Abstract
Monoclonal B cell lymphocytosis (MBL) is both a marker of immune senescence and a potential precursor of B cell malignancy. Most MBL populations have a chronic lymphocytic leukemia-like (CLL-like) immunophenotype, but those that are CD5-negative (non-CLL-like) are also recognized and may represent a distinct diagnostic entity. To date, MBL studies have taken place in relatively homogenous populations, although risk of CLL varies across racial groups and geographic regions. We report flow cytometry data from 597 ethnically diverse 64–94-year-old women from across the USA who are participants in the Women’s Health Initiative (WHI) Long-Life Study (LLS). Overall, MBL was detected in 26 % of the participants and included 20.9 % with a CLL-like immunophenotype, 5 % with a non-CLL-like immunophenotype, and 1.3 % with both. White and Hispanic women were more than twice as likely to have a CLL-like MBL population detected than African American women, corrected for age (P = 0.003). By contrast, detection of non-CLL-like MBL did not vary significantly by race, but did increase markedly with advancing age, being present in 12.7 % of those aged 85 and older. We provide new evidence that rates of detection of CLL-like MBL are lower in African Americans, and further suggest that non-CLL-like clonal expansions should be regarded as distinct from CLL-like MBL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monoclonal B cell lymphocytosis (MBL) is a common but poorly understood aging phenomenon, estimated to occur in approximately 5–12 % of all adults over the age of 40, depending on the sensitivity of the flow cytometry assay [1–3]. Existing evidence suggests that MBL is both a marker of immune senescence and a potential precursor of B cell malignancy [4]. The large majority of MBL clones are identical in immunophenotype to chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), having expression of CD5 with dim expression of CD20 and surface light chain, but a smaller subset of MBL clones have an immunophenotype that would not be characteristic of CLL/SLL [1, 3, 5, 6]. These atypical or non-CLL-like MBL populations usually have normal intensity expression of CD20 and light chain without CD23; this immunophenotype would be typical of, but not entirely specific for, marginal zone lymphoma (MZL); CD5 is typically negative but may be expressed in some cases [7, 8]. Recent evidence suggests that clonal B cell subpopulations with a non-CLL-like immunophenotype are distinct from CLL-like MBL [3], and some have proposed different terminology to describe clonal expansions of potential marginal zone origin [8].
The clinical significance of MBL remains unclear, regardless of the immunophenotype. While it appears that virtually all cases of CLL/SLL are preceded by a preclinical monoclonal B cell expansion [9, 10], the converse does not appear to be the case. Only a very small subset of MBL (<1 % overall) clones progress to CLL/SLL, and the risk of progression is believed to be negligible for the very small MBL populations typically encountered in the population-based setting [11, 12]. The relationship between non-CLL-like clonal B cell expansions and frank lymphoma has not yet been fully defined [8, 13]. MBL is also presumed to be a marker of immune senescence in a manner analogous to well-known alterations in circulating T cell subsets that occur with age [14–16]. MBL detection has been reported to increase markedly with age, with rates of detection exceeding 25 % in those over the age of 80 in some studies [1], leading some authors to suggest that development of MBL might be inevitable in the extreme elderly [4, 17].
It is unknown whether MBL detection rates vary among different racial or ethnic groups, although rates of CLL/SLL are known to vary among racial groups within the USA [18] as well as across global geographic regions [19]. Most studies that have evaluated the prevalence of MBL have taken place in geographically limited and relatively homogenous populations, such as in Salamanca, Spain [1], Northern Italy [20], and the Midwestern United States (U.S.) [3]. Comparison of MBL detection rates between studies is challenging because of variable sensitivities of the assays employed [21]. To our knowledge, no prior study has directly compared rates of MBL detection across a broad geographic region or among racially diverse populations [2]. In this paper, we describe rates of detection of MBL, both CLL-like and non-CLL-like, in a geographically and demographically diverse population of older African-, White-, and Hispanic- American women.
Materials and methods
Study population and sample collection
For this study, 600 blood samples were randomly selected for flow cytometry evaluation out of a pool of 7481 successful blood draws undertaken as a part of the Women’s Health Initiative (WHI) Long Life Study (LLS). The WHI is a long-term national health study that enrolled a total of 161,808 community-dwelling, postmenopausal women from 1993 to 1998. The WHI was designed to study strategies for the prevention and control of common causes of morbidity and mortality; details of the study design have been published previously [22]. Briefly, 93,676 women were enrolled in the observational arm of the study and 68,132 were enrolled in three clinical trials of hormone therapy, dietary modification, and calcium/vitamin D supplementation. Participants were enrolled through 40 clinical centers distributed widely throughout the USA, with targeted enrollment of minority women.
A subset of the WHI participants (7875 women) were subsequently enrolled into the WHI-LLS and had additional biospecimens, physiometric, and questionnaire data collected between March 2012 and May 2013. Enrollment criteria for the WHI-LLS have been described previously [23]. Briefly, all surviving Hormone Trial participants followed through 2010 were eligible, as well as additional African American and Hispanic/Latino participants that met defined enrollment criteria; women residing in an institution or unable/unwilling to provide informed consent were excluded. Blood was collected at locations across the USA using a standardized protocol between March 2012 and May 2013 (Examination Management Services, Inc.) Fresh peripheral blood samples were packaged in Styrofoam with cold packs and were sent overnight to a central testing facility at the Seattle Cancer Care Alliance (SCCA) in Seattle, WA. This ancillary study was reviewed and approved by the human subjects division at the University of Washington.
Flow cytometry
In this ancillary study to the WHI-LLS, a random sample of 600 residual fresh peripheral blood specimens (single tube, following CBC analysis) were transported to the University of Washington Medical Center’s (UWMC’s) flow cytometry laboratory and high-sensitivity, multi-parameter flow cytometry was performed utilizing a modified four-laser, multi-color Becton-Dickinson (BD; San Jose, CA) LSRII flow cytometer. All of the flow cytometry studies were performed within 72 h of sample collection between June 2012 and February 2013.
A full 1 mL of sample (or all of the remaining sample) was bulk-lysed and run with the following B lymphocyte antibody panel to evaluate B lymphocyte subsets: CD45 (APC-H7), CD20 (V450), kappa (F), lambda (PE), CD23 (ECD), CD5 (PC5.5), CD19 (BV650), CD38 (A594), CD10 (APC), CD27 (PC7), CD3 (APC-A700). The first 150 uL of sample was run collecting all events. The remainder of the evaluation collected events in the B lymphocyte gate only in order to evaluate for the presence of very small clonal B lymphocyte populations; this procedure was designed to achieve analytical sensitivity comparable to that reported by other high-sensitivity assays [1]. Research technologists quantified categories of circulating cells based on a predefined population-based gating strategy using Woodlist software (created by BW). Each case was also evaluated by a hematopathologist (KE) to confirm the gating strategy and the presence or absence of an MBL population.
Lymphocytes were defined as events expressing bright CD45 with low side-scatter, and B cells were defined as CD19-positive lymphocytes lacking CD3 expression. CLL-like MBL was defined as a distinct cohesive population of B cells representing at least 30 events and expressing CD5 along with dim expression of CD20 and surface light chain (biclonal or monoclonal). The large majority of these populations also expressed both CD23 and CD27. All non-CLL-like MBL populations were evaluated together as a single group, defined as a distinct cohesive population of B cells representing at least 30 events that showed light chain restriction and normal intensity of CD20 expression, regardless of expression of CD5.
Demographic characteristics
A broad array of demographic and epidemiologic characteristics were collected from each participant in the WHI at enrollment, as has been described previously [22]. Race was indicated by self-report at the time of study enrollment, and included the categories White, Black, Hispanic, Asian/Pacific Islander, and other. Smoking status (present, former, never), USA region of residence (Northeast, South, Midwest, West), and income strata (divided into six income categories: <10,000; 10,000–19,000; 20,000–34,999; 35,000–49,999; 50,000–74,999; and >75,000) were based on self-reported data collected at the time of initial enrollment in the WHI. Additional physiometric data including height and weight were recorded at the time of enrollment in the LLS. BMI was calculated using these parameters. Age was calculated based on the date of the participant’s blood draw and date of birth.
Statistical analysis
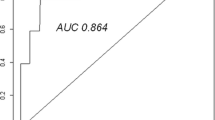
Demographic characteristics and MBL detection were summarized as proportions. Age-corrected detection rates (with 95 % CI) were estimated separately for total MBL, CLL-like MBL, and non-CLL-like MBL among the three racial groups. Race-corrected detection rates (with 95 % CI) were estimated for three different age brackets (64–74 years, 75–84 years, and 85 years and older) for total MBL, CLL-like MBL, and non-CLL-like MBL. Multivariate log-binomial regression models [24] were used to estimate risk (prevalence) ratios and 95 % confidence intervals for total MBL or MBL subtypes after adjusting for the effects of covariates, including age (continuous variable), race, smoking status, income level, US geographic region, and BMI. These regression analyses were performed twice, first correcting for only age or race and secondarily correcting for all covariates. All analyses were performed using Stata v13.0.
Results
Overall, 46.8 % of the participants were White, 37.3 % African American, and 15.8 % Hispanic American; no Asian American women were enrolled. The majority of the participants were over the age of 75 (62.6 %) and 41.3 % were 80 years of age or older. Nineteen participants (3.2 %) were 90 or older. There were significant differences in the age distribution among the three racial groups, as summarized in Table 1, reflecting the enrollment criteria of the parent WHI-LLS study. Flow cytometry data on 597 random blood samples was included in the analyses. Three samples were excluded because B cell antigen expression data could not be interpreted due to suboptimal antibody binding.
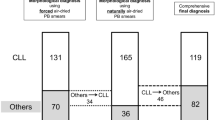
MBL was detected in a total of 155 (26.0 %) participants. A fifth (20.9 %) of the participants had a single MBL population with a classic CLL-like immunophenotype while 30 participants (5 %) had a non-CLL-like MBL. In total, eight (1.3 %) participants had both CLL-like and non-CLL-like MBL populations and one participant had two immunophenotypically distinct CD5-negative MBL populations with different light chain restrictions. Of the 30 participants with non-CLL-like MBL populations, seven expressed some level of CD5 with normal intensity of CD20 expression; in all of these cases, the CD5 expression was either dim or of variable intensity. The majority of the non-CLL-like populations also expressed light chain at a normal intensity level, and expression of CD23 and CD27 was variable. Overall, 44.4 % of the CLL-like MBL populations were biclonal, i.e., included subsets with both kappa and lambda light chain expression. Examples of the flow cytometry data are shown in Fig. 1.
Examples of flow cytometry data from five cases with clonal B cell subsets (lambda: yellow; kappa: pale blue; MBL clone: dark blue or red; the MBL populations are emphasized in all images except a. a CLL-like, monoclonal kappa. b CLL-like, biclonal. c MZL-like with CD5, monoclonal kappa. d MZL-like, CD5- and CD27-negative, monoclonal kappa. e Two MBL, one MZL-like, CD5-negative and CD27-positive (monoclonal lambda, colored red) and one CLL-like (monoclonal kappa, colored dark blue)
The MBL populations detected ranged in size from 0.003 % of the total lymphocyte population to up to 74 %. The large majority of the MBL populations were very small, regardless of the immunophenotype. Among CLL-like MBL, 81.2 % represented less than 1 % of the total lymphocytes and 22.6 % represented less than 0.01 %; the CLL-like MBL population represented >50 % of the leukocytes in only three participants. The 23 MBL populations that were CD5-negative tended to be somewhat larger than CD5-positive MBL; however, this may be secondary to their less distinct immunophenotypes. These populations ranged in size from 0.12 to up to 33.5 % of the total lymphocytes, with only 30.4 % representing less than 1 % of the lymphocytes. There were seven MBL populations detected having a CD5-positive (typically dim) immunophenotype with a normal intensity of CD20 expression and dim to absent CD23. These populations ranged in size from 0.02 to 2.9 % of the lymphocytes, and all but one represented less than 1 % of the lymphocytes.
Rates of MBL detection increased by age for both CLL-like and non-CLL-like MBL. In the uncorrected data, MBL were detected in 19.7 % of participants aged 64–74 years, 25.4 % aged 75–84, and 41.2 % of those aged 85 to 94. Rates of detection of MBL with a non-CLL-like immunophenotype rose even more markedly with age. While these populations were only present in 0.9 % of those in the youngest age bracket (64–74), they were present in 5.5 % of those aged 75–84 and in 12.7 % of those aged 85–94. Because of the significant variation in the age distribution among the three racial groups (see Table 1), the age data is corrected for race (Fig. 2). Following correction, MBL was detected in 24.1 % (95 % CI 17.4–30.8 %) of those aged 64–74, 24.6 % (95 % CI 19.5–30.0 %) of those 75–84 years old, and 49.5 % (95 % CI 40.1–59.0 %) of those 85 and older. Compared with the youngest age group (64–74 years), the race-adjusted prevalence ratio for total MBL was 1.66 (95 % CI 1.11–2.48; P = 0.014) for the 85 and older age group (Table 2). By comparison, the race-adjusted prevalence ratio for non-CLL-like MBL was 6.6 (95 % CI 1.5–28.8) among 75 to 84 years old (P = 0.013) and 15.8 (95 % CI 3.4–72.4) among those 85 and older (P = 0.0004), when compared with the youngest age group (64–74 years).
Nineteen participants were over the age of 90, and the crude prevalence of MBL detection in this group was 31.6 % including 10.5 % with a non-CLL-like immunophenotype (absolute numbers, not corrected for race). Among the 14 White participants over the age of 90, six (42.9 %) had an MBL detected (two of which had a non-CLL-like immunophenotype). No Hispanic women over the age of 90 were included in our dataset, and of the five African American women, none had an MBL identified.
Our data also revealed differences in MBL detection rates by race (Fig. 3). Compared with Whites, the age-adjusted prevalence ratio for total MBL was 0.56 (95 % CI 0.39–0.80; P .002) for African Americans and 0.90 (95 % CI 0.59–1.38; P .64) for Hispanic Americans. Race-specific rates of detection of MBL differed according to MBL immunophenotype. When corrected for age, the rate of detection of CLL-like MBL was 13.2 % (95 % CI 8.2–18.1 %) among African Americans, 36.0 % (95 % CI 27.4–44.5 %) among Hispanic Americans, and 30.1 % (95 % CI 23.7–36.6 %) among White participants. Age-corrected prevalence ratios for CLL-like MBL were 0.44 (95 % CI 0.29–0.67; P .0001) among African Americans, and 1.03 (95 % CI 0.67–1.59; P 0.89) among Hispanics, compared to Whites.
Although there was no statistically significant difference in detection rates of non-CLL-like MBL by race, there was a trend towards increased detection in African American women. When adjusted for age, detection of non-CLL-like MBL was highest among African Americans (7.3 %; 95 % CI 3.2–11.5 %), intermediate among Whites (4.5 %; 95 % CI 2.3–6.8 %), and lowest among Hispanics (1.9 %; 95 % CI 0–4.4 %). Age-corrected prevalence ratios for non-CLL-like MBL were 1.50 (95 % CI, 0.71–3.16; P .288) among African Americans and 0.83 (95 % CI 0.19–3.65; P 0.809) among Hispanics, relative to Whites.
In order to exclude the possibility that the apparent differences in MBL detection by age and race were secondary to other factors such as socioeconomic or smoking status, a multivariate model was created including the following variables: US geographic region, smoking status, income level, and BMI, as well as both race and age. In this model, race was the only independent risk factor for CLL-like MBL. Interestingly, age did not emerge as an independent risk factor for detection of CLL-like MBL, although it is noted that all of our participants were elderly (which is distinct from most prior MBL studies). In contrast, age but not race was independently associated with detection of non-CLL-like MBL. There was no significant association between detection of MBL (total or when restricted to CLL-like or non-CLL-like) and the other covariates including US geographic region, smoking status, income level, or BMI in a multivariate regression model correcting for both race and age (data not shown).
Discussion
Clonal B cell expansions were detected in about one quarter (26.0 %) of a multi-ethnic sample of older women from across the USA by highly sensitive flow cytometry. Once corrected for age, detection of any MBL was twice as likely in White and Hispanic American participants relative to African American participants. When taking immunophenotype into account, this difference in detection rate by race was restricted to those MBL having a CLL-like immunophenotype, while detection of non-CLL-like MBL was not statistically different across the three racial/ethnic groups. Non-CLL-like MBL showed a very strong association with advanced age, being present in ∼13 % of all participants over the age of 85 relative to only ∼1 % in those aged 64–74.
Our data provide some insight into the prevalence of MBL in the extreme elderly. Few individuals over the age of 90 have been included in prior reports [1, 4], but frequency of MBL detection appears to be very high in this age group based on limited data, being present in ∼50 % (n = 2) and 75 % (n = 4) participants over the age of 90 in data from northern Italy [20] and Spain [1], respectively. This has led to the suggestion by some authors that MBL would ultimately be detected in all individuals of advanced enough age if sensitive enough methods were utilized for detection [17]. However, a more recent study of 50 individuals over the age of 90 in New South Wales [25] identified MBL in only five participants (10 %), although the analytical sensitivity of the assay employed was likely lower than that employed in our study. Nineteen participants over the age of 90 were included in our study, and the absolute rate of MBL detection in this group was 31.6 %. While our data are not sufficient to fully address the question of MBL prevalence in those over the age of 90, they do suggest that MBL detection rates may not rise as markedly as limited data from earlier studies may have suggested.
The demonstration by our study that detection of CLL-like MBL varies by race is not surprising, given that CLL-like MBL is known to be a necessary precursor condition for CLL/SLL. Rates of CLL/SLL vary dramatically across global geographic regions, having particularly low rates in Asian countries like Japan and China [19]. Reasons for this variation are not fully explained, but appear to be largely attributable to genetic differences and not environmental factors [26]; for example, this altered risk of developing CLL/SLL is maintained in migrant populations [27, 28]. Similarly, the risk of CLL/SLL varies significantly within racial groups in the USA, with lower risk in Asian as well as African Americans [18].
Family history is a well-characterized risk factor for CLL/SLL, which is believed to have one of the strongest heritable genetic components of all common malignancies [19, 29]. Familial CLL/SLL is similar in most respects to sporadic CLL/SLL, although the age of onset of both MBL and CLL/SLL is typically younger in high-risk cohorts and MBL is more common in high risk families [19, 30]. While MZL does not have as strong a familial/genetic association as CLL/SLL, there is some evidence of racial variation, including a lower incidence in Blacks based on the United States Surveillance Epidemiology and End Results (SEER) Program data [31]. In our data, the risk of MBL was similar between women identifying as White and Hispanic. It is noted that designation of race/ethnicity was based on self-report at the time of study enrollment, and that participants were only allowed to self-designate a single race (e.g., could select either Hispanic or African ancestry, but not both).
To our knowledge, our overall detection rate is the highest yet reported in any study; this high rate of detection was anticipated based on the sensitivity of our assay and the advanced age of our participants. Nieto et al. employed a flow cytometry assay with similar sensitivity and identified MBL populations in >20 % of participants over the age of 65, similar to our findings [1].
Unlike previous reports, our study allows for a direct comparison of differences in MBL detection by race/ethnicity across a wide geographic region with all of the flow cytometry studies performed in a single flow cytometry laboratory using an identical and highly sensitive protocol. Strengths of this study also include the quality of the demographic and epidemiologic data collected on the subjects as participants in both the WHI and LLS clinical trials. Limitations of this study include that the sample collection was limited to women. While some studies have shown a mild male predominance in MBL detection [3, 32], others have found similar rates between men and women [1, 20, 25]. In addition, the opportunistic nature of the study defined the demographic distribution of the participants (e.g., no Asian women were enrolled in the LLS).
It is noted that in some prior studies, MBL has been defined as a B cell population with a characteristic immunophenotype representing greater than 50 events [1, 3], whereas we used 30 events to define an MBL population in the present study. We employed a population-based gating approach similar to that used in our clinical flow cytometry laboratory for minimal residual disease detection [33–35], and also included CD3 in our gating strategy to definitively exclude T cells. Based on these factors, we felt that 30 events was a more appropriate threshold than 50 in this study. In total, 16 of the MBL samples had 30–49 events with the MBL phenotype. All had a CLL-like immunophenotype, and exclusion of these cases would result in an overall MBL detection rate of 22.8 %. All of the non-CLL-like populations represented greater than 50 total events, and therefore the detection rate of non-CLL-like MBL would be unchanged.
Monoclonal B cell populations having a non-CLL-like immunophenotype were relatively common in our study, likely reflecting both the advanced age of our participants and the particular antibody combination we employed. These MBL populations tend to be less distinct immunophenotypically and may have been more readily identified in our 11-color flow cytometry assay than using the antibody combinations employed in other studies [20, 25]. Further, our population-based gating strategy may allow for detection of smaller CD5-negative clonal subsets than would be detected based on a skewing of the kappa to lambda ratio alone. Still, the prevalence of non-CLL-like MBL reported in this study may remain an underestimate secondary to the limits of sensitivity inherent in antibody combinations primarily designed to detect CLL-like populations.
Interestingly, while CLL/SLL often presents with only a leukemic component (involving blood and marrow but not tissue), MZL typically arises in tissue sites. Recently, Xochelli et al. reported that clonal B cell populations with immunophenotypic features similar to MZL but restricted to blood and marrow follow a relatively indolent clinical course, regardless of the level of peripheral blood or bone marrow involvement [8]. Because these cases also lack a clear diagnostic category according to existing (2008) WHO criteria, the authors argued for the creation of a new provisional diagnostic category that would encompass both MBL with immunophenotypic features typical of MZL, as well as cases that would currently be categorized as MZL but with involvement limited to the blood and marrow. They described the features of these populations in the clinical setting and proposed they be termed clonal B cell lymphocytosis of potential marginal-zone origin (CBL-MZ) [8].
Our population-based data provide evidence that non-CLL-like MBL populations are much more frequently detected in the blood in the most advanced elderly (at least among women), particularly among those greater than 85. Increased detection of non-CLL-like MBL in the very elderly has been noted previously [3]. Incidence of MZL itself also increases with age, but not to the degree typically associated with CLL/SLL. However, MZL is known to develop in states of chronic, ongoing antigen stimulation, in particular as a response to specific bacterial (H. pylori, C. psittaci) or viral (Hepatitis C) infections, as well as in other states of chronic inflammation like chronic sialadinitis. It has also recently been noted that CD5-negative MBL subsets may be overrepresented in hospital-based setting, perhaps reflecting transient immune stimulation in that setting [36]. It is possible that some change in the immune milieu in advanced age may specifically promote these non-CLL-like clonal expansions, given the increasingly recognized alterations in immune function occur in the very elderly [14–16]. Further research is necessary to investigate any potential relationship between non-CLL-like MBL or so-called CBL-MZ and chronic antigen stimulation and/or altered immune function in the elderly.
Our data add to a growing body of evidence suggesting that detection of small clonal B cell populations is common in the peripheral blood of elderly individuals, and provide new evidence that rates of detection of MBL vary among different racial/ethnic groups. We found that detection of CLL-like MBL is twice as likely in White and Hispanic American participants relative to African Americans, and future studies addressing the prevalence of MBL should be cognizant of this racial variation.
Further, we believe that these data provide additional support for regarding non-CLL-like clonal expansions of potential marginal zone origin as an entity distinct from either CLL-like MBL or frank marginal zone lymphoma. Caution is warranted in labeling such clonal expansions as ‘lymphoma,’ particularly in the elderly, and diagnostic criteria should be established to guide management decisions for non-CLL-like clonal B cell expansions, similar to those currently in place to establish a diagnosis of CLL/SLL [37].
References
Nieto WG, Almeida J, Romero A, Teodosio C, Lopez A, Henriques AF, Sanchez ML, Jara-Acevedo M, Rasillo A, Gonzalez M, Fernandez-Navarro P, Vega T, Orfao A, Primary Health Care Group of Salamanca for the Study of MBL (2009) Increased frequency (12%) of circulating chronic lymphocytic leukemia-like B-cell clones in healthy subjects using a highly sensitive multicolor flow cytometry approach. Blood 114(1):33–37. doi:10.1182/blood-2009-01-197368
Shim YK, Middleton DC, Caporaso NE, Rachel JM, Landgren O, Abbasi F, Raveche ES, Rawstron AC, Orfao A, Marti GE, Vogt RF (2010) Prevalence of monoclonal B-cell lymphocytosis: a systematic review. Cytometry B Clin Cytom 78(Suppl 1):S10–18. doi:10.1002/cyto.b.20538
Shim YK, Rachel JM, Ghia P, Boren J, Abbasi F, Dagklis A, Venable G, Kang J, Degheidy H, Plapp FV, Vogt RF, Menitove JE, Marti GE (2014) Monoclonal B-cell lymphocytosis in healthy blood donors: an unexpectedly common finding. Blood 123(9):1319–1326. doi:10.1182/blood-2013-08-523704
Scarfo L, Dagklis A, Scielzo C, Fazi C, Ghia P (2010) CLL-like monoclonal B-cell lymphocytosis: are we all bound to have it? Semin Cancer Biol 20(6):384–390. doi:10.1016/j.semcancer.2010.08.005
Shanafelt TD, Ghia P, Lanasa MC, Landgren O, Rawstron AC (2010) Monoclonal B-cell lymphocytosis (MBL): biology, natural history and clinical management. Leukemia 24(3):512–520. doi:10.1038/leu.2009.287
Mulligan CS, Thomas ME, Mulligan SP (2011) Monoclonal B-lymphocytosis: demographics, nature and subclassification in 414 community patients. Leuk Lymphoma 52(12):2293–2298. doi:10.3109/10428194.2011.598250
Jaso JM, Yin CC, Wang SA, Miranda RN, Jabcuga CE, Chen L, Medeiros LJ (2013) Clinicopathologic features of CD5-positive nodal marginal zone lymphoma. Am J Clin Pathol 140(5):693–700. doi:10.1309/AJCPEMVXES72DUIF
Xochelli A, Kalpadakis C, Gardiner A, Baliakas P, Vassilakopoulos TP, Mould S, Davis Z, Stalika E, Kanellis G, Angelopoulou MK, McIver-Brown N, Ibbotson R, Sachanas S, Korkolopoulou P, Athanasiadou A, Anagnostopoulos A, Papadaki HA, Papadaki T, Stamatopoulos K, Pangalis GA, Oscier D (2014) Clonal B-cell lymphocytosis exhibiting immunophenotypic features consistent with a marginal-zone origin: is this a distinct entity? Blood 123(8):1199–1206. doi:10.1182/blood-2013-07-515155
Rawstron AC, Bennett FL, O’Connor SJ, Kwok M, Fenton JA, Plummer M, de Tute R, Owen RG, Richards SJ, Jack AS, Hillmen P (2008) Monoclonal B-cell lymphocytosis and chronic lymphocytic leukemia. N Engl J Med 359(6):575–583. doi:10.1056/NEJMoa075290
Landgren O, Albitar M, Ma W, Abbasi F, Hayes RB, Ghia P, Marti GE, Caporaso NE (2009) B-cell clones as early markers for chronic lymphocytic leukemia. N Engl J Med 360(7):659–667. doi:10.1056/NEJMoa0806122
Rawstron AC, Shanafelt T, Lanasa MC, Landgren O, Hanson C, Orfao A, Hillmen P, Ghia P (2010) Different biology and clinical outcome according to the absolute numbers of clonal B-cells in monoclonal B-cell lymphocytosis (MBL). Cytometry B Clin Cytom 78(Suppl 1):S19–23. doi:10.1002/cyto.b.20533
Caporaso NE, Marti GE, Landgren O, Azzato E, Weinberg JB, Goldin L, Shanafelt T (2010) Monoclonal B cell lymphocytosis: clinical and population perspectives. Cytometry B Clin Cytom 78(Suppl 1):S115–119. doi:10.1002/cyto.b.20555
Ponzoni M, Ghia P (2014) Clonal B-cell lymphocytosis: a new member? Blood 123(8):1118–1119. doi:10.1182/blood-2013-12-543330
Arnold CR, Wolf J, Brunner S, Herndler-Brandstetter D, Grubeck-Loebenstein B (2011) Gain and loss of T cell subsets in old age—age-related reshaping of the T cell repertoire. J Clin Immunol 31(2):137–146. doi:10.1007/s10875-010-9499-x
Sansoni P, Vescovini R, Fagnoni F, Biasini C, Zanni F, Zanlari L, Telera A, Lucchini G, Passeri G, Monti D, Franceschi C, Passeri M (2008) The immune system in extreme longevity. Exp Gerontol 43(2):61–65. doi:10.1016/j.exger.2007.06.008
Naylor K, Li G, Vallejo AN, Lee WW, Koetz K, Bryl E, Witkowski J, Fulbright J, Weyand CM, Goronzy JJ (2005) The influence of age on T cell generation and TCR diversity. J Immunol 174(11):7446–7452
Almeida J, Nieto WG, Teodosio C, Pedreira CE, Lopez A, Fernandez-Navarro P, Nieto A, Rodriguez-Caballero A, Munoz-Criado S, Jara-Acevedo M, Romero A, Orfao A, Primary Health Care Group of Salamanca for the Study of MBL (2011) CLL-like B-lymphocytes are systematically present at very low numbers in peripheral blood of healthy adults. Leukemia 25(4):718–722. doi:10.1038/leu.2010.305
Shenoy PJ, Malik N, Sinha R, Nooka A, Nastoupil LJ, Smith M, Flowers CR (2011) Racial differences in the presentation and outcomes of chronic lymphocytic leukemia and variants in the United States. Clin Lymphoma Myeloma Leuk 11(6):498–506. doi:10.1016/j.clml.2011.07.002
Goldin LR, Slager SL, Caporaso NE (2010) Familial chronic lymphocytic leukemia. Curr Opin Hematol 17(4):350–355. doi:10.1097/MOH.0b013e328338cd99
Ghia P, Prato G, Scielzo C, Stella S, Geuna M, Guida G, Caligaris-Cappio F (2004) Monoclonal CD5+ and CD5- B-lymphocyte expansions are frequent in the peripheral blood of the elderly. Blood 103(6):2337–2342. doi:10.1182/blood-2003-09-3277
Nieto WG, Almeida J, Teodosio C, Abbasi F, Allgood SD, Connors F, Rachel JM, Ghia P, Lanasa MC, Rawstron AC, Orfao A, Caporaso NE, Hanson CA, Shim YK, Vogt RF, Marti GE (2010) Commentary: comparison of current flow cytometry methods for monoclonal B cell lymphocytosis detection. Cytometry B Clin Cytom 78(Suppl 1):S4–9. doi:10.1002/cyto.b.20556
Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, Johnson KC, Proulx-Burns L, Pastore L, Criqui M, Daugherty S, Morbidity WHI, Mortality C (2003) Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol 13(9 Suppl):S122–128
Sriram U, LaCroix AZ, Barrington WE, Corbie-Smith G, Garcia L, Going SB, LaMonte MJ, Manson JE, Sealy-Jefferson S, Stefanick ML, Waring ME, Seguin RA (2016) Neighborhood Walkability and Adiposity in the Women’s Health Initiative Cohort. American journal of preventive medicine. doi:10.1016/j.amepre.2016.04.007
Deddens JA, Petersen MR (2008) Approaches for estimating prevalence ratios. Occup Environ Med 65(7):481. doi:10.1136/oem.2007.034777, 501-486
Soosapilla A, Pepperell D, Best G, Brizzi C, Mulligan CS, van Bilsen N, Mulligan SP (2015) Monoclonal B-lymphocytosis in patients aged over 90 years is common but not inevitable, and has a prevalence comparable to that in individuals aged 65-90 years. Leukemia & lymphoma:1-3. doi:10.3109/10428194.2014.976822
Yang SM, Li JY, Gale RP, Huang XJ (2015) The mystery of chronic lymphocytic leukemia (CLL): Why is it absent in Asians and what does this tell us about etiology, pathogenesis and biology? Blood Rev 29(3):205–213. doi:10.1016/j.blre.2014.12.001
Pan JW, Cook LS, Schwartz SM, Weis NS (2002) Incidence of leukemia in Asian migrants to the United States and their descendants. Cancer Causes Control 13(9):791–795
Mak V, Ip D, Mang O, Dalal C, Huang S, Gerrie A, Gillan T, Ramadan KM, Toze C, Au WY (2014) Preservation of lower incidence of chronic lymphocytic leukemia in Chinese residents in British Columbia: a 26-year survey from 1983 to 2008. Leuk Lymphoma 55(4):824–827. doi:10.3109/10428194.2013.827785
Goldin LR, Pfeiffer RM, Li X, Hemminki K (2004) Familial risk of lymphoproliferative tumors in families of patients with chronic lymphocytic leukemia: results from the Swedish family-cancer database. Blood 104(6):1850–1854. doi:10.1182/blood-2004-01-0341
Goldin LR, Lanasa MC, Slager SL, Cerhan JR, Vachon CM, Strom SS, Camp NJ, Spector LG, Leis JF, Morrison VA, Glenn M, Rabe KG, Achenbach SJ, Algood SD, Abbasi F, Fontaine L, Yau M, Rassenti LZ, Kay NE, Call TG, Hanson CA, Weinberg JB, Marti GE, Caporaso NE (2010) Common occurrence of monoclonal B-cell lymphocytosis among members of high-risk CLL families. Br J Haematol 151(2):152–158. doi:10.1111/j.1365-2141.2010.08339.x
Khalil MO, Morton LM, Devesa SS, Check DP, Curtis RE, Weisenburger DD, Dores GM (2014) Incidence of marginal zone lymphoma in the United States, 2001-2009 with a focus on primary anatomic site. Br J Haematol 165(1):67–77. doi:10.1111/bjh.12730
Dagklis A, Fazi C, Sala C, Cantarelli V, Scielzo C, Massacane R, Toniolo D, Caligaris-Cappio F, Stamatopoulos K, Ghia P (2009) The immunoglobulin gene repertoire of low-count chronic lymphocytic leukemia (CLL)-like monoclonal B lymphocytosis is different from CLL: diagnostic implications for clinical monitoring. Blood 114(1):26–32. doi:10.1182/blood-2008-09-176933
Wood B (2006) 9-color and 10-color flow cytometry in the clinical laboratory. Arch Pathol Lab Med 130(5):680–690. doi:10.1043/1543-2165(2006)130[680:CACFCI]2.0.CO;2
Chen X, Xie H, Wood BL, Walter RB, Pagel JM, Becker PS, Sandhu VK, Abkowitz JL, Appelbaum FR, Estey EH (2015) Relation of clinical response and minimal residual disease and their prognostic impact on outcome in acute myeloid leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. doi:10.1200/JCO.2014.58.3518
Bar M, Wood BL, Radich JP, Doney KC, Woolfrey AE, Delaney C, Appelbaum FR, Gooley TA (2014) Impact of minimal residual disease, detected by flow cytometry, on outcome of myeloablative hematopoietic cell transplantation for acute lymphoblastic leukemia. Leukemia research and treatment 2014:421723. doi:10.1155/2014/421723
Voigtlaender M, Vogler B, Trepel M, Panse J, Jung R, Bokemeyer C, Bacher U, Binder M (2015) Hospital population screening reveals overrepresentation of CD5(-) monoclonal B-cell lymphocytosis and monoclonal gammopathy of undetermined significance of IgM type. Ann Hematol 94(9):1559–1565. doi:10.1007/s00277-015-2409-9
Marti GE, Rawstron AC, Ghia P, Hillmen P, Houlston RS, Kay N, Schleinitz TA, Caporaso N, International Familial CLLC (2005) Diagnostic criteria for monoclonal B-cell lymphocytosis. Br J Haematol 130(3):325–332. doi:10.1111/j.1365-2141.2005.05550.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Financial support
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
Potential conflicts of interest and disclosures
The authors have no potential conflicts of interest to declare. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 62 kb)
Rights and permissions
About this article
Cite this article
Edlefsen, K.L., Cherian, S., De Roos, A.J. et al. Detection of non-CLL-like monoclonal B cell lymphocytosis increases dramatically in the very elderly, while detection of CLL-like populations varies by race: findings in a multiethnic population-based cohort of elderly women. Ann Hematol 95, 1695–1704 (2016). https://doi.org/10.1007/s00277-016-2760-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-016-2760-5