Abstract
Background
Intestinal microbiota have been suggested to play an important role in the pathogenesis of obesity and type 2 diabetes. Bariatric surgery improves both conditions and has been associated with changes in intestinal microbiota composition. We investigated the effect of a nonsurgical bariatric technique on intestinal microbiota composition in relation to metabolic improvement.
Methods
Seventeen patients with obesity and type 2 diabetes were treated with the nonsurgical duodenal–jejunal bypass liner, which excludes the proximal 60 cm small intestine from food. Fecal samples as well as metabolic parameters reflecting obesity and type 2 diabetes were obtained from the patients at baseline, after 6 months with the device in situ, and 6 months after explantation.
Results
After 6 months of treatment, both obesity and type 2 diabetes had improved with a decrease in weight from 106.1 [99.4–123.5] to 97.4 [89.4–114.0] kg and a decrease in HbA1c from 8.5% [7.6–9.2] to 7.2% [6.3–8.1] (both p < 0.05). This was paralleled by an increased abundance of typical small intestinal bacteria such as Proteobacteria, Veillonella, and Lactobacillus spp. in feces. After removal of the duodenal–jejunal bypass liner, fecal microbiota composition was similar to that observed at baseline, despite persistent weight loss.
Conclusion
Improvement of obesity and type 2 diabetes after exclusion of the proximal 60 cm small intestine by treatment with a nonsurgical duodenal–jejunal bypass liner may be promoted by changes in fecal microbiota composition.
Similar content being viewed by others
Introduction
The human gastrointestinal tract is inhabited by an enormous number and diversity of mainly anaerobic microorganisms, referred to as the intestinal microbiota [1]. The collective genome of our intestinal microbiota, the intestinal metagenome, exceeds the human genome by a magnitude of more than 100 [2]. Recent evidence suggests that the intestinal microbiota play an important role in the pathogenesis of obesity and type 2 diabetes [3,4,5]. Following the observation that lean germ-free mice did not gain weight on a high-fat diet, it was reported that colonization of these sterile mice with intestinal microbiota from obese mice led to body fat increases and insulin resistance, while this was not observed after colonization with the microbiota from lean donor mice [6,7,8]. Furthermore, both genetically and diet-induced obese mice carried a different intestinal microbiota composition compared to lean controls. In addition, obesity was associated with an increased ratio of the two most dominant phyla within the gut microbiota, the Firmicutes and the Bacteroidetes [9, 10]. It has been suggested that in these preclinical models, an increased capacity of the ‘obese microbiota’ to harvest energy from ingested food and to facilitate storage of these calories in host adipose tissue could explain the association between gut microbiota composition and the development of obesity and possibly type 2 diabetes [6, 7].
Although the gut microbiota, metabolic rate, and dietary habits of humans and mice show large differences [11], some observations made in mice could be partly reproduced in human studies. In particular, it was observed that an unusual gut microbiota composition was associated with obesity [9, 12,13,14]. In addition, changes in microbiota composition have been found to be related to weight loss [13, 15,16,17]. In line with these findings, bariatric surgery, the most durable obesity and type 2 diabetes treatment, has also been associated with changes in microbiota composition [18,19,20]. Moreover, two studies have shown that fecal transplantation of intestinal microbiota from lean donors into obese human subjects transiently increases insulin sensitivity without affecting body weight [21, 22]. A specific fiber treatment that affected the intestinal microbiota was also shown to improve insulin resistance [23]. These data indicate that intestinal microbiota might promote the development of obesity and type 2 diabetes in humans as well. Since both obesity and the metabolic syndrome have been shown to improve after implantation of the duodenal–jejunal bypass liner (DJBL, GI Dynamics, Boston, MA), a nonsurgical bariatric device excluding the proximal part of the small intestine [24,25,26,27], we investigated intestinal microbiota composition in relation to metabolic changes induced by the DJBL.
Methods
Study design
Seventeen subjects were studied before and during DJBL treatment. Additionally, six patients were studied 6 months after removal of the DJBL. In eight patients, the device was explanted after 6 months; in nine patients, explantation was conducted after 12 months, as previously described [24]. At each time point (prior to DJBL (B), 6 months after initiation of DJBL treatment (6M), and 6 months after explantation (6MPE)), body weight was determined and venous blood samples were obtained in the outpatient clinic. Plasma levels of HbA1c, glucose, and insulin were determined routinely at the Department of Clinical Chemistry. In addition, a standardized meal tolerance test was performed: blood samples were drawn after an overnight fast; thereafter a standard liquid meal (Ensure Plus, Abbott Laboratories, IL; 333 mL, 500 kcal, 20.8 g protein, 67.3 g carbohydrates, and 16.4 g fat) was consumed, followed by collection of blood samples in EDTA with aprotinin at up to 240 min postprandially. Samples were immediately cooled, centrifuged, and stored at −80 °C until further analysis. Fecal samples were collected within 24 h prior to the visits and were kept refrigerated until arrival at the outpatient clinic where the samples were immediately stored at −20 °C until further analysis. Throughout the study, subjects were prescribed a diet with a maximum of 1200 kcal for women and 1500 kcal for men.
Subjects
Subjects were treated with the DJBL at the Maastricht University Medical Center, Maastricht or the Zuyderland Medical Centre, Heerlen, the Netherlands. Inclusion criteria were: age between 18 and 65 years; body mass index (BMI) between 30 and 50 kg/m2; duration of type 2 diabetes <10 years. Main exclusion criteria were: use of weight loss medication or anti-inflammatory drugs; history of inflammatory diseases; exclusion criteria regarding safety of DJBL placement or DJBL compatibility. The study was approved by the Medical Ethics Committee of both centers and conducted according to the revised version of the Declaration of Helsinki (October 2008, Seoul). Written informed consent was obtained from every patient before study participation.
DJBL procedure
The DJBL is a 60-cm long impermeable liner which has been developed to mimic the intestinal bypass component of the Roux-en-Y gastric bypass (RYGB) in a nonsurgical way. The DJBL was delivered and retrieved endoscopically as previously described [24]. In brief, a gastroduodenal endoscopy was performed under general anesthesia. A guide wire was placed into the duodenum over which the encapsulated DJBL was directed through the pylorus into the duodenal bulb. The DJBL was advanced into the small intestine, followed by deployment of the anchor in the duodenal bulb. Correct positioning and patency of the DJBL were verified under fluoroscopy. Explantation was performed endoscopically under general anesthesia using a custom retrieval system containing a grasper and a retrieval hood. By grasping the wires on the anchor, the anchor collapsed and was pulled into the retrieval hood on top of the endoscope. After verification of the collapsed anchor by fluoroscopy, the device was removed.
Fecal microbiota profiling
DNA was isolated as previously described [28] and the intestinal microbiota composition was determined using the Human Intestinal Tract chip (HITChip), a phylogenetic DNA microarray containing over 5000 probes based on 16S rRNA gene sequences of over 1100 intestinal bacterial phylotypes. This microarray has been extensively used for the study of the microbiota in different conditions, including obesity and related diseases [12, 21], and it identifies both variation and relative quantity of the human intestinal tract communities [29]. Hybridizations were performed in duplicate with samples labeled with Cy3 and Cy5 dyes. Slides were scanned and the data were extracted from the microarray images using the Agilent Feature Extraction software, version 10.7.3.1 (http://www.agilent.com). Array normalization was performed as previously described [29, 30] using a set of R-based scripts (http://r-project.org) in combination with a custom designed database that runs under the MySQL database management system (http://www.mysql.com). This was implemented on both dyes for each sample, and duplicate hybridizations with a Pearson correlation over 0.98 were considered for further analysis. Complete linkage was used for the construction of hierarchical clusters of the total microbiota probe profiles, while the distance matrix between the samples was based on Pearson correlation. The bacterial diversity of the fecal samples was assessed by Shannon’s index of diversity using the HITChip probe level [31].
Statistical analysis
Total area under the curve (AUC) of glucose and insulin was calculated using the trapezoidal method. HOMA-IR was calculated with the following formula: fasting glucose (mmol/L) × fasting insulin (mU/L) / 22.5. For comprehensive multivariate statistical analyses, Canoco software for Windows 5.0 was used [32]. Redundancy analysis (RDA) was used to assess correlations between the microbial groups detected by the HITChip analysis in function of sample characteristics. The log transformed hybridization signals of 130 genus-level phylogenetic groups were used as biological variables. As environmental variables, we included BMI, weight, excess weight loss (EWL), HbA1c, fasting glucose, fasting insulin, AUC glucose, AUC insulin, HOMA-IR, and sample source (i.e., a factor combination of treatment and time). Monte Carlo permutation testing (MCPT) as implemented in the Canoco software package was used to assess statistical significance of these variables in the dataset. The bacterial composition of the samples was compared at the phylum level (Class level for the Firmicutes) and at the approximate genus level (130 phylogenetic groups with more than 90% 16S rRNA gene sequence similarity [29]); using the Wilcoxon signed-rank test corrected for false discovery rate for which corrected p < 0.05 was considered significant. Differences in microbiota diversity were assessed by Student’s t test. Differences in weight and plasma parameters over time were assessed with the Wilcoxon Matched-pairs Signed Rank test. Values were considered significant at corrected p values <0.05. Data are presented as median and interquartile range.
Results
Metabolic changes initiated by DJBL treatment
Before implantation, patients had a median body weight of 106.1 [99.4–123.5] kg, a BMI of 35.2 [32.2–40.9] kg/m2, and an HbA1c of 8.5% [7.6–9.2]. Fasting glucose and insulin levels were 9.8 [8.9–12.8] mmol/L and 16.4 [10.1–21.3] IU/L, respectively. HOMA-IR was 7.3 [5.0–10.4].
Changes after 6 months of DJBL treatment are depicted in Fig. 1. Median body weight had decreased to 97.4 [89.4–114.0] kg (p < 0.05, Fig. 1a). This corresponds to a BMI of 31.5 [29.5–38.1] kg/m2 and an EWL of 18.3% [10.2–26.4] (both p < 0.05, Fig. 1b, c). HbA1c had decreased to 7.2% [6.3–8.1] (p < 0.05, Fig. 1d). In addition, fasting glucose levels, fasting insulin levels, and HOMA-IR decreased to 7.8 [7.1–8.7] mmol/L, 10.8 [8.4–16.1] IU/L, and 3.5 [2.5–6.4], respectively (all p < 0.05, Fig. 1e–g). Moreover, the glucose response to a meal as reflected by the AUC for glucose had decreased (Fig. 1h, p < 0.05). The AUC for insulin was not significantly changed (Fig. 1i, p = 0.07). Taken together, these data show that DJBL treatment significantly improved body weight and type 2 diabetes parameters.
Effects of DJBL treatment on metabolic parameters. a The body weight of patients before and 6 months after initiation of DJBL treatment. b BMI changes. c The excess weight loss after 6 months of DJBL treatment. d The HbA1c concentrations. e, f The fasting glucose and insulin levels obtained at baseline and at 6 months after initiation of DJBL treatment. g The changes in HOMA-IR initiated by DJBL treatment. h, i The area under the curve calculations for glucose and insulin, respectively. An asterisk (*) indicates p < 0.05
DJBL treatment induces gut microbiota composition alterations
Fecal microbiota composition was profoundly affected by DJBL treatment, as shown in Table 1. The DJBL intervention was notably associated with several changes within the Firmicutes phylum. Specifically, an ~25-fold increased relative abundance of Lactobacillus gasseri et rel., an ~11-fold increase in Lactobacillus plantarum et rel., as well as an almost 7-fold increase in Veillonella spp. were observed. Furthermore, many genera within the Proteobacteria phylum were increased in relative abundance by the DJBL treatment. The relative levels of Enterobacter aerogenes et rel. (~8-fold), Escherichia coli et rel. (~5-fold), Klebsiella pneumoniae et rel. (~12-fold), and Serratia (~6-fold) all increased after 6 months of DJBL treatment. In addition, the diversity of the fecal microbiota composition, as reflected by the Shannon diversity index, tended to increase from 5.4 [5.2–5.7] to 5.8 [5.4–5.9] by DJBL treatment (Fig. 2, p = 0.053).
Relationship between DJBL-induced metabolic improvement and microbiota composition
Next, we studied the relationship between changes in microbiota composition and changes in body weight and metabolic parameters induced by DJBL treatment. Clustering by RDA indicated that the DJBL-induced improvement in body weight and type 2 diabetes parameters negatively correlated with the relative abundance of Clostridium cluster XIVa and other Firmicutes (Fig. 3). In addition, a positive correlation was found between EWL and the relative abundance of Bacilli, Proteobacteria, and Bacteroidetes. This suggests that the metabolic improvement as observed after DJBL treatment is associated with rather specific changes in gut microbiota composition.
RDA plot of metabolic parameters and microbiota composition before and after DJBL treatment. Redundancy analysis of the association between metabolic parameters and the baseline microbiota composition of patients (blue dots), the microbiota composition of patients after 6 months of DJBL intervention (green dots), and 6 months post-intervention (red dots). The plotted first and second ordinations axes explain 13% and 5% of the variability in the dataset. Associations are shown with Bacilli and Proteobacteria, Bacteroidetes, and Clostridium cluster XIVa and other Firmicutes. In addition, correlations with all included variables are shown, though none were significant
Additional analyses further revealed that changes in specific bacterial groups correlate with the decreases in obesity and type 2 diabetes-related parameters (Fig. 4). For example, reductions in fasting glucose and HbA1c strongly correlated with increases in relative abundance of members of the Firmicutes phylum, specifically bacteria related to Ruminococcus callidus and Oscillospira guillermondii, respectively. Furthermore, changes in several other bacterial groups correlated negatively with EWL. As displayed in Fig. 4, positive correlations were found between EWL and both bacteria related to L. gasseri and L. plantarum, which abundance was greatly increased after DJBL treatment. Additional positive correlations were found between EWL and members from the Proteobacteria phylum: bacteria related to E. coli, Yersinia, K. pneumoniae, and E. aerogenes. Thus, changes in specific bacterial groups were associated with the metabolic improvement induced by DJBL treatment.
Reversal of microbiota alterations after DJBL explantation
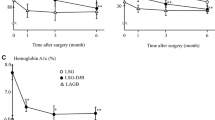
Six months after explantation of the DJBL, the fecal microbiota composition of the patients was similar to that observed before DJBL implantation (Fig. 3). In addition, no significant difference was found between the Shannon diversity index before implantation vs. 6 months post-explantation (5.4 [5.2–5.7] vs. 5.5 [5.4–5.6], Fig. 5a, p = 0.87). In contrast, 6 months after explantation, EWL, HOMA-IR, and the AUC for glucose remained significantly improved when compared to baseline (Fig. 5d, h, i). This indicates a sustained effect of the DJBL after explantation of the device, independent of microbiota changes.
Changes in metabolic parameters after DJBL explantation. a The Shannon diversity index at baseline and at 6 months post-explantation. b Changes in patients’ weight. c Changes in BMI. d The percentage of excess weight loss at 6 months post-explantation of the DJBL. e HbA1c levels. f, g The fasting glucose and insulin levels, respectively. h HOMA-IR levels. i, j The area under the curve calculations for glucose and insulin at baseline and 6 months post-explant, respectively. An asterisk (*) indicates p < 0.05
Discussion
Gut microbiota are considered to play an important role in the development of obesity and its related comorbidities. In the current study, the relationship between a reduction of obesity and type 2 diabetes-related parameters following a nonsurgical bariatric and metabolic technique and the resulting impact on intestinal microbiota composition were investigated. Our results indicate that metabolic improvement after a bariatric intervention excluding the proximal small intestine correlates with changes in colonic microbiota composition.
The DJBL can be considered to mimic the intestinal bypass component of the conventional RYGB. Interestingly, the current data regarding changes in microbiota composition in relation to weight loss and metabolic improvement after initiation of DJBL treatment are in line with previous results reported in the context of RYGB surgery. Changes in gut microbiota after RYGB were shown to be associated with weight loss and metabolic improvement [18, 20].
As shown in Table 1, the abundance of several members of the Proteobacteria phylum was increased in feces after DJBL implantation. In both animals and humans undergoing RYGB surgery, similar increases of Proteobacteria have been reported [5, 18, 20, 33, 34]. An explanation for this shift might be found in the effects of proximal small intestinal exclusion. After DJBL implantation as well as after RYGB, digestion and absorption of nutrients is delayed to the mid-jejunum as the proximal small intestine is excluded from alimentary flow [35]. As a result, undigested nutrients will be available more distal in the small intestine. This might relocate typical small intestinal microbiota, such as Proteobacteria, to the colon. In line, we observed a large increase of Veillonella, a frequently encountered commensal in the human small intestine belonging to the Firmicutes phylum [36], in the feces of DJBL-treated subjects.
Next to these changes, DJBL treatment induced a microbiota shift in favor of lactobacilli. Both bacteria related to L. plantarum and L. gasseri increased greatly after initiation of DJBL treatment. Interestingly, these and other Lactobacillus spp. have previously been associated with weight loss. In overweight/obese small animal models, administration of L. plantarum caused body weight loss [8, 37]. Administration of fermented milk containing the probiotic L. gasseri SBT2055 to humans also led to a decrease in body weight and abdominal adiposity [38]. In addition, trans-10,cis-12-conjugated linoleic acid-producing L.plantarum has been shown to have an antiobesity effect in mice [39, 40]. This supports an important role for the observed shift in favor of these lactobacilli in the improvement of body weight following DJBL treatment. Although speculative, the bloom in lactobacilli may also be related to an increased availability of unabsorbed nutrients in more distal intestinal segments. Importantly, at the species level, different effects of lactobacilli on obesity have been found [41,42,43]. However, since the HITChip does not allow identification beyond genus level, these observations cannot be verified in our study.
Shannon’s diversity index, representing the number of different bacteria and their relative abundances in the fecal microbiota composition, was increased by DJBL treatment, similar to what has been reported after bariatric surgery [44]. Importantly, decreased microbiota diversity has been shown to be associated with both obesity and type 2 diabetes [45, 46]. In addition, the Shannon diversity index as calculated from the fecal samples obtained from non-obese controls from our previous study was similar to the index obtained from the samples collected 6 months after initiation of DJBL treatment (5.9 [5.6–6.1] vs. 5.8 [5.4–5.9], non-obese control vs. 6 months after initiation of DJBL treatment, p = 0.15). This suggests a normalization of intestinal microbial diversity by DJBL treatment.
Although the abundance of Clostridium cluster IV tended to be increased by DJBL treatment, the abundance of Clostridium cluster XIVa tended to be decreased. Within the Clostridium cluster IX, decreases as well as increases were observed after DJBL treatment. Therefore, conclusions regarding whether or not the observed changes within the Clostridium clusters are beneficial are difficult to draw. Similarly, the applicability of the recently proposed concept of the impact of the gut redox status on chronic disease conditions [47] remains to be determined. However, it is conceivable that the DJBL alters oxygen consumption in the proximal gastro-intestinal tract, potentially leading to an increased fecal abundance of aerotolerant bacteria [48, 49].
After explantation of the DJBL, the EWL, HOMA-IR, and the AUC for glucose during a meal tolerance test remained significantly improved when compared to pre-implantation, indicating a prolonged effect of DJBL treatment. However, the microbiota composition returned to the pre-implantation situation. This may suggest that the metabolic improvement after DJBL treatment is independent of microbiota composition changes. Alternatively, the effect of DJBL treatment on gut microbiota composition may primarily drive the initial improvement in glucose homeostasis; other mechanisms, such as hormonal changes [26, 50], may be responsible for the prolonged improvement. Another explanation could be that the microbiota changes are too small to be detected with the present approach, as would be the case when they primarily affect the small intestine microbes. However, the number of patients studied at 6 months post explantation was small (n = 6), warranting further investigation.
In summary, we have shown for the first time that improvement of obesity and type 2 diabetes after exclusion of the proximal small intestine by DJBL treatment is associated with changes in microbiota composition. Our data may provide keys to the pathogenesis of obesity and type 2 diabetes, and further studies might lead to new treatment modalities based on prebiotics and next-generation probiotics.
References
Tilg H, Moschen AR, Kaser A. Obesity and the microbiota. Gastroenterology. 2009;136:1476–83.
Cani PD, Delzenne NM. The gut microbiome as therapeutic target. Pharmacol Ther. 2011;130:202–12.
DiBaise JK, Zhang H, Crowell MD, Krajmalnik-Brown R, Decker GA, Rittmann BE. Gut microbiota and its possible relationship with obesity. Mayo Clin Proc. 2008;83:460–9.
Tilg H, Kaser A. Gut microbiome, obesity, and metabolic dysfunction. J Clin Investig. 2011;121:2126–32.
Tremaroli V, Karlsson F, Werling M, Stahlman M, Kovatcheva-Datchary P, Olbers T, et al. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab. 2015;22:228–38.
Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA. 2004;101:15718–23.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31.
Arora T, Singh S, Sharma RK. Probiotics: interaction with gut microbiome and antiobesity potential. Nutrition. 2013;29:591–6.
Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci USA. 2005;102:11070–5.
Turnbaugh PJ, Backhed F, Fulton L, Gordon JI. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe. 2008;3:213–23.
Hugenholtz F, de Vos WM. Mouse models for human intestinal microbiota research: a critical evaluation. Cell Mol Life Sci. 2018;75:149–60.
Verdam FJ, Fuentes S, de Jonge C, Zoetendal EG, Erbil R, Greve JW, et al. Human intestinal microbiota composition is associated with local and systemic inflammation in obesity. Obesity (Silver Spring). 2013;21:E607–15.
Santacruz A, Collado MC, Garcia-Valdes L, Segura MT, Martin-Lagos JA, Anjos T, et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr. 2010;104:83–92.
Schwiertz A, Taras D, Schafer K, Beijer S, Bos NA, Donus C, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity 2010;18:190–5.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444:1022–3.
Duncan SH, Lobley GE, Holtrop G, Ince J, Johnstone AM, Louis P, et al. Human colonic microbiota associated with diet, obesity and weight loss. Int J Obes (Lond). 2008;32:1720–4.
Nadal I, Santacruz A, Marcos A, Warnberg J, Garagorri JM, Moreno LA, et al. Shifts in clostridia, bacteroides and immunoglobulin-coating fecal bacteria associated with weight loss in obese adolescents. Int J Obes (Lond). 2009;33:758–67.
Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y, et al. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci USA. 2009;106:2365–70.
Bjorneklett A, Viddal KO, Midtvedt T, Nygaard K. Intestinal and gastric bypass. Changes in intestinal microecology after surgical treatment of morbid obesity in man. Scand J Gastroenterol. 1981;16:681–7.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59:3049–57.
Vrieze A, Van Nood E, Holleman F, Salojarvi J, Kootte RS, Bartelsman JF, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143:913–6.e7.
Kootte RS, Levin E, Salojarvi J, Smits LP, Hartstra AV, Udayappan SD, et al. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline intestinal microbiota composition. Cell Metab. 2017;26:611–9.e6.
Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359:1151–6.
Schouten R, Rijs CS, Bouvy ND, Hameeteman W, Koek GH, Janssen IM, et al. A multicenter, randomized efficacy study of the EndoBarrier Gastrointestinal Liner for presurgical weight loss prior to bariatric surgery. Ann Surg. 2010;251:236–43.
de Moura EG, Martins BC, Lopes GS, Orso IR, de Oliveira SL, Galvao Neto MP, et al. Metabolic improvements in obese type 2 diabetes subjects implanted for 1 year with an endoscopically deployed duodenal-jejunal bypass liner. Diabetes TechnolTher. 2012;14:183–9.
de Jonge C, Rensen SS, Verdam FJ, Vincent RP, Bloom SR, Buurman WA, et al. Endoscopic duodenal-jejunal bypass liner rapidly improves type 2 diabetes. Obes Surg. 2013;23:1354–60.
Escalona A, Pimentel F, Sharp A, Becerra P, Slako M, Turiel D, et al. Weight loss and metabolic improvement in morbidly obese subjects implanted for 1 year with an endoscopic duodenal-jejunal bypass liner. Ann Surg. 2012;255:1080–5.
Salonen A, Nikkila J, Jalanka-Tuovinen J, Immonen O, Rajilic-Stojanovic M, Kekkonen RA, et al. Comparative analysis of fecal DNA extraction methods with phylogenetic microarray: effective recovery of bacterial and archaeal DNA using mechanical cell lysis. J Microbiol Methods. 2010;81:127–34.
Rajilic-Stojanovic M, Heilig HG, Molenaar D, Kajander K, Surakka A, Smidt H, et al. Development and application of the human intestinal tract chip, a phylogenetic microarray: analysis of universally conserved phylotypes in the abundant microbiota of young and elderly adults. Environ Microbiol. 2009;11:1736–51.
Jalanka-Tuovinen J, Salonen A, Nikkila J, Immonen O, Kekkonen R, Lahti L, et al. Intestinal microbiota in healthy adults: temporal analysis reveals individual and common core and relation to intestinal symptoms. PLoS ONE. 2011;6:e23035.
Magurran AE. Measuring biological diversity. Malden/Oxford: Blackwell; 2004. viii, 256 pp.
ter Braak CJF, Similauer P. Canoco reference manual and user’s guide: software for ordination, version 5.0. Microcomputer Power: Ithaca, USA; 2012.
Li JV, Ashrafian H, Bueter M, Kinross J, Sands C, le Roux CW, et al. Metabolic surgery profoundly influences gut microbial-host metabolic cross-talk. Gut. 2011;60:1214–23.
Liou AP, Paziuk M, Luevano JM Jr, Machineni S, Turnbaugh PJ, Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Trans Med. 2013;5:178ra41.
Goldfine AB, Shoelson SE, Aguirre V. Expansion and contraction: treating diabetes with bariatric surgery. Nat Med. 2009;15:616–7.
van den Bogert B, Erkus O, Boekhorst J, de Goffau M, Smid EJ, Zoetendal EG, et al. Diversity of human small intestinal Streptococcus and Veillonella populations. FEMS Microbiol Ecol. 2013;85:376–88.
Million M, Angelakis E, Paul M, Armougom F, Leibovici L, Raoult D. Comparative meta-analysis of the effect of Lactobacillus species on weight gain in humans and animals. Microb Pathog. 2012;53:100–8.
Kadooka Y, Sato M, Imaizumi K, Ogawa A, Ikuyama K, Akai Y, et al. Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr. 2010;64:636–43.
Lee K, Paek K, Lee HY, Park JH, Lee Y. Antiobesity effect of trans-10,cis-12-conjugated linoleic acid-producing Lactobacillus plantarum PL62 on diet-induced obese mice. J Appl Microbiol. 2007;103:1140–6.
Takemura N, Okubo T, Sonoyama K. Lactobacillus plantarum strain No. 14 reduces adipocyte size in mice fed high-fat diet. Exp Biol Med (Maywood). 2010;235:849–56.
Million M, Raoult D. Species and strain specificity of Lactobacillus probiotics effect on weight regulation. Microb Pathog. 2013;55:52–4.
Million M, Maraninchi M, Henry M, Armougom F, Richet H, Carrieri P, et al. Obesity-associated gut microbiota is enriched in Lactobacillus reuteri and depleted in Bifidobacterium animalis and Methanobrevibacter smithii. Int J Obes (Lond). 2012;36:817–25.
Million M, Angelakis E, Maraninchi M, Henry M, Giorgi R, Valero R, et al. Correlation between body mass index and gut concentrations of Lactobacillus reuteri, Bifidobacterium animalis, Methanobrevibacter smithii and Escherichia coli. Int J Obes (Lond). 2013;37:1460–6.
Kong LC, Tap J, Aron-Wisnewsky J, Pelloux V, Basdevant A, Bouillot JL, et al. Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am J Clin Nutr. 2013;98:16–24.
Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500:541–6.
Zhang X, Shen D, Fang Z, Jie Z, Qiu X, Zhang C, et al. Human gut microbiota changes reveal the progression of glucose intolerance. PLoS ONE. 2013;8:e71108.
Million M, Raoult D. Linking gut redox to human microbiome. Hum Microbiome J. 2018;10:27–32.
Million M, Tidjani Alou M, Khelaifia S, Bachar D, Lagier JC, Dione N, et al. Increased gut redox and depletion of anaerobic and methanogenic prokaryotes in severe acute malnutrition. Sci Rep. 2016;6:26051.
Qiao Y, Sun J, Ding Y, Le G, Shi Y. Alterations of the gut microbiota in high-fat diet mice is strongly linked to oxidative stress. Appl Microbiol Biotechnol. 2013;97:1689–97.
de Jonge C, Rensen SS, Verdam FJ, Vincent RP, Bloom SR, Buurman WA, et al. Impact of duodenal-jejunal exclusion on satiety hormones. Obes Surg. 2016;26:672–8.
Acknowledgements
The authors would like to thank the patients contributing to this trial; the trial nurse Y. Wils, the students who helped conducting this research, Dr. R.J. de Ridder, Dr. G.H. Koek, and Dr. C.M. Bakker for their help with the DJBL procedures; and Prof. Dr. A.A. Masclee, Dr. J. Maljaars, Y. Slaats, and Dr. F.J. Verdam for their help regarding the study design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N.D.B. received an open research grant from GI dynamics. J.W.G. received an open research grant and support for travel to meetings for the study or other purposes from GI dynamics. W.M.d.V. received a Spinoza award and a Gravitation grant (SIAM 024.002.002) of the Netherlands organization for Scientific Research (NWO). All other authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Jonge, C., Fuentes, S., Zoetendal, E.G. et al. Metabolic improvement in obese patients after duodenal–jejunal exclusion is associated with intestinal microbiota composition changes. Int J Obes 43, 2509–2517 (2019). https://doi.org/10.1038/s41366-019-0336-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0336-x
- Springer Nature Limited
This article is cited by
-
Shifts in gut microbiota and their metabolites induced by bariatric surgery. Impact of factors shaping gut microbiota on bariatric surgery outcomes
Reviews in Endocrine and Metabolic Disorders (2021)