Abstract
Objective:
To investigate whether the intestinal microbiota composition in early infancy is associated with subsequent weight development in children.
Methods:
Analyses were conducted within the KOALA Birth Cohort Study (n=2834). This cohort originates from two recruitments groups: pregnant women with a conventional lifestyle (no selection based on lifestyle) and pregnant women recruited through alternative channels (organic shops, anthroposophic clinicians/midwives, Steiner schools and relevant magazines). From 909 one-month-old infants, fecal samples were collected and analyzed by quantitative PCR targeting bifidobacteria, Bacteroides fragilis group, Clostridium difficile, Escherichia coli, Lactobacilli and total bacteria counts. Between the ages of 1 and 10 years, parent-reported weight and height was collected at 7 time points. Age- and gender-standardized body mass index (BMI) z-scores were calculated. Data were analyzed using generalized estimating equation.
Results:
Colonization with B. fragilis group was borderline significantly associated with a higher BMI z-score of 0.15 (95% confidence interval (CI): −0.02 to 0.31), in the conventional subcohort. After stratification for fiber intake (Pforinteraction=0.003), colonization with B. fragilis group was associated with a 0.34 higher BMI z-score among children with a low-fiber intake in this subcohort (95% CI: 0.17–0.53). Higher counts among colonized children were positively associated with BMI z-score only in children within the conventional subcohort and a high-fiber diet (BMI z-score 0.08; 95% CI: 0.01–0.14), but inversely associated in children with a low-fiber diet (BMI z-score −0.05; 95% CI: −0.10 to 0.00), and in children recruited through alternative channels (BMI z-score −0.10; 95% CI: −0.17 to −0.03). The other bacteria were not associated with BMI z-scores, regardless of subcohort.
Conclusion:
Using a targeted approach, we conclude that the intestinal microbiota, particularly the B. fragilis group, is associated with childhood weight development. To identify the potential impact of additional bacterial taxa, further prospective studies applying an unconstrained in-depth characterization of the microbiota are needed.
Similar content being viewed by others
Introduction
Overweight and obesity can have serious health consequences, including type 2 diabetes and cardiovascular diseases that are major public health problems.1 Not only in adults, but also in children, the prevalence of overweight and obesity is increasing.2, 3 The development of obesity is a complex process involving both genetic and environmental factors, such as an increased energy intake and reduced energy expenditure. However, these factors do not fully explain the increased obesity prevalence.4, 5
Our human gut is colonized with a complex 100 trillion microbe cells, the intestinal microbiota. The intestinal microbiota composition varies between individuals; the development of the infant microbiota is mainly influenced by prenatal exposure: mode of delivery, type of infant feeding and antibiotic use.6 Recently, the intestinal microbiota has been identified as a potential determinant of obesity, both in animal and human studies. The study by Ley et al.,7 published in 2005, showed for the first time that the intestinal microbiota differs between lean and obese mice. Obese mice harbor significantly less Bacteroidetes and more Firmicutes compared with their lean siblings.7 Furthermore, colonization of germ-free mice with an intestinal microbiota of obese donor mice led to a significantly greater increase in fat deposition than colonization with an intestinal microbiota of lean donors.8 A limited number of human studies, usually comparing obese with normal-weight subjects in a cross-sectional design, have been conducted so far. In addition, the many different methods for characterization of the indigenous microbiota complicate the direct comparison of results between studies (summarized in Table 1). So far, studies have provided contradictory results: some demonstrated a reduced level of Bacteroidetes to be associated with obesity,9, 10, 11, 12, 13, 14 whereas others found the opposite15, 16, 17 or no association.18, 19, 20, 21, 22 Specific bacterial and archeal genera or species have also been associated with obesity in humans, such as the Lactobacillus spp,10, 22, 23 bifidobacteria,15, 24, 25 Escherichia coli25 and Methanobrevibacter smithii10, 15, 23 (Table 1), but findings were not consistent between studies. To determine whether a different microbiota composition in early infancy is related to subsequent weight development, longitudinal cohort studies are needed. To our knowledge, only four human observational studies investigated the relation between intestinal microbiota composition and weight development in a longitudinal manner,25, 26, 27, 28, 29 two of which addressed microbiota in infancy with short-term follow-up but not beyond infancy28, 29 and two others addressed microbiota at ages 6–12 months and 3 months, in children with follow-up until 7 years and 10 years, respectively25, 26, 27 (Table 1).
Several mechanisms have been put forward to explain how the interaction between microbiota and host metabolism may contribute to obesity.30, 31 Certain species are able to digest dietary fiber, that is, complex carbohydrates that cannot be degraded by human enzymes, thus yielding energy for microbial growth and end products such as short-chain fatty acids. The latter have profound effects on human metabolism because they can serve as energy substrates for the gut (butyrate) and peripheral tissues (acetate, propionate), modulate inflammation and wound healing and act as vasodilators.30, 31 In addition, short-chain fatty acids can signal through G protein-coupled receptors, such as GPR41, on enteroendocrine cells, inducing the secretion of peptide YY.32, 33
The aim of this study was to investigate whether the intestinal microbiota composition in early infancy is associated with subsequent weight development during childhood. The fecal samples of 909 one-month-old infants were analyzed with quantitative PCR assays to enumerate several bacterial groups and species and related to weight development up to the age of 10 years.
Materials and methods
Subjects and study design
The current analyses were conducted within the KOALA Birth Cohort Study in the Netherlands. The design of the KOALA study has been described in detail elsewhere.34 Briefly, this cohort originates from two recruitment groups: healthy pregnant women with a conventional lifestyle (n=2343) and pregnant women recruited through alternative channels (n=491). The women with a conventional lifestyle were retrieved from an on-going prospective pregnancy cohort study on pregnancy-related pelvic girdle pain in the Netherlands.35 The second group of pregnant women were recruited through alternative channels, that is, posters in organic food shops, anthroposophic doctors and midwives, anthroposophic under-five clinics, Rudolf Steiner schools and magazines for special interest groups. This latter group of women was considered to have an alternative lifestyle that could involve dietary habits (vegetarian, organic), child-rearing practices, vaccination schemes and/or use of antibiotics. All participants were enrolled at 34 weeks of gestation.
Women recruited from January 2002 until December 2002 (n=1176) collected a fecal sample from their child ∼1 month postpartum. Inclusion criteria for the present analyses were: availability of a fecal sample collected between 3 and 6 weeks of life, sufficient amount of feces (≥1 g) and parental completion of the accompanying questionnaire (fecal collection questionnaire).
Exclusion criteria were: prematurity (infants born before 37 weeks of gestation), twins, congenital abnormalities related to growth (such as Down’s syndrome, Turner syndrome, Fallot’s tetralogy multiple disabilities), administration of antimicrobial agents before feces collection and children without any body mass index (BMI) measurement (Figure 1). All parents signed the informed consent and the study was approved by the medical ethics committee of Maastricht University Medical Center+.
Flowchart of the study population. The KOALA Birth Cohort study included pregnant women with a conventional lifestyle (recruited from the on-going Pregnancy-related Pelvic Girdle Pain study (PPGP)) or an alternative lifestyle (recruited from ‘alternative’ channels). Participants recruited from January 2002 onwards were asked to collect a fecal sample of their child. Reasons for exclusion with numbers, and response rates on the seven weight and height questionnaires are presented.
Fecal collection and microbial analysis
Parents were asked to collect the feces of their child at 1 month postpartum. They received a feces tube with a spoon attached to the lid (Sarstedt, Nümbrecht, Germany), together with a sanitary napkin, an instruction form about the correct collection and sending procedure and a brief questionnaire. Parents placed a sanitary napkin in the diaper to prevent absorption by the diaper; collection of the feces was done by spoon and deposited in the tube. The tube was sent to the Medical Microbiology department at Maastricht University Medical Center+ by post as soon as possible. Transport time was minimized by asking the parents to collect the feces on a Monday, Tuesday or Wednesday so that the samples did not remain in the mail over the weekend.
At the laboratory, fecal samples were 10-fold diluted in peptone water (Oxoid CM009, Hampshire, UK) containing 20% v/v glycerol (Merck, Darmstadt, Germany) and stored at −20 °C until analysis.
DNA extraction from the feces and the subsequent microbial analyses by means of real-time PCR assays has been described in detail elsewhere.6 Briefly, the DNA was extracted by a combination of bead-beating and the QIAamp DNA Stool Mini Kit (Qiagen, Hilden, Germany). DNA from all fecal samples was subjected to real-time PCRs for quantification of bifidobacteria, Bacteroides fragilis group, Clostridium difficile, E. coli, Lactobacilli and total bacteria based on 16S rDNA gene sequences. For detection of the bifidobacteria, C. difficile, E. coli and members of the bacteroides, the 5′-nuclease technique was used. For quantification of Lactobacilli and total bacteria load, real-time detection of PCR products was conducted by means of SYBR Green I (Bio-Rad Laboratories, Hercules, CA, USA). The validation of the real-time PCR assays has been described in detail elsewhere.36, 37, 38 Log10 colony-forming units per g (log10 CFU g−1) were calculated for each stool sample from the threshold cycle values by using the constructed standard curves. The prevalence of colonization was expressed as the percentage of infants colonized with a specific bacterial group or species. As almost all infants were colonized with bifidobacteria, a cutoff value of 10.68 log10 CFU g−1 (the median) was used to divide the population into those with a low or high abundance of the genus.
Outcome variable
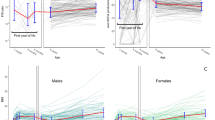
Information on the child’s weight, height and age at the time of measurements was collected using self-administered questionnaires. Parents were asked to report their child’s body weight and height at seven different time points. At the first and second time points, where the children had an average age±s.d. of 11±1 months and 22±3 months, respectively, parents were asked to report the most recent weight and height measured at the child health clinic, and to also report the age (in months) at the time of these measurements. At the further follow-up time points, in 2006 (age 56±4 months), 2007 (age 73±5 months), 2008 (age 80±5 months), 2009 (age 92±5 months) and 2010 (age 103±5 months), parents were asked to measure weight (in kg specified to one decimal) and height (in cm) without shoes and clothes and to report the exact date of measurement. BMI (weight/height2, kg m−2) was standardized by recoding it into age- and gender specific BMI z-scores using data from the Dutch reference population.39
Statistical analysis
The characteristics of the participants are given as mean values±s.d. for continuous variables and as numbers and proportions for categorical variables. Missing values for continuous covariables were replaced with the mean (maternal prepregnancy BMI n=2, age at collection of fecal sample n=10), and missing values for categorical covariables were classified as ‘unknown’ (place and mode of delivery n=23, maternal education of the mother n=10).
Generalized estimating equation (GEE) models with unstructured correlation structure were used for analysis of the repeated BMI z-scores. The analyses included only one bacterial group or species at a time. When bacterial counts were used as an independent variable, only infants who were colonized with that specific bacterial group or species were included. The age of the child at the time of BMI measurement was included in all models as the time variable. We tested whether the association between intestinal microbiota composition and BMI z-scores differed with increasing age by including an interaction term in the GEE models. When the interaction term was significant (P<0.05), we performed linear regression analyses for each BMI measurement separately. Participants were recruited through two different recruitment channels (representing a conventional or alternative lifestyle); we therefore tested for interaction between the intestinal microbiota and recruitment group. The interaction term was significant for C. difficile (P=0.037) and B. fragilis group (P=0.032); we therefore performed all analyses stratified for lifestyle.
First, unadjusted GEE analyses were performed to determine the association between colonization (yes/no) and bacterial counts (log10 CFU g−1) and BMI z-scores. Second, adjusted GEE analyses were conducted that included potential confounders. If the potential confounder changed the regression coefficient of any of the main determinants by more than 10%, it was consequently included in all models. The following variables were considered: infant gender (male, female), place and mode of delivery (vaginal delivery at home, vaginal delivery in hospital, artificial delivery in hospital, cesarean section in hospital), birth weight (in g), maternal prepregnancy BMI (kg m−2), age at collection of fecal sampling (in days), maternal smoking during pregnancy (number of cigarettes per day), type of infant feeding in the first month (exclusive breastfeeding, exclusive bottle-feeding or a combination), duration of breastfeeding (months), education level of the mother (lower education, vocational education, higher general secondary/pre-university or higher vocational/academic education) and total counts of bacteria. Finally, a third model additionally included the following dietary variables: total energy intake, energy percentage from fat and energy percentage from protein. Dietary information was collected during a period of 4 weeks by a food frequency questionnaire (FFQ) administered at the age of 4 years. The FFQ was specifically developed to assess children’s energy intake and validated by using the doubly labeled water method.40 The questionnaire consisted of 71 items and, in addition, for 27 foods the specific types or brands consumed and preparation methods were asked. Parents reported their child’s habitual food consumption by indicating the frequency of consumption (‘never’ to ‘6–7 days a week’) and by specifying proportion sizes in natural units (for example, pieces, slices), household units (for example, glasses of spoons) or g (for example, g of fish). Parents were asked to measure volume of the cups and glasses they used for the children. The average energy intake (kJ) and fiber intake (in g per MJ) per day were calculated using the Netherlands Food Composition Table 2001 (NEVO).41 For the products that were not included in the NEVO 2001 table, the nutritional values were provided by a dietician.
Fiber intake was considered as a potential effect modifier. Information on dietary fiber intake at the age of 4 years was also obtained from the FFQ. To determine whether dietary fiber modified the associations between the intestinal microbiota and weight development, a test for interaction with fiber intake was conducted in both recruitment groups. If the interaction term was significant, the analysis was stratified by level of dietary fiber intake (above or below the median of 15.0 g per day).
Data analysis was performed using the SPSS statistical software package version 19.0 (SPSS Inc., Chicago, IL, USA). The unadjusted (crudeβ) and adjusted (adjβ) regression coefficients with the corresponding 95% confidence interval (95% CI) are presented. A P-value of <0.05 was considered statistically significant in all analyses.
Results
Of the 1176 collected fecal samples, the samples that were too small (<1 g; n=65), were collected before the age of 3 weeks or after the age of 6 weeks (n=54) or where the fecal questionnaire was missing (n=25) were excluded. In total, 1032 fecal samples were appropriate for microbial analysis.6 After exclusion of premature infants (n=2), twins (n=10), children with congenital abnormalities related to growth (n=6), children without any BMI measurement (n=18) and children who received antibiotics before fecal sampling (n=95), the study population consisted of 909 children (Figure 1). Table 2 shows the baseline characteristics of the KOALA cohort (n=2834) and the study population (n=909). In general, the two groups were comparable, except that the study population had more participants with an alternative lifestyle, a higher level of maternal education and longer duration of breastfeeding, but less mothers who smoked during pregnancy. These differences are mainly because of the period of fecal sampling that coincided with recruitment of the alternative group. Almost all infants were colonized with bifidobacteria (98.6%), followed by E. coli (88.2%) and B. fragilis group (81.2%), whereas colonization with C. difficile (25.3%) and Lactobacilli (31.9%) was less frequent (Table 2). Neonatal colonization with B. fragilis group in the conventional subcohort was associated with a statistically significant higher BMI z-score of 0.16, compared with infants who were not colonized (Table 3). However, this did not remain significant after adjustment (Adjβ 0.11; 95% CI: −0.05 to 0.26). Other bacterial groups or species were not associated with BMI z-scores in children in the conventional subcohort. In children from the alternative subcohort (Table 4), a higher count of B. fragilis group was associated with a significantly lower BMI z-score in both crude and adjusted models (Adjβ −0.07; 95% CI: −0.15 to 0.00). Other bacterial groups or species were not associated with BMI z-scores in the alternative subcohort.
In the conventional subcohort, the interaction term between colonization with B. fragilis group and fiber intake was significant (P=0.003). There was no significant interaction with fiber for any of the other bacteria. After stratification for fiber intake (Table 5) in children with a lower than median fiber intake (<15 g per day), colonization with B. fragilis group was associated with a higher BMI z-score (Adjβ 0.34; 95% CI: 0.17–0.53); however, higher counts of B. fragilis group in colonized children was associated with a lower BMI z-score after adjustment for potential confounders (Adjβ −0.05; 95% CI: −0.10 to 0.01). Furthermore, in children with a higher than median fiber intake (>15 g per day), colonization with B. fragilis group was not associated with BMI z-scores, but a higher count of B. fragilis group was associated with a higher BMI z-score (Adjβ 0.07; 95% CI: 0.01–0.14). For all analyses, adding the dietary variables to the adjusted models (model 3) did not substantially alter the results.
Finally, we examined whether associations of bacterial groups and species with BMI z-scores changed over time (age of BMI measurement). Only for C. difficile the time interaction term was significant (P=0.002). Linear regression analysis showed that children in the conventional subcohort, who were colonized with C. difficile at 1 month postpartum, had a lower BMI z-score of −0.24 (Adjβ 0.24; 95% CI: −0.45 to −0.03) at 103±5 months of age. For the other time points, no significant effects were found (data not shown).
Discussion
The current study showed that colonization with B. fragilis group at 1 month postpartum tended to be associated with a higher BMI in children up to 10 years of age, in particular among children in the conventional subcohort and a low-fiber diet. In line with our results, Bäckhed et al.42 showed that host total body fat content increased after colonization of germ-free mice with Bacteroides thetaiotaomicron, the most abundant member of the B. fragilis group in the human gut. These latter results were explained by the ability of B. thetaiotaomicron to ferment plant- or host-derived polysaccharides to short-chain fatty acids, in particular acetate. Acetate can serve as a source of energy for peripheral tissues, and is taken up by the liver and used as a substrate for lipogenesis and gluconeogenesis. Colonized mice have higher levels of liver triglycerides that suppress the expression of fasting-induced adipose factor and increase the storage of triglycerides in adipocytes.30, 31 Our results are furthermore in accordance with the observational study by Vael et al.,28 who showed a positive association between B. fragilis group in the feces of 3- and 26-week-old infants, and BMI z-score at preschool age (up to 36 months) (n=138). In contrast to our study, White et al.29 showed that presence of Bacteroides spp. in 30-day-old infants was associated with lower body weight z-scores at the age of 6 months in males (n=108), but not in females. However, these studies used traditional culture and a microarray respectively to assess the microbiota composition, and caution is therefore required when comparing these results with our study. The role of fiber in children colonized with members of the B. fragilis group is contradictory. Only in children with a low-fiber diet (<15 g per day) colonization with B. fragilis group resulted in a higher BMI. In children with a high-fiber diet, colonization with B. fragilis group did not influence BMI. A potential explanation for this loss of association between colonization with the B. fragilis group and BMI in the high-fiber consumers might be that consuming a high-fiber diet at the age of 4 years might compensate for the effect that early B. fragilis group colonization has on BMI.
Our results for higher counts of B. fragilis group in children who are colonized are less clear. Higher counts are positively associated with BMI only in children in the conventional subcohort and a high-fiber diet, but inversely associated in children with a low-fiber diet, and in children in the alternative subcohort. A plausible explanation might be a different composition of B. fragilis group species between infants in the two different recruitments groups. The pregnant women recruited through alternative channels might introduce a different lifestyle for their children, promoting early colonization with other bacteroides species than in the conventional subgroup. Indeed, species within the B. fragilis group might differentially affect weight development as suggested by Bervoets et al.22 who showed more B. fragilis in obese and more B. vulgatus in control subjects. Identification of bacteroides at the species level in future prospective studies is warranted to address whether a different species distribution actually precedes (over)weight development during childhood.
We are not aware of any previous human studies that investigated the interaction between bacteroides and dietary fiber intake. It is important to note that although we were able to study this interaction, collection of fecal samples (at 1 month) and dietary information (at 4 years) did not take place at the same time, and this is clearly a weakness of this study. Despite the high instability of the microbiota in infancy, it may be speculated that the presence of B. fragilis group as pioneer species in the neonatal gut could be indicative for the subsequent persistence of these bacteria or other developmental processes toward an adult-like microbiota. Although dietary information was only collected once, at the age of 4 years, we used a validated FFQ to determine the habitual dietary intake. The FFQ reflects the long-term dietary pattern and gives a much better estimate of habitual dietary intake than instruments such as food diaries and 24-h recall. In addition, previous studies showed that dietary patterns stay relatively stable during childhood.43, 44
Furthermore, we observed that neonatal colonization with C. difficile was associated with a lower BMI at the age of 103±5 months. As asymptomatic carriage of C. difficile is very common in the first years of life and a significant effect was only found in the children in the conventional subcohort, after adjustment of potential confounders, and merely in the last time point of BMI measurement (average age of 105 months), caution in drawing conclusions is required. As we conducted several tests for the five different bacteria groups/species, a type I error because of multiple testing cannot be excluded. Therefore, further research is required to replicate our findings.
We did not find an association between bifidobacteria and BMI development. This is in contrast to the results from Kalliomäki et al.,26 who found lower levels of bifidobacteria at 6 and 12 months of age in children with normal weight (n=24) compared with overweight or obesity (n=25) at 7 years of age. That study was the first to show an association between intestinal microbiota composition and development of overweight. In our study, fecal samples were collected only at age 1 month when almost all children are colonized with high concentrations of bifidobacteria, and this might mask a potential effect of bifidobacteria.
The prospective study design, a large study population, adjustment for the main determinants of the microbiota composition in early infancy (for example, place and mode of delivery, type of infant feeding in the first month) and repeated measurements of BMI on 7 occasions over a time period of 10 years are major strengths of our study. Nevertheless, the present study also has some limitations; one drawback is that only five bacterial groups and genera were measured, although others may also be involved in weight development in childhood.45 Previous studies using extensive profiling of the neonatal gut microbiota, have however shown that the microbiota at this age is still very simple and dominated by the bacterial groups targeted in the present study.46 Another drawback of this study was the timing of fecal sampling collection at 1 month of age. In early infancy, the gut microbiota composition is relatively unstable and its role in shaping the microbiota at a later age is to date unknown.47, 48 This study only provides information on the role of the intestinal microbiota at early infancy. The measured species might actually indicate presence or absence of other unstudied co-occurring bacterial genera or species that influence weight development.49 Another limitation relates to the time between collection of the fecal sampling by the parents and analyzing the samples in the laboratory that was 1 day for the majority of samples. Even though the total amount of bacterial DNA, as well as the diversity of the microbiota, may decrease significantly in such a time period, the similarities of the fecal samples processed directly and those processed after 24 h remain high.36 This also applies for the temperature at which the fecal samples are held in the first 24 h after collection.50
Finally, in the present study, we made use of parent-reported body weight and height. Even though the procedure of measuring weight and height of their child was explained and numerous studies have demonstrated that self-reported questionnaires are a valid method to estimate body weight and height,51, 52 it is known that parents of children with a low BMI tend to overreport body weight, whereas parents of children with a high BMI tend to underreport body weight.53, 54 Recently, we reported a similar underestimation in the KOALA study.55 This implies that the association we observed between the intestinal microbiota and BMI may actually have been stronger than reported.
Conclusion
Our study indicates that presence of B. fragilis group in early infancy tended to be associated with a higher BMI later in childhood. If causal, this may have important public health implications as children with an elevated BMI are more likely to remain overweight as adults.56 Even a moderate increase in BMI over a long period of time has been shown to increase disease risk.57 Some studies found that a reduction of 0.25 BMI z-scores results in a small improvement in metabolic markers among obese adolescents,58 and a reduction of 0.5 BMI z-scores leads to a major improvement.59 Modification of the composition of the intestinal microbiota could contribute to the prevention of overweight and obesity.
References
Bastien M, Poirier P, Lemieux I, Despres JP . Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 2014; 56: 369–381.
Lakshman R, Elks CE, Ong KK . Childhood obesity. Circulation 2012; 126: 1770–1779.
Schonbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA et al. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PLoS One 2011; 6 e27608.
Raoult D . Obesity pandemics and the modification of digestive bacterial flora. Eur J Clin Microbiol Infect Dis 2008; 27: 631–634.
Farooqi S, O’Rahilly S . Genetics of obesity in humans. Endocr Rev 2006; 27: 710–718.
Penders J, Thijs C, Vink C, Stelma FF, Snijders B, Kummeling I et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 2006; 118: 511–521.
Ley RE, Bäckhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI . Obesity alters gut microbial ecology. Proc Natl Acad Sci USA 2005; 102: 11070–11075.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI . An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006; 444: 1027–1031.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI . Microbial ecology: human gut microbes associated with obesity. Nature 2006; 444: 1022–1023.
Armougom F, Henry M, Vialettes B, Raccah D, Raoult D . Monitoring bacterial community of human gut microbiota reveals an increase in Lactobacillus in obese patients and Methanogens in anorexic patients. PLoS One 2009; 4: e7125.
Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE et al. A core gut microbiome in obese and lean twins. Nature 2009; 457: 480–484.
Zuo HJ, Xie ZM, Zhang WW, Li YR, Wang W, Ding XB et al. Gut bacteria alteration in obese people and its relationship with gene polymorphism. World J Gastroenterol 2011; 17: 1076–1081.
Nadal I, Santacruz A, Marcos A, Warnberg J, Garagorri M, Moreno LA et al. Shifts in clostridia, bacteroides and immunoglobulin-coating fecal bacteria associated with weight loss in obese adolescents. Int J Obes 2009; 33: 758–767.
Xu P, Li M, Zhang J, Zhang T . Correlation of intestinal microbiota with overweight and obesity in Kazakh school children. BMC Microbiol 2012; 12: 283.
Schwiertz A, Taras D, Schafer K, Beijer S, Bos NA, Donus C et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring) 2010; 18: 190–195.
Abdallah Ismail N, Ragab SH, Abd Elbaky A, Shoeib AR, Alhosary Y, Fekry D . Frequency of Firmicutes and Bacteroidetes in gut microbiota in obese and normal weight Egyptian children and adults. Arch Med Sci 2011; 7: 501–507.
Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y et al. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci USA 2009; 106: 2365–2370.
Balamurugan R, George G, Kabeerdoss J, Hepsiba J, Chandragunasekaran AM, Ramakrishna BS . Quantitative differences in intestinal Faecalibacterium prausnitzii in obese Indian children. Br J Nutri 2010; 103: 335–338.
Duncan SH, Lobley GE, Holtrop G, Ince J, Johnstone AM, Louis P et al. Human colonic microbiota associated with diet, obesity and weight loss. Int J Obes 2008; 32: 1720–1724.
Mai V, McCrary QM, Sinha R, Glei M . Associations between dietary habits and body mass index with gut microbiota composition and fecal water genotoxicity: an observational study in African American and Caucasian American volunteers. Nutr J 2009; 8.
Karlsson CL, Onnerfalt J, Xu J, Molin G, Ahrne S, Thorngren-Jerneck K . The microbiota of the gut in preschool children with normal and excessive body weight. Obesity 2012; 20: 2257–2261.
Bervoets L, Van Hoorenbeeck K, Kortleven I, Van Noten C, Hens N, Vael C et al. Differences in gut microbiota composition between obese and lean children: a cross-sectional study. Gut Pathog 2013; 5: 10.
Million M, Maraninchi M, Henry M, Armougom F, Richet H, Carrieri P et al. Obesity-associated gut microbiota is enriched in Lactobacillus reuteri and depleted in Bifidobacterium animalis and Methanobrevibacter smithii. Int J Obes 2012; 36: 817–825.
Collado MC, Isolauri E, Laitinen K, Salminen S . Distinct composition of gut microbiota during pregnancy in overweight and normal-weight women. Am J Clin Nutr 2008; 88: 894–899.
Santacruz A, Marcos A, Warnberg J, Marti A, Martin-Matillas M, Campoy C et al. Interplay between weight loss and gut microbiota composition in overweight adolescents. Obesity (Silver Spring) 2009; 17: 1906–1915.
Kalliomäki M, Collado MC, Salminen S, Isolauri E . Early differences in fecal microbiota composition in children may predict overweight. Am J Clin Nutr 2008; 87: 534–538.
Luoto R, Kalliomaki M, Laitinen K, Delzenne NM, Cani PD, Salminen S et al. Initial dietary and microbiological environments deviate in normal-weight compared to overweight children at 10 years of age. J Pediatr Gastroenterol Nutr 2011; 52: 90–95.
Vael C, Verhulst SL, Nelen V, Goossens H, Desager KN . Intestinal microflora and body mass index during the first three years of life: an observational study. Gut Pathog 2011; 3: 8.
White RA, Bjornholt JV, Baird DD, Midtvedt T, Harris JR, Pagano M et al. Novel developmental analyses identify longitudinal patterns of early gut microbiota that affect infant growth. PLoS Comput Biol 2013; 9: e1003042.
Diamant M, Blaak EE, de Vos WM . Do nutrient-gut-microbiota interactions play a role in human obesity, insulin resistance and type 2 diabetes? Obes Rev 2011; 12: 272–281.
Tremaroli V, Bäckhed F . Functional interactions between the gut microbiota and host metabolism. Nature 2012; 489: 242–249.
Samuel BS, Shaito A, Motoike T, Rey FE, Bäckhed F, Manchester JK et al. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc Natl Acad Sci USA 2008; 105: 16767–16772.
Xiong Y, Miyamoto N, Shibata K, Valasek MA, Motoike T, Kedzierski RM et al. Short-chain fatty acids stimulate leptin production in adipocytes through the G protein-coupled receptor GPR41. Proc Natl Acad Sci USA 2004; 101: 1045–1050.
Kummeling I, Thijs C, Penders J, Snijders BEP, Stelma F, Reimerink J et al. Etiology of atopy in infancy: the KOALA Birth Cohort Study. Pediatr Allergy Immunol 2005; 16: 679–684.
Bastiaanssen JM, de Bie RA, Bastiaenen CH, Heuts A, Kroese ME, Essed GG et al. Etiology and prognosis of pregnancy-related pelvic girdle pain; design of a longitudinal study. BMC Public Health 2005; 5: 1.
Ott SJ, Musfeldt M, Ullmann U, Hampe J, Schreiber S . Quantification of intestinal bacterial populations by real-time PCR with a universal primer set and minor groove binder probes: a global approach to the enteric flora. J Clin Microbiol 2004; 42: 2566–2572.
Rinttila T, Kassinen A, Malinen E, Krogius L, Palva A . Development of an extensive set of 16S rDNA-targeted primers for quantification of pathogenic and indigenous bacteria in faecal samples by real-time PCR. J Appl Microbiol 2004; 97: 1166–1177.
Nadkarni MA, Martin FE, Jacques NA, Hunter N . Determination of bacterial load by real-time PCR using a broad-range (universal) probe and primers set. Microbiology 2002; 148: 257–266.
Kwaliteitsinstituut voor Gezondheidszorg CBO. Diagnostiek en behandeling van obesitas bij volwassenen en kinderen, 2008.
Dutman AE, Stafleu A, Kruizinga A, Brants HA, Westerterp KR, Kistemaker C et al. Validation of an FFQ and options for data processing using the doubly labelled water method in children. Public Health Nutr 2011; 14: 410–417.
Stichting Nederlands Voedingsstoffenbestand. Nederlands voedingsstoffenbestad 2001 (Netherlands Food Composition Table 2001) 2001.
Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA 2004; 101: 15718–15723.
Singer MR, Moore LL, Garrahie EJ, Ellison RC . The tracking of nutrient intake in young children: the Framingham Children’s Study. Am J Public Health 1995; 85: 1673–1677.
Bjelland M, Brantsaeter AL, Haugen M, Meltzer HM, Nystad W, Andersen LF . Changes and tracking of fruit, vegetables and sugar-sweetened beverages intake from 18 months to 7 years in the Norwegian Mother and Child Cohort Study. BMC Public Health 2013; 13: 793.
Kallus SJ, Brandt LJ . The intestinal microbiota and obesity. J Clin Gastroenterol 2012; 46: 16–24.
Azad MB, Konya T, Maughan H, Guttman DS, Field CJ, Chari RS et al. Gut microbiota of healthy Canadian infants: profiles by mode of delivery and infant diet at 4 months. CMAJ 2013; 185: 385–394.
Palmer C, Bik EM, DiGiulio DB, Relman DA, Brown PO . Development of the human infant intestinal microbiota. PLoS Biol 2007; 5: 1556–1573.
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M et al. Diversity of the human intestinal microbial flora. Science 2005 308 1635–1638.
Rousseau C, Levenez F, Fouqueray C, Dore J, Collignon A, Lepage P . Clostridium difficile colonization in early infancy is accompanied by changes in intestinal microbiota composition. J Clin Microbiol 2011; 49: 858–865.
Cardona S, Eck A, Cassellas M, Gallart M, Alastrue C, Dore J et al. Storage conditions of intestinal microbiota matter in metagenomic analysis. BMC Microbiol 2012; 12: 158.
Spencer EA, Appleby PN, Davey GK, Key TJ . Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr 2002; 5: 561–565.
Nyholm M, Gullberg B, Merlo J, Lundqvist-Persson C, Rastam L, Lindblad U . The validity of obesity based on self-reported weight and height: implications for population studies. Obesity (Silver Spring) 2007; 15: 197–208.
Scholtens S, Brunekreef B, Visscher TL, Smit HA, Kerkhof M, de Jongste JC et al. Reported versus measured body weight and height of 4-year-old children and the prevalence of overweight. Eur J Public Health 2007; 17: 369–374.
Shields M, Connor Gorber S, Janssen I, Tremblay MS . Obesity estimates for children based on parent-reported versus direct measures. Health Rep 2011; 22: 47–58.
Timmermans SH, Mommers M, Gubbels JS, Kremers SP, Stafleu A, Stehouwer CD et al. Maternal smoking during pregnancy and childhood overweight and fat distribution: the KOALA Birth Cohort Study. Pediatr Obes 2013.
Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ . Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008; 9: 474–488.
Baker JL, Olsen LW, Sorensen TI . Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007; 357: 2329–2337.
Ford AL, Hunt LP, Cooper A, Shield JP . What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child 2010; 95: 256–261.
Reinehr T, de Sousa G, Toschke AM, Andler W . Long-term follow-up of cardiovascular disease risk factors in children after an obesity intervention. Am J Clin Nutr 2006; 84: 490–496.
Santacruz A, Collado MC, García-Valdés L, Segura MT, Martín-Lagos JA, Anjos T et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr 2010; 104: 83–92.
Acknowledgements
We are grateful to the children and parents who participated in the KOALA Birth Cohort Study. The following sponsors contributed to data collection for the present study: Netherlands Organisation for Health Research and Development (ZonMw Grant No. 2100.0090), Netherlands Asthma Foundation (Grants No. 3.2.03.48 and No. 3.2.07.022), Netherlands Heart Foundation (Grant No. 2008B112), Triodos Foundation, Phoenix Foundation, Raphaël Foundation, Iona Foundation, Foundation for the Advancement of Heilpedagogiek, Royal Friesland Foods (currently FrieslandCampina); Netherlands Sugar Foundation and the Ministry of Economic affairs, all in The Netherlands. The sponsors had no influence on the analysis and reporting of the present study.
Author Contributions
LEJM Scheepers performed the literature search, carried out the statistical analyses, wrote the manuscript with the help of J Penders and ICW Arts and approved the final manuscript as submitted; J Penders contributed to the design of the study and collection of the data, performed the literature search, interpreted the data, contributed to the writing of the manuscript, critically reviewed and revised the manuscript and approved the final manuscript as submitted; C Mbakwa Akwi contributed to the analyses and interpretation of the data, reviewed and revised the manuscript and approved the final manuscript as submitted; C Thijs was the principal investigator and was responsible for the design and conduct of the study, contributed to the collection of the data, critically reviewed the manuscript and approved the final manuscript as submitted; M Mommers contributed to the design of the study and collection of the data, critically reviewed and revised the manuscript and approved the final manuscript as submitted; ICW Arts performed the literature search, interpreted the data, contributed to the writing of the manuscript, critically reviewed and revised the manuscript and approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Scheepers, L., Penders, J., Mbakwa, C. et al. The intestinal microbiota composition and weight development in children: the KOALA Birth Cohort Study. Int J Obes 39, 16–25 (2015). https://doi.org/10.1038/ijo.2014.178
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.178
- Springer Nature Limited
This article is cited by
-
Correlation of Gut Microbiota with Children Obesity and Weight Loss
Indian Journal of Microbiology (2024)
-
Association between gut microbiota at 3.5 years of age and body mass index at 5 years: results from two French nationwide birth cohorts
International Journal of Obesity (2023)
-
Gut Microbiome and Its Impact on Obesity and Obesity-Related Disorders
Current Gastroenterology Reports (2023)
-
Gut microbiota accelerates obesity in peri-/post-menopausal women via Bacteroides fragilis and acetic acid
International Journal of Obesity (2022)
-
Gut microbiota and BMI throughout childhood: the role of firmicutes, bacteroidetes, and short-chain fatty acid producers
Scientific Reports (2022)