Abstract
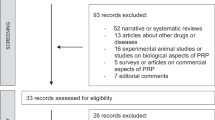
The emerging of intracavernosal injection (ICI) of vasoactive materials was a major breakthrough in the treatment of erectile dysfunction (ED). However, the current state and future direction of ICI role in the armamentarium of diagnosis, prevention and treatment of ED are not well defined. The aim of this study was to address the current place of ICI in the armamentarium of ED diagnosis and treatment. An English-language MEDLINE review for the utilization of 'intracavernosal injection & erectile dysfunction' was performed from 1990 to present time. Four hundred forty-eight articles were analyzed and classified according to the current utilization of ICI in the following conditions; diagnosis of ED, phosphodiesterase-5 inhibitor (PDE5I) non-responders, diabetes, post radical prostatectomy (RP), stem cells and gene therapy, new intracavernosal drugs, adverse effects and couple satisfaction. This paper is not a standard systematic review; it is eventually a literature review of original peer-reviewed manuscripts and clinical trials reported in Medline. The comprehensive analyses of all the reviewed data were not possible as the level of evidence for utility of ICI in each topic was not available. Current date have established the role of ICI of vasoactive materials as a very common alternative domain in treatment of severe ED particularly in diabetic patients, post-RP, PDE5I non-responders. Further, new studies have denoted the potential future role of intracavernosal treatment for ED in the era of stem cells and gene therapy. ICI of vasoactive material continues to be a highly effective and safe treatment tool for men with wide varieties of ED etiologies. Several experimental and clinical studies are currently investigating new ICI materials. Hopefully in the near future, we might witness evolved molecules and innovative strategies that could help to treat ED patients with different etiologies.
Similar content being viewed by others
Introduction
Amelioration of cavernosal fibrosis remains a controversial issue. The relative smooth muscle cells (SMCs) loss that happens with aging, cavernosal nerve injury and diabetes are detrimental factors in the process of penile fibrosis.1 Furthermore, chronic ischemia that occurs with those conditions is associated with the reduction of nitric oxide (NO)-cyclic guanosine monophosphate (cGMP) and ultimately cavernosal fibrosis. Encouraging recent results demonstrated the role of intracavernosal injection (ICI) of vasoactive material in the prevention of cavernosal fibrosis and ultimately improvement of erectile function; however, debate regarding the exact mechanism still exists.
ICI therapy introduced as monotherapy by Virag in 1982, and evolved into combination therapy with as many as four different compounds in the injectate.2, 3, 4 Alprostadil was the only agent for which FDA approval was sought. It was approved in 1994. Alprostadil is targeted at the end organ and acts directly on the penile and vascular SMCs. The mechanism of action is through stimulation of cAMP production with subsequently intracellular calcium sequestration and ultimately smooth muscle relaxation and penile erection. Men with pure neurogenic erectile dysfunction (ED) respond to significantly lower doses of alprostadil as its effect does not depend on NO or an intact nervous system, whereas older men with multiple medical co-morbidities need higher doses and might not respond as well.5, 6
Resurgence of the ICI role in management of ED was highlighted with a growing population of men who are initially refractory or become refractory to phosphodiesterase-5 inhibitors (PDE5Is), combination oral and ICI therapy has been shown to salvage those patients.7 The reported incidence of ED following radical prostatectomy (RP) range from 20 to 90%, depending upon which series is analyzed and whether the series is uni-institutional or multi-centered. Other contributing factors such as nerve sparing, pre-op ED assessment score and definition of erection should be considered. Furthermore, a more delayed recovery of erection that might happen take up to 3 years for the return of partial erections.8, 9 Additionally, ICI is introduced as a useful tool in penile rehabilitation, prevention and treatment of post-RP ED. In another important ICI domain, diabetic men with severe ED and patients who are PDE5I non-responders are more likely to achieve a satisfactory response to ICI than those with other types of ED.10
Achieving durable erection and better functioning penis was a dream for longtime. Promising recent experimental and ongoing clinical trials might bring this dream true. ICI of vasoactive agents may still have a key role in the alleviation of ED-associated cavernosal fibrosis in the future. Furthermore, the early introduction of ICI has been shown to accelerate the resumption of natural function and expedite PDE5I responsiveness.11 In this review, we intended to address the current place of ICI in the armamentarium of ED diagnosis and treatment.
Diagnosis of ED
Several studies were designed to evaluate whether PDE5Is could be used as alternatives to vasoactive agent injections.12 Some of them demonstrated that oral sildenafil was as effective as injection papaverine in evaluating ED. A more recent study concluded that, although PDE5Is and papaverine ICI showed similar effects on penile color-duplex ultrasound parameters in detecting arterial ED, more patients had better clinical responses to ICI, and oral PDE5Is administration still showed some pitfalls in practical use.13
Another interesting study had compared the clinical response and the change in nucleotides correlating with hemodynamic changes in the cavernosal arteries after ICI with vasoactive agents with or without oral sildenafil in men with ED. Authors concluded that the hemodynamic changes and cGMP and cAMP production in the cavernosum were improved by trimix plus sildenafil more than with PGE1 plus sildenafil or one ICI with trimix or PGE1. The results suggest that ICI with trimix and sildenafil is the best combination for a pharmacological erection test.14
An interesting study was designed to compare the results of both-side ICI with those of one-side injection. Authors concluded that dividing the total dose of the vasodilating agent and injecting half of the dose into each corpus cavernosum (CC) separately prevents artifactual difference between blood flow and velocity on the right and left side.15 A nice study was designed to identify any useful role of phentolamine redosing in diagnosis of venogenic impotence. Authors concluded that the addition of ICI phentolamine during PGE1 CDU examination carries no advantage over the use of PGE1 alone regarding cavernosal artery response in patients with suspected venogenic ED.16
Combination therapy for ED
PDE5I non-responders
The majority of men report that PDE5Is are effective; however, there is a subgroup of men who require second- and third-line therapies. The efficacy of this class of medication is well established for the general population, as well as in men following RP and radiotherapy for prostate cancer and those with diabetes mellitus (DM), spinal cord injury and other medical co-morbidities.17, 18, 19, 20 This class of medication has several contraindications such as concurrent nitrate therapy, following a recent myocardial infarction, and high-risk cardiovascular disease.
The success rate of PDE5Is is 43–89%. Several detrimental factors are responsible for the poor response to PDE5Is such as following prostate surgery (43%), DM with neuropathy (50%) and peripheral vascular disease (63%). Other factors contributing to the failure of PDE5Is include incorrect dosage/duration, intolerance to side effects and hypoandrogenism.21 A better response is seen in an otherwise healthy male whose ED is secondary to psychological disorders (89%), neurological disease (85%) and smoking (80%).21 Following a complete trial with PDE5Is, second-line therapies can be used as a single therapy or in combination with PDE5Is to improve response. Combination therapy has recently been adopted for more refractory cases of ED, but a critical evaluation of current combination therapies is lacking. Some of these combination treatments appeared to be quite effective in preliminary testing. Caution must be advised, however, as the majority of combination therapy have undergone on a relatively small sample size. Regardless of limitations, present combination therapy research provides a solid foundation for future studies in complex ED management.7 Several ICI agents were used to treat ED in PDE5I non-responders include papaverine, phentolamine and alprostadil or combination of the three agents (Trimix) or Quadmix (phentolamine, papaverine, prostaglandin E1 and atropine) can be initiated after an unsuccessful trial of alprostadil.22, 23 Erection usually occurs within 5–20 min of injection and can last up to 2–3 h. Patients should be educated regarding injection technique, dosing, minor side effects and priapism before beginning home injections. Improvement of natural spontaneous erections has been reported in men undergoing ICI. However, the discontinuation rates still high (40.7–68.0%).24, 25, 26
Unconsummated marriage
A nice study investigated the long-term outcome in 417 patients with male sexual dysfunction and unconsummated marriage, authors strongly advise ICI as the first-line treatment of unconsummated marriage.27
Diabetes mellitus
The incidence of sexual dysfunction in men with DM may exceed 50% and, diabetic men already made up one-quarter of those seeking advice for ED.28 In a study of Saudi diabetic patients we found that 86.1% had various degrees of ED, including mild in 7.7%, moderate in 29.4% and severe in 49.1%.29, 30
Oral PDE5Is are first-line treatment but only 50–60% of these patients see improvements from these drugs.31, 32 Diabetic men are more likely to achieve a satisfactory response to ICI than those with other types of ED.10 Moreover, diabetic patients accept self-injecting and comply better with this method of treatment compared with non-diabetics.33 Treatment with self-injections of vasoactive drugs in diabetic men with severe ED is a safe and effective alternative in the long term; however, in general, the frequency of non-compliance with self-injecting is high, approaching 50%.34 The mixtures of vasoactive drugs that use different mechanisms of action and exert pharmacological synergism are an effective treatment for severe diabetic ED. Diabetic men of both types show the same preferences in quality and quantity of treatment after 10 years. The key point to maintain treatment is the adjustment of the dosage and therapeutic method to reach a satisfactory erection.35 Self-injection is also a safe treatment, it has been reported that priapism never occurred during the long-term treatment phase of experienced patients.36
Although the majority of patients with ED strongly prefer oral therapeutic compounds, diabetic men who have started self-injecting are not likely to switch to oral treatment.37 Those men may decrease the number of self-injections over time, set realistic expectations and create a baseline of satisfactory sexual life with aging. For this reason, systematic follow-up of those patients is mandatory.
A recent interesting experimental study aimed to determine whether adipose-derived stem cells (ADSCs) expressing vascular endothelial growth factor (VEGF) gene can improve endothelial function, recover the impaired VEGF signaling pathway and enhance smooth muscle contents in a rat diabetic model. This study had demonstrated that impaired erectile function, abnormal VEGF signaling pathway, defect in endothelial function, smooth muscle content and pericytes were observed in diabetic rats. ICI of ADSCs expressing VEGF has more efficiently promoted the recovery of the diabetic erectile function. Moreover, the potential mechanisms of these recoveries appear to be due to the rescued endothelial function produced by the paracrine effects of ADSCs.38 Hence, a novel therapy to restore impaired endothelial cells (ECs) and cavernous SMC function is highly desirable for patients with DM-associated ED.32
A recent study was designed to evaluate the therapeutic potential of injectable microspheres for DM-related ED in the rat model and concluded that NO-releasing microspheres significantly improved erectile response in diabetic rats for 3 weeks and hence offer a promising approach to ED therapy, either as monotherapy or as combination therapy.39
Another study showed that an ICI of cartilage oligomeric matrix protein-angiopoietin-1 COMP-Ang1 enhances cavernous angiogenesis by structurally reinforcing the cavernosal endothelium.40 Interesting study investigated the expression of insulin-like growth factor binding protein-3 (IGFBP-3) in penile cavernosal tissue of diabetic rats model and whether downregulation of IGFBP-3 by ICI of short-hairpin ribonucleic acid targeting IGFBP-3 could improve the erectile function in DM rats. This study concluded that gene transfer of short-hairpin ribonucleic acid-IGFBP-3 could improve erectile function in DM rats by an increase in the cyclic guanosine monophosphate concentration in cavernous tissue.41
Post radical prostatectomy
Prostate cancer is the most common cancer among men in the United States representing around 25% of all newly diagnosed cancer.42 Although incontinence and ED are major urological complications of RP, this technique remains the gold standard therapy for clinically localized prostate cancer. The significant negative impact of ED on the quality of life of those patients was clearly shown.43, 44
The mechanisms of post-RP ED have been explored in animal as well as in human studies. Unilateral or more commonly bilateral transection of accessory or aberrant pudendal arteries, which can be the sole arterial supply to the corpora cavernosa, is incriminated in post-RP arteriogenic ED.45 Venogenic ED is mainly due to corporal smooth muscle fibrosis. Cavernous nerve (CN) traction or transection may result in reduction in nitric oxide synthase-producing nerves as well as corporal smooth muscle atrophy and fibrosis.46 Expression of profibrotic cytokines, such as transforming growth factor beta, with expression of more collagen was shown.47 Peyronie’s disease has also been reported in almost 16% of men post-RP.48 Finally, in a rat model of bilateral CN injury a hypogonadal state has been demonstrated that improves with testosterone supplement.49
The pointer study by Montorsi et al.50 popularized the concept of penile rehabilitation by using ICI of alprostadil to enhance erectile recovery post-RP. This study highlighted that the likelihood of spontaneous recovery of erections is not high, only 20% of patients had normal erectile function 6 months postoperatively in the control group compared with 67% in the experimental group P<0.01. Early post-op penile rehabilitation shown to facilitate early sexual intercourse, improve patient satisfaction and possibly promote earlier return of spontaneous erections.51
Prostaglandin E1 (PGE1), either alone or in combination with papaverine and/or phentolamine, is an effective treatment for ED. In men with normal erectile function preoperatively, among whom over 40% had failed prior ED treatments, had good success with ICI of this triple therapy post-RP.52 Raina et al.53 assessed the long-term efficacy and compliance of ICIs for mean duration of 3.7 years, one-third of ED men post-RP chose ICIs alprostadil alone, or triple therapy as their initial treatment. Of them, 48% continued long-term therapy, with significant increases in SHIM (Sexual Health Inventory in Men) compared with preoperative scores. The causes for discontinuation were insufficient erections in 33%, preference for oral therapy in 32%, fear of injections in 11%, troublesome procedure in 8%, priapism in 1% and return of natural erections in 1%. The combination of ICI alprostadil and PDE5Is improves erection based on SHIM scores in patients who were not completely satisfied with PDE5Is alone.54 ICIs with only PGE1 or combinations therapy in a monitored clinical setting are fairly successful in men with post-RP ED. Moreover, this strategy is effective for men who have tried and failed oral agents.
In an interesting recent study that investigated the effect of different agents on erectile function in a rat model of CN injury: PnTx2-6 protein from Phoneutria nigriventer spider toxin improved erectile function and prevented muscle atrophy in a rat model of bilateral CN injury via increased synthesis of nitric oxide and cGMP.55 In another study that investigated erectile responses to ICI of a soluble guanylate cyclase activator (BAY 60-277), under physiological and pathophysiological conditions. This study suggested that BAY 60-2770 would be effective in the treatment of ED when NO bioavailability is reduced, after pelvic nerve injury and when soluble guanylate cyclase is oxidized.56
A bilateral CN crush in adult Sprague-Dawley rats was used to mimic RP-induced ED. ICI of COX-2-10aa-PGIS is a newly engineered protein demonstrated that COX2-10aa-PGIS improved erectile function after CN injury through antifibrotic and anti-apoptotic mechanisms.57
Other study evaluated whether periprostatic implantation (PPI) of human bone marrow-derived mesenchymal stem cells (hBMSCs) potentiates recovery of erectile function after ICI of hBMSCs in a rat model of CN injury. This study showed that PPI of hBMSCs potentiates recovery of erectile function by decreasing corporeal smooth muscle deterioration and collagen deposition and via regeneration of nNOS-containing nerve fibers.57, 58 Another comparative study compared PPI and ICI of human ADSC to facilitate recovery of erectile function in a rat model of CN injury. This study showed that PPI or ICI of ADSCs in a rat model of CN injury was equally effective in recovering penile erection, but may address different types of pathophysiology.59
A clinical study evaluated the clinical outcomes of ICI use in an undifferentiated group of men with ED at various stages after RP. ICI use among patients after prostatectomy can be highly effective but has a significant attrition rate.60 Comparing early vs late rehab of erectile function after nerve-spring cystoprostatectomy in a prospective randomized manner showed that early erectile rehabilitation brings forward the natural healing time of potency and maintains nerve-assisted erection.61 A survey study of practice patterns among the International Society for sexual medicine practitioners regarding post-RP pharmacological penile rehabilitation concluded that post-RP penile rehabilitation is widely practiced, commenced early and based predominantly on PDE5Is and ICI.62
Stem cells and gene therapy
Cell transplantation and tissue engineering is an emerging field of science. In the field of urology, attempts have been made to engineer urological tissues, including the urethra, bladder and ureter.63, 64, 65 Endothelial dysfunction and subsequent decreased smooth muscle content may be one of the pivotal reasons for the refractory response to the conventional treatment in patients with medical co-morbidities associated ED. Therefore, new therapeutic strategies targeted toward repairing endothelial function, particularly in the early stage of these disorders, are needed.
Cell-based and gene therapies have become the new revolutionary therapeutic strategies aimed at discovering a cure for ED.66 Previous study illustrated that VEGF-transfected ADSCs improved erectile function in diabetic rats by enhancing VEGF stimulated endothelial function and increasing the contents of smooth muscle cells and pericytes.38 Other mesenchymal stem cells (MSCs), such as rat bone marrow-derived mesenchymal stem cells (BMSCs),67, 68 VEGF-transfected BMSCs,65 VEGF-transfected endothelial progenitor cells (EPCs)69 and autologous ADSCs,70 were reported capable of restoring erectile function in different animal models. A recent clinical study reported promising result of stem cell therapy for ED.71 Recently, urine-derived stem cells (USCs) reported to possess the features of a progenitor and are a convenient cell source. USCs display many characteristics of MSCs and are capable of differentiating into multiple cell lines including endothelial and smooth muscle cells.72 A recent study illustrated that USCs can secrete several proangiogenic growth factors, and hold endothelial differentiation potential. These characteristics of USCs indicate a strong potential to improve endothelial function in diabetic ED.73
Fibroblast growth factors (FGFs) are multifunctional proteins with a wide variety of functions; one important function of FGF1 and FGF2 is the promotion of EC proliferation and the physical organization of ECs.74 They induce angiogenesis and enhance the growth of new blood vessels from pre-existing vasculature in vivo.75 Both FGF1 and FGF2 are more potent angiogenic factors than VEGF or platelet-derived growth factor.76 A nice recent study aimed to determine the proangiogenic paracrine effect of USCs on improving ED using cell therapy with USCs or USCs genetically-modified with FGF2 in a rat model of type 2 diabetic ED. This study concluded that the paracrine effect of USCs or USCs-FGF2 induced improvement of erectile function in type 2 diabetic rats by recruiting resident cells and increasing the endothelial expression and contents of smooth muscle.73
Interesting studies have revealed that direct injection of the VEGF gene or protein into the corpora cavernosa restored erectile function in rabbits with hypercholesterolemia-induced ED and rats with traumatic arteriogenic ED.77, 78 A recent study transplanted ex vivo endothelial nitric oxide synthase (NOS) gene-modified MSCs into the corpora cavernosa of geriatric rats and reported restoration of erectile function.79
Stem cells have emerged as the current trend in the study of cell transplantation and tissue engineering during the past decade. Muscle-derived stem cells (MDSCs) are adult stem cells located in muscles that are known to proliferate into muscle cells and also differentiate into various tissues such as bone, cartilage and fat.80 Previously, umbilical cord blood MSCs showed improved erectile function in a rat model of CN injury.81 A recent study investigated the effect of intracavernosal transplantation of MDSCs on erectile function in rats with bilateral CN injury, and concluded that MDSCs can improve erectile function in a CN injury rat model. ED resulting from RP may be treated with ICI of MDSCs.82
A more recent study reported that ICI of both autologous or allogeneic MSCs improves erectile functions in a rat model of CN injury. Allogeneic MSCs might provide clinicians with ready to use, standardized and, in certain cases, more effective products.83
New intracavernosal drugs
Avanafil
A recent study was designed to determine the effect of ICI of avanafil, a novel PDE5I, on the treatment of ED associated with type 2 DM. After induction of diabetes, intracavernosal pressure was evaluated after 10 weeks on ICI of avanafil. The relaxant and contractile responses of CC strips were obtained in in vitro studies. Avanafil partially restored diminished ICP responses in diabetic rats. In CC strips from the diabetic group, electrical field stimulation-induced relaxation responses were markedly enhanced by 45%, whereas acetylcholine-induced relaxation responses were diminished by 73%. In addition, phenylephrine- and electrical field stimulation-induced contractile responses were significantly reduced in the diabetic group compared with controls. CC relaxant responses to sodium nitroprusside and avanafil were unaltered in both groups. This study concluded that ICI of avanafil in type 2 DM rats resulted in partial improvement in erectile responses. These findings suggest that ICI of avanafil might be beneficial for the treatment of ED in patients with type 2 DM.84
AVE 0991
A recent experimental study has hypothesized that the synthetic non-peptide Mas agonist, AVE 0991, would potentiate penile erectile function. This study showed that ICI of AVE 0991 potentiated the erectile response. The facilitatory effect of AVE 0991 on erectile function was dose dependent and completely blunted by the nitric oxide synthesis inhibitor, N-nitro-l-arginine methyl ester (l-NAME). Concomitant intracavernosal infusion of the specific Mas receptor blocker, A-779, abolished the effect of AVE 0991. This study concluded that AVE 0991 potentiates the penile erectile response through Mas in an NO-dependent manner, which might have significant therapeutic benefits for the treatment of ED.85
BAY 41-8543 and BAY 60-2770
A recent study aimed to investigate erectile responses to the sGC stimulator BAY 41-8543 under physiologic and pathophysiologic conditions. Increases in ICP/MAP in response to ICI of BAY 41-8543 and the interaction of BAY 41-8543 with exogenous and endogenously released NO were investigated; and the effect of the sGC stimulator on cavernosal nerve injury was assessed. This study demonstrated that BAY 41-8543 has significant erectile activity and can synergize with exogenous and endogenously released NO. Atropine and nerve crush attenuate the response to cavernosal nerve stimulation and that BAY 41-8543 can restore the response. The results indicated that the response to ICI of acetylcholine is mediated by muscarinic receptors and the release of NO with no significant role for nicotinic receptors. BAY 41-8543 might be useful in the treatment of ED.86
Another study investigated erectile responses to BAY 60-2770, an sGC activator, under physiological and pathophysiological conditions. Under baseline conditions, ICI of BAY 60-2770 increases ICP and area under the ICP curve. Responses to BAY 60-2770 were not altered by l-NAME or cavernosal nerve crush injury. These data indicate that BAY 60-2770 has potent erectile activity and show that responses to BAY 60-2770 are not attenuated by NOS inhibition or cavernosal nerve injury. These results suggest that BAY 60-2770 would be effective in the treatment of ED when NO bioavailability is reduced, after pelvic nerve injury, and when sGC is oxidized.56
PnTx2-6
Interesting study investigated the action of PnTx2-6, a toxin purified from the Phoneutria nigriventer spider venom that causes priapism in rats and mice erectile function was evaluated during electrical stimulation of the major pelvic ganglion of normotensive and deoxycorticosterone-acetate-salt hypertensive rats. This study demonstrated that PnTx2-6 enhanced erectile function in normotensive and deoxycorticosterone-acetate-salt hypertensive rats, via the NO pathway. The conclusion was PnTx2-6 could be important for development of new pharmacological agents for the treatment of ED.87 A recent experimental study investigated the effect of PnTx2-6 on the erectile function of aged rats. Intracavernosal pressure during electrical field stimulation of the pelvic ganglion was used to evaluate the erectile function. The results demonstrated that the decrease in erectile function associated with age was partially restored after injection of PnTx2-6 and further improved by sildenafil. PnTx2-6 enhanced electrical field stimulation-induced relaxation, as well as cGMP levels in CC, from young and aged rats. Relaxation due to PnTx2-6 was further increased after incubation with Y-27632, a Rho-kinase inhibitor, in aging CC. NOS activity in aged and young cavernosal tissue was increased by incubation with PnTx2-6. However, this toxin did not modify NOS expression. This study concluded that PnTx2-6 improves penile relaxation in aged rats, via increased NOS activity and NO release, resulting in enhanced cGMP levels.88
Fibroblast growth factor
Investigational study determined the effects of ICI of recombinant basic FGF on corporal tissue in hypercholesterolemic rabbits. All animals were maintained on the high cholesterol diet until the time of killing 3 weeks after last injection. Strips of corporal tissue were submaximally contracted with norepinephrine, and dose-response curves were generated to evaluate endothelial-dependent (acetylcholine) and endothelial-independent (sodium nitroprusside) vasoreactivity. Protein levels of basic fibroblast growth factor (bFGF) and VEGF were assessed. Vasoreactivity was improved by bFGF treatment. The expression of bFGF protein, VEGF protein, nNOS protein and mRNA was all increased after bFGF treatment. ICI of bFGF improved vasoreactivity in hypercholesterolemic rabbit corporal tissue, offering a new direction to explore for the treatment of ED.89
Vascular endothelial growth factor
A nice study investigated whether ICI of VEGF can restore erectile function in the aging rat. At 2 and 4 weeks after treatment, erectile function and histology were evaluated by hemodynamic study, histomorphometric analysis and immunohistochemistry. The study concluded that ICI of VEGF appears to restore smooth muscle integrity and improve erectile function in aged rats.90
Another recent study investigated the effect of transplanting EPCs transfected with the VEGF165 into the corpora cavernosa of rats with diabetic ED. ICP increased significantly among rats in the trial group when compared with the results from rats in the blank-plasmid and control groups during basal conditions and electrical stimulation. Histological examination revealed extensive neovascularization in the corpora cavernosa of rats in the trial group. Fluorescence microscopy indicated that many of the transplanted EPCs in the trial group survived, differentiated into ECs and integrated into the sites of neovascularization. This study concluded that transplantation of VEGF165-transfected EPCs into the corpora cavernosa of rats with diabetic ED restores erectile function.91
Sodium nitrite (NaNO2)
A nice study aimed to evaluate the effects of NaNO2 on erectile function in the rat. The ICI of NaNO2 produced dose-related increases in intracavernosal pressure and decreases in systemic arterial pressure. NaNO2 was 1000-fold less potent than sodium nitroprusside in increasing intracavernosal pressure. Increases in intracavernosal pressure in response to NaNO2 were attenuated by the NOS inhibitor l-NAME. The present data suggest that the conversion of NaNO2 to vasoactive NO is mediated by NOS in the corpora cavernosum and by xanthine oxidoreductase in the systemic vascular bed of the rat. These data show that NaNO2 can serve as an NO donor that increases erectile activity in the rat.92
Adverse effects and couple satisfaction
A nice recent study aimed to investigate the rate of withdrawal and its associated reasons in patients undergoing ICI therapy. Evaluation of intercourse rates, withdrawal rates and their associated reasons, adverse events and the patients' satisfaction were conducted. Most patients had previously failed PDE5I treatment before the ICI therapy. Adequate penile rigidity after ICI therapy was restored in 60.2% of patients. The reasons for discontinuation of ICI were poor response (43.1%), inconvenience of use (18.3%), switch to other treatments (10.7%), loss of libido (6.7%), adverse events (5.5%) and return of spontaneous erection (2.8%). Pain was the most common adverse event in the withdrawal group. Before initiating ICI treatments, sufficient counseling is necessary.93 Another study aimed to examine injection anxiety and injection pain in patients using ICI and conclude that although injection anxiety decreased with ICI use, mean injection anxiety remained at a moderate level; however, 42% of men continued to report 'high' injection anxiety at 4 months.94
A satisfaction study addressed ICI satisfaction in a modern cohort of patients in the PDE5I era and concluded that although the dropout rates were significant, high levels of satisfaction using the IIEF were reported. Older age, younger partner age and fully rigid erections were predictors of increased satisfaction. ICI remains a robust second-line therapy in the treatment of ED even in the era of PDE5I.95 Another study surveyed patient satisfaction, using validated questionnaires, in a group of men with ED who had used and responded to both sildenafil citrate and ICI therapy. Authors concluded that in patients who alternate the use of sildenafil and ICI therapy, satisfaction appears to be higher with ICI, although the erectogenic performance is similar.96 Another study supported this finding and concluded that more ED patients using ICI preferred it as their main treatment than was expected, even though they had a good response to oral sildenafil. A better quality of erection with ICI was the reason why experienced patients chose this method.97 Previous study had investigated the reliability of ICI of PGE1 office vs self injection therapy in patients with ED. This study demonstrated that there were significant differences between number of injections and amount of PGE1 per month, total number of injections and total amount of PGE1 on office and self-injection programs. There was a significant increase in the dropout rate in the office injection group compared with the self-injection group. There was an increase in penile fibrosis in the self-injection program compared with the office program. Minor hematoma had occurred in patients in the self-injection program in the first 3 months and had resolved spontaneously. No cases of infection or elevated liver enzymes were detected in the study population. There was no significant difference between improvement of natural erection or satisfaction rate after 1 year between patients in both programs. We concluded that self-injection program is reliable. Office injection program can be reserved for a subset of ED patients with special preferences.26
Summary and Conclusion
Aging, DM and cavernosal nerve damage are associated with the relative SMCs loss. Reversion of SMCs loss should be the target of therapy to prevent ED associated with these conditions.98 Although the introduction of ICI of vasoactive materials was a major breakthrough in the treatment of ED, however, the current place of ICI in the prevention and treatment of ED is not yet well established. ICI of vasoactive material continues to be a highly effective and safe treatment tool for men with wide varieties of ED etiologies. The key point for maintaining the treatment is the adjustment of the therapeutic method and dosage to optimize a satisfactory erection. For this reason, systematic follow-up of ED patients is of the utmost importance. Men with ED may decrease the number of self-injections over time and more importantly set up a realistic expectation to create a baseline of satisfactory sexual life.
ICI of vasoactive materials is reported as a very common alternative way of therapy for treatment of severe ED in diabetic patients. PDE5I non-responders usually are frustrated and sometimes anxious; resurgence of the ICI role in management of ED was highlighted with a growing population of men who are initially refractory or become refractory to PDE5I, combination oral and ICI therapy has been shown to salvage to those patients.
Urologist may prefer to institute early post-RP penile rehabilitation. Administration of ICI of vasoactive material following CN injury improves cavernous smooth muscle-to-collagen corporal ratios and ultimately erectile hemodynamics. There is strong support for some program of post-RP penile rehabilitation, defined as medical treatment to improve the restoration of natural penile mechanics, which results in spontaneous EF. Each of the ED management options had its own limitation and should be presented to the patient with realistic goals and expectations. Moreover, ICI was introduced as a remarkable tool in penile rehabilitation, prevention and treatment of post-RP ED. In this context, penile rehabilitation defined as medical treatment at the time of or after RP to improve the restoration of natural penile mechanics, which results in spontaneous erection. Although some evidence exists for the benefit of ICIs in a rehabilitative setting; however, the findings of these studies are limited. This could be due to the retrospective natures of the studies, small patient numbers, absences of control or placebo groups for comparison and unspecified lengths of follow-up, which might prevents definitive conclusions from being reached.
Although PDE5Is are first-line treatment they are contraindicated in several contexts. ICI as a second line can be solely offered or in conjunction with PDE5I for treatment of men with ED. As numerous experimental and clinical studies are in different stages of investigating ICI of new agents therefore, hopefully in the near future, we might witness evolved molecules and innovative strategies that could help to treat ED patients with challenging associated conditions.
References
Ferrini MG, Davila HH, Kovanecz I, Sanchez SP, Gonzalez-Cadavid NF, Rajfer J . Vardenafil prevents fibrosis and loss of corporal smooth muscle that occurs after bilateral cavernosal nerve resection in the rat. Urology 2006; 20: 429–435.
Virag R . Intracavernous injection of papaverine for erectile failure. Lancet 1982; 2: 938.
Shmueli J, Israilov S, Segenreich E, Baniel J, Livne P . Progressive treatment of erectile dysfunction with intracorporeal injections of different combinations of vasoactive agents. Int J Impot Res 1999; 11: 15–19.
Baniel J, Israilov S, Engelstein D, Shmueli J, Segenreich E, Livne PM . Three-year outcome of a progressive treatment program for erectile dysfunction with intracavernous injections of vasoactive drugs. Urology 2000; 56: 647–652.
Vaidyanathan S, Soni BM, Krishnan KR . Special precautions to be observed while using alprostadil in patients with spinal cord injury. Spinal Cord 1997; 35: 402–403.
Purvis K, Brekke I, Christiansen E . Determinants of satisfactory rigidity after intracavernosal injection with prostaglandin E1 in men with erectile failure. Int J Impot Res 1996; 8: 9–16.
Dhir RR, Lin HC, Canfield SE, Wang R . Combination therapy for erectile dysfunction: an update review. Asian J Androl 2011; 13: 382–390.
Mulhall JP, Morgentaler A . Penile rehabilitation should become the norm for radical prostatectomy patients. J Sex Med 2007; 4: 538–543.
Burnett AL . Erectile dysfunction following radical prostatectomy. JAMA 2005; 293: 2648–2653.
Bancroft J, Gutierrez P . Erectile dysfunction in men with and without diabetes mellitus: a comparative study. Diabetic Med 1996; 13: 84–89.
Raina R, Nandipati KC, Agarwal A, Mansour D, Kaelber DC, Zippe CD . Combination therapy: medicated urethral system for erection enhances sexual satisfaction in sildenafil citrate failure following nerve-sparing radical prostatectomy. J Androl 2005; 26: 757–760.
Viswaroop B, B A, Gopalakrishnan G . Evaluating erectile dysfunction: oral sildenafil versus intracavernosal injection of papaverine. Natl Med J India 2005; 18: 299–301.
Yang Y, Hu JL, Ma Y, Wang HX, Chen Z, Xia JG et al. Pharmaco-induced erections for penile color-duplex ultrasound: oral PDE5 inhibitors or intracavernosal injection? Int J Impot Res 2012; 24: 191–195.
Park JK, Park JS, Jeon SB, Cui WS, Kim SZ, Kang KK et al. Why a combined intracavernosal injection with trimix and oral sildenafil is reliable therapy in the ultrasonographic evaluation of erectile dysfunction. BJU Int 2008; 102: 993–997.
Ghafoori M, Hoseini K, Shakiba M . Comparison of one-side and bilateral intracavernosal papaverine injection on a Doppler study of the penis. Int J Impot Res 2009; 21: 382–386.
Arafa M, Eid H, Shamloul R . Significance of phentolamine redosing during prostaglandin E1 penile color Doppler ultrasonography in diagnosis of vascular erectile dysfunction. Int J Urol 2007; 14: 476–477.
Ellsworth P, Kirshenbaum EM . Current concepts in the evaluation and management of erectile dysfunction. Urol Nurs 2008; 28: 357–369.
Fink HA, Mac Donald R, Rutks IR, Nelson DB, Wilt TJ . Sildenafil for male erectile dysfunction: a systematic review and meta-analysis. Arch Intern Med 2002; 162: 1349–1360.
El-Sakka AI, Anis T, Khadr N, Ismail TA, Hegazy AM, Fekry O et al. Sildenafil treatment of erectile dysfunction in the Middle East: an observational analysis of patients with diabetes and/or hypertension treated in the clinical practice setting. J Int Med Res 2011; 39: 558–568.
El-Sakka AI . Efficacy of sildenafil citrate in treatment of erectile dysfunction: effect of type 2 diabetes. Eur Urol 46: 503–509 2004.
Kendirci M, Tanriverdi O, Trost L, Hellstrom WJ . Management of sildenafil treatment failures. Curr Opin Urol 2006; 16: 449–459.
Sivalingam S, Hashim H, Schwaibold H . An overview of the diagnosis and treatment of erectile dysfunction. Drugs 2006; 66: 2339–2355.
Brant WO, Bella AJ, Lue TF . Treatment options for erectile dysfunction. Endocrinol Metab Clin North Am 2007; 36: 465–479.
Montorsi F, Salonia A, Zanoni M, Pompa P, Cestari A, Guazzoni G et al. Current status of local penile therapy. Int J Impot Res 2002; 14 (Suppl 1): S70–S81.
Urciuoli R, Cantisani TA, Carlini M, Giuglietti M, Botti FM et al. Prostaglandin E1 for treatment of erectile dysfunction. Cochrane Database Syst Rev 2004; 2: Art. No. CD001784.
El-Sakka AI . Intracavernosal prostaglandin E1 self versus office injection therapy in patients with erectile dysfunction. Int J Impot Res 2006; 18: 180–185.
Zargooshi J . Male sexual dysfunction in unconsummated marriage: long-term outcome in 417 patients. J Sex Med 2008; 5: 2895–2903.
Guay AT . Sexual dysfunction in the diabetic patient. Int J Impot Res 2001; 13: S47–S50.
El-Sakka AI, Tayeb KA . Erectile dysfunction risk factors in non-insulin dependent diabetic Saudi patients. J Urol 2003; 169: 1043–1047.
El-Sakka AI . Association of risk factors and medical co-morbidities with male sexual dysfunctions. J Sexual Med 2007; 4: 1691–1700.
Stuckey BG, Jadzinsky MN, Murphy LJ, Montorsi F, Kadioglu A, Fraige F et al. Sildenafil citrate for treatment of erectile dysfunction in men with type 1 diabetes: results of a randomized controlled trial. Diabetes Care 2003; 26: 279–284.
Kolluru GK, Bir SC, Kevil CG . Endothelial dysfunction and diabetes: effects on angiogenesis, vascular remodeling, and wound healing. Int J Vasc Med 2012; 2012: 918267.
Perimenis P, Gyftopoulos K, Athanasopoulos A, Barbalias G . Diabetic impotence treated by intracavernosal injections: high treatment compliance and increasing dosage of vaso-active drugs. Eur Urol 2001; 40: 398–403.
Althof SE, Turner LA, Levine SB, Risen C, Kursh E, Bodner D et al. Why do so many people drop out from auto-injection therapy for impotence? J Sex Marital Ther 1989; 15: 121–129.
Perimenis P, Konstantinopoulos A, Perimeni PP, Gyftopoulos K, Kartsanis G, Liatsikos E et al. Long-term treatment with intracavernosal injections in diabetic men with erectile dysfunction. Asian J Androl 2006; 8: 219–224.
Perimenis P, Athanasopoulos A, Geramoutsos I, Barbalias G . The incidence of pharmacologically induced priapism in the diagnostic and therapeutic management of 685 men with erectile dysfunction. Urol Int 2001; 66: 22–26.
Perimenis P, Markou S, Gyftopoulos K, Athanasopoulos A, Giannitsas K, Barbalias G . Switching from long-term treatment with self-injections to oral sildenafil in diabetic patients with severe erectile dysfunction. Eur Urol 2002; 41: 387–391.
Liu G, Sun X, Bian J, Wu R, Guan X, Ouyang B et al. Correction of diabetic erectile dysfunction with adipose derived stem cells modified with the vascular endothelial growth factor gene in a rodent diabetic model. PLoS One 2013; 8: e72790.
Soni SD, Song W, West JL, Khera M . Nitric oxide-releasing polymeric microspheres improve diabetes-related erectile dysfunction. J Sex Med 2013; 10: 1915–1925.
Kim SO, Lee HS, Ahn K, Park K . COMP-angiopoietin-1 promotes cavernous angiogenesis in a type 2 diabetic rat model. J Korean Med Sci 2013; 28: 725–730.
Yang Z, Zhou Z, Wang X, Peng M, Zhou H, Meng Z et al. Short hairpin ribonucleic acid constructs targeting insulin-like growth factor binding protein-3 ameliorates diabetes mellitus-related erectile dysfunction in rats. Urology 2013; 81: e11–e16.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ . Cancer statistics 2009. CA Cancer J Clin 2009; 59: 225–249.
Arai Y, Okubo K, Aoki Y, Maekawa S, Okada T, Maeda H et al. Patient-reported quality of life after radical prostatectomy for prostate cancer. Int J Urol 1999; 6: 78–86.
Litwin MS, Flanders SC, Pasta DJ, Stoddard ML, Lubeck DP, Henning JM . Sexual function and bother after radical prostatectomy or radiation for prostate cancer: multivariate quality of life analysis from CaPSURE. Cancer of the Prostate Strategic Urologic Research Endeavor. Urology 1999; 54: 503–508.
Rogers CG, Trock BP, Walsh PC . Preservation of accessory pudendal arteries during radical retropubic prostatectomy: Surgical technique and results. Urology 2004; 64: 148–151.
Leungwattanakij S, Bivalacqua TJ, Usta MF, Yang DY, Hyun JS, Champion HC et al. Cavernous neurotomy causes hypoxia and fibrosis in rat corpus cavernosum. J Androl 2003; 24: 239–245.
User HM, Hairston JH, Zelner DJ, McKenna KE, McVary KT . Penile weight and cell subtype specific changes in a post-radical prostatectomy model of erectile dysfunction. J Urol 2003; 169: 1175–1179.
Tal R, Heck M, Teloken P, Siegrist T, Nelson CJ, Mulhall JP . Peyronie’s disease following radical prostatectomy: incidence and predictors. J Sex Med 2010; 7: 1254–1261.
Vignozzi L, Filippi S, Morelli A, Marini M, Chavalmane A, Fibbi B et al. Cavernous neurotomy in the rat is associated with the onset of an overt condition of hypogonadism. J Sex Med 2009; 6: 1270–1283.
Montorsi F, Guazzoni G, Strambi LF, Da Pozzo LF, Nava L, Barbieri L et al. Recovery of spontaneous erectile function after nerve-sparing radical retropubic prostatectomy with and without early intracavernous injections of alprostadil: results of a prospective, randomized trial. J Urol 1997; 158: 1408–1410.
Nandipati K, Raina R, Agarwal A, Zippe CD . Early combination therapy: intracavernosal injections and sildenafil following radical prostatectomy increases sexual activity and the return of natural erections. Int J Impot Res 2006; 18: 446–451.
Claro Jde A, de Aboim JE, Maríngolo M, Andrade E, Aguiar W, Nogueira M et al. Intracavernous injection in the treatment of erectile dysfunction after radical prostatectomy: an observational study. Sao Paulo Med J 2001; 119: 135–137.
Raina R, Lakin MM, Thukral M, Agarwal A, Ausmundson S, Montague DK et al. Long term efficacy and compliance of intracorporeal (IC) injection for erectile dysfunction following radical prostatectomy: SHIM (IIEF-5) analysis. Int J Impot Res 2003; 15: 318–322.
Mydlo JH, Viterbo R, Crispen P . Use of combined intracorporal injection and a phosphodiesterase-5 inhibitor therapy for men with a suboptimal response to sildenafil and/or vardenafil monotherapy after radical retropubic prostatectomy. BJU Int 2005; 95: 843–846.
Jung AR, Choi YS, Piao S, Park YH, Shrestha KR, Jeon SH et al. The effect of PnTx2-6 protein from Phoneutria nigriventer spider toxin on improvement of erectile dysfunction in a rat model of cavernous nerve injury. Urology 2014; 84: e9–e17.
Lasker GF, Pankey EA, Frink TJ, Zeitzer JR, Walter KA, Kadowitz PJ . The sGC activator BAY 60-2770 has potent erectile activity in the rat. Am J Physiol Heart Circ Physiol 2013; 304: H1670–H1679.
Lin H, Yuan J, Ruan KH, Yang W, Zhang J, Dai Y et al. COX-2-10aa-PGIS gene therapy improves erectile function in rats after cavernous nerve injury. J Sex Med 2013; 10: 1476–1487.
You D, Jang MJ, Lee J, Jeong IG, Kim HS, Moon KH et al. Periprostatic implantation of human bone marrow-derived mesenchymal stem cells potentiates recovery of erectile function by intracavernosal injection in a rat model of cavernous nerve injury. Urology 2013; 81: 104–110.
You D, Jang MJ, Lee J, Suh N, Jeong IG, Sohn DW et al. Comparative analysis of periprostatic implantation and intracavernosal injection of human adipose tissue-derived stem cells for erectile function recovery in a rat model of cavernous nerve injury. Prostate 2013; 73: 278–286.
Domes T, Chung E, DeYoung L, MacLean N, Al-Shaiji T, Brock G . Clinical outcomes of intracavernosal injection in postprostatectomy patients: a single-center experience. Urology 2012; 79: 150–155.
Mosbah A, El Bahnasawy M, Osman Y, Hekal IA, Abou-Beih E, Shaaban A . Early versus late rehabilitation of erectile function after nerve-sparing radical cystoprostatectomy: a prospective randomized study. J Sex Med 2011; 8: 2106–2111.
Teloken P, Mesquita G, Montorsi F, Mulhall J . Post-radical prostatectomy pharmacological penile rehabilitation: practice patterns among the international society for sexual medicine practitioners. J Sex Med 2009; 6: 2032–2038.
Bach AD, Bannasch H, Galla TJ, Bittner KM, Stark GB . Fibrin glue as matrix for cultured autologous urothelial cells in urethral reconstruction. Tissue Eng 2001; 7: 45–53.
Fraser M, Thomas DF, Pitt E, Harnden P, Trejdosiewicz LK, Southgate J . A surgical model of composite cystoplasty with cultured urothelial cells: a controlled study of gross outcome and urothelial phenotype. BJU Int 2004; 93: 609–616.
Matsunuma H, Kagami H, Narita Y, Hata K, Ono Y, Ohshima S et al. Constructing a tissue-engineered ureter using a decellularized matrix with cultured uroepithelial cells and bone marrow derived mononuclear cells. Tissue Eng 2006; 12: 509–518.
Lalu MM, McIntyre L, Pugliese C, Fergusson D, Winston BW, Marshall JC et al. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS One 2012; 7: e47559.
Qiu X, Lin H, Wang Y, Yu W, Chen Y, Wang R et al. Intracavernous transplantation of bone marrow-derived mesenchymal stem cells restores erectile function of streptozocin-induced diabetic rats. J Sex Med 2011; 8: 427–436.
Qiu X, Sun C, Yu W, Lin H, Sun Z, Chen Y et al. Combined strategy of mesenchymal stem cells injection with VEGF gene therapy for the treatment of diabetes associated erectile dysfunction. J Androl 2012; 33: 37–44.
Gou X, He WY, Xiao MZ, Qiu M, Wang M, Deng YZ et al. Transplantation of endothelial progenitor cells transfected with VEGF165 to restore erectile function in diabetic rats. Asian J Androl 2011; 13: 332–338.
Garcia MM, Fandel TM, Lin G, Shindel AW, Banie L, Lin CS et al. Treatment of erectile dysfunction in the obese type 2 diabetic ZDF rat with adipose tissue derived stem cells. J Sex Med 2010; 7: 89–98.
Bahk JY, Jung JH, Han H, Min SK, Lee YS . Treatment of diabetic impotence with umbilical cord blood stem cell intracavernosal transplant: preliminary report of 7 cases. Exp Clin Transplant 2010; 8: 150–160.
Wu S, Wang Z, Bharadwaj S, Hodges SJ, Atala A, Zhang Y . Implantation of autologous urine derived stem cells expressing vascular endothelial growth factor for potential use in genitourinary reconstruction. J Urol 2011; 186: 640–647.
Ouyang B, Sun X, Han D, Chen S, Yao B, Gao Y et al. Human urine-derived stem cells alone or genetically-modified with FGF2 improve type 2 diabetic erectile dysfunction in a rat model. PLoS ONE 2014; 9: e92825.
Bahramsoltani M, De Spiegelaere W, Janczyk P, Hiebl B, Cornillie P, Plendl J . Quantitation of angiogenesis in vitro induced by VEGF-A and FGF-2 in two different human endothelial cultures - an all-in-one assay. Clin Hemorheol Microcirc 2010; 46: 189–202.
Masaki I, Yonemitsu Y, Yamashita A, Sata S, Tanii M, Komori K et al. Angiogenic gene therapy for experimental critical limb ischemia: acceleration of limb loss by overexpression of vascular endothelial growth factor 165 but not of fibroblast growth factor-2. Circ Res 2002; 90: 966–973.
Cao R, Brakenhielm E, Pawliuk R, Wariaro D, Post MJ, Wahlberg E et al. Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a combination of PDGF-BB and FGF-2. Nat Med 2003; 9: 604–613.
Byrne RR, Henry GD, Rao DS, Huynh TT, Pippen AM, Annex BH et al. Vascular endothelial growth factor restores corporeal smooth muscle function in vitro. J Urol 2001; 165: 1310–1315.
Lee MC, El-Sakka AI, Graziottin TM, Ho HC, Lin CS, Lue TF et al. The effect of vascular endothelial growth factor on a rat model of traumatic arteriogenic erectile dysfunction. J Urol 2002; 167: 761–767.
Bivalacqua TJ, Deng W, Kendirci M, Usta MF, Robinson C, Taylor BK et al. Mesenchymal stem cells alone or ex vivo gene modified with endothelial nitric oxide synthase reverse age associated erectile dysfunction. Am J Physiol Heart Circ Physiol 2007; 292: H1278–H1290.
Cao B, Huard J . Muscle-derived stem cells. Cell Cycle 2004; 3: 104–107.
Choi A, Kim SD, Sohn DW, Kim DB, Kim HW, Cho SY et al. The effect of human umbilical cord blood derived mesenchymal stem cell therapy in rat model of cavernosal nerve injury. Korean J Androl 2008; 26: 136–141.
Woo JC, Bae WJ, Kim SJ, Kim SD, Sohn DW, Hong SH et al. Transplantation of muscle-derived stem cells into the corpus cavernosum restores erectile function in a rat model of cavernous nerve injury. Korean J Urol 2011; 52: 359–363.
Mangir N, Akbal C, Tarcan T, Simsek F, Turkeri L . Mesenchymal stem cell therapy in treatment of erectile dysfunction: autologous or allogeneic cell sources? Int J Urol 2014; 21: 1280–1285.
Yilmaz D, Bayatli N, Un O, Kadowitz PJ, Sikka SC, Gur S . The effect of intracavernosal avanafil, a newer phosphodiesterase-5 inhibitor, on neonatal type 2 diabetic rats with erectile dysfunction. Urology 2014; 83: e7–e12.
da Costa Gonçalves AC, Fraga-Silva RA, Leite R, Santos RA . AVE 0991, a non-peptide Mas-receptor agonist, facilitates penile erection. Exp Physiol 2013; 98: 850–855.
Lasker GF, Pankey EA, Allain AV, Dhaliwal JS, Stasch JP, Murthy SN et al. Analysis of erectile responses to BAY 41-8543 and muscarinic receptor stimulation in the rat. J Sex Med 2013; 10: 704–718.
Nunes KP, Costa-Gonçalves A, Lanza LF, Cortes SF, Cordeiro MN, Richardson M et al. Tx2-6 toxin of the Phoneutria nigriventer spider potentiates rat erectile function. Toxicon 2008; 51: 1197–1206.
Nunes KP, Toque HA, Borges MH, Richardson M, Webb RC, de Lima ME . Erectile function is improved in aged rats by PnTx2-6, a toxin from Phoneutria nigriventer spider venom. J Sex Med 2012; 9: 2574–2581.
Xie D, Pippen AM, Odronic SI, Annex BH, Donatucci CF . Intracavernosal basic fibroblast growth factor improves vasoreactivity in the hypercholesterolemic rabbit. J Sex Med 2006; 3: 223–232.
Park K, Ahn KY, Kim MK, Lee SE, Kang TW, Ryu SB . Intracavernosal injection of vascular endothelial growth factor improves erectile function in aged rats. Eur Urol 2004; 46: 403–407.
Gou X, He WY, Xiao MZ, Qiu M, Wang M, Deng YZ et al. Transplantation of endothelial progenitor cells transfected with VEGF165 to restore erectile function in diabetic rats. Asian J Androl 2011; 13: 332–338.
Lasker GF, Matt CJ, Badejo AM Jr, Casey DB, Dhaliwal JS, Murthy SN et al. Intracavernosal administration of sodium nitrite as an erectile pharmacotherapy. Can J Physiol Pharmacol 2010; 88: 770–776.
Sung HH, Ahn JS, Kim JJ, Choo SH, Han DH, Lee SW . The role of intracavernosal injection therapy and the reasons of withdrawal from therapy in patients with erectile dysfunction in the era of PDE5 inhibitors. Andrology 2014; 2: 45–50.
Nelson CJ, Hsiao W, Balk E, Narus J, Tal R, Bennett NE et al. Injection anxiety and pain in men using intracavernosal injection therapy after radical pelvicsurgery. J Sex Med 2013; 10: 2559–2565.
Hsiao W, Bennett N, Guhring P, Narus J, Mulhall JP . Satisfaction profiles in men using intracavernosal injection therapy. J Sex Med 2011; 8: 512–517.
Mulhall JP, Simmons J . Assessment of comparative treatment satisfaction with sildenafil citrate and penile injection therapy in patients responding to both. BJU Int 2007; 100: 1313–1316.
Kim SC, Chang IH, Jeon HJ . Preference for oral sildenafil or intracavernosal injection in patients with erectile dysfunction already using intracavernosal injection for >1 year. BJU Int 2003; 92: 277–280.
El-Sakka AI, Yassin AA . Amelioration of penile fibrosis: myth or reality. J Androl 2010; 31: 324–335.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declare no conflict of interest.
Rights and permissions
About this article
Cite this article
El-Sakka, A. What is the current role of intracavernosal injection in management of erectile dysfunction?. Int J Impot Res 28, 88–95 (2016). https://doi.org/10.1038/ijir.2016.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2016.14
- Springer Nature Limited
This article is cited by
-
Utility of dynamic MRA in the evaluation of male erectile dysfunction
Abdominal Radiology (2020)