Abstract
Background
Recent studies suggest that tirzepatide, a dual glucose-dependent insulinotropic-peptide (GIP) and glucagon-like peptide-1 receptor agonist (GLP-1 RA), has significant weight loss effects. This systematic review and meta-analysis aims to assess the efficacy and safety of tirzepatide for weight loss in patients with overweight or obesity.
Methods
Medline, Embase and Cochrane CENTRAL were searched for randomized controlled trials (RCTs) on tirzepatide’s weight loss efficacy for these patients. A single arm meta-analysis of proportions estimated primary outcomes, ≥5%, ≥10%, and ≥15% weight loss, and adverse events (AEs); while meta-analysis of means estimated secondary outcomes. Comparative meta-analysis was conducted between tirzepatide and control arms where mean differences and odds ratios were estimated for continuous and dichotomous outcomes respectively.
Results
RCTs included in this study revealed that among 5800 patients, 78.22% (95% CI: 72.15% to 83.73%), 55.60% (95% CI: 46.54% to 64.47%), 32.28% (95% CI: 23.17% to 42.12%) achieved ≥5%, ≥10%, and ≥15% weight loss, respectively. Tirzepatide 5 mg demonstrated weight loss superiority relative to placebo (MD: −12.47 kg, 95% CI: −13.94 kg to −11.00 kg) and semaglutide (n = 1409, MD: −1.90 kg, 95% CI: −2.97 kg to −0.83 kg) with dose-dependent increase for 10 mg and 15 mg doses. The comparison between tirzepatide and semaglutide was examined in the SURPASS-2 trial that was included in this systematic review. For AEs, there was increase odds of experiencing gastrointestinal AEs with tirzepatide compared to placebo, but no significant difference with semaglutide.
Conclusion
Tirzepatide has significant potential as a weight loss drug in patients with overweight and obesity, with little increase in AEs compared to other weight loss drugs. With its ability to concurrently target multiple aspects of metabolic syndrome, it should be considered as the next helm of weight loss therapies.
Similar content being viewed by others
Introduction
Obesity is a leading cause of early morbidity and mortality [1, 2]. Global estimates that up to 39% and 13% of the global population are afflicted by overweight and obesity respectively [3, 4]. As a complex disease with multifactorial aetiology, it has been linked to a greater risk of major preventable causes of death and disability, including cardiometabolic and musculoskeletal diseases, type 2 diabetes mellitus (T2DM), stroke, nonalcoholic fatty liver disease (NAFLD), and various forms of malignancies [5,6,7,8,9]. Consequentially, patients with overweight and obesity suffer from not only decrease in quality of life [8], but also a 3.9% decrease in life expectancy [10]. Due to the constellation of interrelated factors that contribute to metabolic syndrome, there has been increasing focus towards holistic care of the patient where multiple aspects of metabolic syndrome are targeted concurrently, instead of treating the individual disorders alone [11].
The mainstay of treatment for obesity and other metabolic diseases such as diabetes includes a combination of lifestyle modification programs, pharmacotherapy, and if indicated, bariatric surgery [12]. Recently, the US Food and Drug Administration (FDA) has approved the dual glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) agonist, tirzepatide, as a once-weekly injection to improve blood glucose control in T2DM patients. The dual GIP/GLP-1 agonist properties of tirzepatide distinguish it from existing anti-obesity drugs and has been shown to produce higher efficacies for inducing weight loss and blood glucose control, with favourable side effect profile as compared to GLP-1 agonist, semaglutide [13]. Numerous studies have explored the efficacy of tirzepatide in the treatment of T2DM [14,15,16]. However, there is a paucity of data regarding its pooled efficacy and safety in patients in the context of individuals with obesity. Studies have suggested that patients on tirzepatide have close to two times the odds of having ≥5% weight loss compared to semaglutide, with a dose-dependent weight reduction [14]. In view of emerging trials reporting the efficacy of tirzepatide in the treatment of patients with overweight or obesity, we conducted a systematic review and meta-analysis to examine the efficacy and safety of tirzepatide on weight loss of participants with overweight or obesity in randomized controlled trials.
Methods
Search strategy
With reference to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [17], Medline, Embase, and Cochrane CENTRAL databases were searched for relevant randomised controlled trials relating to tirzepatide’s efficacy in inducing weight loss in patients with overweight or obesity. Relevant papers were identified from 2017 to 24 July 2022. Keywords and MeSH terms synonymous with “tirzepatide”, “LY3298176”, “dual GIP and GLP-1RA”, and “clinical trials” were utilised (Supplementary Material 1). Citations were imported into EndNote 20 for the initial sieve with the removal of duplicates. References of related reviews and included articles were also hand-screened to ensure a comprehensive search [18, 19].
Study selection and data extraction
Four authors (BTX, PXH, CYH and RG) independently screened the studies identified within the initial search, and studies that met the inclusion criteria were marked for inclusion. The following criteria were used for the inclusion of studies: (1) randomized controlled trials written in or translated into English; (2) studies evaluating adult patients (aged 18 and above) who were overweight or obese (with or without T2DM) for weight loss; (3) no use of any weight loss or weight gain medications other than tirzepatide and control drug; (4) reported weight change of participants. All observational studies, case-control studies, reviews, meta-analyses, editorials, commentaries, conference abstracts, and non-English language articles were excluded. Studies that obtained results from the same databases were excluded, and the latest or the most comprehensive publication was included in this paper. Overweight and obesity were defined, where possible, as a body mass index (BMI) of 23–24.9 kg/m2 and ≥25 kg/m2 for Asians [20], and a BMI of 25–29.9 kg/m2 and ≥30 kg/m2 for Europeans [3], respectively. Any disputes regarding inclusion of articles were resolved through consensus from a fifth independent author (CHN).
Using a predetermined datasheet, data from the included articles were extracted independently by three authors (BTX, PXH, CYH). Information extracted included the study characteristics (country, region, clinical trial registration number/code, year of study, phase, duration of study, and multi/single centre trials), baseline characteristics (total sample size, mean age, gender, race, body mass index [BMI], weight, waist circumference, total cholesterol [TC], high-density lipoprotein [HDL], low-density lipoprotein [LDL], triglyceride [TG], glycated haemoglobin [HbA1c], fasting blood glucose [FBG], presence of other comorbidities), outcomes (≥5%, ≥10%, and ≥15% total weight loss, change in BMI, weight, waist circumference, lipids profile, glucose profile, blood pressure) and adverse events (AEs) of both treatment and control arms of the included trials. Estimated values of the mean and standard deviation were derived from their respective median and interquartile ranges using formulas devised by Wan et al. when they were not provided [21]. The units for cholesterol, triglycerides and glucose were millimoles per litre (mmol/l). Secondary outcomes included the change in body weight, waist circumference, lipid profile, glycaemic profile (HbA1c and FBG) and blood pressure (systolic and diastolic). Additional comparative analyses were performed on both primary and secondary outcomes according to the tirzepatide doses and choice of control drug. With regards to the safety profile of tirzepatide, we examined the possible AEs that participants experienced through the course of the trial.
Statistical analysis
All analyses were performed in RStudio (version 4.0.3). Two main analyses were conducted in this meta-analysis. Firstly, a single arm meta-analysis of proportions for dichotomous variables and mean differences for continuous variables of participants in the trials was pooled using a generalized linear mixed model (GLMM) for each cut-off (≥5, 10, 15% weight loss) with Clopper-Pearson intervals to stabilise the variance [22, 23]. Secondly, a comparative meta-analysis was used to compare the effectiveness of tirzepatide with the control arms of the included RCTs. Mean differences (MD) and odds ratios (OR) were estimated for continuous and dichotomous outcomes respectively using DerSimonian and Liard random effects [24]. Statistical heterogeneity was measured using I2, and Cochran Q test, where an I2 value of <25% is low, 25% to 50% low-moderate, 50–75% moderate-high and >75% high degrees of heterogeneity [25]. Additionally, a Cochran Q test value of ≤0.10 was deemed statistically significant. The random effects model was used regardless of heterogeneity scores [26]. Hartung-Knapp adjustments were employed to adjust for confidence intervals by controlling for heterogeneity arising from between-study estimations [27]. Analyses were only conducted when sufficient data could be extracted for the outcome of interest. Funnel plots were generated to illustrate publication bias as seen in Supplementary Material 2 for ≥5, 10 and 15% weight loss. The asymmetrical nature of the funnel plots can be attributed to the limited number of studies included in this meta-analysis (n < 10) as well as the different dosages of tirzepatide given [28]. Additional analyses were performed on both primary and secondary outcomes according to the tirzepatide doses and choice of control drug. Where possible, a sensitivity analysis was conducted on studies that included only T2DM patients. A p-value of <0.05 was considered as statistically significant.
Quality and risk-of-bias assessment
The risk-of-bias of the outcomes of the RCTs were assessed using the Cochrane Risk-of-Bias tool for randomized trials (RoB-2). This evaluates quality and bias of the included outcomes across five domains. The five domains include the trial’s randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result [29]. Two authors (BTX and PXH) independently assessed the included trials, and any disagreements were resolved following discussion with a third independent author (CYH). The outcomes assessed in this systematic review include ≥5%, 10%, 15% weight loss, percentage weight loss from baseline, HbA1c and fasting blood glucose, lipid profile, systolic and diastolic blood pressure, gastrointestinal adverse effects and discontinuations from adverse events. The final assessment of the outcomes was presented using the Robvis visualisation tool.
Results
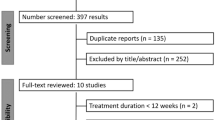
A total of 204 publications were identified in the initial search strategy, among which 84 were excluded as duplicates. Another 61 papers were then excluded after the initial sieve, with a full-text review being conducted for 59 papers. Finally, 7 articles involving 5905 patients and 7 trials were included in this meta-analysis (Fig. 1). Of the trials included, 5 were multinational [13, 30,31,32,33], one was conducted in Japan [34] and one in Germany [35]. All the studies were multicentre trials (n = 7), with participants with overweight or obesity, where most participants have concomitant diabetes. Out of the 7 trials involved, six trials examined the effect of 5 mg and 10 mg tirzepatide, while all seven trials assessed 15 mg tirzepatide. Of these trials, three used placebos as control, two used insulin and one used semaglutide as the comparator. The SURPASS J-combo clinical trial was used only for single arm analysis as there was no comparator in the study [34]. The primary outcomes of the included studies were percentage change in body weight from baseline and proportion of patients who achieved ≥5% weight loss [30], change in HbA1c from baseline [13, 31, 32] and safety and tolerability of tirzepatide [33, 34]. At baseline, the mean age, BMI, weight, and waist circumference of included patients were 54.95 years, 34.47 kg/m2, 95.50 kg and 110.16 cm, respectively. The baseline mean TC, LDL, HDL, and TG were 4.45, 2.51, 1.16, 1.72 mmol/L, respectively. Baseline mean HbA1c was 7.58% and fasting blood glucose 8.24 mmol/L. A summary of the included publications and baseline characteristics of participants is shown in Supplementary Material 3. Most of the included studies’ outcomes were assessed to have low to moderate risk of bias, and the detailed RoB-2 assessment can be seen in Supplementary Material 4.
Efficacy of tirzepatide in weight loss
A summary of the meta-analysis findings can be found in Table 1. A total of 5800 participants in the tirzepatide groups had data available for ≥5%, ≥10% and ≥15% weight loss. Among them, 78.22% (95% CI: 72.15% to 83.73%), 55.60% (95% CI: 46.54% to 64.47%), and 32.28% (95% CI: 23.17% to 42.12%) of patients achieved ≥5%, ≥10%, and ≥15% total weight loss, respectively. When analysed by the dose of tirzepatide given, a dose-dependent effect was found (Fig. 2), where 5 mg, 10 mg, and 15 mg, had 65.91% of patients (95% CI: 53.92% to 76.95%), 80.72% (95% CI: 75.42% to 85.52%) and 86.95% (95% CI: 84.42% to 89.29%) achieving ≥5% weight loss, respectively. Similar findings were noted for ≥10% and ≥15% weight loss as shown in Table 1. A further sensitivity analysis was conducted for studies which only included patients with type 2 diabetes, we observed a lower proportion of patients with diabetes achieved ≥5%, ≥10% and ≥15% weight loss (Supplementary Material 5).
Tirzepatide showed superiority relative to placebo and semaglutide in participants having ≥5%, 10%, and 15% weight loss. Participants taking 5 mg, 10 mg and 15 mg doses of tirzepatide had 1.50 (95% CI: 1.15 to 1.96), 3.05 (95% CI: 2.27 to 4.08) and 4.25 (95% CI: 3.10 to 5.82) odds of achieving ≥5% weight loss compared to semaglutide. Compared to placebo, patients on 5 mg, 10 mg and 15 mg doses of tirzepatide had 10.95 (95% CI: 8.33 to 14.40), 15.33 (95% CI: 11.40 to 20.63) and 19.06 (95% CI: 13.88 to 26.18) odds of achieving ≥5% weight loss. Similar trends for achieving 10% and 15% or more weight loss for tirzepatide relative to placebo and semaglutide are shown in Supplementary Material 6.
Secondary outcomes
Data on the efficacy of varying doses of tirzepatide on weight loss can be found in Table 2. The pooled analysis revealed that overall weight loss with tirzepatide was −9.36 kg (95% CI: −12.08 kg to −6.63 kg). A dose-dependent relationship with weight loss was observed (p < 0.01), with higher weight loss observed for 5 mg (−7.20 kg, 95% CI: −12.35 kg to −2.06 kg), 10 mg (−10.18 kg, 95% CI: −16.30 kg to −4.06 kg), and 15 mg (−11.77 kg, 95% CI: −17.12 kg to −6.43 kg) of tirzepatide. Tirzepatide also reduced overall waist circumference by −11.04 cm (95% CI: −13.47 cm to −8.62 cm). We observed a dose-dependent reduction in waist circumference for 5 mg (−9.09 cm, 95% CI: −14.48 cm to −3.70 cm), 10 mg (−11.75 cm, 95% CI: −18.14 cm to −5.37 cm), and 15 mg (−12.27 cm, 95% CI: −19.02 cm to −5.52 cm) of tirzepatide. Tirzepatide significantly reduced TC, LDL and TG, with improvement in HDL. Tirzepatide reduced FBG by a mean of −2.56 mmol/L (95% CI: −3.14 mmol/L to −1.97 mmol/L) and HbA1c −2.04% (95% CI: −2.52% to −1.56%).
Compared to placebo, tirzepatide 5 mg was more effective in weight loss (MD: −12.47 kg, 95% CI: −13.94 kg to −11.00 kg) and reduction in waist circumference (MD: −10.00 cm, 95% CI: −11.64 cm to −8.54 cm), where greater reduction was noted with a higher tirzepatide dose. Similar improvements were noted for lipid profile, HbA1c and blood pressure (Supplementary Material 7). Compared to semaglutide, tirzepatide 5 mg was more effective in weight loss (MD: −1.90 kg, 95% CI: −2.97 kg to −0.83 kg) and reduction in waist circumference (MD: −1.30 cm, 95% CI: −2.45 cm to −0.15 cm), with a dose-dependent increase with 10 mg and 15 mg. Slight but significant improvements were also noted for TG, HDL, HbA1c, and FBG at 5 mg and 10 mg doses. No significant difference was observed between tirzepatide and semaglutide for LDL and TC (Supplementary Material 7).
Safety of tirzepatide use
A detailed summary of overall AEs is presented in Table 3. The overall rate of AE was 75.15% (95% CI: 71.45% to 78.69%). The reported rates of serious AEs and discontinuations were 6.22% (95% CI: 4.64% to 7.97%) and 6.34% (95% CI: 5.04% to 7.76%), respectively in a pooled analysis where 5905 participants were studied. Among the reported AEs, the most prevalent were gastrointestinal adverse events (18.42%, 95% CI: 4.74% to 38.27%), including diarrhoea (16.02%, 95% CI: 14.10% to 18.02%) and nausea (10.24%, 95% CI: 5.54% to 16.02%). A small proportion of patients (0.77%, 95% CI: 0.23% to 1.55%) experienced cardiovascular adverse events. Of note, no dose dependent relationship was noted for adverse events for all AEs examined (Supplementary Material 8).
A summary of the safety of tirzepatide as compared to placebo, semaglutide and insulin is shown in Supplementary Material 9. Tirzepatide had comparable overall adverse events and mortality when compared to placebo and semaglutide. Discontinuation of treatment due to adverse effects did not differ between tirzepatide 5 mg and semaglutide (OR 1.50, 95%CI: 0.83 to 2.73). However, tirzepatide 10 mg and 15 mg was associated with higher odds of discontinuation compared to semaglutide (10 mg, OR 2.21, 95% CI: 1.26 to 3.87; 15 mg, OR 2.23, 95% CI 1.15 to 4.30). The odds of discontinuation is also significant comparing tirzepatide 10 mg and placebo (OR 2.80, 95% CI: 1.59 to 4.95). For gastrointestinal AEs, no differences were noted for all doses of tirzepatide when compared to semaglutide, except for diarrhea with tirzepatide 10 mg (OR 1.51, 95% CI: 1.04 to 2.19). However, compared to placebo, tirzepatide 5 mg was associated with higher odds of constipation (OR 3.31 95% CI: 2.24 to 5.90), and dyspepsia (OR 2.23, 95% CI: 1.39 to 3.57). Tirzepatide 10 mg was associated with higher odds of constipation (OR 3.39, 95% CI: 2.29 to 4.01) and diarrhea (OR 3.42, 95% CI: 3.27 to 3.57) compared to placebo.
Discussion
Glucagon-like peptide 1 agonists, such as liraglutide and semaglutide, have been shown to improve weight loss and cardiometabolic risk factors [36]. Tirzepatide is a novel dual GIP and GLP-1 agonist and has been effective in treating T2DM, with concurrent superiority in body weight reduction as compared to other glucose-lowering medications [14, 15]. Our study shows that tirzepatide has a larger weight loss effect compared to placebo and semaglutide, with more favourable lipid profile and glycemia indices. These weight loss benefits should not be underestimated; approximately 80% and 57% of participants receiving tirzepatide 5 mg achieved a ≥ 5% and ≥10% weight loss respectively [16, 30]. Across all doses, tirzepatide has a higher proportion of patients achieving ≥10% and 15% weight loss as compared to semaglutide, suggesting the superiority of tirzepatide in inducing weight loss [16, 30].
There is a paradigm shift in the treatment approach of metabolic diseases towards care of the overall metabolic milieu rather than individual components; these can potentially be achieved by tirzepatide as it targets multiple aspects of metabolic syndrome concurrently [11]. By targeting both incretin hormones, GLP-1 and GIP, tirzepatide causes synergistic effect which stimulates insulin release from the pancreas as well as glucagonostatic effect [37]. Also, tirzepatide’s effect on GLP-1 decreases appetite, slows down gastric emptying and reduces food consumption; GIP has also been hypothesized to improve lipid metabolism by increasing lipolysis in fasting state and lipogenesis post-meal, thereby contributing to the improvement in management of metabolic diseases and obesity [38, 39].
Obesity has long been shown to be the precursor towards development of other metabolic diseases such as hyperlipidemia, hypertension, diabetes mellitus, and NAFLD [40, 41]. Currently, FDA approves the use of liraglutide, phentermine/topiramate, lorcaserin, naltrexone/bupropion and orlistat for long-term use (≥12 weeks), of which GLP-1 RA and phentermine/topiramate hold the greatest efficacy [42, 43]. In our study, tirzepatide treatment had an edge over GLP-1 RA (semaglutide) in inducing weight loss with dose-dependent superiority [14], hence providing physicians with an alternative treatment in metabolic weight management [44,45,46,47,48]. Several trials have been planned that can further expand tirzepatide’s indications, including its impact on NAFLD (SYNERGY-NASH). NAFLD is strongly associated with metabolic syndrome, with insulin resistance being a common pathology in both conditions [49]. Obesity and T2DM are strong independent risk factors for NAFLD, highlighting the complex intertwined relationship among these chronic conditions [50, 51]. With preliminary results from the SURPASS-3 trial revealing that tirzepatide is potentially hepatoprotective and can reduce hepatic steatosis, we highly anticipate the upcoming trials studying the impact of tirzepatide on NAFLD [52].
One of the limitations to the use of tirzepatide could be attributed to its high rates of adverse events; with up to 75% of patients experiencing AEs. However, occurrence of adverse events was not significantly higher when compared to placebo and semaglutide. Although gastrointestinal AEs (18.4%) of tirzepatide were not statistically higher compared to semaglutide, it is of concern as gastrointestinal adverse effects are common causes of discontinuation of T2DM medications [53]. Another important point to note is the potential long term cardiovascular benefits tirzepatide may provide. Our results revealed that a small proportion of participants (0.77%) experienced cardiovascular adverse events, with no increase in incidence as compared to placebo or insulin; this is supported by other studies that revealed a reduction in cardiovascular mortality as well [54, 55]. This is a potential advantage compared to existing weight loss medications including phentermine/topiramate and naltrexone/bupropion, as their cardiovascular risks have yet to be determined, with preliminary results revealing that both drugs have the potential of increasing heart rate and raising systolic blood pressure [56]. Ongoing trials examining the efficacy and safety of tirzepatide as compared to other medications, such as the SURPASS-CVOT trial (NCT04255433) and the SUMMIT trial (NCT04847557), will provide more information on the impact of tirzepatide on cardiovascular disease and outcomes [57,58,59].
Strengths and limitations
In this study, we aimed to examine the impact of tirzepatide on weight loss and metabolic markers (weight, BMI, waist circumference, glucose and lipid markers). There were some limitations in this study. Firstly, we were unable to quantify or account for potential effects that the various trials’ prescribed exercise and diet interventions have on the participants. Among the seven RCTs, only SURMOUNT-1 trial had specified lifestyle intervention while the other trials did not track the exercise or diet regimes of patients. Secondly, adverse events could be confounded by the concomitant medications or co-morbidities of the study population. Thirdly, of the studies examined, entire population of 6 out of the 7 studies consisted of patients with diabetes mellitus. This could cause bias on the occurrence of adverse events and cause deviation of the primary and secondary outcome data from that of a non-diabetic population. We attempted to control this by performing a sensitivity analysis, which we found no significant differences between the overall population and T2DM patients. Fourthly, as tirzepatide is relatively new, most of our studies came from North America, Europe and Japan; hence the interethnic variations and limited studies available may affect the generalisability of our findings and lead to high heterogeneity among the studies for certain outcomes. Additionally, as tirzepatide is a newly discovered drug, there is a sparse number of studies comparing tirzepatide to placebo or semaglutide. Thus, our findings may not be representative of the actual effects of the medication and may not be able to accurately reflect regional and time differences between included studies. Lastly, long-term effects of tirzepatide on cardiovascular, hepatic and renal AEs might not be reflected due to the relatively short nature of selected studies; this will improve with trials conducted for longer duration. This paper supports the findings of other systematic reviews on tirzepatide’s superiority over both semaglutide and placebo in inducing dose-dependent weight loss and improving glycemic control [14, 16]. Our study provides new insights on the favourable lipid profile that tirzepatide has over semaglutide and placebo, and focuses on patients with overweight or obesity. Besides considering tirzepatide’s effect on weight loss, future studies can explore its effects on changes in body composition, including loss of fat mass and body mass, where the latter may lead to complications including fatigue and reduction in resting energy expenditure [60]. Tirzepatide’s effect on liver enzymes such as aspartate transaminase (AST), alanine transaminase (ALT) and overall liver profile also remain a compelling aspect to explore to reveal tirzepatide’s potential effects on NAFLD and other obesity-related hepatic diseases.
Conclusion
Tirzepatide, a dual GIP/GLP1 agonist, is very effective in achieving weight loss in patients with overweight or obesity. With its ability to concurrently target multiple aspects of metabolic syndrome with relatively low rate of adverse events, it should be considered as the next helm of weight loss therapies.
Data availability
All articles in this manuscript are available from Medline and Embase.
References
Chong B, Kong G, Shankar K, Chew HSJ, Lin C, Goh R, et al. The global syndemic of metabolic diseases in the young adult population: a consortium of trends and projections from the Global Burden of Disease 2000–2019. Metabolism. 2023;141:155402. https://doi.org/10.1016/j.metabol.2023.155402.
Chew NWS, Ng CH, Tan DJH, Kong G, Lin C, Chin YH, et al. The global burden of metabolic disease: Data from 2000 to 2019. Cell Metab. 2023;35:414–28.e3. https://doi.org/10.1016/j.cmet.2023.02.003.
Organisation WH. Obesity and overweight fact sheet. World Health Organisation. Accessed 01/05/2022, 2022. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
Kinlen D, Cody D, O’Shea D. Complications of obesity. QJM. 2018;111:437–43. https://doi.org/10.1093/qjmed/hcx152.
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American association of clinical endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22:1–203. https://doi.org/10.4158/EP161365.GL.
Muthiah MD, Cheng Han N, Sanyal AJ. A clinical overview of non-alcoholic fatty liver disease: a guide to diagnosis, the clinical features, and complications—what the non-specialist needs to know. Diabetes Obes Metab. 2022;24:3–14. https://doi.org/10.1111/dom.14521.
Chew NWS, Ng CH, Muthiah MD, Sanyal AJ. Comprehensive review and updates on holistic approach towards non-alcoholic fatty liver disease management with cardiovascular disease. Curr Atheroscler Rep. 2022; https://doi.org/10.1007/s11883-022-01027-5.
Avila C, Holloway AC, Hahn MK, Morrison KM, Restivo M, Anglin R, et al. An overview of links between obesity and mental health. Curr Obes Rep. 2015;4:303–10.
Nyberg ST, Batty GD, Pentti J, Virtanen M, Alfredsson L, Fransson EI, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. Lancet Public Health. 2018;3:e490–7.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
de la Iglesia R, Loria-Kohen V, Zulet MA, Martinez JA, Reglero G, de Molina AR. Dietary strategies implicated in the prevention and treatment of metabolic syndrome. Int J Mol Sci. 2016;17. https://doi.org/10.3390/ijms17111877.
Lin C, Yeong TJJ, Lim WH, Ng CH, Chun EY, Chin YH, et al. Comparison of mechanistic pathways of bariatric surgery in patients with diabetes mellitus: a Bayesian network meta-analysis. Obesity (Silver Spring). 2022;30:1380–90. https://doi.org/10.1002/oby.23453.
Frías JP, Davies MJ, Rosenstock J, Manghi FCP, Lando LF, Bergman BK, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. Clinical Trial, Phase III; Comparative Study; Equivalence Trial; Journal Article; Multicenter Study; Randomized Controlled Trial; Research Support, Non‐U.S. Gov’t. N Engl J Med. 2021;385:503–15. https://doi.org/10.1056/NEJMoa2107519.
Karagiannis T, Avgerinos I, Liakos A, Del Prato S, Matthews DR, Tsapas A, et al. Management of type 2 diabetes with the dual GIP/GLP-1 receptor agonist tirzepatide: a systematic review and meta-analysis. Diabetologia. 2022;65:1251–61. https://doi.org/10.1007/s00125-022-05715-4.
Bhagavathula AS, Vidyasagar K, Tesfaye W. Efficacy and safety of tirzepatide in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized phase II/III trials. Pharmaceuticals (Basel, Switzerland). 2021;14. https://doi.org/10.3390/ph14100991.
Jung HN, Jung CH. The upcoming weekly tides (Semaglutide vs. Tirzepatide) against obesity: STEP or SURPASS? Review. J Obes Metab Syndr. 2022;31:28–36. https://doi.org/10.7570/JOMES22012.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Kolkailah AA, Doukky R, Pelletier MP, Volgman AS, Kaneko T, Nabhan AF. Transcatheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis in people with low surgical risk. Cochrane Database Syst Rev. 2019;12:Cd013319. https://doi.org/10.1002/14651858.CD013319.pub2.
Liao YB, Li YJ, Jun-Li L, Zhao ZG, Wei X, Tsauo JY, et al. Incidence, predictors and outcome of prosthesis-patient mismatch after transcatheter aortic valve replacement: a systematic review and meta-analysis. Sci Rep. 2017;7:15014. https://doi.org/10.1038/s41598-017-15396-4.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. https://doi.org/10.1016/S0140-6736(03)15268-3.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–13. https://doi.org/10.2307/2331986.
Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rucker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019;10:476–83. https://doi.org/10.1002/jrsm.1348.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. https://doi.org/10.1016/0197-2456(86)90046-2.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.
Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions. 2008:243–96. https://training.cochrane.org/handbook/current/chapter-10.
Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing Meta-Analysis With R: A Hands-On Guide. 1st ed. Chapman & Hall/CRC Press; 2021.
Collaboration TC. Recommendations on testing for funnel plot asymmetry. Accessed 17 August 2022, 2022. https://handbook-5-1.cochrane.org/chapter_10/10_4_3_1_recommendations_on_testing_for_funnel_plot_asymmetry.htm.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. Journal: Article in Press. N Engl J Med. 2022; https://doi.org/10.1056/NEJMoa2206038.
Ludvik B, Giorgino F, Jodar E, Frias JP, Lando LF.Brown K, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet (London, England). 2021;398:583–98. https://doi.org/10.1016/S0140-6736(21)01443-4. Comment in: Lancet. 2021; 398:560–561. PMID: 34370968 https://www.ncbi.nlm.nih.gov/pubmed/34370968.
Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Journal Article; Clinical Trial Protocol. Lancet. 2021;398:1811–24. https://doi.org/10.1016/S0140-6736(21)02188-7.
Coskun T, Sloop KW, Loghin C, Alsina-Fernandez J, Urva S, Bokvist KB, et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab. 2018;18:3–14. https://doi.org/10.1016/j.molmet.2018.09.009.
Kadowaki T, Chin R, Ozeki A, Imaoka T, Ogawa Y. Safety and efficacy of tirzepatide as an add-on to single oral antihyperglycaemic medication in patients with type 2 diabetes in Japan (SURPASS J-combo): a multicentre, randomised, open-label, parallel-group, phase 3 trial. Lancet Diabetes Endocr. 2022;10:634–44. https://doi.org/10.1016/s2213-8587(22)00187-5.
Heise T, Mari A, DeVries JH, Urva S, Li J, Pratt EJ, et al. Effects of subcutaneous tirzepatide versus placebo or semaglutide on pancreatic islet function and insulin sensitivity in adults with type 2 diabetes: a multicentre, randomised, double-blind, parallel-arm, phase 1 clinical trial. Clinical Trial, Phase I; Journal Article; Multicenter Study; Randomized Controlled Trial; Research Support, Non‐U.S. Gov’t. Lancet Diabetes Endocrinol. 2022;10:418–29. https://doi.org/10.1016/S2213-8587(22)00085-7.
O’Neil PM, Birkenfeld AL, McGowan B, Mosenzon O, Pedersen SD, Wharton S, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet. 2018;392:637–49. https://doi.org/10.1016/S0140-6736(18)31773-2.
Min T, Bain SC. The role of tirzepatide, dual GIP and GLP-1 receptor agonist, in the management of type 2 diabetes: the SURPASS clinical trials. Rev Diabetes Ther. 2021;12:143–57. https://doi.org/10.1007/s13300-020-00981-0.
Frias JP, Nauck MA, Van J, Kutner ME, Cui X, Benson C, et al. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet. 2018;392:2180–93. https://doi.org/10.1016/s0140-6736(18)32260-8.
Chin YH, Ng CH, Chew NW, Kong G, Lim WH, Tan DJH, et al. The placebo response rate and nocebo events in obesity pharmacological trials. A systematic review and meta-analysis. EClinicalMedicine. 2022;54:101685. https://doi.org/10.1016/j.eclinm.2022.101685.
Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17. https://doi.org/10.1007/978-3-319-48382-5_1.
Muthiah M, Ng CH, Chan KE, Fu CE, Lim WH, Tan DJH, et al. Type 2 diabetes mellitus in metabolic-associated fatty liver disease vs. type 2 diabetes mellitus non-alcoholic fatty liver disease: a longitudinal cohort analysis. Ann Hepatol. 2023;28:100762. https://doi.org/10.1016/j.aohep.2022.100762.
Bramante CT, Raatz S, Bomberg EM, Oberle MM, Ryder JR. Cardiovascular risks and benefits of medications used for weight loss. Front Endocrinol (Lausanne). 2019;10:883. https://doi.org/10.3389/fendo.2019.00883.
Salari N, Jafari S, Darvishi N, Valipour E, Mohammadi M, Mansouri K, et al. The best drug supplement for obesity treatment: a systematic review and network meta-analysis. Diabetol Metab Syndr. 2021;13:110. https://doi.org/10.1186/s13098-021-00733-5.
Vosoughi K, Atieh J, Khanna L, Khoshbin K, Prokop LJ, Davitkov P, et al. Association of glucagon-like peptide 1 analogs and agonists administered for obesity with weight loss and adverse events: a systematic review and network meta-analysis. EClinicalMedicine. 2021;42:101213. https://doi.org/10.1016/j.eclinm.2021.101213.
Cacciottolo TM, Evans K. Research in brief: effective pharmacotherapy for the management of obesity. Clin Med (Lond). 2021;21:e517–8. https://doi.org/10.7861/clinmed.2021-0253.
Fornes A, Huff J, Pritchard RI, Godfrey M. Once-weekly semaglutide for weight management: a clinical review. J Pharm Technol. 2022;38:239–46. https://doi.org/10.1177/87551225221092681.
Ng CH, Lin SY, Chin YH, Lee MH, Syn N, Goh XL, et al. Antidiabetic medications for type 2 diabetics with nonalcoholic fatty liver disease: evidence from a network meta-analysis of randomized controlled trials. Endocr Pract. 2022;28:223–30. https://doi.org/10.1016/j.eprac.2021.09.013.
Quek J, Chan KE, Wong ZY, Tan C, Tan B, Lim WH, et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8:20–30. https://doi.org/10.1016/s2468-1253(22)00317-x.
Le MH, Yeo YH, Zou B, Barnet S, Henry L, Cheung R, et al. Forecasted 2040 global prevalence of nonalcoholic fatty liver disease using hierarchical bayesian approach. Clin Mol Hepatol. 2022;28:841–50. https://doi.org/10.3350/cmh.2022.0239.
Kang SH, Cho Y, Jeong SW, Kim SU, Lee JW, Korean NSG. From nonalcoholic fatty liver disease to metabolic-associated fatty liver disease: big wave or ripple? Clin Mol Hepatol. 2021;27:257–69. https://doi.org/10.3350/cmh.2021.0067.
Paschos P, Paletas K. Non alcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009;13:9–19.
Gastaldelli A, Cusi K, Fernandez Lando L, Bray R, Brouwers B, Rodriguez A. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10:393–406. https://doi.org/10.1016/S2213-8587(22)00070-5.
Roborel de Climens A, Pain E, Boss A, Shaunik A. Understanding reasons for treatment discontinuation, attitudes and education needs among people who discontinue type 2 diabetes treatment: results from an online patient survey in the USA and UK. Diabetes Ther. 2020;11:1873–81. https://doi.org/10.1007/s13300-020-00843-9.
Sattar N, McGuire DK, Pavo I, Weerakkody GJ, Nishiyama H, Wiese RJ, et al. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat Med. 2022;28:591–8. https://doi.org/10.1038/s41591-022-01707-4.
Kong G, Chin YH, Chong B, Goh RSJ, Lim OZH, Ng CH, et al. Higher mortality in acute coronary syndrome patients without standard modifiable risk factors: results from a global meta-analysis of 1,285,722 patients. Int J Cardiol. 2023;371:432–40. https://doi.org/10.1016/j.ijcard.2022.09.062.
Vorsanger MH, Subramanyam P, Weintraub HS, Lamm SH, Underberg JA, Gianos E, et al. Cardiovascular Effects of the New Weight Loss Agents. J Am Coll Cardiol. 2016;68:849–59. https://doi.org/10.1016/j.jacc.2016.06.007.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394:121–30. https://doi.org/10.1016/S0140-6736(19)31149-3.
Nct. A study of tirzepatide (LY3298176) compared with dulaglutide on major cardiovascular events in participants with type 2 diabetes (SURPASS-CVOT). https://www.clinicaltrials.gov/ct2/show/NCT04255433.
A study of tirzepatide (LY3298176) in participants with heart failure with preserved ejection fraction and obesity (SUMMIT). https://ClinicalTrials.gov/show/NCT04847557.
Willoughby D, Hewlings S, Kalman D. Body composition changes in weight loss: strategies and supplementation for maintaining lean body mass, a brief review. Nutrients. 2018;10. https://doi.org/10.3390/nu10121876.
Acknowledgements
All authors have made substantial contributions to all the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. No writing assistance was obtained in the preparation of the manuscript. The manuscript, including related data, figures and tables has not been previously published and that the manuscript is not under consideration elsewhere.
Author information
Authors and Affiliations
Contributions
Conceptualization—YHC, NWSC, MDM, MN, CHN. Data curation—BT, X-HP, YHC. Formal analysis—YHC, RSJG, CL, VVA, ECZL. Supervision—DYY, MYC, CMK, AM, MDM, MN, CHN, NWSC. Validation—YHC, NWSC, CHN, NWSC. Writing, original draft – BT, X-HP, YHC. Writing, review, and editing—BT, X-HP, YHC, HSJC, RSJG, CL, VVA, ECZL, KEC, GK, CEYO, HCC, DYY, MYC, CMK, AM, MDM, MN, CHN, NWSC. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
MYC: Speaker’s fees and research grants Astra Zeneca, Abbott Technologies and Boston Scientific. MN: MN has been on the advisory board for 89BIO, Gilead, Intercept, Pfizer, Novo Nordisk, Blade, EchoSens, Fractyl, Terns, Siemens and Roche diagnostic; he has received research support from Allergan, BMS, Gilead, Galmed, Galectin, Genfit, Conatus, Enanta, Madrigal, Novartis, Pfizer, Shire, Viking and Zydus; he is a minor shareholder or has stocks in Anaetos, Rivus Pharma and Viking. All other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, B., Pan, XH., Chew, H.S.J. et al. Efficacy and safety of tirzepatide for treatment of overweight or obesity. A systematic review and meta-analysis. Int J Obes 47, 677–685 (2023). https://doi.org/10.1038/s41366-023-01321-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01321-5
- Springer Nature Limited
This article is cited by
-
Exploration of the potential association between GLP-1 receptor agonists and suicidal or self-injurious behaviors: a pharmacovigilance study based on the FDA Adverse Event Reporting System database
BMC Medicine (2024)
-
Associations of metabolic disorders with hypertension and cardiovascular disease: recent findings and therapeutic perspectives
Hypertension Research (2024)
-
Efficacy and safety of tirzepatide versus placebo in overweight or obese adults without diabetes: a systematic review and meta-analysis of randomized controlled trials
International Journal of Clinical Pharmacy (2024)