Abstract
Background/Objectives:
Evidence suggests diet, physical activity (PA) and sedentary behaviour cluster together in children, but research supporting an association with overweight/obesity is equivocal. Furthermore, the stability of clusters over time is unknown. The aim of this study was to examine the clustering of diet, PA and sedentary behaviour in Australian children and cross-sectional and longitudinal associations with overweight/obesity. Stability of obesity-related clusters over 3 years was also examined.
Subjects/Methods:
Data were drawn from the baseline (T1: 2002/2003) and follow-up waves (T2: 2005/2006) of the Health Eating and Play Study. Parents of Australian children aged 5–6 (n=87) and 10–12 years (n=123) completed questionnaires. Children wore accelerometers and height and weight were measured. Obesity-related clusters were determined using K-medians cluster analysis. Multivariate regression models assessed cross-sectional and longitudinal associations between cluster membership, and body mass index (BMI) Z-score and weight status. Kappa statistics assessed cluster stability over time.
Results:
Three clusters, labelled ‘most healthy’, ‘energy-dense (ED) consumers who watch TV’ and ‘high sedentary behaviour/low moderate-to-vigorous PA’ were identified at baseline and at follow-up. No cross-sectional associations were found between cluster membership, and BMI Z-score or weight status at baseline. Longitudinally, children in the ‘ED consumers who watch TV’ cluster had a higher odds of being overweight/obese at follow-up (odds ratio=2.8; 95% confidence interval: 1.1, 6.9; P<0.05). Tracking of cluster membership was fair to moderate in younger (K=0.24; P=0.0001) and older children (K=0.46; P<0.0001).
Conclusions:
This study identified an unhealthy cluster of TV viewing with ED food/drink consumption, which predicted overweight/obesity in a small longitudinal sample of Australian children. Cluster stability was fair to moderate over 3 years and is a novel finding. Prospective research in larger samples is needed to examine how obesity-related clusters track over time and influence the development of overweight and obesity.
Similar content being viewed by others
Introduction
In 2011–2012, one in four Australian children and adolescents aged 5–17 years were overweight or obese and while the prevalence has remained stable since 2007, it is nonetheless unacceptably high.1 It is well documented that many of these children will remain obese into adult life, increasing their risk of developing chronic diseases such as type 2 diabetes and sleep apnoea, as well as poor social outcomes.2, 3
Obesity aetiology is complex because of its multiplicity of determinants; however, high intake of energy-dense (ED) nutrient poor foods and high levels of sedentary behaviour are well-known modifiable promoters of weight gain.4, 5 Research also suggests that physical activity (PA) and intake of high fibre foods such as fruit and vegetables (FVs) may protect against weight gain.5
Emerging evidence suggests that obesity-related behaviours co-occur or cluster together in children and adolescents.6, 7, 8, 9, 10, 11 For example, in a sample of 1568 Australian adolescents aged approximately 12–16 years, Hardy et al.9 found that 51% of boys and 43% of girls had three or more obesity-related behavioural risk factors. Using cluster analysis (CA) to analyse data from 317 Flemish adolescents, Seghers and Rutten12 found four unique lifestyle clusters, in one of which unhealthy eating, low PA and high levels of screen-based sedentary behaviours clustered together. However, the evidence to support a synergistic effect of multiple obesity-related behaviours on the development of overweight and obesity is equivocal.13 Boone-Heinonen et al.14 and Huh et al.11 both found specific patterning of dietary, PA and sedentary behaviours to be associated with obesity prevalence, whereas other studies have found no association.7, 8, 12
Of the studies that have examined clustering of obesity-related behaviours,13 few have included a longitudinal study design,6, 14, 15, 16 have used an objective measure of weight status6, 8, 11, 14 or have examined younger children (<9 years of age).8, 15 Most studies have been cross-sectional, focusing on only two of the three behaviours17, 18, 19, 20 or included other health-related behaviours such as smoking or alcohol use.6, 21 Although understanding how obesity-related behaviours cluster together will help identify those children and adolescents most at risk of weight gain, it is also imperative to understand how these clusters change over time, and the critical periods where unhealthy behaviours increase. This information will help inform the timing of interventions, however, no study could be found that has examined the stability of clusters over time.
Therefore, this study aimed to fill gaps in the existing literature by determining whether clustering patterns of dietary, PA and sedentary behaviours in Australian children aged 5–6 and 10–12 years13 are associated with objectively measured weight status both cross-sectionally and prospectively, 3 years later. An additional aim was to examine the stability of these obesity-related behaviour clusters over time.
Materials and methods
The data for this study were drawn from the baseline (T1) and first follow-up (T2) waves of the Health, Eating and Play Study (HEAPS), conducted in 2002/2003 and 2006, respectively. The HEAPS study has been described in detail previously.22, 23 The study received ethical approval by the Deakin University Human Research Ethics Committee, the Victorian Department of Education and Training and the Catholic Education Office.
Participants
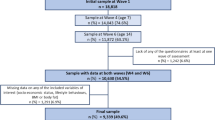
Participants included 204 children aged 5–6 (herein referred to as ‘younger children’) and 188 children aged 10–12 years (herein referred to as ‘older children’) who participated at both T1 and T2. In 2002/2003, state and Catholic primary schools in greater Melbourne, Australia, with an enrolment over 200 students were randomly selected from postcodes with the highest, middle and lowest quintiles of socioeconomic disadvantage according to the Australian Bureau of Statistic’s Socioeconomic Index for Areas (SEIFA).24 The two cohorts of children were recruited from 24 schools: 9 schools from high, 7 from middle and 8 from low SEIFA postcodes. In total, families of 1612 younger children and 2085 older children were invited to participate. Under existing ethical guidelines, only families who provided active consent were eligible to participate. Active consent was received for 615 younger children (38% response rate; mean age=5.8±0.4) and 947 older children (46% response rate; mean age=11.2±0.6 years). Active consent to participate at follow-up (mean length of follow-up=3.1±0.2 years) was received for 204 younger children (33% follow-up rate; mean age=9.0±0.5 years) and 188 older children (20% follow-up rate; 14.16±0.58 years) of the 351 and 474 families who agreed at baseline to be re-contacted for future research, respectively. At each time-point, questionnaires were completed by parents in their own time and children were fitted with an accelerometer, to be worn for 7 days. Among younger children, baseline data were collected from October 2002 to November 2003 and follow-up data from May to December 2006. Among older children, baseline data were collected from February to October 2003 and follow-up data from May to October 2006. Mean time between baseline and follow-up across the two cohorts was 3.1 (s.d.=0.2) years. Test–retest reliability was established for all questionnaire items in a subsample of 133 parents who completed the questionnaire a second time 2–3 weeks later.
Measures
BMI Z-score and weight status
Children’s height was measured with a portable stadiometer (to the nearest 0.1 cm) and weight was measured with digital scales (to the nearest 0.1 kg) by trained researchers using standardised protocols. Body mass index (BMI) was calculated (BMI=weight (kg) per height (m2)) and converted to BMI Z-scores using the 2000 growth chart data from the Center for Disease Control and Prevention.25 Children were classified as a healthy weight or overweight/obese according to age- and sex-specific BMI cut-points developed by the International Obesity Taskforce.26
Dietary intake
Methods used to assess dietary intake have been described previously.27 In brief, dietary intake at each time-point was assessed using a 56-item food frequency questionnaire (FFQ), which was adapted from the FFQ used in 1995 National Nutrition Survey and reported consumption in the previous week. Response categories were recoded to daily frequencies. Participants with 10 or more missing items on the FFQ at each time-point were excluded from the analyses (T1: n=47; T2; n=2). For remaining participants, missing values were set to zero (T1: n=808; T2: n=29), as previous research indicates that missing items are usually not consumed.28 The FFQ items were subsequently summed to compute total frequency of FV consumption per day (27 items, excluding potatoes) total frequency of ED food/drink consumption per day (24 items). These summary variables had acceptable reliability over 2–3 weeks (intra-class correlation 0.84; 95% confidence interval (CI): 0.76–0.91 and intra-class correlation= 0.65; 95% CI: 0.51–0.79).
PA and sedentary behaviour
Methods used to determine children’s PA and sedentary behaviour have been described previously.27 PA was assessed using accelerometry (Actigraph Model AM7164–2–2.2C, Manufacturing Technology Inc. [MT1], Fort Walton Beach, FL, USA). Children were asked to wear the accelerometer on their right hip for 7 days, except during water-based activities and while sleeping. Daily non-wear-time was defined as the sum of 20- min periods of consecutive zero counts,29 and a daily wear-time of ⩾8 h day–1 constituted a valid day.30 Children who wore the accelerometer for a minimum of 4 valid days, including one weekend day, were included in analyses (as this is the minimum monitoring period required to estimate habitual PA).30 Age-specific cut-points were used to determine the amount of time per day spent in moderate-to-vigorous PA (MVPA, defined as ⩾4 metabolic equivalents of rest).31 Time (min day–1) spent in MVPA was calculated by summing and averaging these values across valid days.
Sedentary time was defined as accelerometer counts <100 counts min–1 (as this cut-point has previously shown good to excellent classification accuracy).32, 33 Time (min day–1) spent being sedentary was calculated by summing and averaging these daily totals across all valid days, using the same criteria for valid wear-time as per the MVPA measure.
Parents reported how often their child watched commercial and non-commercial TV/DVDs on a typical school and weekend day. Parents provided the number of hours in 30-min blocks that most accurately described their child’s viewing time. Usual daily TV viewing (min day–1) was calculated (test–retest reliability: intra-class correlation=0.78; 0.69–0.84).22
Sociodemographics
At baseline, parents were asked to report their child’s gender, whether English was usually spoken at home, marital status and the highest attained education level of the mother. Maternal education was categorised as: low (completed some high school or less); medium (completed some high school and/or a technical or trade certificate, or apprenticeship); or high (having a university qualification). Marital status was categorised as: married or defacto/living together; or other (not married or defacto/living together).
Data analyses
All data management and statistical analyses were conducted using Stata statistical software, version 12.1 (Stata Inc., College Station, TX, USA). The cluster development for this study has been described in detail previously.27 In brief, a non-hierarchical k-medians CA was conducted by age group on the five diet, PA and sedentary behaviour variables.34 This was restricted to participants who had no missing data for the five cluster variables at T1 (younger children: n=157; older children: n=131): FV consumption (frequency per day); ED food/drink consumption (frequency per day); MVPA (min day–1; and sedentary time (min day–1). Cluster variables were standardised (converted to Z-scores) before the analysis to minimise the influence of different measurement scales of each of the variables.34
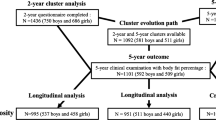
The k-medians partition method aims to minimise the distance between observed median scores and the cluster medioids and is therefore more robust to outliers.34 The Calinski–Harabasz rule was used to determine the first two optimal number of cluster solutions, with higher values corresponding to more distinct clusters.34 These procedures were also conducted in all baseline participants, including those without follow-up data (n=1004) and kappa was applied to assess the reliability of the created cluster solution. The final number of clusters chosen was based on the following three criteria: high values of the Calinski–Harabasz index, interpretability and distinctiveness of the cluster solution and the Kappa (K) statistic of the agreement between cluster solutions derived from all participants in the baseline sample and those derived from the longitudinal sample (participants with follow-up data) at baseline.35 Following these procedures, a three-cluster solution using k-medians was identified as the most appropriate and reliable (younger children: κ=0.88, P<0.001; older children κ=0.96, P<0.001) representation of the study population at T1 based on the five obesity-related behaviours. The same clustering procedure was repeated on younger and older children with no missing data for the five cluster variables at T2 (younger children: n=168; older children: n=124).
Descriptive statistics were used to summarise the baseline characteristics of respondents. Pearson’s chi-square test and independent t-tests were used to examine age group differences in baseline characteristics for categorical and continuous variables, respectively. Both cross-sectional and longitudinal linear and logistic regression models were used to test associations between baseline cluster membership and (1) BMI Z-scores and (2) weight status categories. Owing to the small sample size, younger and older children were combined for these analyses. These models were adjusted for gender, age group, maternal education and clustering by school. Longitudinal models were additionally adjusted for baseline BMI Z-score and baseline weight status, respectively.
The stability (tracking) of cluster membership between T1 and T2 was assessed by age group using K statistics. Weightings were not applied as there appeared to be no natural order to the cluster categories. The degree of tracking was evaluated using the cut-offs suggested by Landis and Koch35: <0.2, poor; 0.2–0.4, fair; 0.41–0.6, moderate; 0.61–0.8, good; >0.81, very good.
The final analytic sample included 123 younger and 87 older children who had complete data at both time-points, for all cluster, outcome and covariate variables. A P-value <0.05 was considered significant.
Results
Table 1 presents the baseline characteristics of participants by age group. There was no significant differences (P>0.05) in gender, marital status and maternal education between younger children and older children. However, BMI Z-scores were significantly lower among older children compared with younger children (mean difference=0.3, 95% CI: 0.1, 0.6; P=0.0083).
There were no significant differences in gender, marital status, maternal education, overweight prevalence, BMI Z-score, ED food/drink consumption, FV consumption and TV viewing for younger children who were followed-up compared with those who were not followed-up (data not shown). However, the prevalence of English spoken at home and sedentary time were significantly lower (P=0.013 and P=0.047, respectively) and time spent in MVPA significantly higher (P=0.0061) in the younger children who were followed-up. Among older children, there were no significant differences in gender, marital status, maternal education, overweight prevalence, BMI Z-score, FV consumption, MVPA, sedentary time and TV viewing compared with those who were not followed-up. However, the prevalence of English spoken at home (P=0.043), ED food/drink consumption (P=0.0033) and TV viewing time (P=0.01) were significantly lower in the older children who were followed-up compared with those who were not followed-up.
The clusters for younger and older children have been described previously, including a graphical representation.27 In brief, three clusters were identified in younger and older children and were qualitatively similar. Very good agreement (younger children: K=0.88; P<0.0001 and older children: K=0.96; P<0.001) was found between the three-cluster solution in the entire baseline sample27 and the three-cluster solution in the baseline sample with follow-up data. Table 2 shows the median (interquartile range) scores of the final cluster solutions at each time-point. The labels given to each cluster are based on high or low scores for each of the five behaviours relative to the other clusters at baseline. Cluster 1, labelled ‘most healthy’ (gender distribution within cluster: 49% younger boys, 61% older boys), was characterised by high median scores for MVPA and low scores for ED food/drink consumption, sedentary time and TV viewing time. Cluster 2, labelled ‘ED consumers who watch TV’ (65% younger boys, 61% older boys), was characterised by high median scores for ED food/drink consumption and TV viewing time. Cluster 3, labelled ‘high sedentary behaviour/low MVPA’ (45% younger boys, 22% older boys), was characterised by low median scores for MVPA and high scores for sedentary time. For both younger and older children, a similar three-cluster solution was identified at T1 and T2. The gender distribution within these clusters were as follows: cluster 1: 64% younger boys, 60% older boys; cluster 2: 61% younger boys, 68% older boys and cluster 3: 40% younger boys, 32% older boys.
After combining both age groups, there was no cross-sectional associations between baseline cluster membership and baseline BMI Z-score or weight status (Table 3). However, children in the ‘ED consumers who watch TV’ cluster at baseline had higher odds (odds ratio=2.0; 95% CI: 1.19, 3.42; P<0.01) of being overweight/obese at follow-up, and this association remained significant after additionally controlling for baseline weight status (odds ratio=2.8; 95% CI: 1.1, 6.9; P<0.05).
Table 4 shows the proportion of children who changed clusters and the percent agreement and K values of agreement of cluster membership between T1 and T2. The longitudinal stability of cluster membership was fair among younger children (K=0.24; P=0.0001) and moderate among older children (K=0.46; P<0.0001). Tracking (percent agreement) was highest for the ‘high sedentary behaviour/low MVPA’ (younger children: 58%; older children: 78%) and lowest for the ‘ED consumers who watch TV’ cluster among younger children (42%) and the ‘most healthy’ cluster among older children (56%). Of the 63 (51%) younger and 32 (37%) older children who shifted cluster membership over time, the highest proportion shifted to the ‘high sedentary behaviour/low MVPA’ cluster (younger children: 51%; older children: 59%).
Discussion
This study examined the clustering of diet, PA and sedentary behaviour and associations with overweight and obesity in younger and older children, both cross-sectionally and prospectively over 3 years. To the best of the authors’ knowledge, this was the first study among children to investigate the stability of cluster membership over time.
Using CA, three clusters, which were similar at baseline and at follow-up, were identified for both younger and older children. No significant cross-sectional associations between cluster membership and BMI Z-score were observed; however, children in the ‘ED consumers who watch TV’ cluster at baseline had a higher odds of being overweight/obese 3 years later, compared with children in the ‘most healthy’ cluster. At baseline, children in this cluster had the highest intake of ED food/drink and watched <2 h of TV per day. FV intake among these children also declined over 3 years.
The finding of a longitudinal association between this cluster and overweight/obesity suggests a possible cumulative effect of exposure to an unhealthy clustering of diet and sedentary behaviour over time, however, the literature to support this finding is limited. A recent longitudinal study of 1833 Australian children aged 6–7 years found a higher odds of obesity after 2 years among children in the ‘short sleepers/unhealthy eaters’ cluster, when compared with the ‘healthy’ cluster.15 Of note, approximately 41% of children in the ‘short sleepers/unhealthy eaters’ cluster also exceeded the 2-h screen-time recommendation. Gubbels et al.16 reported a longitudinal association between a ‘sedentary (TV viewing)/snacking’ pattern at 5 years of age and BMI Z-score at 7–8 years. In a cross-sectional study, Huh et al.11 reported a significantly higher prevalence of overweight children in the clusters characterised by consumption of ED snack foods, high sedentary behaviour and weight consciousness, and physical inactivity, respectively. Patnode et al.18 and te Velde et al.20 also found a positive cross-sectional association between the clustering of low PA/high sedentary behaviour and the risk of being overweight.
However, the documented relationship between weight status and clustering of obesity-related behaviours is overall inconsistent with a number of cross-sectional studies also finding either an unexplained inverse association with the unhealthy clusters10, 36 or no association at all.7, 8, 12, 19 Further, quality, large-scale, prospective studies are therefore needed to establish the effects of long-term exposure to unhealthy clustering patterns of obesity-related behaviours.
Over 3 years, cluster membership tracking was fair in younger children and moderate in older children, with tracking highest among children in the ‘high sedentary behaviour/low MVPA’ cluster. Among participants who changed their cluster membership over time, the highest proportion shifted to the ‘high sedentary behaviour/low MVPA’ cluster. Although, to the best of our knowledge, this is the first study to assess the stability of cluster membership of obesity-related behaviours among children over time, the findings are consistent with tracking studies that have examined diet, PA and sedentary behaviour in isolation. A review on the tracking of PA, based mostly on studies that use self-report measures, suggest low-to-moderate tracking of PA during childhood and adolescence.37 Research using accelerometry suggests both PA and sedentary behaviour track moderately during childhood.38, 39 The research also suggests low-to-moderate stability of dietary patterns during childhood and adolescence.40, 41, 42 In support of these findings, a systematic review of 27 studies found evidence of similar magnitude of tracking of both PA and diet between childhood and adulthood.43 In this study, the ‘ED consumers who watch TV’ and the ‘most healthy’ cluster showed the lowest stability over time among younger and older children, respectively. Why some clusters tracked better than others is currently unclear but warrants further investigation; understanding the critical periods of time where obesity-related behaviours change during childhood and adolescence may provide insight into this. However, reliance on parental report measures of diet and TV viewing possible misreporting of these behaviours may have introduced misclassification bias and needs to be considered. Low tracking may also be explained in part to potential mismatch in season between baseline and follow-up for some participants (19% were followed-up <3 months either side of their baseline month of data collection). Importantly, further larger-scaled longitudinal studies examining the stability of cluster membership over time are needed to support the novel findings from this study.
Although this study examined longitudinal associations between baseline clusters and overweight or obesity 3 years later, it may be more important to examine how cluster stability influences obesity development. That is, maintaining healthy or unhealthy habits over long periods of time is likely to be more important than being in a cluster at a single time-point. Post-hoc sensitivity analysis that examined the 115 children who remained in the same clusters over time produced similar findings. The only exception was a stronger association between the ‘ED consumers who watch TV cluster’ and overweight or obesity at T2 (odds ratio: 3.51, 95% CI: 1.26–9.78, P=0.016). However, these preliminary findings are based on a small sample; longitudinal research in larger samples, over longer time frames is needed.
Of note, the PA and sedentary behaviours within the clusters tended to change in an unhealthy direction over time. For example, at baseline, older children in the ‘high sedentary behaviour/low MVPA’ cluster did not achieve 60 min of MVPA per day and by follow-up were only achieving a median of 26 min. Although an age-related decline in PA is well established,38, 44 this study highlights that a decline in PA may be more profound in those who are also highly sedentary and that intervention efforts should begin early in primary school. Interestingly, no single cluster was immune to the age-related decline in obesity-related behaviours; across all clusters, including the ‘most healthy’ cluster, television viewing and sedentary behaviour increased and time spent in MVPA decreased among both younger and older children. These findings highlight the relative nature of clusters derived using data-driven approaches that would not have been detected if ‘cut-off scores’ for behaviours had have been applied.
A limitation of this study includes a reliance on parental report of children’s dietary behaviours, which is prone to recall bias, including social-desirability bias, leading to over- and under-reporting.45, 46 This may explain why clusters discriminated poorly by FV intake and also why ED food/drink intake did not increase over time. It is also possible that the FFQ did not include the range of ED food and drinks commonly consumed by older children and adolescents. TV viewing was also estimated by parents in 30-min time blocks; it is therefore possible that TV time was overestimated. In addition, mismatch between reported TV viewing and sedentary time may in part be due to other less sedentary activities undertaken while the TV was on.
Although the analyses addressed some important confounders, maturation status, previously associated with obesity (negatively in boys and positively girls),47 was not assessed and is a limitation of the study. Another important limitation is that the low response rates, low follow-up rates and missing data may have introduced bias; indeed response rates were lowest for families from low and middle socioeconomic areas. Age-specific differences were also found in the follow-up group for TV viewing, MVPA, ED food/drink consumption and sedentary behaviour in a direction conducive with a healthier lifestyle. However, among both age groups, there were no significant difference in gender, maternal education, marital status, overweight prevalence, BMI Z-score and FV consumption in children who were followed-up compared with those who were not (data not shown). There was also very good agreement between the three-cluster solution in the longitudinal sample at baseline the three-cluster solution derived from the entire baseline sample,27 suggesting that the cluster solutions were not affected by the loss to follow-up. In addition, similar direction and effect sizes for cross-sectional associations between cluster membership and overweight were observed when all baseline participants were examined (data not shown). Nonetheless, the finding of a longitudinal association between cluster membership and weight status was observed in a small prospective sample and should be interpreted with caution.
The CA method, although widely used, is a person-centred approach and findings are therefore not necessarily generalisable to other populations.13 There is also no consensus on how to best minimise researcher subjectivity when determining the optimal number of clusters within a given data set.34 A strength of this study is that it used an empirical stopping rule in the cluster development process. Other strengths include a focus on a range of important obesity-related behaviours and the inclusion of a longitudinal study design, which spanned important periods of childhood and adolescence (age range: 5–16 years). This study also developed cluster patterns from objective measures of habitual MVPA and sedentary time, and BMI Z-scores and weight status were calculated from measured height and weight. The regression models also adjusted for important confounders, including baseline overweight/obesity.
The three-cluster patterns identified in this study emphasise the complexity of the relationship between diet, PA and sedentary behaviour. Although the identification of obesity-related clusters is informative, their utility in improving the health status of populations requires realistic appraisal. In an ideal world, an intervention to reduce the prevalence and incidence of obesity would simultaneously improve multiple health behaviours.48 Interventions that effectively bring about multiple health behaviour change are likely to be more efficient, cost-effective and maximise reach.48 For example, in this study, TV viewing clustered with higher intakes of ED food/drinks and previous research suggests snacking while watching TV49 or TV advertising50 may mediate this association. Therefore, reducing TV time may also help decrease intake of unhealthy foods in this population, however, future studies that also examine cluster variables such as snacking while watching TV and watching commercial versus non-commercial TV could add weight to this hypothesis.
In a small longitudinal sample of children aged 5–12 years, baseline clustering of TV viewing with ED food/drink consumption predicted overweight/obesity 3 years later. Cluster membership also tracked fairly to moderately over 3 years in younger and older children, respectively. However, this is a novel finding in a small sample and further prospective research in larger samples, examining how obesity-related clusters track over time and influence the development of overweight and obesity are needed. Nonetheless, the tracking of unhealthy obesity-related clusters and the age-related increase in physical inactivity and sedentary behaviours found in this study underscore that, above all else, interventions targeting obesity should begin in early childhood.
References
Australian Bureau of Statistics Australian Health Survey: First Results, 2011-12. Cat. no. 4364.0.55001. ABS: Canberra, 2012.
World Health Organization (WHO) Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risk Factors. World Health Organization: Geneva, 2009.
Lobstein T, Bauer L, Uauy R, The IASO International Obesity TaskForce. Obesity in children and young people: a crisis in public health. Obes Rev 2004; 5 (Suppl 1): 4–85.
Carlson JA, Crespo NC, Sallis JF, Patterson RE, Elder JP . Dietary-related and physical activity-related predictors of obesity in children: a 2-year prospective study. Child Obes 2012; 8: 110–115.
Swinburn BA, Caterson I, Seidell JC, James WPT . Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr 2004; 7: 123–146.
Landsberg B, Plachta-Danielzik S, Lange D, Johannsen M, Seiberl J, Müller MJ . Clustering of lifestyle factors and association with overweight in adolescents of the Kiel Obesity Prevention Study. Public Health Nutr 2010; 13: 1708–1715.
Ottevaere C, Huybrechts I, Benser J, De Bourdeaudhuij I, Cuenca-Garcia M, Dallongeville J et al. Clustering patterns of physical activity, sedentary and dietary behavior among European adolescents: the HELENA study. BMC Public Health 2011; 11: 328.
Cameron AJ, Crawford DA, Salmon J, Campbell K, McNaughton SA, Mishra GD et al. Clustering of obesity-related risk behaviors in children and their mothers. Ann Epidemiol 2011; 21: 95–102.
Hardy LL, Grunseit A, Khambalia A, Bell C, Wolfenden L, Milat AJ . Co-occurrence of obesogenic risk factors among adolescents. J Adolesc Health 2012; 51: 265–271.
Sanchez A, Norman GJ, Sallis JF, Calfas KJ, Cella J, Patrick K . Patterns and correlates of physical activity and nutrition behaviors in adolescents. Am J Prev Med 2007; 32: 124–130.
Huh J, Riggs NR, Spruijt-Metz D, Chou C-P, Huang Z, Pentz M . Identifying patterns of eating and physical activity in children: a latent class analysis of obesity risk. Obesity (Silver Spring, MD) 2011; 19: 652–658.
Seghers J, Rutten C . Clustering of multiple lifestyle behaviours and its relationship with weight status and cardiorespiratory fitness in a sample of Flemish 11- to 12-year-olds. Public Health Nutr 2010; 13: 1838–1846.
Leech RM, McNaughton SA, Timperio A . The clustering of diet, physical activity and sedentary behavior in children and adolescents: a review. Int J Behav Nutr Phys Act 2014; 11: 4.
Boone-Heinonen J, Gordon-Larsen P, Adair LS . Obesogenic clusters: multidimensional adolescent obesity-related behaviors in the U.S. Ann Behav Med 2008; 36: 217–230.
Magee CA, Caputi P, Iverson DC . Patterns of health behaviours predict obesity in Australian children. J Paediatr Child Health 2013; 49: 291–296.
Gubbels JS, Kremers SP, Goldbohm RA, Stafleu A, Thijs C . Energy balance-related behavioural patterns in 5-year-old children and the longitudinal association with weight status development in early childhood. Public Health Nutr 2012; 15: 1402–1410.
Marshall SJ, Biddle SJH, Sallis JF, McKenzie TL, Conway TL . Clustering of sedentary behaviors and physical activity among youth: a cross-national study. Pediatr Exerc Sci 2002; 14: 401–417.
Patnode CD, Lytle LA, Erickson DJ, Sirard JR, Barr-Anderson DJ, Story M . Physical activity and sedentary activity patterns among children and adolescents: a latent class analysis approach. J Phys Act Health 2011; 8: 457–467.
Sabbe D, De Bourdeaudhuij I, Legiest E, Maes L . A cluster-analytical approach towards physical activity and eating habits among 10-year-old children. Health Educ Res 2008; 23: 753–762.
te Velde SJ, De Bourdeaudhuij I, Thorsdottir I, Rasmussen M, Hagstromer M, Klepp KI et al. Patterns in sedentary and exercise behaviors and associations with overweight in 9-14-year-old boys and girls—a cross-sectional study. BMC Public Health 2007; 7: 16.
Turner K, Dwyer JJM, Edwards AM, Allison KR . Clustering of specific health-related behaviours among Toronto adolescents. Can J Diet Pract Res 2011; 72: e155–e160.
Salmon J, Campbell KJ, Crawford DA . Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust 2006; 184: 64–67.
Leech RM, McNaughton SA, Crawford DA, Campbell KJ, Pearson N, Timperio A . Family food involvement and frequency of family dinner meals among Australian children aged 10-12years. Cross-sectional and longitudinal associations with dietary patterns. Appetite 2014; 75: 64–70.
Australian Bureau of Statistics Socio-Economic Indexes for Areas, 1996. ABS: Canberra, 1998. Report no.: Catalogue No. 2033.0.30.001.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R et al. CDC growth charts: United States. Adv Data 2000; (314): 1–27.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Leech RM, McNaughton SA, Timperio A . Clustering of children's obesity-related behaviours: associations with sociodemographic indicators. Eur J Clin Nutr 2014; 68: 623–628.
Willett W . Nutritional Epidemiology 2nd edn (Oxford University Press: New York, 1998.
Catellier DJ, Hannan PJ, Murray DM, Addy CL, Conway TL, Yang S et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc 2005; 37 (11 Suppl): S555–S562.
Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP . Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc 2005; 37 (11 Suppl): S582–S588.
Freedson P, Pober D, Janz KF . Calibration of accelerometer output for children. Med Sci Sports Exerc 2005; 37 (11 Suppl): S523–S530.
Trost SG, McIver KL, Pate RR . Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc 2005; 37 (11 Suppl): S531–S543.
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA . Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011; 43: 1360–1368.
Everitt BS, Landau S, Leese M, Stahl D . Cluster Analysis 5th edn (John Wiley & Sons, Ltd: West Sussex, 2011.
Landis JR, Koch GG . The analysis of categorical data in longitudinal studies of behavioral development. In: Nesselroade JR, Baltes PB (eds). Longitudinal Methodology in the Study of Behavior and Development. Academic Press: New York, 1979, pp 233–261.
van der Sluis ME, Lien N, Twisk JWR, Steenhuis IHM, Bere E, Klepp K-I et al. Longitudinal associations of energy balance-related behaviours and cross-sectional associations of clusters and body mass index in Norwegian adolescents. Public Health Nutr 2010; 13: 1716–1721.
Telama R . Tracking of physical activity from childhood to adulthood: a review. Obes Facts 2009; 2: 187–195.
Basterfield L, Adamson AJ, Frary JK, Parkinson KN, Pearce MS, Reilly JJ et al. Longitudinal study of physical activity and sedentary behavior in children. Pediatrics 2011; 127: e24–e30.
Kwon S, Janz KF . Tracking of accelerometry-measured physical activity during childhood: ICAD pooled analysis. Int J Behav Nutr Phys Act 2012; 9: 68.
Oellingrath IM, Svendsen MV, Brantsaeter AL . Tracking of eating patterns and overweight—a follow-up study of Norwegian schoolchildren from middle childhood to early adolescence. Nutr J 2011; 10: 106.
Lake AA, Mathers JC, Rugg-Gunn AJ, Adamson AJ . Longitudinal changes in food habits between adolescence (11-12 years) and adulthood (32-33 years): the ASH30 study. J Public Health (Oxf) 2006; 28: 10–16.
Madruga SW, Araujo CL, Bertoldi AD, Neutzling MB . Tracking of dietary patterns from childhood to adolescence. Rev Saude Publica 2012; 46: 376–386.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC . Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011; 70: 266–284.
Nelson MC, Neumark-Stzainer D, Hannan PJ, Sirard JR, Story M . Longitudinal and secular trends in physical activity and sedentary behavior during adolescence. Pediatrics 2006; 118: e1627–e1634.
Byers T . Food frequency dietary assessment: how bad is good enough? Am J Epidemiol 2001; 154: 1087–1088.
Magarey A, Watson J, Golley RK, Burrows T, Sutherland R, McNaughton SA et al. Assessing dietary intake in children and adolescents: Considerations and recommendations for obesity research. Int J Pediatr Obes 2011; 6: 2–11.
Wang Y . Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics 2002; 110: 903–910.
Prochaska JJ, Spring B, Nigg CR . Multiple health behavior change research: an introduction and overview. Prev Med 2008; 46: 181–188.
Pearson N, Ball K, Crawford D . Mediators of longitudinal associations between television viewing and eating behaviours in adolescents. Int J Behav Nutr Phys Act 2011; 8: 23.
Harris JL, Bargh JA, Brownell KD . Priming effects of television food advertising on eating behavior. Health Psychol 2009; 28: 404–413.
Acknowledgements
The HEAPS was funded by the Victorian Health Promotion Foundation (baseline) and the Australian Research Council (follow-up, ID: DP0664206). SAM is supported by an Australian Research Council (ARC) Future Fellowship (FT100100581). AT is supported by a National Heart Foundation of Australia Future Leader fellowship (ID: 100046). The funding bodies had no role in the analysis or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Leech, R., McNaughton, S. & Timperio, A. Clustering of diet, physical activity and sedentary behaviour among Australian children: cross-sectional and longitudinal associations with overweight and obesity. Int J Obes 39, 1079–1085 (2015). https://doi.org/10.1038/ijo.2015.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.66
- Springer Nature Limited
This article is cited by
-
Clustering of diet, physical activity and sedentary behaviour and related physical and mental health outcomes: a systematic review
BMC Public Health (2023)
-
Clustering of lifestyle and health behaviours in Australian adolescents and associations with obesity, self-rated health and quality of life
BMC Public Health (2023)
-
Clustering of lifestyle behaviors and adiposity in early adolescents in Spain: findings from the SI! Program for Secondary Schools
BMC Public Health (2023)
-
Clustering of Physical Activity, Sleep, Diet, and Screen-Based Device Use Associated with Self-Rated Health in Adolescents
International Journal of Behavioral Medicine (2022)
-
How physical activity, diet, and sedentary behavior cluster according to age in adolescents?
Sport Sciences for Health (2022)