Abstract
Background
In the United States, one in five adolescents are obese. Index-based dietary patterns are measures of the overall diet that have the potential to serve as valuable obesity risk stratification tools. However, little is known about the association between adherence to index-based dietary patterns in childhood and BMI during the transition from childhood to adolescence.
Objective
To prospectively examine the relationship between adherence to three index-based dietary patterns in childhood and BMI trajectory during the transition to adolescence.
Methods
The study included 581 children enrolled in a Colorado prospective cohort study conducted between 2006 and 2015. Dietary intake was assessed with the Block Kids Food Frequency Questionnaire at age 10 years. Scores were calculated for the Healthy Eating Index—2010 (HEI-2010), the alternate Mediterranean (aMED) diet, and the Dietary Approaches to Stop Hypertension (DASH) diet. Weight and height were assessed via anthropometry at two research visits (ages 10 and 16 years), with interim clinical measurements extracted from Kaiser Permanente medical records. Separate mixed models were used to assess the association between each diet index score and BMI over a 6-year period. Models were stratified by sex and adjusted for age, race/ethnicity, income, and exposure to gestational diabetes.
Results
Median (IQR) number of BMI assessments was 14 (10–18). Among girls, for every ten-unit increase in HEI-2010 score, there was an average 0.64 kg/m2 decrease (p = 0.007) in BMI over time, after adjustment for covariates. Among girls, there was no association between BMI and aMED (β = −0.19, p = 0.24) or DASH (β = 0.28, p = 0.38). Among boys, there was no statistically significant association between BMI and HEI-2010 (0.06, p = 0.83), aMED (0.07, p = 0.70), or DASH (0.42, p = 0.06).
Conclusions
Efforts to prevent adolescent obesity could benefit from considering the degree of adherence to federal dietary guidance, as assessed by the HEI, in the period preceding adolescence, especially among girls.
Similar content being viewed by others
Introduction
In the United States, 20% of adolescents are obese [1]. Obesity in adolescence, defined as a body mass index (BMI) at or above the 95th percentile, is associated with poor cardiovascular health, depression, and lower self-esteem and quality of life [2,3,4,5]. The prevalence of obesity is higher among adolescents aged 12–19 years than children aged 6–11 years [1], and the increase in obesity from childhood to adolescence may be larger among girls than boys [6]. This indicates that the transition from childhood to adolescence may be a critical period [7] for preventing adolescent obesity. Therefore, the development of effective obesity prevention strategies for adolescents requires an understanding of the factors that influence BMI trajectories between childhood and adolescence. Further, understanding BMI trajectories and their determinants among youth is important because growth trajectories have been linked to adverse cardio-metabolic outcomes across the life course [8, 9].
Dietary patterns established during childhood may influence BMI trajectories between childhood and adolescence. Dietary patterns differ from traditional approaches to describing what children eat because they measure the overall diet versus intake of individual foods or nutrients. The use of dietary patterns may be a practical approach to operationalizing dietary intake in studies related to obesity prevention because it is likely easier for individuals to adopt an overall dietary pattern than adhere to dozens of separate recommendations for single foods or nutrients [10]. Two key approaches have been used to operationalize dietary patterns: (1) data-driven dietary patterns that use variable reduction statistical techniques to describe which foods and beverages are most likely to be consumed in combination and, (2) index-based dietary patterns, which are defined a priori based on dietary recommendations, and assess how well individuals adhere to an “ideal” diet [10, 11].
Little is known about the association between adherence to index-based dietary patterns and BMI trajectories during the transition from childhood to adolescence. The Healthy Eating Index (HEI), the alternate Mediterranean diet (aMED), and the Dietary Approaches to Stop Hypertension (DASH) diet [12] are index-based dietary patterns with the potential to serve as valuable obesity risk stratification tools among youth. Foods, food groups, and nutrient components of these indices have been individually linked to adolescent obesity [13, 14]. However, many studies that assess the association between these index-based dietary patterns and adolescent adiposity rely on cross-sectional study designs that cannot establish a temporal relationship between diet and body size [15] or are conducted among populations outside the US [16, 17]. Further, studies that consider the association between all three index-based dietary patterns and adiposity in a single cohort are needed to determine whether one of the three is a better predictor of BMI during the transition to adolescence.
The overall objective of this study was to prospectively examine the relationship between adherence to three index-based dietary patterns (HEI, aMED, DASH) in childhood and BMI trajectory during the transition from childhood to adolescence. Specifically, we used data on adherence to index-based dietary patterns in childhood, and longitudinal data on BMI collected at multiple time points over a 6-year period during the transition from childhood to adolescence from the Exploring Perinatal Outcomes in Children (EPOCH) study. We expected that dietary intake in childhood would be associated with BMI trajectory because there is growing evidence that childhood exposures, even at a single time point, have implications for growth, development, and chronic disease risk across the life course [18], especially when those exposures occur during periods of high developmental plasticity [7]. Given that the strength of the relationship between dietary intake and obesity may vary by sex [19, 20], we evaluated the association for boys and girls separately.
Methods
Study design and participants
The EPOCH study is a historical prospective cohort study conducted among children born to women who were exposed or not to gestational diabetes mellitus (GDM) during pregnancy and were members of the Kaiser Permanente of Colorado health plan. Children enrolled in EPOCH were invited to participate in two research visits, 6 years apart. The first visit occurred between 2006 and 2009 (Visit 1: mean age 10.4 years, SD 1.4) and the second between 2012 and 2015 (Visit 2: mean age 16.7 years, SD 1.2). In addition to the two research visits, weight and height data collected during pediatric office visits were abstracted from medical records. The eligible cohort for the present analysis included youth with data on BMI, dietary intake, GDM exposure, sex, household income, and race/ethnicity at Visit 1 (n = 581). The study was approved by the Colorado Multiple Institutional Review Board. Mothers provided written informed consent, and children provided written assent.
Variables
Body mass index (BMI)
BMI was calculated as weight (kg)/height (m2). The study included weight and height measurements from two research visits and medical record abstraction. At the two EPOCH research visits, weight was measured to the nearest 0.1 kg with a calibrated electronic scale and height was measured to the nearest 0.1 cm using a stadiometer. Weight and height were measured in duplicate, and an average was taken. Participants were lightly clothed without shoes for all measurements. For weight and height measurements obtained from the medical records, weight and height were assessed using usual clinical practice. The outcome measure was BMI trajectories versus change in BMI or BMI category for two reasons. First, trajectories can reflect the timing of obesity onset, the duration of excess weight, the velocity and acceleration of weight gain, and the degree of excess adiposity [21], while BMI category only reflects the degree of excess adiposity. Second, the baseline research visit occurred around age 10, which coincides with the onset of puberty and puberty-related changes in fat deposition for some, but not all, children [22]. The use of BMI trajectory as the outcome measure avoids reliance on a single estimate of BMI that may occur at unstandardized stages in pubertal development within the analytic sample. We additionally used the World Health Organization SAS macro to calculate sex-specific BMI z-scores for each child.
Dietary intake
Dietary intake was assessed with the Block Kids Food Frequency Questionnaire (FFQ) at the first research visit. This validated questionnaire [23] was used to assess intake frequency and average portion size of 85 commonly consumed foods and beverages over the preceding 7 days. The FFQ also included open-ended questions that allowed participants to report intake of foods and beverages not included in the list of commonly consumed foods. Responses were converted into estimates of energy intake, macronutrient intake, and intake of different food types or food groups. Estimates of dietary intake from the FFQ were used to calculate scores for three diet indices: the Healthy Eating Index—2010 (HEI-2010) [24], aMED [25], and DASH [26]. The scoring rubric for each index is shown in Table 1. Slight modifications (described below) were made to the computations because the Block Kids FFQ did not query some index components. Our analysis was limited to dietary exposures at the first research visit only to ensure a temporal relationship between the exposure and the outcome. The life stage at which diet was measured (pre-puberty) is a pivotal time developmentally because children at this age can express more autonomy in food selection, and it may be an important predictor of dietary intake in adolescence. We therefore expected diet at Visit 1 to be a proxy for dietary patterns during adolescence.
Healthy Eating Index—2010 (HEI-2010)
The HEI-2010 was a diet quality index that compared usual intake to the Dietary Guidelines for Americans 2010–2015 [24]. Individual diets were scored based on the intake of ten food groups (total vegetables, greens and beans, total fruit, whole fruit, whole grains, dairy, total protein foods, seafood and plant protein, refined grains, and empty calories), one nutrient (sodium), and one nutrient ratio (fatty acid ratio). The empty calories component was standardized to total energy intake. All other components, except the fatty acid ratio, were standardized to daily intake of 1000 kilocalories (kcal). Components were awarded a point value and prorated based on the maximum scores. The scores for all twelve components were summed to compute an overall HEI-2010 score. The total possible score ranged from 1 to 100, where higher scores indicate greater adherence to the dietary guidelines. In order to convert data from the Block Kids FFQ to an HEI-2010 score, the scoring algorithm was altered for the empty calories and whole fruit components (see Table 1).
Alternate Mediterranean diet (aMED)
The Mediterranean diet index, initially created for European populations, was based on epidemiologic studies, which showed that adherence to a diet typically consumed among Mediterranean populations was associated with reduced mortality [27,28,29]. In 2005, the Mediterranean diet index was adapted into a new version, the aMED diet, for use among populations in the United States [12, 25]. Scores were based on one nutrient ratio (mono-unsaturated fatty acids to saturated fatty acid), and intake of eight food groups, including whole grains, fruits, nuts, legumes, fish, red and processed meat, alcohol, and vegetables (excluding potatoes). For each of the nine components, the index awarded a score of zero for intake below the sex-specific median, and a score of one for intake at or above the sex-specific median [12]. The total possible score ranged from one to nine, where higher scores indicated greater adherence to a Mediterranean diet. For the current study, the calculation of aMED scores was modified for the alcohol component and the vegetable component (see Table 1). Fish, legumes, and whole grains were scored as zero for no intake and one for greater than zero intake because median intake among EPOCH youth for these dietary components was zero.
Dietary Approaches to Stop Hypertension (DASH)
The DASH index was based on two randomized controlled trials, which evaluated the effect of dietary patterns on hypertension [26, 30]. Scores on the DASH index were based on intake of one nutrient (sodium) and seven food groups, including whole grains, vegetables (excluding potatoes), fruit, nuts, legumes, low-fat diary, sugar-sweetened beverages, red and processed meats [31]. The DASH score awarded between 1 and 5 points for each food group or nutrient based on sex-specific quintile rankings within the study population [12]. The total possible score ranged from 1 to 40, where higher scores indicated greater adherence to the DASH diet. In the current analysis, the DASH computation was modified to include potatoes in the vegetable category.
Other covariates
Demographic characteristics (sex, age, household income, race/ethnicity) were self-reported. Household income was categorized as <$50,000/year or ≥$50,000/year. Race/ethnicity was self-reported as non-Hispanic White, Hispanic, African-American, or other. Exposure to GDM (yes/no) was obtained from Kaiser Permanente of Colorado medical records. Exposure to GDM was included as a covariate because it is known to be associated with adiposity among youth and because the EPOCH study oversampled youth exposed to GDM [32].
Data analysis
All analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, North Carolina, United States). For Table 2, differences in sociodemographic characteristics by sex were evaluated using t tests for continuous variables (child age and diet index scores) and χ2 tests for categorical variables (race/ethnicity, maternal education, household income, BMI category). To evaluate the association between diet and BMI trajectory, we fit six separate general linear mixed models. For all six models, the outcome was the repeated BMI measurements throughout childhood and adolescence. We selected a continuous outcome (BMI trajectories) versus a categorical outcome (e.g., change in BMI category from Visit 1 to Visit 2) to increase statistical power [33]. Three models were constructed for girls and three for boys because the association between diet and BMI trajectory was expected to vary by sex [34,35,36]. Each model included HEI-2010, aMED, or DASH as a predictor. Mixed models [37] were used to assess the association between each diet index score and BMI after adjustment for covariates selected a priori. The covariates included household income, race/ethnicity, GDM exposure, age, a cubic polynomial for age, and an age squared by GDM interaction term because the association between age and BMI was expected to vary by GDM exposure [38]. Unstructured covariance structures were used to account for repeated measurements of BMI within participants and for the increase in the variance of BMI over time. Degrees of freedom were adjusted using methods from Kenward and Roger [39], and the normality of the residuals was assessed using jackknife studentized residuals. This modeling approach was also repeated using the same predictors and covariates with BMI z-score as the outcome.
Previous studies among youth with BMI trajectories as the outcome have used linear [40], quadratic [38, 40], or cubic [41, 42] terms for age. Therefore, multiple polynomial terms for age were added to the base model to determine if the best fit model for the effects of age on BMI was linear, quadratic, or cubic. This approach for selecting the best fit polynomial term for age was similar to what has been previously used for modeling BMI trajectories among EPOCH participants in infancy and early childhood [38]. All parameters were statistically significant except for the quadratic and cubic terms among boys. For comparability across sexes, we included the same cubic polynomial term for age in the models for girls and boys. However, we also fit a linear model for BMI among boys as part of a sensitivity analysis. The two-sided alpha level was set at 0.05.
Results
Complete data on the variables of interest were collected from 581 participants. Demographic characteristics by sex are shown in Table 2. In the full sample, 50.4% of participants were female. Children were 48.4% Non-Hispanic white, 38.0% Hispanic, 8.1% African-American, and 5.5% other. Almost 30% of children were overweight or obese at the first research visit. Demographic characteristics, diet index scores, and the proportion of children in each BMI category did not vary by sex (see Table 2). The mean and median number of BMI data points was 14, with a standard deviation of 5.6 and an interquartile range of 10–18, including the two research visits and the medical record abstraction.
Mean HEI-2010 score was 49 (SD 10), with range 25–78. For the 12 components of the HEI, participants were most adherent to the Dietary Guidelines for Americans for sodium, whole fruit, total fruit, and refined grains; and least adherent for the components whole grains, greens and beans, total vegetables, total protein, seafood and plant proteins, low-fat dairy, empty calories, and fatty acid ratio. Mean aMED score was 3 (SD 1), with range 0–7. Mean DASH score was 22 (SD 4), with range 11–33.
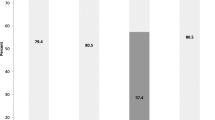
The association between adherence to each diet index and BMI trajectory by child sex is shown in Table 3. Among girls, for every ten-unit increase in HEI-2010 score, there was an average 0.64 kg/m2 decrease (p = 0.007) in BMI over time, even after adjustment for age, GDM exposure, household income, and race/ethnicity. In contrast, aMED and DASH scores were not significantly associated with BMI among girls. For boys, there was no association between BMI trajectory and HEI-2010 score (0.06, p = 0.83), aMED score (0.07, p = 0.70), or DASH score (0.42, p = 0.06) (Table 3). The finding of no association between diet and BMI among boys was the same when linear or cubic polynomial terms for age were included in the statistical model. When BMI z-score was the outcome, we similarly found among girls only that for every ten-unit increase in HEI-2010 score, there was an average 0.18 decrease (p = 0.006) in BMI z-score over time. Consistent with the findings for the BMI outcome, there was no association between HEI-2010 score and BMI z-score for boys (0.005, p = 0.95). There was no association between BMI z-score and aMED score or DASH score for boys or girls. Table 4 shows the observed mean BMI by diet index percentile and age, for girls and boys.
Discussion
We found that adherence to all three diet indices was low in EPOCH participants, which is consistent with findings from studies conducted among nationally representative child and adolescent populations in the US [43,44,45]. Among girls, greater adherence to HEI-2010, but not aMED or DASH, at age 10, was associated with lower BMI levels and BMI z-scores at all ages over the next 6 years, but not the velocity of BMI changes. Among boys, there was no association between adherence to any of the three indices and BMI or BMI z-score trajectory.
The finding that higher HEI-2010 scores were associated with lower BMI levels and BMI z-score was expected, given that this index is a measure of adherence to evidence-based federal dietary recommendations (the Dietary Guidelines for Americans) that focus on the prevention of chronic diseases, including obesity [46]. This finding provides insight into the types and timing of interventions that may be successful in reducing the burden of adolescent obesity. For the type of intervention, the present study provides support for obesity prevention strategies that promote adherence to the Dietary Guidelines for Americans, especially among girls. For the timing of interventions to prevent adolescent obesity, the present study provides support for approaches that target not only the adolescent years [47], but also middle childhood. Dietary patterns in middle childhood track into adolescence [48,49,50,51], so the estimates of dietary intake collected at a single research visit in this study may also reflect adolescent dietary patterns. Adhering to recommended dietary practices at age 10 may set the stage for future dietary practices that support healthy growth in the adolescent years. In fact, dietary patterns at age 10 may have been established as early as the toddler years. If so, then preventing adolescent obesity may require diet-related interventions even before age 10. Further, intervention studies have shown no effect or a marginal effect of diet interventions on obesity among adolescents [52, 53]. Interventions that promote recommended lifestyle behaviors in middle childhood may be more cost effective than interventions to treat obesity among adolescents [54].
The finding that HEI-2010 was associated with BMI and BMI z-score trajectory among female youth, but not male youth, is novel. A few studies provided evidence for an inverse association between HEI scores and BMI among adolescents, but these studies did not disaggregate the findings by sex and were primarily conducted outside of the US [15, 16, 55]. Sex differences in the association between HEI-2010 and BMI in the present study could reflect sex differences in the role of diet on BMI trajectory. Diet may be a stronger determinant of BMI among girls, while physical activity, which is higher overall among male than female youth [56, 57], may be a more important determinant of BMI among boys. Future studies that include measures of diet and physical activity could disentangle the relative effects of each lifestyle behavior by sex. The observed association between HEI-2010 and BMI among girls only may also be due to sex differences in the validity of the Block Kids FFQ for estimating food and nutrient intake for the HEI-2010 components. Sex differences are rarely considered in FFQ development or validation studies [58]. As such, dietary intake assessed at age 10 may be a better reflection of habitual dietary intake during the transition to adolescence among girls than boys. Habitual dietary intake will likely better predict body size changes than a fleeting dietary pattern.
The sex-specific association between diet and BMI trajectory reported in the current study appears to be reversed among adults. A systematic review published in 2017 concluded that earlier versions of the HEI (e.g., HEI-2005) were better predictors of obesity among adult men than women [19]. More recent studies among adults indicated that HEI-2010 score was inversely associated with central adiposity and percent body fat among men, but not women [20, 59].
The finding that aMED and DASH are not associated with BMI and BMI z-score trajectory is unexpected, given the partial overlap in dietary components between HEI-2010 and aMED (whole grains, total fruit, fatty acid ratio) and HEI-2010 and DASH (whole grains, total fruit, fatty acid ratio, low-fat dairy, sodium) [12]. One possible explanation is that aMED and DASH indices were based on epidemiological studies that aimed to identify dietary practices associated with lower mortality risk and blood pressure, respectively [25, 60], so they may be stronger predictors of other health outcomes besides obesity [27]. A second possible explanation is that scoring for the HEI-2010 is based on an individual’s intake relative to absolute cutoffs for food and nutrient quantities that reflect intake recommendations (e.g., 1100 mg of sodium per 1000 kcal). In contrast, scoring for aMED and DASH is based on intake relative to others in the study population, regardless of how closely intake is aligned with dietary guidance [12]. Accordingly, individuals could obtain a high score on the aMED and DASH indices, even with a relatively poor diet quality, if the reference study population consumed a diet poorly aligned with recommended practices. For example, total fruit intake was adequate for most children in EPOCH; however, half of children received a score of zero for total fruit intake on the aMED index because their intake was below the median. Consistent with the findings reported here, cross-sectional studies among youth also indicated no association between adherence to a Mediterranean [17] or DASH [44, 61] diet and adiposity outcomes, after adjustment for potential confounding factors. Nevertheless, two longitudinal studies in the US indicated that youth with greater adherence to the DASH index or a modified version of the Mediterranean diet index (KidMed) showed smaller gains in BMI over a 7–10-year period [45, 62].
This study has several strengths. First, body size may influence lifestyle behaviors among youth [63], so the longitudinal study design minimizes the risk of reverse causality. Second, the predictor and outcome variables were assessed using rigorous methods: an interviewer-administered dietary questionnaire validated for this age group [23], standardized anthropometric procedures to assess weight and height during the research visits, and objective measures of weight and height in the medical record. Third, the use of index-based dietary patterns is a strength because these analyses can be replicated in other populations. Studies that assess the predictive value of data-driven dietary patterns among youth are unique to those study populations [49, 64] and cannot necessarily be replicated in other groups of youth. Fourth, findings were replicated using BMI and BMI z-score trajectories as the outcomes, suggesting that the findings are robust.
This study also has limitations. First, the Block Kids FFQ was not designed to be converted to scores on the HEI-2010, aMED, and DASH indices, so modifications to the score computations were required. For example, the alcohol intake component was removed from the HEI-2010 and aMED scoring rubric because alcohol intake was not assessed with the Block Kids FFQ. However, this modification was unlikely to have clinically relevant effects on the diet index scores because alcohol intake is minimal among pre-adolescent youth [65]. Another example of a modification was in the computation of aMED scores. A component score of zero instead of one was awarded to participants who consumed the median intake for fish, legumes, and whole grains. Among EPOCH youth, the median intake for fish, legumes, and whole grains was zero. Maintaining the original scoring system would have led to an assignment of maximum component score for participants who consumed no fish, legumes, and whole grains. Another limitation of this study is that estimates of the association between diet and BMI trajectory may have been influenced by confounding factors not included in the analysis. Maternal prepregnancy BMI and children’s habitual physical activity, for example, have been linked to BMI among youth [66, 67], and may also be associated with children’s dietary intake [66]. Thus, these factors could be confounders or effect modifiers for the association between diet and BMI. Finally, scores on the HEI-2010, aMED, and DASH at age 10 were assumed to be an accurate estimation of habitual dietary intake in the period preceding the dietary assessment. However, if dietary intake at age 10 was not reflective of habitual dietary intake, then children’s diet index scores may not reflect intake that preceded the BMI trajectory.
This study identified an index-based dietary pattern, HEI-2010, that is associated with BMI trajectory in girls during the transition from childhood to adolescence. Future studies can build on this finding. One important next step is to identify the specific dimensions of BMI trajectories that are affected by adherence to the dietary guidelines. The specific dimensions of BMI trajectories that merit attention include the timing of obesity onset, the duration of excess weight, the velocity and acceleration of weight gain, and the degree of excess adiposity. Randomized controlled trials are needed to assess whether improving adherence to the Dietary Guidelines for Americans in childhood reduces the risk of adolescent obesity. Studies are also needed to describe how and why sex may modify the association between diet quality and BMI trajectory among youth. These types of studies will help determine if sex-specific lifestyle interventions are needed to reduce the prevalence of adolescent obesity. In addition, changes in body weight result from an imbalance of energy intake and energy expenditure. Studies among adults indicate sex differences in the association between physical activity and weight loss [68]. Therefore, future studies should evaluate the association between physical activity and BMI trajectory during the transition from childhood to adolescence, after adjustment for the degree of adherence to the dietary guidelines. If future studies indicate a stronger association between physical activity and BMI trajectory among boys than girls, this may help provide context to the lack of association between diet and BMI trajectory among boys participating in EPOCH. Finally, future studies which look at sex-specific BMI trajectories among youth should consider differences in the shape of the BMI trajectory by sex. Findings from EPOCH, as well as studies conducted in other populations, demonstrated a linear BMI trajectory among boys and a cubic trajectory among girls [40].
In conclusion, adherence to the HEI-2010, aMED, and DASH diet indices was low among EPOCH youth. Among girls, adherence to the Dietary Guidelines for Americans in childhood, as assessed by the HEI, was associated with higher BMI and BMI z-score during the transition to adolescence. Efforts to prevent adolescent obesity should take into consideration dietary practices in the period leading up to adolescence, especially among girls.
References
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–9.
Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev. 2017;18:742–54.
Griffiths LJ, Parsons TJ, Hill AJ. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes. 2010;5:282–304.
Buttitta M, Iliescu C, Rousseau A, Guerrien A. Quality of life in overweight and obese children and adolescents: a literature review. Qual Life Res. 2014;23:1117–39.
Gooding HC, Milliren C, Shay CM, Richmond TK, Field AE, Gillman MW. Achieving cardiovascular health in young adulthood-which adolescent factors matter? J Adolesc Health. 2016;58:119–21.
Dai S, Labarthe DR, Grunbaum JA, Harrist RB, Mueller WH. Longitudinal analysis of changes in indices of obesity from age 8 years to age 18 years. Project HeartBeat! Am J Epidemiol. 2002;156:720–9.
Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59:955–9.
Peneau S, Giudici KV, Gusto G, Goxe D, Lantieri O, Hercberg S, et al. Growth trajectories of body mass index during childhood: associated factors and health outcome at adulthood. J Pediatr. 2017;186:64–71.e1.
Aris IM, Rifas-Shiman SL, Li LJ, Kleinman KP, Coull BA, Gold DR, et al. Patterns of body mass index milestones in early life and cardiometabolic risk in early adolescence. Int J Epidemiol. 2019;48:157–67.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9.
Hodge A, Bassett J. What can we learn from dietary pattern analysis? Public Health Nutr. 2016;19:191–4.
Reedy J, Krebs-Smith SM, Miller PE, Liese AD, Kahle LL, Park Y, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144:881–9.
Harrington S. The role of sugar-sweetened beverage consumption in adolescent obesity: a review of the literature. J Sch Nurs. 2008;24:3–12.
Wall CR, Stewart AW, Hancox RJ, Murphy R, Braithwaite I, Beasley R, et al. Association between frequency of consumption of fruit, vegetables, nuts and pulses and BMI: analyses of the International Study of Asthma and Allergies in Childhood (ISAAC). Nutrients. 2018;10:316. https://doi.org/10.3390/nu10030316.
An R. Diet quality and physical activity in relation to childhood obesity. Int J Adolesc Med Health. 2017;29. https://doi.org/10.1515/ijamh-2015-0045.
Mohseni-Takalloo S, Hosseini-Esfahani F, Mirmiran P, Azizi F. Associations of pre-defined dietary patterns with obesity associated phenotypes in tehranian adolescents. Nutrients. 2016;8:505. https://doi.org/10.3390/nu8080505.
Cagiran Yilmaz F, Cagiran D, Ozcelik AO. Adolescent obesity and its association with diet quality and cardiovascular risk factors. Ecol Food Nutr. 2019;58:207–18.
Baird J, Jacob C, Barker M, Fall CH, Hanson M, Harvey NC, et al. Developmental origins of health and disease: a lifecourse approach to the prevention of non-communicable diseases. Healthcare. 2017;5:14. https://doi.org/10.3390/healthcare5010014.
Asghari G, Mirmiran P, Yuzbashian E, Azizi F. A systematic review of diet quality indices in relation to obesity. Br J Nutr. 2017;117:1055–65.
Drenowatz C, Shook RP, Hand GA, Hebert JR, Blair SN. The independent association between diet quality and body composition. Sci Rep. 2014;4:4928.
Jones-Smith JC, Neufeld LM, Laraia B, Ramakrishnan U, Garcia-Guerra A, Fernald LC. Early life growth trajectories and future risk for overweight. Nutr Diabetes. 2013;3:e60.
Biro FM, Kiess W. Contemporary trends in onset and completion of puberty, gain in height and adiposity. Endocr Dev. 2016;29:122–33.
Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. J Am Diet Assoc. 2008;108:862–6.
Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144:399–407.
Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82:163–73.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24.
Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72:30–43.
Hu FB. The Mediterranean diet and mortality-olive oil and beyond. N Engl J Med. 2003;348:2595–6.
Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, et al. Diet and overall survival in elderly people. BMJ. 1995;311:1457–60.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–20.
Hockett CW, Harrall KK, Moore BF, Starling AP, Bellatorre A, Sauder KA, et al. Persistent effects of in utero overnutrition on offspring adiposity: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabetologia. 2019;62:2017–24.
Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:1080.
Durao C, Oliveira A, Santos AC, Severo M, Guerra A, Barros H, et al. Protein intake and dietary glycemic load of 4-year-olds and association with adiposity and serum insulin at 7 years of age: sex-nutrient and nutrient-nutrient interactions. Int J Obes. 2017;41:533–41.
Durao C, Severo M, Oliveira A, Moreira P, Guerra A, Barros H, et al. Association between dietary patterns and adiposity from 4 to 7 years of age. Public Health Nutr. 2017;20:1973–82.
Wisniewski AB, Chernausek SD. Gender in childhood obesity: family environment, hormones, and genes. Gend Med. 2009;6:76–85.
Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–74.
Crume TL, Ogden L, Daniels S, Hamman RF, Norris JM, Dabelea D. The impact of in utero exposure to diabetes on childhood body mass index growth trajectories: the EPOCH study. J Pediatr. 2011;158:941–6.
Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–97.
Peckins MK, Negriff S, Schneiderman JU, Gordis EB, Susman EJ. The moderating role of cortisol reactivity on the link between maltreatment and body mass index trajectory across adolescence. J Adolesc Health. 2019;65:239–47.
Zhang T, Whelton PK, Xi B, Krousel-Wood M, Bazzano L, He J, et al. Rate of change in body mass index at different ages during childhood and adult obesity risk. Pediatr Obes. 2019;14:e12513.
Min J, Wen X, Xue H, Wang Y. Ethnic disparities in childhood BMI trajectories and obesity and potential causes among 29,250 US children: findings from the early childhood longitudinal study-birth and kindergarten cohorts. Int J Obes. 2018;42:1661–70.
Thomson JL, Tussing-Humphreys LM, Goodman MH, Landry AS. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am J Clin Nutr. 2019;109:127–38.
Cohen JFW, Lehnerd ME, Houser RF, Rimm EB. Dietary approaches to stop hypertension diet, weight status, and blood pressure among children and adolescents: National Health and Nutrition Examination Surveys 2003–2012. J Acad Nutr Diet. 2017;117:1437–44.e2.
Martin-Calvo N, Chavarro JE, Falbe J, Hu FB, Field AE. Adherence to the Mediterranean dietary pattern and BMI change among US adolescents. Int J Obes. 2016;40:1103–8.
DeSalvo KB, Olson R, Casavale KO. Dietary guidelines for Americans. JAMA. 2016;315:457–8.
Psaltopoulou T, Tzanninis S, Ntanasis-Stathopoulos I, Panotopoulos G, Kostopoulou M, Tzanninis IG, et al. Prevention and treatment of childhood and adolescent obesity: a systematic review of meta-analyses. World J Pediatr. 2019;15:350–81.
Oellingrath IM, Svendsen MV, Brantsaeter AL. Tracking of eating patterns and overweight—a follow-up study of Norwegian schoolchildren from middle childhood to early adolescence. Nutr J. 2011;10:106.
Cutler GJ, Flood A, Hannan P, Neumark-Sztainer D. Major patterns of dietary intake in adolescents and their stability over time. J Nutr. 2009;139:323–8.
Ambrosini GL, Emmett PM, Northstone K, Jebb SA. Tracking a dietary pattern associated with increased adiposity in childhood and adolescence. Obesity. 2014;22:458–65.
Mikkilä V, Räsänen L, Raitakari OT, Marniemi J, Pietinen P, Rönnemaa T, et al. Major dietary patterns and cardiovascular risk factors from childhood to adulthood. The Cardiovascular Risk in Young Finns Study. Br J Nutr. 2007;98:218–25.
Langford R, Bonell C, Jones H, Pouliou T, Murphy S, Waters E, et al. The World Health Organization’s Health Promoting Schools framework: a Cochrane systematic review and meta-analysis. BMC Public Health. 2015;15:130.
Luckner H, Moss JR, Gericke CA. Effectiveness of interventions to promote healthy weight in general populations of children and adults: a meta-analysis. Eur J Public Health. 2012;22:491–7.
Gortmaker SL, Long MW, Resch SC, Ward ZJ, Cradock AL, Barrett JL, et al. Cost effectiveness of childhood obesity interventions: evidence and methods for CHOICES. Am J Prev Med. 2015;49:102–11.
Khalil CB, Johnson-Down L, Egeland GM. Emerging obesity and dietary habits among James Bay Cree youth. Public Health Nutr. 2010;13:1829–37.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320:2020–8.
Bekelman TA, Sauder KA, Rockette-Wagner B, Glueck DH, Dabelea D. Sociodemographic predictors of adherence to national diet and physical activity guidelines at age 5 years: the Healthy Start Study. Am J Health Promot. 2021;35:514–24.
Lee H, Kang M, Song WO, Shim JE, Paik HY. Gender analysis in the development and validation of FFQ: a systematic review. Br J Nutr. 2016;115:666–71.
Yoshida Y, Scribner R, Chen L, Broyles S, Phillippi S, Tseng TS. Diet quality and its relationship with central obesity among Mexican Americans: findings from National Health and Nutrition Examination Survey (NHANES) 1999–2012. Public Health Nutr. 2017;20:1193–202.
Sacks FM, Obarzanek E, Windhauser MM, Svetkey LP, Vollmer WM, McCullough M, et al. Rationale and design of the Dietary Approaches to Stop Hypertension trial (DASH). A multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann Epidemiol. 1995;5:108–18.
Golpour-Hamedani S, Mohammadifard N, Khosravi A, Feizi A, Safavi SM. Dietary approaches to stop hypertension diet and obesity: a cross-sectional study of Iranian children and adolescents. ARYA Atheroscler. 2017;13:7–13.
Berz JP, Singer MR, Guo X, Daniels SR, Moore LL. Use of a DASH food group score to predict excess weight gain in adolescent girls in the National Growth and Health Study. Arch Pediatr Adolesc Med. 2011;165:540–6.
Metcalf BS, Hosking J, Jeffery AN, Voss LD, Henley W, Wilkin TJ. Fatness leads to inactivity, but inactivity does not lead to fatness: a longitudinal study in children (EarlyBird 45). Arch Dis Child. 2011;96:942–7.
Ambrosini GL, Huang RC, Mori TA, Hands BP, O’Sullivan TA, de Klerk NH, et al. Dietary patterns and markers for the metabolic syndrome in Australian adolescents. Nutr Metab Cardiovasc Dis. 2010;20:274–83.
Mesirow MS, Welsh JA. Changing beverage consumption patterns have resulted in fewer liquid calories in the diets of US children: National Health and Nutrition Examination Survey 2001–2010. J Acad Nutr Diet. 2015;115:559–66.e4.
Maier JH, Barry R. Associations among physical activity, diet, and obesity measures change during adolescence. J Nutr Metab. 2015;2015:805065.
Chaparro MP, Koupil I, Byberg L. Maternal pre-pregnancy BMI and offspring body composition in young adulthood: the modifying role of offspring sex and birth order. Public Health Nutr. 2017;20:3084–9.
Donnelly JE, Smith BK. Is exercise effective for weight loss with ad libitum diet? Energy balance, compensation, and gender differences. Exerc Sport Sci Rev. 2005;33:169–74.
Funding
T32 DK007658, R01DK068001, R01DK068001, R01GM121081.
Author information
Authors and Affiliations
Contributions
TAB, SLJ, DHG, KAS, and DD conceptualized the project; TAB, BMR, KHH, and DHG analyzed the data; TAB drafted the manuscript. All authors played an important role in interpreting the results, provided substantive feedback on the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bekelman, T.A., Ringham, B.M., Sauder, K.A. et al. Adherence to index-based dietary patterns in childhood and BMI trajectory during the transition to adolescence: the EPOCH study. Int J Obes 45, 2439–2446 (2021). https://doi.org/10.1038/s41366-021-00917-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00917-z
- Springer Nature Limited