Abstract
It is unknown whether individuals with monoclonal B-cell lymphocytosis (MBL) are at risk for adverse outcomes associated with chronic lymphocytic leukemia (CLL), such as the risk of non-hematologic cancer. We identified all locally residing individuals diagnosed with high-count MBL at Mayo Clinic between 1999 and 2009 and compared their rates of non-hematologic cancer with that of patients with CLL and two control cohorts: general medicine patients and patients who underwent clinical evaluation with flow cytometry but who had no hematologic malignancy. After excluding individuals with prior cancers, there were 107 high-count MBL cases, 132 CLL cases, 589 clinic controls and 482 flow cytometry controls. With 4.6 years median follow-up, 14 (13%) individuals with high-count MBL, 21 (4%) clinic controls (comparison MBL P<0.0001), 18 (4%) flow controls (comparison MBL P=0.0001) and 16 (12%) CLL patients (comparison MBL P=0.82) developed non-hematologic cancer. On multivariable Cox regression analysis, individuals with high-count MBL had higher risk of non-hematologic cancer compared with flow controls (hazard ratio (HR)=2.36; P=0.04) and borderline higher risk compared with clinic controls (HR=2.00; P=0.07). Patients with high-count MBL appear to be at increased risk for non-hematologic cancer, further reinforcing that high-count MBL has a distinct clinical phenotype despite low risk of progression to CLL.
Similar content being viewed by others
Introduction
Chronic lymphocytic leukemia (CLL) is one of the most common hematologic malignancies, affecting ~5–10 people per 100 000.1 Population-based data indicate that patients with CLL are at increased risk for developing second cancers compared with the general population.2, 3, 4, 5 Specific malignancies for which patients with CLL seem to be at risk include other lymphoid malignancies, myelodysplastic syndromes and certain solid tumors (e.g. melanoma, breast, lung).2, 3, 4, 6, 7 In addition, patients who develop non-hematologic cancer in the setting of CLL may have inferior overall survival (OS) and cancer-specific survival (i.e. death due to breast cancer in a patient with breast cancer).8 A variety of factors may explain the increased risk of cancer in patients with CLL including: (i) shared genetic risk factors, (ii) shared behavioral risks or exposures, (iii) side effects of CLL treatment, (iv) dysregulation of immune surveillance and (v) ascertainment bias.
The need for a better understanding of the risk between CLL and the risk of second cancers has been heightened by the discovery of monoclonal B-cell lymphocytosis (MBL). MBL is a common asymptomatic condition characterized by a clonal B-cell population detected in the blood or bone marrow without cytopenias, lymphadenopathy or organomegaly.9 In screening studies of the population, MBL is prevalent in 3–5% of adults over age 40 years, and this rate increases with age.10, 11, 12, 13 MBL is an asymptomatic precursor state to CLL and other types of indolent non-Hodgkin lymphoma.14 Only a small subset of patients with MBL will come to clinical attention, typically during evaluation for low-grade lymphocytosis (designated now as high-count MBL). The rate of progression to CLL requiring treatment among individuals with high-count MBL is ~1% per year, and the vast majority of patients with high-count MBL will never develop a B-cell malignancy.10, 12, 14, 15 Recent data indicate that individuals with high-count MBL are at increased risk of infection similar to patients with CLL.16 It is unknown whether individuals with high-count MBL are at risk for other adverse outcomes associated with CLL, such as increased risk of non-hematologic cancer.2, 3, 4, 5
We investigated the incidence of non-hematologic cancer in a cohort of locally dwelling individuals with newly identified high-count MBL compared with two control cohorts and a cohort of patients with newly diagnosed CLL.
Materials and methods
Mayo Clinic Rochester is located in Olmsted County, Minnesota, and is the primary center for hematologic care in a region including southeastern Minnesota, northern Iowa and western Wisconsin. No other hematology specialty centers are available within a 50-mile radius of Mayo Clinic. The methods to assemble our MBL, CLL and clinic control cohorts have been described previously.16, 17
Patients
To explore the risk of non-hematologic cancer in a local, community-dwelling cohort of individuals with CLL-phenotype high-count MBL, we used the Mayo Clinic CLL database to identify all individuals with newly diagnosed high-count MBL seen in the Mayo Clinic Hematology Division between 1 January 1999 and 31 December 2009. Of the 154 high-count MBL cases residing within 50 miles of Mayo Clinic, the analysis was limited to 107 high- count MBL cases who did not have a prior non-hematologic cancer diagnosis at the time high-count MBL was identified.
Two control cohorts were used for comparison. The first consisted of 596 adult general medicine patients (clinic controls), residing within 50 miles of Mayo Clinic, who were seen for a general medical exam, and who enrolled as controls in a prospective case–control study of non-Hodgkin lymphoma between 25 April 2004 and 31 December 2009.18 The 589 (98.8%) individuals in this cohort with no prior cancer diagnosis at the time of enrollment were included in the analysis. To account for potential bias in the types of individuals undergoing flow cytometry evaluation (e.g., the group from which individuals with MBL was identified), a second comparison cohort (flow controls) was identified, which consisted of all adult residents of Olmsted County, Minnesota, without a known hematologic malignancy who underwent peripheral blood flow cytometry at Mayo Clinic during the study interval and were found to have normal flow cytometry results (e.g., no hematologic malignancy). A total of 482 individuals meeting these criteria had approved use of their clinical records for research purposes and were included in this analysis.
Rates of non-hematologic cancer in the MBL cohort were also compared with a cohort of patients with newly diagnosed CLL seen in the same time interval as the MBL cohort and also living within 50 miles of Mayo Clinic. Of the 174 identified CLL cases fitting these criteria, 132 had no prior non-hematologic cancer and were included in the analysis.
Non-hematologic cancer diagnoses were identified using the Mayo Clinic Tumor Registry, as well as by review of medical records in all four cohorts (MBL, CLL, Clinic Controls, Flow Controls). The Mayo Clinic Tumor Registry is an information system that prospectively collects and maintains data on patients diagnosed with a malignant condition, excluding non-melanoma skin cancer, at Mayo Clinic. The registry includes demographic information, diagnostic findings, primary site of malignancy, tumor stage and treatment/follow-up information obtained from the medical record. Patients with MBL/CLL with a non-hematologic cancer diagnosis >2 months before the diagnosis date of MBL/CLL were excluded from analysis. Patients who were diagnosed with a non-hematologic cancer within 2 months of diagnosis with MBL or CLL (e.g. 2 months before or 2 months after) were considered to have a ‘concurrent’ diagnosis. Patients in the control cohorts with cancer before the consent date (clinic controls) or normal flow cytometry date (flow controls) were excluded from the analysis. To evaluate for possible ascertainment bias, analysis was conducted both including and excluding ‘concurrently’ diagnosed cancers in the MBL, CLL, and flow control cohorts. Data on comorbid conditions was collected from the medical record as described previously.17 This study was conducted with approval from the Mayo Clinic Institutional Review Board and in accordance with the Declaration of Helsinki.
Differences in patient characteristics and cancers were compared between groups using χ2 or Fisher’s exact tests for qualitative variables or Kruskal–Wallis test for quantitative variables. The primary end point was development of new non-hematologic cancer. When the death rate is high, the standard Kaplan–Meier approach will overestimate the cumulative incidence rate of second cancers, as those who die are coded as censored events; therefore, death was primarily modeled using the more conservative approach modeling death as a competing event which provides a more accurate estimate of incidence (Kaplan–Meier estimates provided in Supplementary Figures 1A and B).19 Gray’s test for equality of cumulative incidence functions was used to compare time to first non-hematologic cancer between groups.20 To access the effect of risk factors on time to non-hematologic cancer after adjusting for confounding factors such as age, sex and major comorbidities,17 we modeled the proportional hazards of the subdistributions of the cumulative incidence function for the disease groups.21
Results
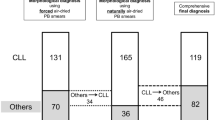
After excluding patients with prior cancers, there were 107 patients in the MBL cohort, 132 in the CLL cohort, 482 in the flow control cohort and 589 in the clinic control cohort. Individuals with high-count MBL and CLL tended to be older and were more likely to be male compared with both the clinic controls and flow cytometry controls (Table 1). A summary of comorbid health conditions is provided in Supplementary Table 2. Individuals with high- count MBL and CLL were more likely to have comorbid health conditions compared with clinic controls (P=0.001) but not flow cytometry controls (P=0.72).
Median follow-up of the MBL, CLL, flow control and clinic control cohorts was 4.8, 4.5, 5.1 and 4.3 years, respectively. Fourteen (13%) individuals with high-count MBL developed non-hematologic cancer as compared with 21 (4%) of the clinic controls (P<0.0001; Table 2). Sixteen (12%) CLL patients developed non-hematologic cancer, suggesting a similar rate to that of high-count MBL patients (P=0.82; Table 2). Eighteen (4%) flow controls developed non-hematologic cancer; this rate was significantly lower compared with that in the MBL cohort (P=0.0001; Table 3). Specifically, the MBL cohort had a higher cumulative incidence of cancer of the breast, lung and gastrointestinal tract compared with both clinic (Table 2) and flow cytometry controls (Table 3). The higher rate of second cancer in individuals with MBL (11%) relative to clinic controls (4%; P=0.002) and flow controls (3%; P=0.0004) persisted when patients with concurrent diagnosed cancers were excluded from the analysis.
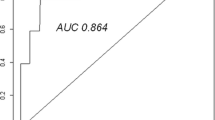
Time to development of non-hematologic cancer was shorter in MBL and CLL cohorts vs either the clinic controls (P-value=0.003; Figure 1a) or the flow controls (P-value=0.0001; Figure 1b). The shorter time to non-hematologic cancer in individuals with high-count MBL and CLL remained when patients treated for progressive CLL (in both CLL and MBL cohort) were censored at the date of their treatment (clinic controls, P=0.002 (Figure 1c); flow controls, P=0.0002 (Figure 1d)). Shorter time to non-hematologic cancer in individuals with high-count MBL also remained when patients with concurrently diagnosed cancers were excluded from the analysis (clinic controls, P=0.03 (Figure 1e); flow controls, P=0.0006 (Figure 1f)).
Time to diagnosis non-hematologic cancer. (a) Time from diagnosis to non-hematologic cancer, clinic control (Gray’s test P-value=0.003). (b) Time from diagnosis to non-hematologic cancer, flow control (Gray’s test P-value=0.0001). (c) Time from diagnosis to non-hematologic cancer, censored at treatment, clinic control (Gray’s test P-value=0.002). (d) Time from diagnosis to non-hematologic cancer, censored at treatment, flow control (Gray’s test P-value=0.0002). (e) Time from diagnosis to non-hematologic cancer, clinic control, exclude concurrent cancers (Gray’s test P-value=0.03). (f) Time from diagnosis to non-hematologic cancer, flow control, exclude concurrent cancers (Gray’s test P-value =0.0006).
Finally, we performed a pooled analysis of all of the MBL, CLL and clinic controls using Cox regression (n=828) adjusting for age, sex, major comorbidities, presence of high-count MBL and diagnosis of CLL (Table 4). Age (hazard ratio (HR) each year older=1.02; 95% confidence interval (CI)=1.003–1.04; P=0.02) was a risk factor for non-hematologic cancer, whereas high-count MBL was borderline significant (HR=2.00; 95% CI=0.94–4.24; P=0.07). When multivariable analysis was repeated using the flow controls: age (HR each year older=1.03; 95% CI=1.01–1.05; P=0.004), high-count MBL (HR=2.36; 95% CI=1.05–5.34; P=0.042) and CLL (HR=2.25; 85% CI=1.01–5.01; P=0.047) were independent risk factors for non-hematologic cancer. The results were similar for both models when the effect of age was modeled in a nonlinear (e.g. logarithmic) manner (Supplementary Table 1).
Discussion
We present the first study, to our knowledge, to explore the risk of non-hematologic cancer in patients with high-count MBL relative to controls. This cohort study, comparing the risk of non-hematologic cancer in individuals with high-count MBL to two separate control groups, demonstrates increased risk of non-hematologic cancer in patients with high-count MBL. Individuals with high-count MBL were at an ~2-fold risk for non-hematologic cancer compared with both clinic controls and flow cytometry controls. The risk of non-hematologic cancer among individuals with high-count MBL was similar to the risk in patients with CLL. This increased risk persisted and was of similar magnitude in multivariate analysis with flow controls adjusting for age, gender and major comorbidities, whereas the multivariate analysis using clinic controls demonstrated risk of similar magnitude at the threshold of statistical significance. The results for both models were also similar when age was modeled on the logarithmic scale.
In a previous analysis, we found individuals with high-count MBL were at increased risk of infection requiring hospitalization,16 suggesting that immune function may be impaired in individuals with high-count MBL. The increased risk of non-hematologic cancer in patients with high-count MBL seen in the current study adds to the evidence that high-count MBL has a clinical phenotype, despite the low risk of progression to CLL requiring treatment. In addition to increased risk of developing a second cancer, large population-based studies have demonstrated that patients with coexistent CLL and certain malignancies have inferior overall and cancer-specific survival compared with controls without CLL.8, 22 This observation raises important questions regarding risk stratification and management of a second primary cancer in patients with CLL. It is unknown whether high-count MBL may also be associated with inferior prognosis in patients with other malignancies.
Despite increased risk of non-hematologic cancer, the appropriate cancer screening approach for individuals with high-count MBL or CLL is unknown. In the current study, patients with high-count MBL appeared to have an increased risk of cancer of the breast, lung and gastrointestinal tract. Among these, screening is recommended for female breast, colorectal and lung cancer, depending on patient age and risk factors.23, 24, 25 At a minimum, patients with high-count MBL should be encouraged to undergo age- and gender-appropriate cancer screening consistent with national screening guidelines.
It should be noted that, before 2005, many individuals now classified as having high-count MBL would have been diagnosed with Rai stage 0 CLL.9, 26, 27 Although some have debated the appropriateness of this reclassification,28 multiple studies have demonstrated the reclassification better anchors the diagnosis of CLL to the likelihood a patient will develop clinical manifestations of their disease that actually require treatment.10, 15, 29, 30 Given the low rates of clinical progression among most individuals with high-count MBL12, 15 and the fact that this diagnosis does not appear to impact survival,31 this reclassification may also decrease unnecessary anxiety and emotional distress precipitated by diagnosing individuals with ‘leukemia’ when they have a very low risk of developing disease-related symptoms or requiring treatment during their lifetime. Despite these potentially beneficial aspects of this reclassification, the apparent increased risk of infection16 and non-hematologic cancers suggests that individuals with high-count MBL are at risk for various complications and may benefit from some of the supportive care measures (e.g., vaccination strategies, screening for skin cancer) recommended for patients with CLL.32, 33 Collectively, the risk of serious infection and/or non-hematologic cancer among individuals with high-count MBL appear to be greater than the likelihood they will progress to require treatment for CLL.
It should be emphasized that our findings relate to patients with high-count MBL. It is unknown whether the increased risk of non-hematologic cancer also applies to individuals with low-count MBL. Additional studies exploring that aspect would be noteworthy, given that low-count MBL impacts ~5% of the general population over the age of 40 years. Given this high prevalence in the general population, an increased risk of non-hematologic cancer among patients with low-count MBL could have substantial population-level implications.
Our study has several limitations. First, the CLL and MBL cohorts were derived from patients residing within 50 miles of Mayo Clinic. Consistent with the demographic composition of this region, the cohorts were comprised predominately of Caucasian individuals, and these results may or may not generalize to a more diverse patient population. Second, while both the Mayo Clinic CLL database and the Mayo Clinic Cancer Registry were cross-referenced, it is possible that there was incomplete ascertainment of all new non-hematologic cancer diagnoses. We did not have data on non-melanoma skin cancers. We also did not have data on screening. Third, we were unable to adjust for socioeconomic and lifestyle factors, particularly smoking and body mass index, that could influence risk of malignancy. Although these factors do not relate to the risk of developing CLL, they do relate to the risk of developing other cancers. Fourth, the cohorts were of insufficient size to provide enough statistical power to detect small differences in the risk of uncommon malignancies.
Our study also has several strengths. First, although many studies have demonstrated increased risk of non-hematologic cancer in patients with CLL, ours is the only study to evaluate the risk of non-hematologic cancer in a community-dwelling cohort of patients with high-count MBL. Second, we were able to use two separate control groups. Although we cannot exclude a healthy volunteer bias leading to a decreased rate of non-hematologic cancer in the clinic controls, this bias would not affect the flow cytometry control cohort. The flow control cohort also provides evidence that the increased incidence of non-hematologic cancer in the MBL cohort, relative to clinic controls, was not simply because of ascertainment bias in a cohort under increased medical scrutiny. It is also notable that the hazard ratio for risk of non-hematologic cancer in high-count MBL was similar regardless of which control group was used for comparison and regardless of whether age was used as a linear or logarithmic variable. Third, both control groups were drawn from the same region as the MBL and CLL cohorts, which is more appropriate than a population-based control sample, which can introduce bias in the context of clinic-based case ascertainment.18
In summary, patients with high-count MBL appear to carry an ~2-fold increased risk of non-hematologic malignancy. Growing evidence suggests that high-count MBL is not only a risk factor for progression to CLL but also a risk factor for some of the recognized complications observed in individuals with CLL, such as infection and malignancy.
References
Call TG, Phyliky RL, Noel P, Habermann TM, Beard CM, O'Fallon WM et al. Incidence of chronic lymphocytic leukemia in Olmsted County, Minnesota, 1935 through 1989, with emphasis on changes in initial stage at diagnosis. Mayo Clin Proc 1994; 69: 323–328.
Hisada M, Biggar RJ, Greene MH, Fraumeni JF Jr, Travis LB . Solid tumors after chronic lymphocytic leukemia. Blood 2001; 98: 1979–1981.
Morton LM, Curtis RE, Linet MS, Bluhm EC, Tucker MA, Caporaso N et al. Second malignancy risks after non-Hodgkin's lymphoma and chronic lymphocytic leukemia: differences by lymphoma subtype. J Clin Oncol 2010; 28: 4935–4944.
Tsimberidou AM, Wen S, McLaughlin P, O'Brien S, Wierda WG, Lerner S et al. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J Clin Oncol 2009; 27: 904–910.
Manusow D, Weinerman BH . Subsequent neoplasia in chronic lymphocytic leukemia. JAMA 1975; 232: 267–269.
Maddocks-Christianson K, Slager SL, Zent CS, Reinalda M, Call TG, Habermann TM et al. Risk factors for development of a second lymphoid malignancy in patients with chronic lymphocytic leukaemia. Br J Haematol 2007; 139: 398–404.
Schollkopf C, Rosendahl D, Rostgaard K, Pipper C, Hjalgrim H . Risk of second cancer after chronic lymphocytic leukemia. Int J Cancer 2007; 121: 151–156.
Solomon BM, Rabe KG, Slager SL, Brewer JD, Cerhan JR, Shanafelt TD . Overall and cancer-specific survival of patients with breast, colon, kidney, and lung cancers with and without chronic lymphocytic leukemia: a SEER population-based study. J Clin Oncol 2013; 31: 930–937.
Marti GE, Rawstron AC, Ghia P, Hillmen P, Houlston RS, Kay N et al. Diagnostic criteria for monoclonal B-cell lymphocytosis. Br J Haematol 2005; 130: 325–332.
Fazi C, Scarfo L, Pecciarini L, Cottini F, Dagklis A, Janus A et al. General population low-count CLL-like MBL persists over time without clinical progression, although carrying the same cytogenetic abnormalities of CLL. Blood 2011; 118: 6618–6625.
Ghia P, Prato G, Scielzo C, Stella S, Geuna M, Guida G et al. Monoclonal CD5+ and CD5- B-lymphocyte expansions are frequent in the peripheral blood of the elderly. Blood 2004; 103: 2337–2342.
Rawstron AC, Bennett FL, O'Connor SJ, Kwok M, Fenton JA, Plummer M et al. Monoclonal B-cell lymphocytosis and chronic lymphocytic leukemia. N Engl J Med 2008; 359: 575–583.
Rawstron AC, Green MJ, Kuzmicki A, Kennedy B, Fenton JA, Evans PA et al. Monoclonal B lymphocytes with the characteristics of ‘indolent’ chronic lymphocytic leukemia are present in 3.5% of adults with normal blood counts. Blood 2002; 100: 635–639.
Shanafelt TD, Ghia P, Lanasa MC, Landgren O, Rawstron AC . Monoclonal B-cell lymphocytosis (MBL): biology, natural history and clinical management. Leukemia 2010; 24: 512–520.
Shanafelt TD, Kay NE, Rabe KG, Call TG, Zent CS, Maddocks K et al. Brief report: natural history of individuals with clinically recognized monoclonal B-cell lymphocytosis compared with patients with Rai 0 chronic lymphocytic leukemia. J Clin Oncol 2009; 27: 3959–3963.
Moreira J, Rabe KG, Cerhan JR, Kay NE, Wilson JW, Call TG et al. Infectious complications among individuals with clinical Monoclonal B-cell Lymphocytosis (MBL): a cohort study of newly diagnosed cases compared to controls. Leukemia 2012; 27: 136–141.
Thurmes P, Call T, Slager S, Zent C, Jenkins G, Schwager S et al. Comorbid conditions and survival in unselected, newly diagnosed patients with chronic lymphocytic leukemia. Leuk Lymphoma 2008; 49: 49–56.
Cerhan JR, Fredericksen ZS, Wang AH, Habermann TM, Kay NE, Macon WR et al. Design and validity of a clinic-based case-control study on the molecular epidemiology of lymphoma. Int J Mol Epidemiol Genet 2011; 2: 95–113.
Gooley T, Leisenring W, Crowely J, Storer B . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Gray R . A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988; 16: 1141–1154.
Fine J, Gray R . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Brewer JD, Shanafelt TD, Otley CC, Roenigk RK, Cerhan JR, Kay NE et al. Chronic lymphocytic leukemia decreases survival of patients with malignant melanoma and Merkel cell carcinoma in a SEER Population-Based Study. J Clin Oncol 2012; 30: 843–849.
Moyer VA . Screening for lung cancer: U.S. Preventative Services Task Force Recommendation Statement. Ann Intern Med 2014; 160: 330–338.
Force USPST. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151: 716–726, W-236.
Force USPST. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2008; 149: 627–637.
Cheson BD, Bennett JM, Grever M, Kay N, Keating MJ, O'Brien S et al. National Cancer Institute-sponsored Working Group guidelines for chronic lymphocytic leukemia: revised guidelines for diagnosis and treatment. Blood 1996; 87: 4990–4997.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero D, Dohner H et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood 2008; 111: 5446–5456.
Scarfo L, Fazi C, Ghia P . MBL versus CLL: how important is the distinction? Hematol Oncol Clin North Am 2013; 27: 251–265.
Molica S, Mauro FR, Giannarelli D, Lauria F, Cortelezzi A, Brugiatelli M et al. Differentiating chronic lymphocytic leukemia from monoclonal B-lymphocytosis according to clinical outcome: on behalf of the GIMEMA chronic lymphoproliferative diseases working group. Haematologica 2011; 96: 277–283.
Shanafelt TD, Kay NE, Jenkins G, Call TG, Zent CS, Jelinek DF et al. B-cell count and survival: differentiating chronic lymphocytic leukemia from monoclonal B-cell lymphocytosis based on clinical outcome. Blood 2009; 113: 4188–4196.
Shanafelt TD, Kay NE, Rabe KG, Call TG, Zent CS, Schwager SM et al. Survival of patients with clinically identified monoclonal B-cell lymphocytosis (MBL) relative to the age- and sex-matched general population. Leukemia 2012; 26: 373–376.
Mansfield AS, Rabe KG, Slager SL, Schwager SM, Call TG, Brewer JD et al. Skin cancer surveillance and malignancies of the skin in a community-dwelling cohort of patients with newly diagnosed chronic lymphocytic Leukemia. J Oncol Pract 2013; 10: e1–e4.
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M et al. 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host. Clin Infect Dis 2013; 58: e44–100.
Acknowledgements
This work was supported in part by R01 CA92153 and the Henry J Predolin Foundation. Dr Shanafelt is a Clinical Scholar of the Leukemia and Lymphoma Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Solomon, B., Chaffee, K., Moreira, J. et al. Risk of non-hematologic cancer in individuals with high-count monoclonal B-cell lymphocytosis. Leukemia 30, 331–336 (2016). https://doi.org/10.1038/leu.2015.235
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2015.235
- Springer Nature Limited
This article is cited by
-
Chronic lymphocytic leukemia treatment algorithm 2022
Blood Cancer Journal (2022)
-
Chronic lymphocytic leukemia in 2020: a surfeit of riches?
Leukemia (2020)
-
Trends in the risk of second primary malignancies among survivors of chronic lymphocytic leukemia
Blood Cancer Journal (2019)
-
Chronic lymphocytic leukemia treatment algorithm 2018
Blood Cancer Journal (2018)