Environ. 2018;643:1216–22.
Chen G, Morawska L, Zhang W, Li S, Cao W, Ren H, et al. Spatiotemporal variation of PM1 pollution in China. Atmos Environ. 2018;178:198–205.
Hassanvand MS, Naddafi K, Faridi S, Arhami M, Nabizadeh R, Sowlat MH, et al. Indoor/outdoor relationships of PM10, PM2. 5, and PM1 mass concentrations and their water-soluble ions in a retirement home and a school dormitory. Atmos Environ. 2014;82:375–82.
Meng X, Ma Y, Chen R, Zhou Z, Chen B, Kan H. Size-fractionated particle number concentrations and daily mortality in a Chinese city. Environ Health Perspect. 2013;121:1174–8.
Hassanvand MS, Naddafi K, Faridi S, Nabizadeh R, Sowlat MH, Momeniha F, et al. Characterization of PAHs and metals in indoor/outdoor PM10/PM2. 5/PM1 in a retirement home and a school dormitory. Sci Total Environ. 2015;527:100–10.
Hassanvand MS, Naddafi K, Kashani H, Faridi S, Kunzli N, Nabizadeh R, et al. Short-term effects of particle size fractions on circulating biomarkers of inflammation in a panel of elderly subjects and healthy young adults. Environ Pollut. 2017;223:695–704.
Vallero DA. Fundamentals of air pollution. (Academic press; 2014).
Moya J, Phillips L, Schuda L, Wood P, Diaz A, Lee R, et al. Exposure factors handbook 2011 edn (Final Report). US Environmental Protection Agency, Washington, DC, EPA/600/R-09/052F, 2011.
Gumus AT. Evaluation of hazardous waste transportation firms by using a two step fuzzy-AHP and TOPSIS methodology. Exp Syst Appl. 2009;36:4067–74.
Sun C-C. A performance evaluation model by integrating fuzzy AHP and fuzzy TOPSIS methods. Exp Syst Appl. 2010;37:7745–54.
Borza S, Inta M, Serbu R, Marza B. Multi-criteria analysis of pollution caused by auto traffic in a geographical area limited to applicability for an eco-economy environment. Sustainability. 2018;10:4240.
Yao B-g, Wang Y-x, Ye X-y, Zhang F, Peng Y-l. Impact of structural features on dynamic breathing resistance of healthcare face mask. Sci Total Environ. 2019;689:743–53.
Mahdavi A, Bahloul A, Haghighat F, Ostiguy C. Contribution of breathing frequency and inhalation flow rate on performance of N95 filtering facepiece respirators. Ann Occup Hyg. 2013;58:195–205.
Acknowledgements
This study was financially supported by the Iran National Science Foundation (INSF) (grant number: 97011909). The authors are also grateful to Institute for Environmental Research (IER), Tehran Heart Center (THC), and the Exceptional Talents Development Center at Tehran University of Medical Sciences. It should be noted that the use of any brand names in the current study in no way endorses the use of its RFM and other products. This article is the first part of a randomized crossover trial entitled “Evaluating performance of face masks in reducing ambient particulate matter exposure and their wearing on acute cardiovascular effects” with registration number “IRCT20181214041961N1”, in Tehran megacity and its results will be used in the next article. We sincerely acknowledge Sadegh Niazi, PhD candidate at Queensland University of Technology, for his assistance in the revision of our manuscript.
Author information
Authors and Affiliations
Contributions
SF, MSH, and KN provided the idea for this work and designed the method. SF, MSH, and SHN performed the experiments. SF and RNN contributed to the data analysis. SF prepared all figures and tables, and wrote the main manuscript. SS, MH, MT, MY, and MSH revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Faridi, S., Nodehi, R.N., Sadeghian, S. et al. Can respirator face masks in a developing country reduce exposure to ambient particulate matter?. J Expo Sci Environ Epidemiol 30, 606–617 (2020). https://doi.org/10.1038/s41370-020-0222-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-020-0222-6
- Springer Nature America, Inc.
Keywords
This article is cited by
-
Atmosphere particulate matter and respiratory diseases during COVID-19 in Korea
Scientific Reports (2024)
-
Cardiovascular health effects of wearing a particulate-filtering respirator to reduce particulate matter exposure: a randomized crossover trial
Journal of Human Hypertension (2022)
-
Quantitative fit testing of filtering face-piece respirators during the COVID-19 pandemic reveals anthropometric deficits in most respirators available in Iran
Journal of Environmental Health Science and Engineering (2021)