Abstract
Background
The goal of this systematic review is to synthesize the published meta-analyses assessing the role of nutritional, behavioral and physical activity factors/interventions on the prevention or treatment of pediatric and adolescent obesity.
Methods
An online search was conducted in PubMed (end-of-search: September 30, 2015); English-language meta-analyses pooling observational and/or interventional studies examining weight-related indices on children and adolescents were included.
Results
Sixty-six meta-analyses corresponding to more than 900,000 children and adolescents were retrieved. The majority of meta-analyses included interventional studies most of which referred to mixed or combined interventions, including components such as diet, physical activity and sedentary behavior reduction. Discrepancies between meta-analyses on observational and interventional studies were noted. Combined interventions including physical activity and nutritional modifications seemed to represent the most effective means for tackling childhood obesity.
Conclusions
Synthesis of interventional or observational evidence may yield discrepant results. The combination of enhanced physical activity and improved nutrition emerged as a promising intervention in the fight against childhood/adolescent obesity. However, further research is needed about the most effective multidimensional prevention strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization, overweight and obesity are defined as the abnormal and the excessive fat accumulation, respectively, that may impair health [1]. A child or adolescent is considered overweight if it is above the 85th percentile and obese if it is above the 95th percentile [2]. Childhood and adolescence obesity has skyrocketed during the latest decades and has become extremely prevalent in the developed world leading to a modern “obesity epidemic” [3]. Four out of ten children in North America, in Europe, and almost three out of ten in the western Pacific were predicted to have abnormally high weight by 2010 [4]. Childhood obesity is associated with various morbidities later in life such as adulthood obesity [5] and diabetes mellitus [6]. The subsequent health consequences [7,8,9] including the increased mortality risk [10] are currently considered among the major public health challenges [2, 7, 11].
To tackle this progressing problem, a great number of trials, meta-analyses and systematic reviews have been published. Many interventions including diet, increase in physical activity and behavioral modifications have been proposed either separately or combined [12, 13]. Given that high quality metaanalyses play a central role in shaping “level A” grades of recommendations [14], the present systematic review focuses especially on the published meta-analyses that summarized observational and/or interventional evidence on nutritional, physical activity and behavioral factors regarding the prevention and/or treatment of childhood and adolescent obesity. Drug interventions were beyond the scope of the present study.
Methods
Search strategy and eligibility of studies
The present systematic review was performed following the guidelines of the PRISMA statement [15]; the PRISMA Checklist is provided as supplementary material. A systematic search was conducted in PubMed (end-of-search: September 30, 2015) using the following search algorithm: (child OR childhood OR children OR adolescent OR adolescents OR puberty OR pubertal) AND (obese OR obesity OR overweight OR “body mass”) AND (diet OR dietary OR nutrition OR nutritional OR eating OR food OR foods OR protein OR proteins OR lipid OR lipids OR fat OR fats OR macronutrient OR macronutrients OR micronutrient OR micronutrients OR vitamin OR vitamins OR milk OR dairy OR fruit OR fruits OR vegetable OR vegetables OR meat OR poultry OR fish OR grain OR grains OR legumes OR juice OR breakfast OR dinner OR water OR alcohol OR beverage OR beverages OR coffee OR tea OR chocolate OR sweet OR sweets OR exercise OR “physical activity” OR sedentary) AND (meta-analysis OR meta-analyses OR “systematic review”). A detailed list of nutritional terms was included due to the anticipated heterogeneity of nutritional terminology that is applied across the studies in contrast to studies regarding physical activity. Studies pertaining exclusively to behavioral changes were anticipated to be included in the search results since the vast majority of behavioral interventions concern either dietary modifications or physical activity or sedentary life interventions. Subsequently, the reference lists of the retrieved articles were searched in a “snowball procedure”, to include further eligible articles in this review.
Inclusion criteria were as follows: (1) the study had to be a meta-analysis published in English language; (2) meta-analyses synthesizing interventional as well as observational studies were deemed eligible; (3) the study subjects or a fraction of them should be children and adolescents according to the age range definition provided by each study separately and there should be a specific subgroup analysis for this age range; (4) if the intervention/exposure was multifactorial, it should include at least a modification of one diet-related or physical activity-related factor. These included also behavioral modifications on parents/children aiming at nutrition/dietary modifications of children, increase in physical activity and sedentary life reduction; (5) the outcome should pertain to the prevention or treatment of obesity [in terms of weight change, body mass index (BMI), Z scores, overweight/obesity status, fat mass reduction, central obesity]. Although we acknowledge the inherent limitations of assessing each of the abovementioned obesity indices separately, we opted to include all the relevant studies to provide a more complete overview of the available evidence and formulate enhanced directions for future research. Proxy outcomes such as eating habits, quantity of meals, etc., were not included; (6) meta-analyses examining surgical or drug-related interventions for obesity were not included. Two reviewers (ST and MK) independently performed the selection of studies; in case of disagreement, final decision was reached by team consensus.
Data extraction and effect estimates
The extraction of data comprised the first author’s name, publication year, description of the population, time frame and eligibility criteria regarding the studies included in each meta-analysis, type and description of the intervention/exposure as well as the corresponding outcomes, number of studies/subjects, and the results of each meta-analysis. Effect estimates yielded by random effects models were preferred over the fixed-effect ones, due to the superiority of the first in accommodating the heterogeneity. Studies describing provision of meals or implementation of specific physical activity programs were referred to as “actual” interventions, whereas studies concerning behavioral or educational interventions were allocated in the corresponding subcategory. Regarding physical activity interventions, “actual” were considered those interventions pertaining to specific exercise programs implementation such as those in the context of the school curriculum, whereas the remaining interventions such as the family-based ones were included in the behavioral and educational groups.
If the required data for the review were not readily available in the published article, the corresponding authors were contacted twice (a reminder e-mail was sent after the first e-mail). Two reviewers (ST and MK) independently performed data abstraction, and, in case of disagreement, final decision was reached by team consensus.
Results
Description of eligible studies
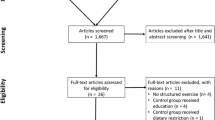
The flowchart describing the subsequent steps of the selection of eligible studies is presented as a Supplementary Fig. 1. Through the algorithm, 933 articles were retrieved, among which 711 were considered irrelevant to the present topic and 154 were relevant but were not meta-analyses. Four studies [16,17,18,19] were excluded due to overlap with more updated articles by the same research teams [20,21,22,23]. In particular, a Cochrane meta-analysis [16] was updated [21] in 2009, a report by Wang et al. [17] overlapped with a newer study by the same team [20], the Cochrane report [18] by Langford et al. overlapped with a newer article [22] and the study by Collins et al. [19] was excluded due to overlap with another more recent study [23] by the same authors. One meta-analysis was excluded due to language [24], one due to insufficient data regarding children and adolescents [25] and another one because it was a letter to the editor [26]. Two corresponding authors replied and provided further data for their studies [27, 28]. After adding five articles from the snowball procedure [29,30,31,32,33], 66 articles were finally included in the review [20,21,22,23, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88].
Dietary factors and interventions (Table 1, Supplementary Table 1)
Meta-analyses including only non-interventional studies
Increased dietary energy density (DED) is a relatively new parameter associated with obesity [89]. It is calculated by dividing total food energy (kJ) by total food weight (g) excluding beverages. A meta-analysis [41] of six cross-sectional studies including 6800 children in the age group of 4–11 years showed a marginal positive correlation between DED and children’s fat mass index (FMI = fat mass in kg/height in m2) [change in FMI = 0.064, 95% confidence interval (CI) 0.01–0.11, P = 0.013]. However, the results became statistically non-significant when they were adjusted for internal and external biases.
The impact of meal frequency on childhood obesity has been the topic of two meta-analyses [28, 46]. Hammons et al. [46] analyzed eight studies with 44,016 children and suggested that having three or more family-shared meals per week reduced the possibility of a child becoming obese by 12% in comparison with those that consumed less than three family meals per week. Similar results came up from Kaisari et al. [28] who investigated the total number of meals/eating episodes consumed on a daily basis on 18,849 children and adolescents. An inverse association between eating frequency and overweight/obesity status emerged, increased eating frequency, as compared with the lowest category, was associated with 22% lower likelihood of being overweight/obese [log(odds ratio) = − 0.24, 95% CI − 0.41 to − 0.06].
Meta-analyses including interventional studies with actual interventions
Two meta-analyses [23, 27] pooling the effects of dietary randomized controlled trials (RCTs) concluded that diet alone could produce significant weight loss and reduce many obesity-related outcomes in children and adolescents. These effects were observed among children above 5 years of age and adolescents. Collins et al. [23] found that these outcomes were not only reduced [standardized mean difference (SMD) = − 1.82, 95% CI − 2.40 to − 1.23, P < 0.001], but also the result could be maintained during the follow-up, to a lesser extent (SMD = − 0.64, 95% CI − 0.89 to − 0.39, P < 0.001). However, some dietary interventions with active components did not achieve statistically significant results [22, 45], others’ results were marginally clinically significant [47] and some meta-analyses had a limited number of included studies to provide a safe conclusion [88].
Meta-analyses including interventional studies with behavioral and/or educational interventions
Nutritional education alone [36] yielded a mean BMI reduction of 0.33 kg/m2 (95% CI − 0.55 to − 0.11) in a meta-analysis including eight RCTs and 8451 participants. Despite that, the majority of dietary behavioral modification studies did not show any statistically significant effect on various weight-related outcomes [40, 44, 48, 80, 83, 84].
Meta-analyses including both interventional and non-interventional studies
Forshee et al. [51] found a very weak association between the sugar-sweetened beverages’ (SSB) consumption and children and adolescents BMI [effect size (ES) = 0.017 kg/m2 change in BMI (95% CI − 0.009 to 0.044) during the time period defined by the study for each serving per day change in SSB consumption]. Another meta-analysis [58] with the same topic indicated that SSBs could cause weight gain: one daily serving of SSBs could lead to a 0.06-unit increase in BMI (95% CI 0.02–0.10) over a year’s period, and a 0.07-unit increase in BMI (95% CI 0.01–0.12) over the time period of each study, whereas replacing SSBs with non-caloric beverages could induce a reduction in BMI of about 0.34 kg/m2 (95% CI − 0.50 to − 0.18). However, another meta-analysis [42] did not find any correlation between dietary sugars and children’s BMI/BMI-Z score.
High frequency of cereal consumption [43] seemed to be associated with lower BMI and BMI-Z scores (ES = − 1.13 units; 95% CI − 0.81 to − 1.46, P < 0.0001) and may halve the possibility of becoming overweight.
Another meta-analysis [71] regarding the efficacy of nutritional school programs and policies including children 4–11 years old did not show any significant results, except for the implementation of the School Breakfast Program according to the Dietary Guidelines for Americans [weighted mean difference (WMD) = − 0.08 (95% CI − 0.14 to − 0.02)]; however, the results suffered from a significant degree of heterogeneity among the pooled studies. Finally, no association was found between dairy product consumption and adiposity-related outcomes in children [76]; nevertheless, an inverse relation appeared (ES = − 0.26, 95% CI − 0.38 to − 0.14, P < 0.0001) in adolescents.
Physical activity-related factors and interventions (Table 2, Supplementary Table 2)
No pure observational meta-analyses were yielded by the search strategy. Regarding interventional approaches, the results are summarized below.
Physical activity: actual interventions
Various exercise intensities and modalities (e.g., aerobic, resistance or a combination of both) have been shown to positively affect body composition [33] by reducing body fat [61, 63, 77] while increasing fat-free mass [59]. Furthermore, body fat percentage was reduced to a greater extent when aerobic activity was combined with resistance exercise (ES = 1.20 ± 0.35, 95% CI 0.34–2.10) than when aerobic activity was implemented alone (ES = 0.58 ± 0.31, 95% CI 0.18–0.90), it was also inversely correlated with the intensity of the program [59] (low intensity ES = 0.97 ± 0.33, 95% CI 0.31–1.90 vs high intensity ES = 0.29 ± 0.10, 95% CI 0.01–0.35). Body fat percentage reduction might be maintained for a significant period of time [60] (ES after 1 year follow-up = 0.84 ± 0.51; 95% CI 0.22–0.94).
Physical activity could often reduce fat mass per se [27, 48, 68, 70] but, on the other hand, the effect on lean mass was not always statistically significant [65, 68, 70, 79]. Physical activity alone often did not have a notable effect on BMI in pediatric and adolescent populations [44, 48, 64, 71, 72, 78]. Only few meta-analyses indicated a significant BMI reduction [22, 57, 79], while others showed that exercise and especially resistance exercise could even increase it [27, 59, 68]. As for absolute body weight, the results were mixed as well. There was absolute weight loss in two meta-analyses [47, 79], whereas some showed that physical activity could cause weight gain [27, 47, 59] especially when resistance training was included [68] and others showed no effect at all [27, 61, 63, 73]. Two meta-analyses referred to waist circumference but the results were not statistically significant [68, 79]. Furthermore, it has to be noted that most of the eligible meta-analyses in this category reported on studies whose participants were above 4 years old; thus the results should be extrapolated with caution to younger ages.
Physical activity: behavioral and/or educational interventions
The meta-analysis of Katz et al. [47] showed diversity between the effects of behavioral interventions targeting increase in physical activity. In populations including both sexes, there was an increase in absolute weight in kilograms (SMD = 1.87, 95% CI 1.31–2.42); in girls’ population, absolute weight slightly fell (SMD = − 0.38, 95% CI − 0.74 to − 0.02), whereas in boys’ population it was not affected significantly (SMD = − 0.14, 95% CI − 0.17 to 0.44). Luckner et al. [45] investigated the effects of exercise-promoting educational interventions in the general population which significantly reduced both BMI (WMD = − 0.15, 95% CI − 0.34 to 0.04) and body fat percentage (WMD = − 0.7, 95% CI − 1.05 to − 0.31) in subjects up to 18 years old. It should be noted, however, that such physical activity interventions based solely on behavioral/educational modification often failed to elicit significant results [40, 83] and, in addition, the number of eligible studies included in some of the meta-analyses was very limited [47, 80, 84].
Combination of physical activity and dietary interventions (Table 3—upper panels, Supplementary Table 3)
Two meta-analyses [32, 59] including participants aged above 5 years found that interventions combining diet and exercise yielded a better outcome when compared to exercise-only interventions or a no-intervention group. However, the same combination was not proven to be superior to diet alone [38]. Resistance training alone or added to diet increased lean body mass over a period of 4 months compared to diet only (pooled difference = 0.44 kg, 95% CI 0.04–0.84), and reduced body fat percentage more, in comparison with diet-only interventions (pooled difference = − 2.73%; 95% CI − 4.38 to − 1.09) [38]. In turn, Clark [27] showed that the combination of diet with resistance and endurance exercise could cause a remarkable decrease in fat mass and in BMI among children older than 5 years and adolescents.
School-based combined interventions were also effective in reducing multiple obesity-related indices [56] (r = 0.128, 95% CI 0.126–0.171, P < 0.001) and especially BMI according to Lavelle et al. [57] (overall BMI reduction = − 0.17 kg/m2, 95% CI − 0.29 to − 0.06, P < 0.001) and Wang et al. [20] (overall BMI reduction = − 0.30 kg/m2, 95% CI − 0.45 to − 0.15). School-based combined interventions also reduced absolute body weight in kilograms [47] in mixed boys’ and girls’ populations (SMD = − 0.29 kg, 95% CI − 0.45 to − 0.14, P = 0.0002).
Combined interventions with or without family participation might reduce multiple obesity-related outcomes such as BMI, percentage of overweight or body fat percentage [48]. The largest effect size was observed in young children between 2 and 8 years old (ES = − 0.70, 95% CI − 1.00 to − 0.40). It has to be noted that among the included studies only this meta-analysis by McGovern et al. provided subgroup analyses according to different age groups (2–8 and 9–18 years old). Interestingly, combined lifestyle interventions produced significant results irrespective of the age group.
School-based behavioral interventions which improved dietary habits and increased physical activity were effective both in preventing weight gain [83] (reduction on BMI/BMI-Z score = − 0.10, 95% CI − 0.17 to − 0.03, P < 0.001) and in causing weight loss [84] (BMI/BMI-Z score reduction = − 1.09 units, 95% CI − 1.84 to − 0.34, P < 0.001). Similar effectiveness in BMI reduction [44] was observed by combining nutritional education and physical exercise in students’ population (SMD = − 0.37 kg/m2, 95% CI − 0.63 to − 0.12, P < 0.01). However, three meta-analyses [22, 40, 73] showed ineffectiveness on BMI alone and another one [71] in BMI-SDS (standard deviation score) reduction by combining the aforementioned interventions.
Combination of physical activity or diet plus another intervention (Table 3—lower panels, Supplementary Table 3)
Three meta-analyses [45, 59, 74] investigated the potential of combining diet or physical activity plus another intervention. LeMura et al. [59], who included parental and family behavioral interventions in addition to exercise among participants older than 4 years, found a significant boost to the body fat percentage reduction compared to the one caused by exercise alone. Luckner et al. [45] examined two combinations, namely education plus physical activity, as well as education plus diet, but neither combination elicited statistically significant difference in BMI and body fat percentage. The combination of sedentary behavior reduction combined with exercise [74] induced mild changes in ΒΜΙ (ES = − 0.089, 95% CI − 0.202 to 0.025, P = 0.125). The pooled results [74] of the combinations of sedentary behavior reduction with either diet or physical activity or both produced an overall BMI reduction of 0.073 kg/m2 (95% CI − 0.135 to − 0.011, P = 0.021).
Sedentary behavior reduction interventions (Table 4, Supplementary Table 4)
The search strategy did not yield any pure observational meta-analyses. Regarding interventional approaches, the reduction of sedentary lifestyle has been purported to aid weight loss and prevent or treat obesity through many direct and indirect ways. Seven meta-analyses [45, 47, 48, 66, 74, 85, 86] with a sedentary behavior reduction arm were identified. Screen time and sitting time reduction [74] did not produce statistically significant reduction in BMI (ES = − 0.154, 95% CI − 0.354 to 0.045, P = 0.129). Another meta-analysis [66] combining multiple behavioral interventions reduced the target population’s BMI by 0.25 kg/m2 (95% CI − 0.40 to − 0.09, P = 0.002). Other meta-analyses [45, 85] indicated a BMI reduction up to 0.89 kg/m2 (95% CI − 1.67 to − 0.11) but absolute body weight [48] was not affected. Finally, reducing screen time specifically in children 4–12 years old did not seem to affect BMI [86]. It should be noted that the included studies reporting on screen time reduction did not provide detailed information about what behaviors were substituted for that time, thus the effect of confounders could not be extensively determined.
Diet, physical activity and a third component: multidimensional interventions (Table 5, Supplementary Table 5)
There were four meta-analyses [45, 56, 74, 80] which provided results of multidimensional interventions (namely three or more interventions) on obesity-related outcomes.
Luckner et al. [45] showed that the combination of physical activity, education and nutrition resulted in a small reduction in BMI in six studies including 10,257 subjects (mean difference = − 0.10, 95% CI − 0.16 to − 0.04), but it did not reduce body fat percentage. Similarly, the combination of physical activity, lifestyle modification and nutrition in the school and after-school intervention programs [56] produced a small positive effect on various weight-related outcomes (r = 0.047, 95% CI 0.023–0.070, P < 0.001) in children and adolescents up to 19 years old. No effect was observed [74] by the combination of sedentary behavior reduction, physical exercise and nutrition.
Lastly, physical exercise combined with diet and behavioral therapy [80] reduced BMI-Z score in eleven studies with 1015 children 3–8 years old by 0.25 BMI-Z score units (95% CI − 0.36 to − 0.14) but the heterogeneity was high (I2 = 100%), and, thus, the reliability of the results is rather questionable, taking into consideration the limitations of BMI use in young ages.
Meta-analyses collectively reporting on “any” type of interventions (Supplementary Table 6)
Meta-analyses collectively reporting on school-based interventions
Many mixed interventions were organized within a school environment. A meta-analysis [30] of nineteen RCTs including 9302 children showed that school-based interventions with dietary and/or physical activity components could reduce the incidence of obesity by 26%, while classroom activities and physical education by 27%. Mixed programs conducted both during and after school hours [56] were associated with very small reductions in various weight-related outcomes, but they were all statistically significant. School-based obesity prevention [29] and treatment [57] programs managed to lower BMI and BMI-Z scores in 31,059 students and in 36,579 students, respectively. Educational programs [37] reduced waist circumference by 3.21 cm (95% CI − 6.34 to − 0.07) and BMI by 0.86 kg/m2 (95% CI − 1.59 to − 0.14). Other mixed multi-interventional studies were only mildly effective [55] in obesity prevention or not effective at all [52, 82] in reducing indices such as BMI. However, these results should be interpreted with caution due to the inherent limitations of using BMI among children and adolescents. School nutritional education plus physical activity [73] failed to reach statistical significance in a large meta-analysis with 47 studies and 41,634 participants.
Meta-analyses collectively reporting on behavioral or/and educational interventions
Two meta-analyses [83, 84] conducted by Peirson et al. had multiple behavioral modification arms. Such modifications such as diet, exercise, social support or lifestyle strategies, alone or in combination [83], resulted in a small-scale reduction in BMI/BMI-Z score in 56,342 children and adolescents (ES = − 0.07, 95% CI − 0.10 to − 0.03), in BMI alone (ES = − 0.09 kg/m2, 95% CI − 0.16 to − 0.03) and in the prevalence of overweight and obesity (relative risk = 0.94, 95% CI 0.89–0.99). The meta-analysis of behavioral treatment of obesity [84] yielded clinically greater results. The overall reduction of BMI/BMI-Z score reached 0.54 units (95% CI − 0.73 to − 0.36).
Joint analyses of studies assessing nutritional education combined with either behavioral therapy or physical activity education provided as a very low-intensity intervention [80] did not seem to affect BMI-Z score in overweight/obese young children aged 3–8 years. On the other hand, lifestyle modification [53] did reduce various obesity-related outcomes in older overweight/obese children and adolescents up to 19 years old.
Active behavioral interventions [31] yielded positive effects in all comparisons versus the control or education-only groups. In the same way, combinations of behavioral modification with additional components [62] such as cognitive ones or parental participation were better than behavioral interventions without additional components. Furthermore, mixed behavioral interventions [87] were effective against obesity when parents were also participants, even optionally (WMD = 0.30, SE = 0.11, P = 0.027).
A collective analysis on various modalities of family behavioral treatment [50] indicated mild reductions in various weight-related outcomes among children 5–12 years old. Solely educational interventions [45] did induce BMI reduction in 5667 children 0–18 years old (ES = − 0.18 kg/m2, 95% CI − 0.30 to − 0.05), but they did not affect body fat percentage (ES = 0.13, 95% CI − 0.04 to + 0.3).
Meta-analyses collectively reporting on “lifestyle” interventions without further specification
A Cochrane meta-analysis [21] pooled the results of seventeen RCTs including 5230 children regarding the effects of various lifestyle interventions on BMI or BMI-SDS). The intervention groups showed greater reductions than the control ones in almost all measurements conducted both after 6 and 12 months of follow-up.
Another Cochrane meta-analysis [75] including only a few studies with lifestyle modifications did not affect obesity in children between 3 and 18 years old.
A larger scale meta-analysis [54] of thirty-seven studies with 27,946 children up to 18 years old underscored this protective effect of lifestyle programs on BMI/BMI-Z score (SMD = − 0.15 kg/m2, 95% CI − 0.21 to − 0.09).
A collective analysis on various “lifestyle” interventions [49] suggested that they could effectively cause weight loss in kilograms (ES = − 0.95, 95% CI − 0.79 to − 1.11) in middle-school/pre-teen children younger than 16 years old and reduce BMI [69] by − 0.08 kg/m2 (95% CI − 0.16 to − 0.01, P = 0.02). However, effectiveness was not observed in older children and teenagers [39], but we should note that in this study participants were aged up to 22 years old that poses limitations in the interpretation of the results.
A meta-analysis [34] specifically targeting US (United States) minority children aged 6–19 years old did not reveal any effectiveness of one-component or multiple component interventions.
Discussion
Addressing separately interventional and non-interventional evidence, this systematic review highlights the discrepancies between meta-analyses pooling these two types of studies. Indeed, this notion has been the base of a vivid debate in the field of childhood obesity epidemiology [90]. Among the factors and interventions that were examined in the published meta-analyses, the combination of enhanced physical activity and improved nutrition emerged as a promising, effective intervention against childhood/adolescent obesity. A variety of multidimensional interventions have also been examined in the literature, nevertheless, the optimal scheme remains to be shaped in the future.
The combination of physical activity and diet was proven an effective tool against obesity regarding both prevention [83] and treatment [84], according to evidence stemming from interventional studies. It was commonly implemented within school settings in the synthesized meta-analyses [20, 47, 56, 57]. This combination may improve numerous metabolic outcomes, causing mild weight loss [38, 91], preserving lean mass and protecting from weight regain that may appear when diet is implemented alone [92]. When the intervention targeting physical activity and diet was based on a behavioral approach, the findings of relevant meta-analyses were rather conflicting with protective [44, 83, 84] or neutral results [22, 40, 71, 73]. On the other hand, results derived from combining physical exercise or diet with a second component like education or sedentary behavior reduction were associated with smaller effect sizes [45, 59, 74].
Adding a third component to the combination of physical activity and diet generated significant results in some weight-related indices [45, 56, 74, 80], but effect sizes were often small. The explanation may be small number of included studies in the subgroup analyses [45, 80], high degree of heterogeneity [45, 80] and lack of methodological rigor [56]. Therefore, the optimal combination that would further boost the effectiveness remains an issue under investigation.
Interesting nutritional aspects associated with childhood obesity emerged from our review. Regarding interventional meta-analyses with actual dietary interventions, there were conflicting results; since some [23, 27] found significant and durable positive effect on weight-related indices, but others did not [22, 45]. Dietary behavioral modification did not seem to have any effect on obesity-related outcomes [40, 44, 48, 80, 83, 84]. This may be due to methodological issues regarding the length of follow-up, characteristics of the target population and the intensity [40, 48] of the intervention, as well as the subjects’ compliance [44].
When interventional studies were pooled with non-interventional ones, the findings should be examined critically. Forshee et al. published a meta-analysis [51] which found that SSBs had almost no effect on BMI of children and adolescents. This study was challenged [26, 93] on the ground that it had not taken into account the amount of calories of the SSBs and the phenomenon of underreporting. Α similar meta-analysis [58] clearly indicated their replacement with non-SSBs results in weight loss. Interestingly, dietary sugars per se showed no effect on children’s BMI and BMI-Z score according to a synthesis of interventional and non-interventional studies [42]. Milk and dairy product consumption was effective only in adolescent populations regarding the reduction in BMI/BMI-Z scores, and this was attributed to the molecular ingredients of milk as well as methodological issues [76]. Cereals consumed in breakfast may affect body weight by increasing energy expenditure through the day and reducing appetite, but it should be noted that the large number of included observational studies prevents the establishment of a causational relation and gives ground to many forms of bias [43].
Regarding meta-analyses on non-interventional studies, two of them [28, 46] found an inverse association between the frequency of family-shared meals and the risk of obesity. Overall, families that ate five or more meals together had children who were 25% less likely to encounter nutritional issues than children who ate only one meal with their families [46], while increased eating frequency was associated a 24% lower likelihood of being overweight/obese [28]. This phenomenon may be explained by the fact that such persons are more likely to develop healthy eating behaviors [94]. Observational studies regarding dietary energy density showed a positive association with weight gain; nevertheless, the effect of external and internal bias was considerable [41].
An interesting remark on the topic of nutritional meta-analyses would be that many interventional studies did not reach either clinical or statistical significance in their results; however, observational studies had much more prominent effects. This phenomenon has been underscored in terms of the effectiveness of breakfast in obesity-related indices [90]. In this context, an ongoing debate about the reliability of results of non-interventional studies, compared to those of interventional ones, has been triggered.
No observational studies were found regarding the impact of physical activity on obesity-related outcomes. As for interventional studies, physical activity seems to be mildly to highly effective in improving body composition [33], especially resistance exercise, by reducing body fat [48, 59, 70] and simultaneously increasing lean mass [59]. A direct effect of the latter is that BMI and body weight may not be affected by PA or they can even increase [27, 68]. Nonetheless, a considerable number of actual interventional studies and/or part of their subgroup analyses did not manage to prove the effectiveness of physical activity [40, 44, 61, 64, 65, 68, 71, 73, 78]. Similarly, indirect increase of physical activity through purely educational and behavioral interventions did not produce significant results either [40, 83]. Several reasons may pertain to this, such as RCTs of severely low methodological quality included in the meta-analyses [40], high level of heterogeneity [45, 47], limited number of studies available [80], mixed populations of overweight/obese and non-overweight children and adolescents [83], as well as inadequate description of the interventions [40]. Finally, it should be highlighted that other reviews [95,96,97], as well as a review of meta-analyses [98] about physical activity in childhood obesity, have shown similar results.
Sedentary lifestyle has been positively correlated with body fatness in young people by both reducing energy expenditure and increasing energy intake [47]. Indeed, several meta-analyses showed a reduction in BMI via sedentary behavior reduction interventions [45, 66, 85], but the effects were rather limited. Also, some others did not produce a significant effect [48, 74, 86].
It is noticeable that there were numerous meta-analyses which presented interventions and outcomes regarding “any” type of interventions collectively. Longer duration [23, 30, 47, 55] and better structure [49] seemed to augment their effectiveness, as well as parental participation [87]. On the other hand, the heterogeneity and the various conditions, under which the interventions were organized, provided different results, many of which were not statistically significant [30, 34, 39, 52, 62, 82]. From a methodological point of view, many of these meta-analyses presented a pooled effectiveness of various interventions grouped together, assessing an overall performance; this is a rather crude approach which does not allow the comparative evaluation of the heterogeneous group of adopted interventions. Other methodological concerns were conduction of completers’ analyses instead of intention-to-treat analyses [31], lack of clear description of the intervention [80], unclear assessment of risk of bias [83] and very high heterogeneity [84].
Such collective analyses of various interventional programs were very frequent in school-based studies, as it is easier to try multiple interventions within a school setting [47, 55]. Despite their popularity and anticipated effectiveness, however, aspects such as study type, duration, intervention type, number of intervention components and cost-efficacy need to be taken into account during the planning and structuring of such meta-analyses. In these terms, several school-based studies did not elicit either statistically [52, 73] or clinically [29, 56] significant results, especially in their subgroup analyses. The ideal combination of interventions to be implemented in school-based settings remains elusive.
Purely behavioral and educational interventions also had mixed results, either significant [50, 53, 62, 87] or marginally significant [45, 80, 83, 84]. However, this should not discourage their possible assessment because control groups receiving no intervention at all presented with gain weight and BMI increase [31].
Meta-analyses were exclusively used in our qualitative analysis since their results are considered to constitute highly reliable pieces of evidence [99]. Guidelines by various Expert Panels, have been issued; these guidelines have highlighted a variety of effective points in the prevention of childhood obesity, such as eating more frequently, including parents in the intervention programs, increasing exercise, decreasing caloric intake and decreasing screen time [100,101,102,103]. However, the strict adherence of participants to the intervention programs represents a major obstacle regarding their effective implementation.
The search strategy included a variety of possible ways of fighting childhood and adolescent obesity. However, methodological concerns and possible publication bias should be kept in mind. Moreover, some meta-analyses included several subgroup analyses based on a limited number of studies. It should be also highlighted that subgroup analyses according to the age of the participants were not universally available in the included meta-analyses; therefore, this aspect should be addressed in future studies to reveal potential differentiations in the outcomes and determine the most effective, age-adapted interventions. Furthermore, a very commonly used outcome, namely BMI, is not always reliable in pediatric populations, as well as in tall and thin persons and those with high percentage of muscle mass, since it does not precisely reflect body composition [87]. Children and adolescents can have rapid changes in linear growth and, thus, changes in BMI cannot be safely attributed exclusively to an implicated external parameter. Therefore, studies should ideally report also results regarding the percentage change of body fat to provide a more robust description of the effects of the implemented intervention. Thus, the interpretation and generalization of the reported outcomes restricted to BMI should be extremely cautious.
In conclusion, synthesis of interventional or observational evidence may provide different results. Our findings confirm that the combination of increased physical activity and improved nutrition are currently utilized mainstream interventions against childhood/adolescent obesity. However, further research is needed to identify the most effective age-specific multi-dimensional prevention strategy.
References
World Health Organisation. Obesity and overweight. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 16 Feb 2018.
Centers for Disease Control and Prevention. Basics about childhood obesity. 2012. https://www.cdc.gov/obesity/childhood/defining.html Accessed 16 Feb 2018.
Zwiauer KF. Prevention and treatment of overweight and obesity in children and adolescents. Eur J Pediatr. 2000;159(Suppl 1):S56–68.
Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370:403–11.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: asystematic review. Maturitas. 2011;70:266–84.
Psaltopoulou T, Ilias I, Alevizaki M. The role of diet and lifestyle in primary, secondary, and tertiary diabetes prevention: a review of meta-analyses. Rev Diabet Stud. 2010;7:26–35.
Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet. 2010;375:1737–48.
Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–93.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82.
Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–37.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14.
Osei-Assibey G, Dick S, Macdiarmid J, Semple S, Reilly JJ, Ellaway A, et al. The influence of the food environment on overweight and obesity in young children: a systematic review. BMJ Open. 2012;2:e001538.
Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–6.
Panic N, Leoncini E, de Belvis G, Ricciardi W, Boccia S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS ONE. 2013;8:e83138.
Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;3:CD001871.
Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, et al. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Jun Report No: 13-EHC081-EF.
Langford R, Bonell CP, Jones HE, Pouliou T, Murphy SM, Waters E, et al. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst Rev. 2014;4:CD008958.
Collins CE, Warren J, Neve M, McCoy P, Stokes BJ. Measuring effectiveness of dietetic interventions in child obesity: a systematic review of randomized trials. Arch Pediatr Adolesc Med. 2006;160:906–22.
Wang Y, Cai L, Wu Y, Wilson RF, Weston C, Fawole O, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16:547–65.
Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;1:CD001872.
Langford R, Bonell C, Jones H, Pouliou T, Murphy S, Waters E, et al. The World Health Organization's Health Promoting Schools framework: a Cochrane systematic review and meta-analysis. BMC Public Health. 2015;15:130.
Collins CE, Warren JM, Neve M, McCoy P, Stokes B. Systematic review of interventions in the management of overweight and obese children which include a dietary component. Int J Evid Based Healthc. 2007;5:2–53.
Yang GP, Wang YR, Zuo SY, Zeng XM. Meta-analysis of intervention effects on obesity in Chinese pupils. Zhonghua Yu Fang Yi Xue Za Zhi. 2011;45:944–8 (in Chinese).
Hooper L, Abdelhamid A, Moore HJ, Douthwaite W, Skeaff CM, Summerbell CD. Effect of reducing total fat intake on body weight: systematic review and meta-analysis of randomised controlled trials and cohort studies. BMJ. 2012;345:e7666.
Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. Am J Clin Nutr. 2009;89:438–9.
Clark JE. Does the type intervention method really matter for combating childhood obesity? A systematic review and meta-analysis. J Sports Med Phys Fitness. 2015;55:1524–43.
Kaisari P, Yannakoulia M, Panagiotakos DB. Eating frequency and overweight and obesity in children and adolescents: a meta-analysis. Pediatrics. 2013;131:958–67.
Cook-Cottone C, Casey CM, Feeley TH, Baran J. A meta-analytic review of obesity prevention in the schools: 1997–2008. Psychol Schools. 2009;46:695–719.
Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37:418–27.
Wilfley DE, Tibbs TL, Van Buren DJ, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychol. 2007;26:521–32.
Epstein LH, Goldfield GS. Physical activity in the treatment of childhood overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(Suppl 11):S553–9.
Beets MW, Beighle A, Erwin HE, Huberty JL. After-school program impact on physical activity and fitness: a meta-analysis. Am J Prev Med. 2009;36:527–37.
Seo DC, Sa J. A meta-analysis of obesity interventions among US minority children. J Adolesc Health. 2010;46:309–23.
Ho M, Garnett SP, Baur L, Burrows T, Stewart L, Neve M, et al. Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics. 2012;130:e1647–71.
Silveira JA, Taddei JA, Guerra PH, Nobre MR. The effect of participation in school-based nutrition education interventions on body mass index: a meta-analysis of randomized controlled community trials. Prev Med. 2013;56:237–43.
Sbruzzi G, Eibel B, Barbiero SM, Petkowicz RO, Ribeiro RA, Cesa CC, et al. Educational interventions in childhood obesity: a systematic review with meta-analysis of randomized clinical trials. Prev Med. 2013;56:254–64.
Ho M, Garnett SP, Baur LA, Burrows T, Stewart L, Neve M, et al. Impact of dietary and exercise interventions on weight change and metabolic outcomes in obese children and adolescents: a systematic review and meta-analysis of randomized trials. JAMA Pediatr. 2013;167:759–68.
Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006;132:667–91.
Kamath CC, Vickers KS, Ehrlich A, McGovern L, Johnson J, Singhal V, et al. Clinical review: behavioral interventions to prevent childhood obesity: a systematic review and metaanalyses of randomized trials. J Clin Endocrinol Metab. 2008;93:4606–15.
Wilks DC, Mander AP, Jebb SA, Thompson SG, Sharp SJ, Turner RM, et al. Dietary energy density and adiposity: employing bias adjustments in a meta-analysis of prospective studies. BMC Public Health. 2011;11:48.
Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2012;346:e7492.
de la Hunty A, Gibson S, Ashwell M. Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obes Facts. 2013;6:70–85.
Friedrich RR, Schuch I, Wagner MB. Effect of interventions on the body mass index of school-age students. Rev Saude Publica. 2012;46:551–60.
Luckner H, Moss JR, Gericke CA. Effectiveness of interventions to promote healthy weight in general populations of children and adults: a meta-analysis. Eur J Public Health. 2012;22:491–7.
Hammons AJ, Fiese BH. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics. 2011;127:e1565–74.
Katz DL, O'Connell M, Njike VY, Yeh MC, Nawaz H. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis. Int J Obes (Lond). 2008;32:1780–9.
McGovern L, Johnson JN, Paulo R, Hettinger A, Singhal V, Kamath C, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93:4600–5.
Snethen JA, Broome ME, Cashin SE. Effective weight loss for overweight children: a meta-analysis of intervention studies. J Pediatr Nurs. 2006;21:45–56.
Young KM, Northern JJ, Lister KM, Drummond JA, O'Brien WH. A meta-analysis of family-behavioral weight-loss treatments for children. Clin Psychol Rev. 2007;27:240–9.
Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. Am J Clin Nutr. 2008;87:1662–711.
Kanekar A, Sharma M. Meta-analysis of school-based childhood obesity interventions in the UK and US. Int Q Community Health Educ. 2008;29:241–56.
Kitzmann KM, Dalton WT 3rd, Stanley CM, Beech BM, Reeves TP, Buscemi J, et al. Lifestyle interventions for youth who are overweight: a meta-analytic review. Health Psychol. 2010;29:91–101.
Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:CD001871.
Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity (Silver Spring). 2013;21:2422–8.
Vasques C, Magalhaes P, Cortinhas A, Mota P, Leitao J, Lopes VP. Effects of intervention programs on child and adolescent BMI: ameta-analysis study. J Phys Act Health. 2014;11:426–44.
Lavelle HV, Mackay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf). 2012;34:360–9.
Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–102.
LeMura LM, Maziekas MT. Factors that alter body fat, body mass, and fat-free mass in pediatric obesity. Med Sci Sports Exerc. 2002;34:487–96.
Maziekas MT, LeMura LM, Stoddard NM, Kaercher S, Martucci T. Follow up exercise studies in paediatric obesity: implications for long term effectiveness. Br J Sports Med. 2003;37:425–9.
Atlantis E, Barnes EH, Singh MA. Efficacy of exercise for treating overweight in children and adolescents: a systematic review. Int J Obes (Lond). 2006;30:1027–40.
Gilles A, Cassano M, Shepherd EJ, Higgins D, Hecker JE, Nangle DW. Comparing active pediatric obesity treatments using meta-analysis. J Clin Child Adolesc Psychol. 2008;37:886–92.
Kelley GA, Kelley KS. Effects of aerobic exercise on non-high-density lipoprotein cholesterol in children and adolescents: a meta-analysis of randomized controlled trials. Prog Cardiovasc Nurs. 2008;23:128–32.
Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009;180:719–26.
Wilks DC, Sharp SJ, Ekelund U, Thompson SG, Mander AP, Turner RM, et al. Objectively measured physical activity and fat mass in children: a bias-adjusted meta-analysis of prospective studies. PLoS ONE. 2011;6:e17205.
van Grieken A, Ezendam NP, Paulis WD, van der Wouden JC, Raat H. Primary prevention of overweight in children and adolescents: a meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int J Behav Nutr Phys Act. 2012;9:61.
Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2:CD007651.
Schranz N, Tomkinson G, Olds T. What is the effect of resistance training on the strength, body composition and psychosocial status of overweight and obese children and adolescents? A systematic review and meta-analysis. Sports Med. 2013;43:893–907.
Dellert JC, Johnson P. Interventions with children and parents to improve physical activity and body mass index: a meta-analysis. Am J Health Promot. 2014;28:259–67.
Nogueira RC, Weeks BK, Beck BR. Exercise to improve pediatric bone and fat: a systematic review and meta-analysis. Med Sci Sports Exerc. 2014;46:610–21.
Williams AJ, Henley WE, Williams CA, Hurst AJ, Logan S, Wyatt KM. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int J Behav Nutr Phys Act. 2013;10:101.
Guerra PH, Nobre MR, Silveira JA, Taddei JA. The effect of school-based physical activity interventions on body mass index: a meta-analysis of randomized trials. Clinics (Sao Paulo). 2013;68:1263–73.
Guerra PH, Nobre MR, da Silveira JA, Taddei JA. School-based physical activity and nutritional education interventions on body mass index: a meta-analysis of randomised community trials-project PANE. Prev Med. 2014;61:81–9.
Liao Y, Liao J, Durand CP, Dunton GF. Which type of sedentary behaviour intervention is more effective at reducing body mass index in children? A meta-analytic review. Obes Rev. 2014;15:159–68.
Martin A, Saunders DH, Shenkin SD, Sproule J. Lifestyle intervention for improving school achievement in overweight or obese children and adolescents. Cochrane Database Syst Rev. 2014;3:CD09728.
Dror DK. Dairy consumption and pre-school, school-age and adolescent obesity in developed countries: a systematic review and meta-analysis. Obes Rev. 2014;15:516–27.
Garcia-Hermoso A, Saavedra JM, Escalante Y, Sanchez-Lopez M, Martinez-Vizcaino V. Endocrinology and Adolescence: aerobic exercise reduces insulin resistance markers in obese youth: a meta-analysis of randomized controlled trials. Eur J Endocrinol. 2014;171:R163–R171.
Cesa CC, Sbruzzi G, Ribeiro RA, Barbiero SM, de Oliveira Petkowicz R, Eibel B, et al. Physical activity and cardiovascular risk factors in children: meta-analysis of randomized clinical trials. Prev Med. 2014;69:54–62.
Kelley GA, Kelley KS, Pate RR. Effects of exercise on BMI z-score in overweight and obese children and adolescents: a systematic review with meta-analysis. BMC Pediatr. 2014;14:225.
van Hoek E, Feskens EJ, Bouwman LI, Janse AJ. Effective interventions in overweight or obese young children: systematic review and meta-analysis. Child Obes. 2014;10:448–60.
Brown T, Smith S, Bhopal R, Kasim A, Summerbell C. Diet and physical activity interventions to prevent or treat obesity in South Asian children and adults: a systematic review and meta-analysis. Int J Environ Res Public Health. 2015;12:566–94.
Hung LS, Tidwell DK, Hall ME, Lee ML, Briley CA, Hunt BP. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr Res. 2015;35:229–40.
Peirson L, Fitzpatrick-Lewis D, Morrison K, Ciliska D, Kenny M, Usman Ali M, et al. Prevention of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ Open. 2015;3:E23–33.
Peirson L, Fitzpatrick-Lewis D, Morrison K, Warren R, Usman Ali M, Raina P. Treatment of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ Open. 2015;3:E35–46.
Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98.
Wahi G, Parkin PC, Beyene J, Uleryk EM, Birken CS. Effectiveness of interventions aimed at reducing screen time in children: a systematic review and meta-analysis of randomized controlled trials. Arch Pediatr Adolesc Med. 2011;165:979–86.
Niemeier BS, Hektner JM, Enger KB. Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Prev Med. 2012;55:3–13.
Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell CD, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev. 2015;8:11834.
Pérez-Escamilla R, Obbagy JE, Altman JM, Essery EV, McGrane MM, Wong YP, et al. Dietary energy density and body weight in adults and children: a systematic review. J Acad Nutr Diet. 2012;112:671–84.
Brown AW, Bohan Brown MM, Allison DB. Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am J Clin Nutr. 2013;98:1298–308.
Roberts CK. Combined diet and exercise interventions can improve metabolic outcomes in obese children, even with only small changes in weight. Evid Based Med. 2014;19:e9.
Kaluski DN, Meir C, Rotem N, Zadka P. Sources of nutritional data in Israel. Public Health Rev. 1998;26:73–7.
Bes-Rastrollo M, Martinez-Gonzalez MA. Differential underreporting and other caveats about sugar-sweetened beverages and weight gain. Am J Clin Nutr. 2008;88:1450–1.
Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. J Am Diet Assoc. 2007;107:1502–10.
Tsiros MD, Sinn N, Coates AM, Howe PR, Buckley JD. Treatment of adolescent overweight and obesity. Eur J Pediatr. 2008;167:9–16.
Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40.
Benson AC, Torode ME, Fiatarone Singh MA. Effects of resistance training on metabolic fitness in children and adolescents: a systematic review. Obes Rev. 2008;9:43–66.
Kelley GA, Kelley KS. Effects of exercise in the treatment of overweight and obese children and adolescents: a systematic review of meta-analyses. J Obes. 2013;2013:783103.
Guyatt GH, Haynes RB, Jaeschke RZ, Cook DJ, Green L, Naylor CD, et al. Users' Guides to the Medical Literature: XXV Evidence-based medicine: principles for applying the Users' Guides to patient care Evidence-Based Medicine Working Group. JAMA. 2000;284:1290–6.
American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 10th ed. Baltimore: Lippincott, Williams and Wilkins; 2017.
Committee on Obesity Prevention Policies for Young Children. Early childhood obesity prevention policies. Washington: The National Academies Press; 2011.
Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92.
Speiser PW, Rudolf MC, Anhalt H, Camacho-Hubner C, Chiarelli F, Eliakim A, et al. Childhood obesity. J Clin Endocrinol Metab. 2005;90:1871–87.
Acknowledgements
The authors would like to thank the authors of studies who replied to our letters, as detailed in the Methods section.
Funding
None.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the concept and design, acquisition and interpretation of data, drafting the article and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical approval
Not needed.
Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Psaltopoulou, T., Tzanninis, S., Ntanasis-Stathopoulos, I. et al. Prevention and treatment of childhood and adolescent obesity: a systematic review of meta-analyses. World J Pediatr 15, 350–381 (2019). https://doi.org/10.1007/s12519-019-00266-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-019-00266-y