Abstract
Background
A body of literature suggests a metabolically healthy phenotype in individuals with obesity. Despite important clinical implications, the early origins of metabolically healthy obesity (MHO) have received little attention.
Objective
To assess the prevalence of MHO among the Northern Finland Birth Cohort 1966 (NFBC1966) at 31 years of age, examine its determinants in early life taking into account the sex specificity.
Methods
We studied 3205 term-born cohort participants with data available for cardio-metabolic health outcomes at 31 years, and longitudinal height and weight data. After stratifying the population by sex, adult BMI and a strict definition of metabolic health (i.e., no risk factors meaning metabolic health), we obtained six groups. Repeated childhood height and weight measures were used to model early growth and early adiposity phenotypes. We employed marginal means adjusted for mother and child covariates including socio-economic status, birth weight and gestational-age, to compare differences between the groups.
Results
The prevalence of adult MHO was 6% in men and 13.5% in women. Differences in adult metabolic status were linked to alterations in BMI and age at adiposity peak in infancy (p < 0.0003 in men and p = 0.027 in women), and BMI and age at adiposity rebound (AR) (p < 0.0001 irrespective of sex). Compared to MHO, metabolically unhealthy obese (MUO) women were five and a half months younger at AR (p = 0.007) with a higher BMI while MUO men were four months older (p = 0.036) with no difference in BMI at AR.
Conclusion
At the time of AR, MHO women appeared to be older than their MUO counterparts while MHO men were younger. These original results support potential risk factors at the time of adiposity rebound linked to metabolic health in adulthood. These variations by sex warrant independent replication.
Similar content being viewed by others
Introduction
The prevalence of obesity nearly tripled worldwide over the past 40 years. In 2016, 650 million adults were obese, representing 13% of the world’s adult population [1]. This epidemic represents a major public health concern and an economic threat. Obesity is an important risk factor for common metabolic disorders, low-grade inflammation and clinical end-points such as hypertension, insulin resistance (IR), type 2 diabetes (T2D), cardiovascular diseases (CVD) and several types of cancers [2, 3]. However, there are indications [4, 5] that a subgroup of obese individuals could be protected from the typical obesity-associated disorders such as hypertension, dyslipidaemia and impaired glucose metabolism despite having large quantities of fat mass. They have been identified as metabolically healthy obese (MHO) [6, 7]. The prevalence of MHO varies significantly between studies. Besides study specificities (e.g., age, ethnicity), the main reason for the observed differences would probably be lack of a unified definition of metabolic health and obesity. Many definitions coexist; one of the most frequent relies on the absence of metabolic syndrome. Others include favorable inflammatory profile or insulin sensitivity or use waist circumference or body fat percentage instead of standard BMI [8].
It is unclear whether the MHO phenotype associates with decreased or delayed mortality and morbidity risks compared to metabolically unhealthy obese (MUO) or metabolically healthy non-obese subjects. Overall, the evidence between-group comparisons is contradictory, questioning its clinical and public health relevance. Some studies suggest that MHO individuals are not at increased risk of mortality, T2D, cardiovascular events, all-cause cancers or thicker carotid intima-media, when compared to metabolically healthy non-obese individuals [9,10,11,12] while the Whitehall [13] and Pizarra studies [14] both suggest that MHO individuals were at a lower risk of developing T2D when compared to MUO. However, the analysis of the NHANES III study [15] showed an increase in all-cause mortality in obese individuals regardless of their metabolic health, and Chang and colleagues [16] found an increased risk of Non-Alcoholic Fatty Liver Disease (NASH) linked to adiposity. Most studies investigating MHO apply to adult populations but only a few cover the period from infancy into adulthood [17] despite the established evidence that early growth factors such as birth weight, timing of adiposity rebound and changes in linear growth have been linked to obesity in adult life [18, 19]. Moreover, differences in growth exist between males and females starting as early as in-utero with boys generally having a higher birth weight, a later adiposity rebound and a later puberty than girls [20]. Differences by sex carry on in adulthood with men tending to have more abdominal fat than women among other metabolic adversities. We therefore hypothesized that early life factors, notably the timing of adiposity rebound are linked with MHO in adulthood. The aim of this study was threefold, (i) assess the prevalence of MHO among the Northern Finland Birth Cohort 1966 (NFBC1966) at 31 years of age, (ii) examine the early life origins of MHO and (iii) characterise sex specificity.
Material and methods
Population studied
We analysed the NFBC1966 data until the age of 31 years. Pregnant women from the two northernmost provinces of Finland with expected delivery during the year 1966 were enrolled. The cohort includes 96% of all births in the area with 12 058 live born. During infancy and childhood, the Child Health and Welfare nurses recorded multiple and regular growth measures. At 31 years of age, questionnaires about health and lifestyle were sent to all cohort members whose address was known. Due to the data collection logistics, only those living in Northern Finland (Lapland and Oulu provinces) or Helsinki area were invited to participate in a clinical examination. This subpopulation represents well the whole study population [21].
We excluded participants without fasting blood sample, pregnant women and participants with congenital history of CVD. Following Wildman’s definition, we excluded individuals with a BMI under 18.5 kg/m2, underweight individuals being more prone to adverse health outcomes. We also excluded twins, pre-term (<37 gestational weeks) and post-term (>42 gestational weeks) to reduce confounding by gestational age or otherwise deviant intrauterine growth and those without data available for adiposity peak (AP) or adiposity rebound (AR). The present study includes only participants with complete metabolic data (blood pressure, triglycerides, HDL-cholesterol, fasting glucose, high sensitivity C-Reactive Protein (hsCRP) and HOMA-IR), AP and AR data. Figure 1 shows the flow chart of the study; the remaining 3205 cohort members were included in further analyses (52.0% men). The Ethics Committee of the Northern Ostrobothnia Hospital District approved the study and the study participants signed a written inform consent.
Study variables
Questionnaire at 31 years
The cohort members completed a postal questionnaire about health, lifestyle and socio-economic position. Smoking habits were categorized as non-smoker and smoker, alcohol consumption was estimated in grams per day. Diet score included the frequency of consumption of food rich in fibre and food high in saturated fat and was coded previously [22]. A score of three or less determined a healthy diet whereas four or five indicated an unhealthy diet.
Light physical activity was defined as physical activity causing no sweating or shortness of breath and brisk physical activity causing at least sweating and shortness of breath. Using the duration and intensity of brisk/light physical activity, we calculated Metabolic Equivalent of Task (MET) minutes per week. The socioeconomic status was based on occupation and employment status and categorized as professionals, skilled workers, unskilled workers, farmers and others (students, pensioners, long-term unemployed or not defined). Self-reported medications were classified according to the Anatomical Therapeutic Chemical (ATC) classification system [23].
Clinical examination at 31 years of age
Trained research nurses performed the anthropometric measurements, carried out the medical examinations and supervised the fitness tests. Weight (kg), height (cm), waist circumference (cm) (midway between the lowest rib margin and the iliac crest), hip circumference (cm) (at the widest trochanters) were measured. The BMI (kg/m2) and the waist/hip ratio (WHR) were calculated. Two measures of systolic and diastolic blood pressure were taken in a sitting position using a standard mercury sphygmomanometer after a 15 min rest. We used the average of the readings.
Muscular fitness was assessed by trunk extension test and maximal isometric hand grip test. The trunk extension test involved the subject holding a prone position with the lower body lying on the stand and the upper body unsupported as long as possible with a maximum of four minutes. The maximal isometric handgrip was performed three times on the dominant hand; the highest value of the three trials was reported as a result. The detailed procedures of these tests have been previously described [24].
Cardiorespiratory function and fitness were evaluated using spirometry test and step test described earlier in details in NFBC1966 studies [25]. Respiratory function was measured by forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC). The test was performed three times and the highest FEV1 and FVC measurements were used to calculate FEV% (FEV1/FVC ratio). The submaximal four-minute single step test was conducted without shoes on a bench 33 cm high for the females and 40 cm high for the males, the heart rate was measured after the test.
Biochemical measures
Blood samples at the age 31 years were drawn after overnight fasting, the methods have been reported in previous studies [26]. The samples were aliquoted either as whole blood, kept at 4 °C to be analysed on the same day for glucose by a glucose dehydrogenase method (Granutest 250, diagnostic Merck, Germany) or processed according to standard protocols to acquire plasma and serum. The serum was kept at −20 °C until further analysis. Serum insulin concentrations were measured within seven days by radioimmunoassay (Pharmacia Diagnosis, Sweden). The lipid blood samples (stored at −80 °C) were analysed by enzymatic assays using Hitachi 911 automatic analyser and commercial reagents (Roche, Manheim, Germany) in the accredited laboratory of the Oulu University Hospital. Serum high sensitivity C-reactive protein (hs-CRP) concentrations were analysed by immunoenzymometric assay (Medix Biochemica, Espoo, Finland). The insulin sensitivity was determined using the Homeostatic Model Assessment based Insulin Resistance (HOMA-IR), derived from the following ((glucose (mmol/l)×insulin (mmol/l))/22.5).
Metabolic Health Status
The metabolic health status was defined using a selection of cardio-metabolic and inflammation (proxy: hsCRP) criteria proposed by Wildman and colleagues:[6]
-
Elevated blood pressure (≥130 or ≥85 mmHg) or anti-hypertensive medication (ATC codes: C02, C03, C07, C08, C09).
-
Fasting hypertriglyceridemia (≥1.70 mmol/l).
-
Fasting low HDL-cholesterol level (< 1.04 mmol/l for men and < 1.30 mmol/l for women) or lipid-lowering medication (ATC codes: B04, C10).
-
Elevated fasting plasma glucose (≥5.55 mmol/l) or diabetes medication (ATC codes: A10).
-
Elevated HOMA-IR (>90th percentile value, i.e., 1.66 for men and 1.52 for women).
-
Elevated hsCRP level (>90th percentile value, i.e., 3.50 for men and 5.40 for women).
Wildman and colleagues determine cardio-metabolic health by the presence of zero or one criteria. In the present analysis we opted for a strict definition of cardio-metabolic health; individuals being cardio-metabolically healthy in the absence of any of the criteria mentioned above. The participants were then stratified according to their BMI as normal weight (18.5 kg/m2≤BMI<25 kg/m2), over-weight (25 kg/m2≤BMI<30 kg/m2) and obese (BMI≥30 kg/m2). The six groups resulting from this categorisation were called: metabolically healthy normal weight (MHNW), metabolically unhealthy normal weight (MUNW), metabolically healthy overweight (MHOW), metabolically unhealthy overweight (MUOW), metabolically healthy obese (MHO) and metabolically unhealthy obese (MUO).
Wildman and colleagues did not exclude elevated hsCRP values; hsCRP ≥10 mg/l is commonly used as a threshold for acute inflammation. A sensitivity analyse did not show any differences between inclusion and exclusion of individuals with elevated hsCRP (N = 116) or self-reported fever at the time of the clinical examination (N = 13). We kept these individuals in the analyses, following Wildman’s definition.
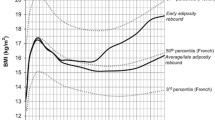
Growth variables
Birth weight (kg) and birth length (cm) were measured using standard methods of care. Gestational age was calculated from the mother’s last menstrual period. In order to model the BMI curve, described in detail elsewhere [27], two growth periods were considered; infancy (from two weeks to 18 months) and childhood (from 18 months to 13 years) [28]. Individuals with fewer than three measurements in each period were excluded. A BMI growth model was fitted to these data, identifying the AP, usually timed around 9 months of age and the AR, at the nadir of the curve generally occurring between 5 and 7 years. Peak height (PHV in cm/month) and peak weight velocity (PWV in kg/month) in infancy were derived from sex stratified non-linear mixed effect Reed1 models, previously described elsewhere [29].
Early life related covariates
These variables were retrieved from questionnaires filled in by mothers during pregnancy at maternity clinics. Maternal smoking at two months pregnancy was categorised as no smoker, former smoker and smoker, wantedness of pregnancy as wanted, mistimed or unwanted, and the marital status of the mother as married, unmarried, widowed or divorced. Social class at birth was assessed by the prestige of father’s occupation: no occupation, professionals and white collar upper level, white collar lower level, blue collar and farmers. The mother’s education ranged from no education to beyond matriculation examination. We also included continuous variables such as parity, age of mother, birth weight, gestational age, and mother’s BMI before pregnancy in the model.
Statistical analysis
We conducted statistical analyses using SAS, version 9.4 (SAS Institute Inc., Cary, North Carolina). Due to the divergences in their physiology and development, all analyses were done separately for men and women [30]. For sensitivity analyses we excluded oral contraceptive (OCPs) users, as OCPs are known to have an impact on women’s cardio-metabolic health [30]. This, however, did not affects. We excluded 1017 cases of incomplete growth data. We compared the distributions of complete and incomplete cases by the cardio-metabolic groups and found no difference (data not shown).
The descriptive statistics are presented as mean values (with standard deviations, SDs) for continuous variables and percentages for categorical variables. Variables with non parametric distributions were log-transformed. The differences between the groups were tested with ANOVA. We performed comparisons of marginal means (LS-means) between the reference and the other groups using Dunnett’s adjustment for multiple testing. We calculated effect sizes using partial omega squared and the results were interpreted as percentage difference between the groups. For theses analyses, we used MHO as a reference. A p value below 0.05 denotes statistical significance.
Results
Table 1 shows the demographic and clinical characteristics of the study population by their cardio-metabolic health status. At the age of 31 years of age, 37.2% of the subjects overall were metabolically healthy. This metabolically healthy group contains half of all women and a quarter of all men.
Prevalence of metabolically healthy obesity
Individuals in the metabolically healthy group were less obese than in the metabolically unhealthy group (respectively 2.6% vs 14.0%). They had also a smaller waist circumference. We observed a smaller proportion of unskilled workers and a greater proportion of skilled workers in the metabolically healthy group in comparison to the metabolically unhealthy group. The metabolically healthy group also reported less smoking and drinking, a healthier diet and showed better fitness (step test and back endurance test) than the metabolically unhealthy phenotype.
Figure 2 illustrates the proportions of the different metabolically healthy (MH) and unhealthy (MUH) groups stratified by categories of BMI (normal weight, overweight, obese) and sex at 31 years. The proportion of MH persons decreases in a stepwise manner with increasing BMI categories in both sexes, with women being metabolically healthier in proportion.
Early life determinants
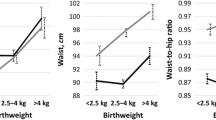
Tables 2a and 2b show the distribution of the early growth parameters in men and women by their metabolic health status and BMI categories at 31 years of age. In men, there was a large difference in birth weight between MUNW group which had the lowest birth weight (3552 (483 SD) grams) and MHOW with the highest (3682 (490 SD) grams) of all groups (p = 0.035). In the women’s group, MUNW also tended to be the lightest at birth with an average birth weight of 3 446 (435 SD) grams and MHO were the heaviest (3581 (390 SD) grams) (p = 0.15). Of all groups, MHO men had the highest BMI at AP, 18.6 (0.84 SD) kg/m2 (p = 0.0003). In men, MHO were the first to experience AR at four years and seven months, followed by MUO, MHOW, MUOW, MHNW and finally MUNW who rebounded more than seventeen months later (p < 0.0001; Table 2a). In contrast, MUO women were the first to rebound at four years and four months of age, followed by MHO, MHOW, MUOW, MHNW and MUNW, seventeen months later (p < 0.0001; Table 2b), i.e., overweight and obese subjects had rebounded earlier than normal weight subjects. At the time of adiposity rebound, MHO men and MUO women had the highest BMI of all groups with 16.5 (1.0 SD) kg/m2 and 16.1 (1.1 SD) kg/m2 respectively.
Figure 3 demonstrates the marginal mean differences for age (3A) and BMI (3B) at AR between metabolic groups using the MHO as a reference. In Fig. 3a, we observed clusters of metabolic groups by the BMI categories. There were significant differences between MHO men and the other groups but the effect sizes were weak in that AR explained around 2% of the variance between MHO and MUNW, as well as between MHO and MHNW. The women showed a similar trend in the BMI clustering described in men except for the obese subgroup where, contrary to men, MUO rebounded earlier than MHO (p = 0.0364). The effects sizes were also small in the female groups.
Forest plots showing differences in marginal means (95% CI) of age at adiposity rebound (years) a, between each group and the MHO reference group (vertical dotted line). The effect size is presented as partial omega squared. b shows the corresponding results for BMI at adiposity rebound. This model is adjusted for birth weight, gestational age, mother’s age, mother’s BMI, mother’s marital status, child wantedness, parity, mother’s smoking at 2 months of pregnancy, mother’s education, father’s occupation. MUO Metabolically Unhealthy Obese, MUOW Metabolically Unhealthy Overweight, MHOW Metabolically Healthy Overweight, MUNW Metabolically Unhealthy Normal Weight, MHNW Metabolically Healthy Normal Weight
Figure 3b shows the differences in BMI at AR between MHO and other metabolic groups. In men, we noticed again clusters by the BMI categories There was no significant difference between MHO and MUO and between MHO and MHOW. In women, there was no difference between MHO and the overweight subgroups except a nominally significant difference between MHO and MUO (p = 0.040) with small effect size.
Discussion
The present analysis supports the evidence of a link between early timing and BMI at adiposity rebound and the metabolically healthy obesity phenotype in adult men.
In our study, we observed that 41.4% of men and 23.3% of women at the age of 31 years were overweight and 8.9% of men and 10.6% of women were obese, which was consistent with national statistics at the time in Finland [31]. Within the obese population studied, we found that only 6.0% of men and 13.5% of women were metabolically healthy by strict criteria. The higher prevalence of MHO in women over men is in accordance with other studies [7, 32]. Our findings also support earlier studies from this cohort [28] where categorisation, according to metabolic health in BMI classes, suggested sex specificity in the growth patterns.
Numerous definitions of metabolic health coexist in the literature, leading to a large variation in the prevalence of MHO [7, 33]. Even when using the same definition, the Bioshare-EU project observed substantial variability with 10–40%, in the prevalence of MHO in several European cohorts [5]. We chose to use a more stringent definition of MHO according to Wildman [6], namely zero out of six criteria needed to qualify as metabolically healthy. This decision was made based on the relative young age and the inherent high blood pressure of our population. Indeed, 57.8% of men and 29.7% of women had a blood pressure greater than 130/85 or were using anti-hypertension medication. Critically, high blood pressure is endemic in Finland although global efforts have been made to tackle it. In the early 1970s the country had the highest prevalence of hypertension and coronary heart disease mortality in the world [34]. After 35 years, health policies exemplified by the North Karelia project [34] have been effective in influencing health behaviour and dietary habits in order to achieve an 80% decline in the coronary mortality in Finland. Yet, mean blood pressure remains high and the current hypertension threshold for Finland is equal or greater than 140/90 [35].
Thirty years ago, Rolland-Cachera and colleagues [36] identified early adiposity rebound as a predictor of adult obesity; this has been corroborated by many studies since [37,38,39]. Adiposity rebound is defined as the nadir of the BMI growth after which BMI starts to rise again and it normally occurs between five and seven years of age in the western countries. The typical pattern associated with early adiposity rebound is low BMI at time of rebound and subsequent increase [40,41,42]. A shift in the BMI growth curve seems to have happened in the early seventies and younger cohorts show adiposity rebound happening earlier. This pattern is now characteristic of children born during the obesity epidemic [42], which NFBC1966 is pre-dating. In the model developed in this study, we did not see a low BMI at time of the rebound for the obese adults, but we observed that both obese men and women had a higher BMI at rebound than in the other groups. Nevertheless, consistently with previous findings [43, 44], we found a negative association between age at adiposity rebound and adult BMI after stratifying by sex and BMI. It confirms earlier studies on NFBC1966 showing that an earlier adiposity rebound was a risk factor for an adverse cardio-metabolic profile, independently of BMI at the time of rebound [28]. However, our findings regarding MHO men tend to contrast with the general hypothesis that an earlier age at adiposity rebound would predict an unhealthy metabolic phenotype. Our results showed that MHO men rebounded earlier than their unhealthy counterparts. In contrast, the earlier obese women rebounded, the more likely they seemed to become metabolically unhealthy in adulthood.
It seems that two main early patterns lead to obesity, tracking and catching up. The first one involves infants with high birth weight who gained weight between birth and two years, a predictor of later insulin sensitivity [19]. These children with obesity display high BMI at all ages, reflecting both lean and fat mass, showing some protection from central obesity and IR; the authors suggested that an always-high BMI could correspond to MHO [45]. The second pattern involves low birth weight babies who underwent a rapid catch-up growth in early life. This process depletes the infant’s fat stores, triggering an early adiposity rebound, subsequently followed by an increase in BMI consisting in the deposition of fat rather than lean mass [45]. In the Flame Study in New Zealand, no differences were found in anthropometry measures and body composition at three years between early and late rebounders except that boys with early AR showed more fat free mass than the late rebounders [46]. At seven years old, marked differences appeared. The early rebounder boys were no taller but heavier with greater BMI than their late counterparts and they showed a greater deposition of fat free mass than fat mass. As for girls, early rebounders were not taller but gained considerably more weight, most of it consisting of fat mass with a small contribution from fat free mass. In another study involving young Swedish boys, early adiposity rebound was associated with higher fat mass, consisting of subcutaneous fat but not of visceral fat [38]. Visceral fat has been associated with unhealthy metabolic status in adulthood and subcutaneous fat with metabolically healthy status [47]. Unfortunately, adiposity data during childhood or at 31 years old in NFBC1966 is not available to replicate this analysis on MHO subpopulation.
Results from the present study reinforce evidence of the role of age at AR as a risk factor for obesity. Although adiposity rebound might be a good marker for later obesity, it could only capture the consequences of previous events, thus earlier steps in infancy are to be considered. The period from birth to two years old appears to be a key period in adult obesity [19]. However, our study did not provide evidence of further link between adult metabolic health and early growth factors preceding adiposity rebound. Earlier studies with NFBC1966 data revealed that low birth weight and rapid infant growth are important determinants of adult blood pressure [21]. Early adiposity rebound was robustly associated with the components of the metabolic syndrome irrespective of sex and adult BMI [28], and according to the authors, an important change in BMI after AR could predict an adverse cardio-metabolic profile in adulthood. In the 1982 Pelotas birth cohort study, a rapid postnatal weight gain after the age of two induced greater adult visceral fat, which was accentuated in low birth weight babies [18]. In addition, Salonen et al. [48] showed that slow weight gain from 0 to 2 years would increase the risk of developing metabolic syndrome in the obese adults. Similarly, they showed that the first six months after birth might be a crucial period in link to impaired glucose tolerance [49].
Strengths and limitations
This study shows important strengths. To our knowledge, this is the first study to show an association between the timing of adiposity rebound and MHO later in adult men. Furthermore, NFBC1966 is a homogeneous birth cohort with detailed reliable data on childhood growth. A limitation of our study was the low number of obese individuals in NFBC1966 at the age of 31 years which leads to the low prevalence of strictly MHO men and women. This was even more pertinent in men and it might have an influence on the statistical power of the study. Another possible limitation is the attrition due to the constraints associated with the BMI growth model and resulting in the exclusion of individuals with missing growth data. However, we did not find any difference between complete and incomplete cases groups that could indicate a bias in the analysis. Another aspect to consider is that NFBC1966 is a pre-obesity epidemic cohort; the participants were children in the early seventies, at a time where child obesity was not so common.
Conclusion
In conclusion, consistently with others, we observed a sub-population of MHO individuals in NFBC1966. The present study establishes a possible link between early age at adiposity rebound and a favourable metabolic health status in term-born obese adult men, suggesting that MHO finds its roots in early childhood and emphasizing the sex difference in the pathways leading to metabolic health later in life. Further longitudinal studies in larger populations are warranted for a better understanding of this concept. Life-course perspective is paramount in the understanding of the development of obesity and non-communicable diseases, and furthermore, prenatal and childhood growth data are equally essential as adult data.
References
WHO. Media Centre. Obesity and Overweight, Fact sheet No. 311. 2017; http://www.who.int/mediacentre/factsheets/fs311/en/.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Hinnouho GM, Czernichow S, Dugravot A, Batty GD, Kivimaki M, Singh-Manoux A. Metabolically healthy obesity and risk of mortality: does the definition of metabolic health matter? Diabetes Care. 2013;36:2294–2300.
van Vliet-Ostaptchouk JV, Nuotio ML, Slagter SN, Doiron D, Fischer K, Foco L, et al. The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: a collaborative analysis of ten large cohort studies. BMC Endocr Disord. 2014;14:9.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med. 2008;168:1617–24.
Pajunen P, Kotronen A, Korpi-Hyovalti E, Keinanen-Kiukaanniemi S, Oksa H, Niskanen L, et al. Metabolically healthy and unhealthy obesity phenotypes in the general population: the FIN-D2D Survey. BMC Public Health. 2011;11:754.
Phillips CM. Metabolically healthy obesity across the life course: epidemiology, determinants, and implications. Ann N Y Acad Sci. 2017;1391:85–100.
Meigs JB, Wilson PW, Fox CS, Vasan RS, Nathan DM, Sullivan LM, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91:2906–12.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97:2482–8.
Li S, Chen W, Srinivasan SR, Xu J, Berenson GS. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol. 2012;176(Suppl 7):142.
Calori G, Lattuada G, Piemonti L, Garancini MP, Ragogna F, Villa M, et al. Prevalence, metabolic features, and prognosis of metabolically healthy obese Italian individuals: the Cremona Study. Diabetes Care. 2011;34:210–5.
Hinnouho GM, Czernichow S, Dugravot A, Nabi H, Brunner EJ, Kivimaki M, et al. Metabolically healthy obesity and the risk of cardiovascular disease and type 2 diabetes: the Whitehall II cohort study. Eur Heart J. 2015;36:551–9.
Soriguer F, Gutierrez-Repiso C, Rubio-Martin E, Garcia-Fuentes E, Almaraz MC, Colomo N, et al. Metabolically healthy but obese, a matter of time? Findings from the prospective Pizarra study. J Clin Endocrinol Metab. 2013;98:2318–25.
Kuk JL, Ardern CI. Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care. 2009;32:2297–9.
Chang Y, Jung HS, Cho J, Zhang Y, Yun KE, Lazo M, et al. Metabolically healthy obesity and the development of nonalcoholic fatty liver disease. Am J Gastroenterol 2016;111:1133–40.
Howe LD, Zimmermann E, Weiss R, Sorensen TI. Do rapid BMI growth in childhood and early-onset obesity offer cardiometabolic protection to obese adults in mid-life? Analysis of a longitudinal cohort study of Danish men. BMJ Open. 2014;4:004827.
Araujo de Franca, GV, Lucia Rolfe E, Horta BL, Gigante DP, Yudkin JS, Ong KK, et al. Associations of birth weight, linear growth and relative weight gain throughout life with abdominal fat depots in adulthood: the 1982 Pelotas (Brazil) birth cohort study. Int J Obes. 2015;40:14–21.
Bouhours-Nouet N, Gatelais F, Dufresne S, Rouleau S, Coutant R. High birth weight and early postnatal weight gain protect obese children and adolescents from truncal adiposity and insulin resistance. Arch Pediatr. 2009;16:573–5.
Eriksson JG, Kajantie E, Osmond C, Thornburg K, Barker DJ. Boys live dangerously in the womb. Am J Hum Biol. 2010;22:330–5.
Jarvelin MR, Sovio U, King V, Lauren L, Xu B, McCarthy MI, et al. Early life factors and blood pressure at age 31 years in the 1966 northern Finland birth cohort. Hypertension. 2004;44:838–46.
Laitinen J, Pietilainen K, Wadsworth M, Sovio U, Jarvelin MR. Predictors of abdominal obesity among 31-y-old men and women born in Northern Finland in 1966. Eur J Clin Nutr. 2004;58:180–90.
WHO collaborating centre for drug statistics methodology. http://www.whocc.no/.
Tammelin T, Nayha S, Rintamaki H, Zitting P. Occupational physical activity is related to physical fitness in young workers. Med Sci Sports Exerc. 2002;34:158–65.
Canoy D, Pekkanen J, Elliott P, Pouta A, Laitinen J, Hartikainen AL, et al. Early growth and adult respiratory function in men and women followed from the fetal period to adulthood. Thorax. 2007;62:396–402.
Taponen S, Martikainen H, Jarvelin MR, Sovio U, Laitinen J, Pouta A, et al. Metabolic cardiovascular disease risk factors in women with self-reported symptoms of oligomenorrhea and/or hirsutism: Northern Finland Birth Cohort 1966 Study. J Clin Endocrinol Metab. 2004;89:2114–8.
Tzoulaki I, Sovio U, Pillas D, Hartikainen AL, Pouta A, Laitinen J, et al. Relation of immediate postnatal growth with obesity and related metabolic risk factors in adulthood: the northern Finland birth cohort 1966 study. Am J Epidemiol. 2010;171:989–98.
Sovio U, Kaakinen M, Tzoulaki I, Das S, Ruokonen A, Pouta A, et al. How do changes in body mass index in infancy and childhood associate with cardiometabolic profile in adulthood? Findings from the Northern Finland Birth Cohort 1966 Study. Int J Obes. 2014;38:53–59.
Sovio U, Bennett AJ, Millwood IY, Molitor J, O’Reilly PF, Timpson NJ, et al. Genetic determinants of height growth assessed longitudinally from infancy to adulthood in the northern Finland birth cohort 1966. PLoS Genet. 2009;5:e1000409.
Morin-Papunen L, Martikainen H, McCarthy MI, Franks S, Sovio U, Hartikainen AL, et al. Comparison of metabolic and inflammatory outcomes in women who used oral contraceptives and the levonorgestrel-releasing intrauterine device in a general population. Am J Obstet Gynecol. 2008;199:529.e10.
Lobstein T, Rigby N, Leach R EU platform on diet, physical activity and health: International Obesity Task Force EU Planning Briefing Paper. 2015. http://ec.europa.eu/health/ph_determinants/life_style/nutrition/documents/iotf_en.pdf.
Velho S, Paccaud F, Waeber G, Vollenweider P, Marques-Vidal P. Metabolically healthy obesity: different prevalences using different criteria. Eur J Clin Nutr. 2010;64:1043–51.
Primeau V, Coderre L, Karelis AD, Brochu M, Lavoie ME, Messier V, et al. Characterizing the profile of obese patients who are metabolically healthy. Int J Obes. 2011;35:971–81.
Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39:504–18.
Käypä hoito. Update on current care guideline: hypertension. Duodecim. 2014;130:2366–8.
Rolland-Cachera MF, Deheeger M, Bellisle F, Sempe M, Guilloud-Bataille M, Patois E. Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr. 1984;39:129–35.
Koyama S, Ichikawa G, Kojima M, Shimura N, Sairenchi T, Arisaka O. Adiposity rebound and the development of metabolic syndrome. Pediatrics. 2014;133:114.
Ohlsson C, Lorentzon M, Norjavaara E, Kindblom JM. Age at adiposity rebound is associated with fat mass in young adult males-the GOOD study. PLoS ONE. 2012;7:e49404.
Hughes AR, Sherriff A, Ness AR, Reilly JJ. Timing of adiposity rebound and adiposity in adolescence. Pediatrics. 2014;134:1354.
Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int J Obesity. 2006;30(Suppl 4):11.
Taylor RW, Grant AM, Goulding A, Williams SM. Early adiposity rebound: review of papers linking this to subsequent obesity in children and adults. Curr Opin Clin Nutr Metab Care. 2005;8:607–12.
Johnson W, Soloway LE, Erickson D, Choh AC, Lee M, Chumlea WC, et al. A changing pattern of childhood BMI growth during the 20th century: 70 y of data from the fels longitudinal study. Am J Clin Nutr. 2012;95:1136–43.
Boonpleng W, Park CG, Gallo AM. Timing of adiposity rebound: a step toward preventing obesity. Pediatr Nurs. 2012;38:37–42.
Williams SM. Weight and height growth rate and the timing of adiposity rebound. Obes Res. 2005;13:1123–30.
Rolland-Cachera MF, Peneau S. Growth trajectories associated with adult obesity. World Rev Nutr Diet. 2013;106:127–34.
Taylor RW, Williams SM, Carter PJ, Goulding A, Gerrard DF, Taylor BJ. Changes in fat mass and fat-free mass during the adiposity rebound: FLAME study. Int J Pediatr Obes. 2011;6:243.
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10:207–15.
Salonen MK, Kajantie E, Osmond C, Forsen T, Yliharsila H, Paile-Hyvarinen M, et al. Role of childhood growth on the risk of metabolic syndrome in obese men and women. Diabetes Metab. 2009;35:94–100.
Eriksson JG, Osmond C, Kajantie E, Forsen TJ, Barker DJ. Patterns of growth among children who later develop type 2 diabetes or its risk factors. Diabetologia. 2006;49:2853–8.
Acknowledgements
We thank the late professor Paula Rantakallio (launch of NFBC1966), the participants in the 31yrs study and the NFBC project center. NFBC1966 received financial support from University of Oulu Grant No. 65354, Oulu University Hospital Grant No. 2/97, 8/97, Ministry of Health and Social Affairs Grant no. 23/251/97, 160/97, 190/97, National Institute for Health and Welfare, Helsinki Grant No. 54121, Regional Institute of Occupational Health, Oulu, Finland Grant No. 50621, 54231. This work was supported by Biocenter Oulu, Grant 24002964, EurHealthAgeing, Grant No. 277849, Academy of Finland, Grant 243007961 and DynaHEALTH, Grant No. 633595.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Nedelec, R., Jokelainen, J., Miettunen, J. et al. Early determinants of metabolically healthy obesity in young adults: study of the Northern Finland Birth Cohort 1966. Int J Obes 42, 1704–1714 (2018). https://doi.org/10.1038/s41366-018-0115-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0115-0
- Springer Nature Limited