Abstract
This nationwide population-based study assessed trends in treatment, trial participation and survival among 1833 adult patients diagnosed with acute lymphoblastic leukemia (ALL) in the Netherlands between 1989 and 2012 reported to the Netherlands Cancer Registry. Patients were categorized into four periods and five age groups (18–24, 25–39, 40–59, 60–69 and ⩾70 years). The application of allogeneic stem cell transplantation (alloSCT), particularly reduced-intensity conditioning (RIC) alloSCT, increased over time up to age 70 years. The inclusion rate in the trials was 67, 66, 55, 58 and 0% for the five age groups. Survival improved over time for patients below 70 years. Five-year relative survival in the period 2007–2012 was 75, 57, 37, 22 and 5% for the five age groups. In that same period, 5-year overall survival among patients aged 18–39 years was 68% for the chemotherapy-alone group and 66% for the alloSCT group. For patients aged 40–69 years, the corresponding estimates were 24 and 41%. Pronounced survival improvement observed among patients aged 18–39 years might mainly be explained by implementation of pediatric-based regimens since 2005, whereas among patients aged 40–69 years, increased application of RIC-alloSCT has contributed significantly to the observed improvement. Outcome of patients aged ⩾70 remains unsatisfactory, indicating a need for specific trials for the elderly.
Similar content being viewed by others
Introduction
Acute lymphoblastic leukemia (ALL) is the most common childhood malignancy with an incidence of ~5 per 100 000, but ALL also occurs in adults, albeit less frequently, with an incidence of around 1 per 100 000.1 In children, 5-year overall survival (OS) has improved from 70 to 80% in the 1990s to ~90% in the 2000s,2, 3, 4, 5, 6 whereas outcome in adults is less favorable, especially in patients above age 40 years.1, 7
Before 2000, the intensity of treatment varied markedly between pediatric and adult treatment protocols.8 Major differences include the dose-intensity of non-myelotoxic therapy and the strict timing of subsequent courses of chemotherapy, which was more cautiously adhered to in pediatric patients. Therefore, to improve outcome in adult patients, treatment strategies were developed that incorporate consolidation and intensification courses based on pediatric protocols.9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Results of that approach in the context of clinical trials showed significantly improved survival among adolescents and young adults compared with similarly aged patients treated with former, less intensive protocols. Furthermore, improved survival was also observed upon incorporation of allogeneic stem cell transplantation (alloSCT) in the consolidation phase of treatment in patients having obtained a hematological remission following conventional remission-induction therapy.19, 20 Also, more recently, the introduction of targeted therapy with tyrosine kinase inhibitors markedly improved remission rates and disease-free survival for patients with Philadelphia chromosome-positive ALL.21 Despite these improvements, adult patients still show worse outcome as compared with pediatric patients.
In clinical trials, there is often a selection bias noted to include healthier patients. Therefore, findings from clinical trials, although clearly essential, may not be entirely representative for the general patient population. Population-based studies can complement clinical trials by assessing whether findings from clinical trials translate into benefits for patients in routine practice.22 Currently, large population-based studies with long-term data on treatment, trial participation and survival in an unselected adult ALL population are lacking.
We have conducted a nationwide population-based study to assess trends in treatment, trial participation and survival among all adult patients with newly diagnosed ALL in the Netherlands between 1989 and 2012.
Patients and methods
The Netherlands Cancer Registry
Founded in 1989, the nationwide population-based Netherlands Cancer Registry (NCR), which is maintained and hosted by the Netherlands Comprehensive Cancer Organization, has a nationwide coverage of at least 95% of all malignancies in the Netherlands.23 All newly diagnosed malignancies in the Netherlands are reported to the NCR by the Nationwide Network of Histopathology and Cytopathology (PALGA) and the National Hospital Discharge Registry (LMR). Information on dates of birth and diagnosis, sex, hospital of diagnosis, disease topography and morphology, and treatment is routinely collected from the medical records by trained registrars of the NCR. Topography and morphology are coded using the International Classification of Diseases for Oncology. Information on last known status for all patients (alive, death or emigration) is obtained through linking the NCR to the nationwide population registries network.
Study population
We included all adult patients (aged 18 years or older) diagnosed with ALL between 1 January 1989 and 31 December 2012 from the NCR using the following International Classification of Diseases for Oncology third edition24 morphology codes: 9836 for precursor B-cell lymphoblastic leukemia, 9837 for precursor T-cell lymphoblastic leukemia and 9835 for precursor cell lymphoblastic leukemia, not otherwise specified. Lymphoblastic lymphoma was excluded. All patients were followed from the date of diagnosis until death, emigration or last follow-up (1 February 2014), whichever occurred first. Patients diagnosed at autopsy (n=3) were excluded. Detailed clinical data such as comorbidities, prognostic factors and remission rates were not available in the NCR.
Treatment
Treatment is registered in the NCR and defined as chemotherapy alone, chemotherapy followed by an SCT and supportive care only. The NCR does not contain information on the type of SCT (autologous or allogeneic), donor and conditioning regimen. To obtain this information, anonymous data were provided by the SCT Working Party of the Dutch-Belgian Hemato-Oncology Cooperative Trial Group (HOVON), which receives notification of all SCTs performed in the Netherlands, and subsequently linked to the NCR using the dates of birth and ALL diagnoses, as well as sex. In addition, information on the type of chemotherapy and the use of tyrosine kinase inhibitors was not available in the NCR.
Trial participation
The NCR does not contain information on trial participation. To obtain this information, anonymous data were provided by the HOVON and the European Organization for Research and Treatment of Cancer (EORTC) covering the accrual period between 1989 and 2007, and subsequently linked to the NCR using the dates of birth and ALL diagnosis, as well as sex (see Supplementary Table S1 for an overview of HOVON and EORTC ALL trials in the Netherlands). Data from ongoing trials from 2008 onwards were not available for this study.
Trial participation was analyzed for four age categories (18–24, 25–39, 40–59 and 60–70 years) and in periods when a trial was open for more than 6 months in every calendar year. Consecutive HOVON and EORTC ALL trials were available throughout the period 1989–2007 for patients up to age 60 years, whereas patients aged 60–70 years could only be enrolled in the HOVON 71 trial that was open from October 2005 to January 2008. There were no trials available for patients above age 70 years.
Statistical analyses
Relative survival rates (RSRs) with 95% confidence intervals (CIs) were calculated as a measure of disease-specific survival according to the cohort methodology.25 RS is defined as the ratio between the observed survival in the group of patients and the expected survival of a comparable group from the general population with respect to age, sex and period. Expected survival was calculated using the Ederer 2 method from the Dutch population life tables according to age, sex and period.26 RSRs were calculated up to 10 years from diagnosis for four calendar periods (1989–1994, 1995–2000, 2001–2006 and 2007–2012), five age categories (18–24, 25–39, 40–59, 60–69 and ⩾70 years), sex and ALL subtype. The actuarial (OS) survival was estimated using the Kaplan–Meier method for treatment by age and calendar period.
To assess linear trends in RS over time, a generalized linear model was used that assumed a Poisson distribution for the observed number of deaths.27 We also used this model to estimate the relative excess risk of mortality during the first 5 years after ALL diagnosis according to calendar period, sex and age at diagnosis after controlling for all these covariates simultaneously, along with years of follow-up. Estimates from this model are interpreted as relative excess mortality ratios (EMRs). The EMR for the reference category was set to 1; thus, an EMR of 1.50 implies 50% higher excess mortality compared with the reference category. A P-value <0.05 was considered statistically significant. All statistical analyses were performed with STATA version 13.1 (StataCorp, College Station, TX, USA).
Results
Demographic characteristics
A total of 1833 adult patients with ALL (median age, 49 years; 54% males) were diagnosed in the Netherlands between 1989 and 2012 (Table 1). The average age-standardized incidence of ALL remained stable over time (0.6 per 100 000; Table 1). The age-specific incidence rate slightly increased with age (Supplementary Figure S1). In the last calendar period, 7% of all cases were classified as ALL, not otherwise specified, whereas B- and T-cell lymphoblastic leukemia constituted 73% and 20% of the cases, respectively (Table 1 and Supplementary Figure S2). Sixty-four percent of patients were diagnosed and/or treated in university hospitals (data not shown).
Treatment
Information on treatment according to age and calendar period of diagnosis is shown in Figure 1. The application of autologous SCTs (autoSCTs) has become very uncommon in the most recent calendar period as compared with more earlier calendar periods. The application of alloSCT increased over time among patients up to age 70 years and was most prominent among age 25–39 and 40–59 years (63% and 54% in the most recent calendar period, respectively). The use of unrelated donors increased over time to up to 50% in the most recent calendar period for all age categories up to age 70 years (Supplementary Figure S3a). Recipients of an alloSCT age 40–69 years more frequently received reduced-intensity conditioning as compared with myeloablative conditioning (Supplementary Figure S3b). The use of chemotherapy alone among patients aged 18–70 years decreased with each calendar period, following the wider application of alloSCT over time. Treatment for patients aged 70 years or older remained essentially unchanged over time and mainly consisted of supportive care only.
Treatment of adult patients with ALL in the Netherlands according to calendar period of diagnosis and age at diagnosis. The table presents the proportion of patients receiving a particular treatment within a specific calendar period and age group. The absolute number of patients within a specific calendar period and age group is shown in Table 1. In the overall series, 323 (18%) patients received supportive care only, 874 (48%) chemotherapy alone, 178 (10%) autoSCT and 458 (25%) alloSCT.
Trial participation
The inclusion rate when a clinical ALL trial was open in the Netherlands was 67%, 66%, 55% and 58% for patients aged 18–24, 25–39, 40–59 and 60–70, respectively (Figure 2). Remarkably, 94%, 90%, 78% and 71% of patients in the above-mentioned four age groups who did not participate in a clinical trial still received intensive therapy, respectively (chemotherapy±auto- or alloSCT; Figure 2). There were no trials available for patients above age 70 years.
Trial participation of patients with ALL in the Netherlands according to age at diagnosis. The pie chart depicts the proportion of trial participation among patients aged (a) 18–24, (b) 25–39, (c) 40–59 and (d) 60–70 years. The bar-plot depicts the treatment given to patients who did not entered into a clinical trial. *Intensive therapy includes chemotherapy alone, auto- and alloSCT.
Information on comorbidity, performance status and leukemia risk is lacking in the NCR. Therefore, we cannot perform a robust comparative analysis to assess the outcome between the trial and non-trial population, as an analysis without correcting for the above-mentioned factors may yield biased outcomes.
Survival
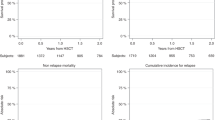
RS increased over time for the entire cohort (Supplementary Figure 4). RS according to age and calendar period of diagnosis is shown in Figure 3. One- and 5-year RSRs increased significantly for all age groups, although this increase was marginal for patients age 70 years or older. The improvement in 1-year RS was most pronounced in patients aged 40–69 years, whereas 5-year RS improved most prominently among patients up to age 40 years, especially in the last calendar period (2007–2012). Ten-year RSRs were similar to 5-year RSRs. Sex did not influence RSRs (data not shown). The overall 5-year RSRs (95% CI) was 38% (32–44%) for B-cell lymphoblastic leukemia and 46% (35–57%) for T-cell lymphoblastic leukemia in the last calendar period.
RSRs of patients with ALL in the Netherlands according to calendar period of diagnosis and age at diagnosis. RSRs are shown according to the following age categories: (a) 18–24 years, (b) 25–39 years, (c) 40–59 years, (d) 60–69 years and (e) ⩾70 years. The table presents the projected 1- and 5-year RSRs with 95% CIs according to calendar period of diagnosis. *P-value for linear trend from the calendar period 1989–1994 to the calendar period 2007–2012.
To evaluate possible contributions for the marked survival improvement among patients aged 18–39 years (Figures 3a and b and 4a), we estimated the OS for these patients according to treatment and calendar period. Five-year OS (95% CI) in the first and last calendar periods was 25% (17–34%) and 68% (55–79%) for patients who received chemotherapy alone (Figure 4b) and 46% (31–59%) and 66% (54–76%) for recipients of an alloSCT (Figure 4c), respectively. The improved outcome over time with chemotherapy alone was less pronounced in patients aged 40–69 years (Figure 4e) compared with patients aged 18–39 years (Figure 4b).
OS of patients up to age 70 years with ALL according to treatment and calendar period of diagnosis. Kaplan–Meier estimates of OS according to (a) the total cohort, (b) chemotherapy alone and (c) alloSCT for patients aged 18–39 years and Kaplan–Meier estimates of OS according to (d) the total cohort, (e) chemotherapy alone and (f) alloSCT for patients aged 40–69 years.
The adjusted EMRs in the 5 years after ALL diagnosis are shown in Table 2. Patients diagnosed in the calendar period 2007–2012 had a 56% lower excess mortality compared with patients diagnosed in the calendar period 1989–1994 (P<0.001). EMRs increased progressively with older age. There was no difference in EMRs between sexes (P=0.469).
Discussion
In this large, comprehensive population-based study, we show that survival over the past two decades has improved markedly among adult patients with ALL up to age 70 years, which improvement was most pronounced among patients up to age 40 years.
Survival improved by ~25% among patients up to age 40 years, which may be explained by the implementation of more intensified, pediatric-based chemotherapy, which was introduced in the Netherlands as from 2005.17 The Dutch protocol, which was evaluated in the phase II HOVON 70 study among patients up to age 40 years,17 was based on the French FRALLE pediatric ALL protocol.9 Results of the HOVON 70 and other clinical studies exploring an intensified pediatric regimen showed a significant improvement of survival compared with results of conventional adult chemotherapeutic strategies.14, 15, 16, 17 In the HOVON 70 study, 2-year OS was 72%,17 which was strikingly similar to that observed in our population-based series. Following the results of the HOVON 70 study, national guidelines set by HOVON recommend that a pediatric-based protocol should be applied to all patients up to the age of 40 years. Our results can only suggest that the marked improvement of OS is mainly explained by the introduction of pediatric-based chemotherapy in patients up to the age of 40 years.
Also, a significant survival improvement was observed among patients aged 40–69 years, although that improvement was not as pronounced as compared with patients up to the age of 40 years. Several possible explanations can be brought forward. First, although the current regimen in patients above age 40 years is less intensive as in young adult patients, a gradual intensification was also apparent in adult patients, but treatment-related toxicity and mortality were considerable and may have prevented a significant improvement on overall outcome.18, 28 Second, advanced age itself is a poor prognostic factor in ALL.29 Poor-risk molecular and cytogenetic aberrations are more abundantly observed in leukemic cells from older patients with ALL (e.g., Philadelphia chromosome positivity or complex aberrations30). In addition, older patients more often exhibit comorbidities,31 which predispose for non-leukemic toxicity and mortality.
Apart from intensified chemotherapy, other factors might be associated with better outcome among patients up to the age of 70 years, particularly the wider application of alloSCT. In the Netherlands, alloSCT is the consolidation therapy of choice in all adult ALL patients in first complete remission, whenever eligible. Although HLA-compatible sibling donors are available for only ~35% of patients,20 the wider use of alternative donors, including well-matched unrelated donors, has greatly contributed to a wider application of alloSCT. Moreover, poor-risk patients (defined as specific cytogenetic abnormalities, no complete remission after induction chemotherapy or high white blood cell count at diagnosis) may also benefit from an alternative donor, including cord blood or incompletely HLA-matched unrelated donors.32 Importantly, because of the introduction of received reduced-intensity conditioning alloSCT as from the early 2000s, treatment-related mortality associated with alloSCT has decreased, which has resulted in increased accessibility and a higher number of elderly patients proceeding to an allograft. Therefore, the increased application of alloSCT over time, as shown in this study, may have contributed considerably to the observed survival improvement. Of note, autoSCTs were virtually not applied in the most recent calendar period, mainly because of reports stating that there is no survival benefit of consolidation by autoSCT compared with chemotherapy alone.19, 20, 33 The use of tyrosine kinase inhibitors since the early 2000s has significantly improved complete remission rates and outcome in patients with Philadelphia chromosome-positive ALL, a subgroup previously known to be less susceptible to standard chemotherapy.34, 35, 36 However, consolidation in Philadelphia chromosome-positive patients by alloSCT is still recommended, as cure without allogeneic immunotherapy is unlikely.35 Collectively, improved survival among patients up to the age of 70 years may be attributed to more intensive chemotherapy, and also to increased application of alloSCT, the introduction of tyrosine kinase inhibitors, as well as improved supportive care.
Survival among patients aged 70 years or older shows marginal, if any, improvement over the past two decades. This is in line with results of several cooperative study groups, which showed that older patients fared poorly, partly because of disease biology and treatment-related morbidity and mortality.7, 28, 37, 38, 39 Currently, there is no evidence-based standard treatment regimen for older patients with ALL as most of them are unsuitable for current clinical trials either because of eligibility criteria or comorbidity.
Information on trial participation in adult ALL at a nationwide level are lacking. In our population-based study, 60% of patients up to the age of 70 years entered a clinical ALL trial if a trial was open for inclusion. This rate is similar with those from smaller series in France (2007–2009).40 It is remarkable that the majority of patients not included in a trial still receive intensive therapy, which suggests that inclusion criteria in current clinical trials might be too stringent.
Earlier population-based cancer registry studies in adult ALL were reported,1, 29, 41, 42, 43, 44, 45, 46, 47, 48 but most of these studies lacked information on treatment for individual patients.1, 41, 44, 45, 46, 47, 48 The strength of our population-based study includes the use of a nationwide population-based cancer registry with comprehensive data available (i.e., incidence, trial participation, treatment and survival) for individual patients over a 24-year period, which has enabled us to assess trends over time. In the Netherlands, all residents have equal access to health care as they are legally obliged to have a health-care insurance policy.49 In this regard, the NCR is a useful instrument to assess whether new therapeutic strategies translate into benefits for patients at the population level. Our study also has some limitations, including lack of detailed information on clinical (e.g., comorbidity), prognostic (e.g., cytogenetics, molecular analysis and minimal residual disease) and treatment characteristics (e.g., remission and relapse rates). Despite these limitations, cancer registries remain the gold standard for cancer surveillance in the general population.22
In conclusion, we show that survival of adult patients with ALL up to the age of 70 years has improved over the past two decades. Since the implementation of pediatric-guided chemotherapeutic regimens in 2005, survival for patients aged 18–39 years improved markedly. Despite improvements observed among patients aged 40 years or older, they still fare worse as compared with younger patients. Prevention of treatment-related toxicity and mortality, as well delineation of the intensification possibilities, remains important. In addition, using less toxic treatment approaches harboring specific mechanisms of action, such as monoclonal and bi-specific antibodies or engineered CAR T-cell therapy, are promising new developments. Last, participation of older patients in clinical trials should be encouraged to establish evidence-based treatment recommendations and also to offer older patients the newest therapeutic possibilities.
References
Dores GM, Devesa SS, Curtis RE, Linet MS, Morton LM . Acute leukemia incidence and patient survival among children and adults in the United States, 2001–2007. Blood 2012; 119: 34–43.
Silverman LB, Gelber RD, Dalton VK, Asselin BL, Barr RD, Clavell LA et al. Improved outcome for children with acute lymphoblastic leukemia: results of Dana-Farber Consortium Protocol 91-01. Blood 2001; 97: 1211–1218.
Arico M, Valsecchi MG, Rizzari C, Barisone E, Biondi A, Casale F et al. Long-term results of the AIEOP-ALL-95 trial for childhood acute lymphoblastic leukemia: insight on the prognostic value of DNA index in the framework of Berlin–Frankfurt–Muenster-based chemotherapy. J Clin Oncol 2008; 26: 283–289.
Kamps WA, van der Pal-de Bruin KM, Veerman AJ, Fiocco M, Bierings M, Pieters R . Long-term results of Dutch Childhood Oncology Group studies for children with acute lymphoblastic leukemia from 1984 to 2004. Leukemia 2010; 24: 309–319.
Stanulla M, Schrappe M . Treatment of childhood acute lymphoblastic leukemia. Semin Hematol 2009; 46: 52–63.
Hunger SP, Lu X, Devidas M, Camitta BM, Gaynon PS, Winick NJ et al. Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: a report from the children's oncology group. J Clin Oncol 2012; 30: 1663–1669.
Rowe JM, Buck G, Burnett AK, Chopra R, Wiernik PH, Richards SM et al. Induction therapy for adults with acute lymphoblastic leukemia: results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood 2005; 106: 3760–3767.
Dombret H, Cluzeau T, Huguet F, Boissel N . Pediatric-like therapy for adults with ALL. Curr Hematol Malig Rep 2014; 9: 158–164.
Boissel N, Auclerc MF, Lheritier V, Perel Y, Thomas X, Leblanc T et al. Should adolescents with acute lymphoblastic leukemia be treated as old children or young adults? Comparison of the French FRALLE-93 and LALA-94 trials. J Clin Oncol 2003; 21: 774–780.
de Bont JM, Holt B, Dekker AW, van der Does-van den Berg A, Sonneveld P, Pieters R . Significant difference in outcome for adolescents with acute lymphoblastic leukemia treated on pediatric vs adult protocols in the Netherlands. Leukemia 2004; 18: 2032–2035.
Hallbook H, Gustafsson G, Smedmyr B, Soderhall S, Heyman M, Swedish Adult Acute Lymphocytic Leukemia G. Treatment outcome in young adults and children >10 years of age with acute lymphoblastic leukemia in Sweden: a comparison between a pediatric protocol and an adult protocol. Cancer 2006; 107: 1551–1561.
Ramanujachar R, Richards S, Hann I, Goldstone A, Mitchell C, Vora A et al. Adolescents with acute lymphoblastic leukaemia: outcome on UK national paediatric (ALL97) and adult (UKALLXII/E2993) trials. Pediatr Blood Cancer 2007; 48: 254–261.
Stock W, La M, Sanford B, Bloomfield CD, Vardiman JW, Gaynon P et al. What determines the outcomes for adolescents and young adults with acute lymphoblastic leukemia treated on cooperative group protocols? A comparison of Children's Cancer Group and Cancer and Leukemia Group B studies. Blood 2008; 112: 1646–1654.
Ribera JM, Oriol A, Sanz MA, Tormo M, Fernandez-Abellan P, del Potro E et al. Comparison of the results of the treatment of adolescents and young adults with standard-risk acute lymphoblastic leukemia with the Programa Espanol de Tratamiento en Hematologia pediatric-based protocol ALL-96. J Clin Oncol 2008; 26: 1843–1849.
Huguet F, Leguay T, Raffoux E, Thomas X, Beldjord K, Delabesse E et al. Pediatric-inspired therapy in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia: The GRAALL-2003 Study. J Clin Oncol 2009; 27: 911–918.
Haiat S, Marjanovic Z, Lapusan S, Vekhoff A, Rio B, Corre E et al. Outcome of 40 adults aged from 18 to 55 years with acute lymphoblastic leukemia treated with double-delayed intensification pediatric protocol. Leuk Res 2011; 35: 66–72.
Rijneveld AW, van der Holt B, Daenen SM, Biemond BJ, de Weerdt O, Muus P et al. Intensified chemotherapy inspired by a pediatric regimen combined with allogeneic transplantation in adult patients with acute lymphoblastic leukemia up to the age of 40. Leukemia 2011; 25: 1697–1703.
Daenen S, van der Holt B, Dekker AW, Willemze R, Rijneveld AW, Biemond BJ et al. Intensive chemotherapy to improve outcome in patients with acute lymphoblastic leukemia over the age of 40: a phase II study for efficacy and feasibility by HOVON. Leukemia 2012; 26: 1726–1729.
Goldstone AH, Richards SM, Lazarus HM, Tallman MS, Buck G, Fielding AK et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the International ALL Trial (MRC UKALL XII/ECOG E2993). Blood 2008; 111: 1827–1833.
Cornelissen JJ, van der Holt B, Verhoef GE, van't Veer MB, van Oers MH, Schouten HC et al. Myeloablative allogeneic versus autologous stem cell transplantation in adult patients with acute lymphoblastic leukemia in first remission: a prospective sibling donor versus no-donor comparison. Blood 2009; 113: 1375–1382.
Thomas DA, O'Brien S, Cortes J, Kantarjian H . New approaches to the management of Philadelphia-chromosome-positive acute lymphocytic leukemia. Curr Hematol Malig Rep 2007; 2: 183–189.
Booth CM, Tannock IF . Evaluation of treatment benefit: randomized controlled trials and population-based observational research. J Clin Oncol 2013; 31: 3298–3299.
Schouten LJ, Hoppener P, van den Brandt PA, Knottnerus JA, Jager JJ . Completeness of cancer registration in Limburg, The Netherlands. Int J Epidemiol 1993; 22: 369–376.
Fritz AG, Percy C, Jack A, Sobin LH, Parkin DM (eds). International Classification of Diseases for Oncology, 3rd edn. World Health Organization: : Geneva, Switzerland, 2000.
Henson DE, Ries LA . The relative survival rate. Cancer 1995; 76: 1687–1688.
Ederer F, Heise H . Instructions to IBM 650 Programmers in Processing, Survival Computations. Methodological Note No. 10. End Results Evaluation Section. National Cancer Institute: Bethesda, MD, USA, 1959..
Dickman PW, Sloggett A, Hills M, Hakulinen T . Regression models for relative survival. Stat Med 2004; 23: 51–64.
Sive JI, Buck G, Fielding A, Lazarus HM, Litzow MR, Luger S et al. Outcomes in older adults with acute lymphoblastic leukaemia (ALL): results from the international MRC UKALL XII/ECOG2993 trial. Br J Haematol 2012; 157: 463–471.
Juliusson G, Karlsson K, Hallbook H . Population-based analyses in adult acute lymphoblastic leukemia. Blood 2010; 116: 1011; author reply 1012.
Moorman AV, Chilton L, Wilkinson J, Ensor HM, Bown N, Proctor SJ . A population-based cytogenetic study of adults with acute lymphoblastic leukemia. Blood 2010; 115: 206–214.
Gokbuget N . How I treat older patients with ALL. Blood 2013; 122: 1366–1375.
Bachanova V, Weisdorf D . Unrelated donor allogeneic transplantation for adult acute lymphoblastic leukemia: a review. Bone Marrow Transplant 2008; 41: 455–464.
Gupta V, Richards S, Rowe J . Acute Leukemia Stem Cell Transplantation Trialists' Collaborative G. Allogeneic, but not autologous, hematopoietic cell transplantation improves survival only among younger adults with acute lymphoblastic leukemia in first remission: an individual patient data meta-analysis. Blood 2013; 121: 339–350.
Cornelissen JJ, Carston M, Kollman C, King R, Dekker AW, Lowenberg B et al. Unrelated marrow transplantation for adult patients with poor-risk acute lymphoblastic leukemia: strong graft-versus-leukemia effect and risk factors determining outcome. Blood 2001; 97: 1572–1577.
Fielding AK, Rowe JM, Buck G, Foroni L, Gerrard G, Litzow MR et al. UKALLXII/ECOG2993: addition of imatinib to a standard treatment regimen enhances long-term outcomes in Philadelphia positive acute lymphoblastic leukemia. Blood 2014; 123: 843–850.
Brissot E, Labopin M, Beckers MM, Socie G, Rambaldi A, Volin L et al. Tyrosine kinase inhibitors improve long-term outcome of allogeneic hematopoietic stem cell transplantation for adult patients with Philadelphia chromosome positive acute lymphoblastic leukemia. Haematologica 2014; 100: 392–399.
Hussein KK, Dahlberg S, Head D, Waddell CC, Dabich L, Weick JK et al. Treatment of acute lymphoblastic leukemia in adults with intensive induction, consolidation, and maintenance chemotherapy. Blood 1989; 73: 57–63.
Larson RA, Dodge RK, Burns CP, Lee EJ, Stone RM, Schulman P et al. A five-drug remission induction regimen with intensive consolidation for adults with acute lymphoblastic leukemia: cancer and leukemia group B study 8811. Blood 1995; 85: 2025–2037.
Kantarjian HM, O'Brien S, Smith TL, Cortes J, Giles FJ, Beran M et al. Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol 2000; 18: 547–561.
Dechartres A, Chevret S, Lambert J, Calvo F, Levy V . Inclusion of patients with acute leukemia in clinical trials: a prospective multicenter survey of 1066 cases. Ann Oncol 2011; 22: 224–233.
Pulte D, Gondos A, Brenner H . Improvement in survival in younger patients with acute lymphoblastic leukemia from the 1980s to the early 21st century. Blood 2009; 113: 1408–1411.
Juliusson G, Karlsson K, Lazarevic V, Wahlin A, Brune M, Antunovic P et al. Hematopoietic stem cell transplantation rates and long-term survival in acute myeloid and lymphoblastic leukemia: real-world population-based data from the Swedish Acute Leukemia Registry 1997–2006. Cancer 2011; 117: 4238–4246.
Toft N, Schmiegelow K, Klausen TW, Birgens H . Adult acute lymphoblastic leukaemia in Denmark. A national population-based retrospective study on acute lymphoblastic leukaemia in Denmark 1998–2008. Br J Haematol 2012; 157: 97–104.
Pulte D, Redaniel MT, Jansen L, Brenner H, Jeffreys M . Recent trends in survival of adult patients with acute leukemia: overall improvements, but persistent and partly increasing disparity in survival of patients from minority groups. Haematologica 2013; 98: 222–229.
Pulte D, Jansen L, Gondos A, Katalinic A, Barnes B, Ressing M et al. Survival of adults with acute lymphoblastic leukemia in Germany and the United States. PLoS One 2014; 9: e85554.
Sant M, Minicozzi P, Mounier M, Anderson LA, Brenner H, Holleczek B et al. Survival for haematological malignancies in Europe between 1997 and 2008 by region and age: results of EUROCARE-5, a population-based study. Lancet Oncol 2014; 15: 931–942.
Guru Murthy GS, Venkitachalam R, Mehta P . Trends in survival outcomes of B-lineage acute lymphoblastic leukemia in elderly patients: analysis of Surveillance, Epidemiology, and End Results database. Leuk Lymphoma 2015, 1–5.
Redaniel MT, Pulte D, Jeffreys M . Survival disparities by age and country of diagnosis for patients with acute leukemia. Leuk Lymphoma 2015; e-pub ahead of print 6 March 2015; doi:10.3109/10428194.2015.1014358.
Dinmohamed AG, van Norden Y, Visser O, Posthuma EF, Huijgens PC, Sonneveld P et al. The use of medical claims to assess incidence, diagnostic procedures and initial treatment of myelodysplastic syndromes and chronic myelomonocytic leukemia in the Netherlands. Leuk Res 2015; 39: 177–182.
Acknowledgements
We thank the Dutch-Belgian Cooperative Trial Group for Hemato-Oncology (HOVON) and the European Organization for Research and Treatment of Cancer (EORTC) for permission to use the data on trial participation from their clinical ALL trials for this research. We also thank the HOVON stem cell transplantation (SCT) Working Party for permission to use data on SCTs for this study. The contents of this publication and methods used are solely the responsibility of the authors and do not necessarily represent the official views of the EORTC. This work was supported by grants from The Netherlands Organization for Health Research and Development (ZonMw; Grant No.152001007).
Author contributions
AGD, AS, MJ-L and AWR: designed the study; MvdM: analyzed the data; OV, AGD and JJC: collected the data; AGD and AS: wrote the manuscript with contributions from MvdM, OV, PS, JJC, MJ-L and AWR; and all authors read, commented on and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Dinmohamed, A., Szabó, A., van der Mark, M. et al. Improved survival in adult patients with acute lymphoblastic leukemia in the Netherlands: a population-based study on treatment, trial participation and survival. Leukemia 30, 310–317 (2016). https://doi.org/10.1038/leu.2015.230
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2015.230
- Springer Nature Limited
This article is cited by
-
Total body irradiation versus busulfan based intermediate intensity conditioning for stem cell transplantation in ALL patients >45 years—a registry-based study by the Acute Leukemia Working Party of the EBMT
Bone Marrow Transplantation (2023)
-
Real-world outcomes in elderly ALL patients with and without allogeneic hematopoietic stem cell transplantation: a single-center evaluation over 10 years
Annals of Hematology (2022)
-
Progress against childhood and adolescent acute lymphoblastic leukaemia in the Netherlands, 1990–2015
Leukemia (2021)
-
Incidence, socioeconomic deprivation, volume-outcome and survival in adult patients with acute lymphoblastic leukaemia in England
BMC Cancer (2018)
-
Treatment of Older Patients with Acute Lymphoblastic Leukaemia
Drugs & Aging (2018)