Abstract
Purpose of Review
This study aimed to review recent evidence on conservative non-surgical options for erectile dysfunction (ED) in men. A narrative review of the literature was performed. A comprehensive search in the MEDLINE, Embase, and Cochrane databases was done. Papers in English language, published from May 2017 until May 2022, were included. Papers reporting basic research or animal research were excluded, as long as reviews or meta-analyses. Congress reports, clinical cases, or clinical trials protocols with no results were also excluded.
Recent Findings
We found a multitude of different treatment modalities for ED. We must take into account the type of patient, their comorbidities, the origin of their ED, and its severity in order to reproduce effective results using these therapies. Some of the treatments show good results with a good level of evidence (new IPDE5 formulations, intracavernous injections, shock wave therapy, hormonal theraphy, psycho-sexual theraphy). However, others (some new molecules, stem cell theraphy, platelet-rich plasma injections, oxygenation-based therapy, nutraceuticals), although some of them present promising results, require randomized studies with a larger number of patients and a longer follow-up time to be able to establish firm recommendations.
Summary
Regarding the conservative treatment of erectile dysfunction, in recent years, some therapies have been consolidated as effective and safe for certain types of patients. On the other hand, other treatment modalities, although promising, still lack the evidence and the necessary follow-up to be recommended in daily practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Erectile dysfunction (ED) is defined as the persistent inability to achieve and maintain an erection hard enough to permit satisfactory sexual intercourse [1]. According to the five-item International Index of Erectile Function questionnaire (IIEF-5) score, ED severity is classified on severe (score 1–7), moderate (8–11), mild-moderate (12–16), mild (17–21), and no ED (22–25) [2].
ED has become a major health concern even in younger men, causing a significant impact on men’s quality of life [3]. Its prevalence varies on the different series published, but it is constantly high. In the Boston area, 52% of men between 40 and 70 years old were shown to suffer some grade of ED, according to the Massachusetts Male Aging Study (MMAS) [4]. Generally, ED can be considered as a natural part of aging, and its prevalence increases with age, ranging from 12% in those men < 59 years, 22% in men 60–69 years, and 30% in men > 69 years old, as per a population-based study of US health professionals [5]. In a cross-sectional real-life study performed among men asking for their first medical help for new-onset ED, 25% of patients were younger than 40 years old, with almost 50% of the younger men complaining of severe ED [6]. It is expected that by the end of 2025, the number of ED cases can rise to as high as 322 million across the world [7].
Treatment of ED has evolved along the years, with the introduction of sildenafil, the first 5-phosphodiesterase inhibitor (5-PDEi), as a major milestone in the late 1990s [8]. Since then, clinical practice guidelines have established different algorithms and recommendations, usually proposing therapeutic lines depending on the invasiveness of the treatments [9]. But recently, the European Association of Urology Guidelines on Sexual and Reproductive Health have proposed some changes in this paradigm [10]. Thereby, some treatments are no longer considered second-line options, and they can be offered to patients according to their preferences and their clinical situation, like intracavernous injections (ICI) or topical or intraurethral alprostadil. Also, some treatments previously considered experimental have recently been included in clinical practice guidelines according to their growing scientific evidence, like shockwave therapy. In the present paper, we aimed to comprehensively review the evidence on non-surgical treatments for ED of the last 5 years (2017–2022), focusing on the new developments.
Methods
Search Strategy
A non-systematic review of the literature was carried out using the MeSH terms “erectile dysfunction/drug therapy” or “erectile dysfunction/therapy,” or using free language terms, erectile dysfunction and treatment or therap*, from May 2017 to May 2022. Language was limited to English. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) recommendations [11] were used to guide reporting of the study. The search was initially carried out in the electronic database PubMed and identified a total of 1871 articles. The search was then limited separately to articles published in EMBASE and Cochrane (1512 publications). Both searches were subsequently compared, duplicates eliminated, and a final total of 2729 articles identified for review.
Eligibility Criteria
Only original papers of clinical prospective and retrospective studies assessing the outcomes of different conservative (non-surgical) therapies for ED in men > 18 years old were included for revision. Therefore, papers reporting basic research or animal research were excluded, as long as reviews or meta-analyses. Congress reports, clinical cases, or clinical trials protocols with no results were also excluded. Papers reporting the results of rehabilitation therapy for ED after radical pelvic surgery were not considered for revision.
Study Selection and Data Extraction
A total of 2729 papers were reviewed by two different experts in the field. After filtering for the previous inclusion/exclusion criteria, and excluding those not matching the search criteria in terms of date, language, and publication type, a total of 199 papers were finally considered for revision. The process of paper selection is represented in Fig. 1. Then, relevant data from these papers were extracted, considering the interventional type of treatment, type of ED, the number of patients included, the follow-up period, rate of success in correcting ED, the tool used to measure ED, adverse events, and satisfaction rate, if available. Each study was identified by the first author and year of publication.
Results
Psycho-sexual Therapy
A total of seven papers evaluating phyco-sexual interventions to treat DE were included, and their characteristics are resumed in Table 1.
Cognitive behavioral sexual therapy (CBST) is the most common intervention studied, with five out of the seven papers evaluating it. In four of them, only non-organic erectile dysfunction (NOED) patients were included, whereas in the remaining three, psycho-sexual therapy was studied in order to improve the results in any kind of ED. Six of the papers analyzed showed a significant and positive result of the psycho-sexual therapies in improving DE, according to the scores of the different questionnaires used. The study by Bossio et al. [17] found a positive but not significant effect of a mindfulness intervention in a small sample of 10 patients with NOED.
Hormonal Therapy
Six papers studied the effect of testosterone therapy (TT) to improve ED as a single therapy in hypogonadal men [19–24], with different formulations. All of them showed a benefit of the TT, according to the scores of the IIEF-EF or the IIEF-5. The remaining paper compared the results of TT alone or in combination with tadalafil 10 mg on alternate days [25], in a randomized, crossover study with 29 patients. It demonstrated higher satisfaction rates in the combination group.
5-PDE5i
Forty papers investigating the effects of PDE5is were identified. The results are resumed in Table 2.
Topical Drugs
Two papers analyzed the use of topical alprostadil to treat ED. In one of them [66], 71 patients were randomized to receive 300 μg of alprostadil over the glans, as the standard administration route, or within the urethral meatus, as an alternative administration route. The results showed that the alternative administration route achieved better results in terms of IIEF-5 score (+ 3.8 vs + 6.3, p < 0.001), and positive response to sex encounter profile (SEP)-2 (10 vs 27, p < 0.001), with no differences in the profile safety. The paper by Garrido-Abad et al. [67] evaluated the efficacy of topical alprostadil alone or in combination with maximum doses of PDE5i in patients non-responding to PDE5i alone. Those in the combination group presented higher IIEF-5 scores after the treatment (12.4 vs 17.1, p < 0.001), whereas those in the alprostadil alone group showed no significant improvement (12.2 vs 12.7, p = 0.148).
A randomized, placebo-controlled trial by Ralph et al. [68] assessed the efficacy of a novel topical gel containing 0.2% of glyceryl trinitrate (GNT), and is currently under investigation to become an agent to treat ED. It is supposed to have a fast absorption, minutes-length erection, and satisfactory safety profile. Treated patients showed a slight but significant higher score in the IIEF-EF comparing with those receiving placebo (19.6 vs 18.5, p = 0.0132), with a greater increase in the mild ED group (23.1 vs 21.3, p < 0.001).
Shockwave Therapy
A number of 29 papers analyzing the results of different regimes of shockwave therapy in the management of ED were identified. Their results are resumed in Table 3.
Stem Cells
A total of 10 papers evaluating the utility of stem cells for ED were found. Great heterogenicity was found in respect to the type of stem cell used: in four [114–117], they used bone marrow cells, whereas in the other six, they used mesenchymal stem cells [118–123]. Additionally, other paper studied the effect of stem cell-derived bioactive molecules to restore erectile function (EF) [124]. In all of them, ED is evaluated according to IIEF-5, and in half of them, they also include an assessment of penile hemodynamics with a color Doppler ultrasound. The number of patients included is low in all of them (5-40), 8 papers being pilot phase I studies. Only one [119] is a randomized single-blinded clinical trial, in which 20 diabetic, PDE5i non-responder patients were administered either intracavernosal autologous mesenchymal stem cells or placebo. In the treatment group, mean IIEF-5 score was 7.2 ± 2.1, 9.2 ± 3.4, and 10.6 ± 4.7 before, 3 months, and 6 months after the injection, respectively (p = 0.01). This follow-up time is common in most of the studies, with the exception of the one by Yiou et al. [117], with a mean follow-up of 62.1 ± 11.7 months, in which a slow decline on EF was observed after the improvement in the first year. This trend was also observed in other papers with lower follow-up times [120, 122].
Phytotherapy/Nutraceuticals
Twenty-six papers investigating the effect in DE of different phytotherapy or nutraceutical agents have been identified. Nineteen studies analyzed the effect of as many substances in mild ED or special-to-treat patients [125–142]. Most of them showed a positive effect of these substances as a single therapy or, most commonly, as a concomitant treatment added to a standard oral therapy.
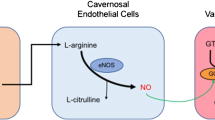
Three papers investigated the utility of l-arginine for patients with ED. Gallo et al. [143] demonstrated that the combination of l-arginine and oral daily tadalafil 5 mg was superior to both therapies alone (IIEF-EF: + 7.1 vs + 3.1 vs + 6, respectively, p < 0.0001). Similar results were reported by Abu El-Hamd et al. [144] (SHIM: + 13.69 vs + 10.33 vs 12.27, p < 0.0001), who also found that treatment with l-arginine, tadalafil, or its combination conducted to a significative increase in testosterone levels in all patients, in contrast to placebo (+ 2.37 vs + 9.04 vs + 11.23 nmol/L for l-arginine, tadalafil, and combination groups, respectively; p < 0.0001). In a recent study, Menafra et al. [145] showed that supplementation with high doses of l-arginine alone for 3 months conducted to an increase in the score of the IIEF-6 (+ 4, p < 0.0001) and in the peak systolic volume (PSV) (+ 4.6 cm/s, p < 0.0001) in contrast to placebo.
Tribulus terrestris is a plant originating from Bulgaria that is considered to be an herbal steroid. Its effect in ED in hypogonadal men has been investigated by GamalEl Din et al. [146], where they found an improvement in IIEF-5 score (+ 5.4, p < 0.0001) and in the testosterone levels (+ 0.58 nmol/L, p < 0.0001), compared to placebo. Kamenov et al. [147] conducted a RCT in a cohort of 180 patients with mild or moderate ED who were treated with Tribulus or placebo. After 12 weeks, they found a significant difference in IIEF scores for the treatment group (+ 4.75 vs 1.97, p < 0.0001).
The response to vitamin D supplementation in patients with ED and deficiency of this element has been studied in two papers, both comparing the effect of regular tadalafil intake only or in combination with vitamin D. Demirci et al. [148] found better scores in IIEF-EF in the combination group after 3 months (+ 13 vs + 8, p = 0.01), similarly to Ali et al. [149] that found a higher improvement in IIEF-5 scores in the combination group compared to tadalafil only (+ 8.44 vs + 5.72, p = 0.012).
Platelet-Rich Plasma Injections
Intracavernosal therapy with platelet-rich plasma (PRP) was assessed in 6 papers in the last years. Their results are presented in Table 4.
Effect of Previously Known Molecules on ED
The effect of different established drugs for other indications has been studied in several papers, including mirabegron, aspirin, bupropion, cabergoline, and levotiroxin.
Mirabegron is a selective β3 adrenergic receptor agonist that is supposed to cause relaxation of the vascular smooth muscle cells of the corpora cavernosa [156]. Its effect on ED has been studied in two recent articles. In the first, a pilot study by Karakus et al. [157], 20 patients with DE and lower urinary tract symptoms (LUTS) were administered mirabegron for 12 weeks. After this period, 38.5% of the patients improved the IIEF-5 score ≥ 4 points, whereas in 61.5 there was no variation. These results were widely studied in a RCT by Elbaz et al. [158], in which 55 patients with ED and LUTS were randomized to receive mirabegron and doxazosin (treatment group) or tolterodine and doxazosin (control) for 12 weeks. The found a significant difference in IIEF score improvement between both groups (+ 15 vs + 3, p < 0.05).
Aspirin has also been evaluated as a potential treatment for ED, given its antiplatelet action. In a paper by Bayraktar and Albayrak [159], 184 patients with vasculogenic ED were randomized to take aspirin 100 mg daily for 6 weeks or placebo. They found significant differences in IIEF-EF (+ 7.2 vs + 2, p < 0.0001), and in the SEP 2 and 3. The same group published later the results of a study in which 336 patients were randomized to take aspirin 100 mg daily, tadalafil 5 mg daily, both drugs, or placebo for 6 weeks [160]. They found similar improvements in IIEF-EF scores in all treatment groups, with a weaker increment in the placebo group (+ 7.2, + 7.3, + 7.5, p < 0.0001 vs + 2.0, p = 0.0204).
Bupropion is an antidepressant with a dual reuptake inhibitor of dopamine and norepinephrine mechanism, and it has been hypothesized to have a benefit on DE. Ghoreishi et al. [161] studied its effects on a cohort of 40 patients with chronic kidney disease, who were randomized to treatment or placebo. After a 10-week period, changes in the IIEF were higher in the treatment than in the control group (+ 2.75 vs + 0.35, p < 0.005). Similarly, Yee et al. [162] studied the effect of bupropion against placebo on a randomized cohort of 80 male patients on methadone with ED for 6 weeks. Significant changes in the IIEF score (+ 8.37, p = 0.02) and in the total plasma testosterone level (+ 4.03 nmol/L, p = 0.01) were observed.
The effect of adding cabergoline to daily tadalafil was compared to daily tadalafil alone in a group of 580 patients diagnosed with psychogenic ED in a paper by Mohammad et al. [163]. They found that 92.7% of the patients in the combination group improved the EF, in contrast with a 53.6% of the patients in the tadalafil group (p < 0.05). Cannarella et al. [164] found that levothyroxine improved arterial ED in patients with subclinical hypothyroidism, according to IIEF-5 score (20.2 in the treatment group, no changes in the control group, p < 0.05). Also, a subanalysis of a systolic blood pressure intervention trial [165] found that an intensive treatment of high systolic blood pressure (goal of < 120 mmHg), in contrast to a standard treatment (goal of < 140 mmHg), had very small impact on ED, according to IIEF-5.
ICI of Vaso-active Agents
A total of six papers analyzing the effect of different types of intracavernosal botulinum toxin injections were evaluated, and the results are resumed in Table 5.
Besides, other ICI were studied in three more papers. Taşkapu et al. [172] demonstrated that adding clomiphene citrate to alprostadil 10 or 20 μg in late-onset hypogonadism men offered great results in ED scores (IIEF-EF + 11.07, EHS + 1.52, p < 0.001). Bernie et al. [173] compared a classical empirical approach algorithm of ICI to a new, risk-based approach, not observing significant differences in multiple domains of sexual function. A retrospective study by Bearelly et al. [174] showed that a cohort of 105 patients treated with different ICI combinations presented good response to their ED after a mean duration of therapy of 8.4 years, according to the IIEF-EF scores (+ 11.8, p < 0.05).
Oxygenation-Based Therapies
The effect on ED of both continuous positive airway pressure (CPAP) and hyperbaric oxygen therapy (HBOT) has been investigated. The results for these therapies are resumed in Table 6.
Other Physical Therapies
Finally, four articles were classified under the epigraph of “other physical therapies.” Two papers referred to the effect of electrostimulation (ES) in the management of ED. The first [183] was a RCT that compared a group of 15 young patients (39.17 ± 6.21) who received ES with another 15 who were proposed to aerobic exercise. After 6 weeks, the ES group presented a better score in the IIEF-5 compared to the exercise group (20.83 vs 14.33, p = 0.001). Similarly, the second paper [184] compared ES against a control group in a cohort of 22 patients, finding better significative (p < 0.05) scores in the IIEF-5 and EHS for the treatment group.
One paper [185] presented the results of a novel therapy of low-intensity pulsed ultrasound (LIPUS) in treating mild to moderate ED. A total of 120 patients were randomized to LIPUS [80] or sham treatment. They defined success as an improvement in the IIEF-5 ≥ 2 points, being the response after the complete therapy of 71.01% of patients in the LIPUS arm compared to 17.65% in the sham group (p < 0.05).
Finally, Juho et al. [186] presented a study in which they evaluated the efficacy of a far-infrarred textile on the underwear of 30 patients with vasculogenic ED, who were randomized to wear the assessed underwear or a regular one. Although an improvement on the IIEF-5 score, the PSV, and the end diastolic flow was observed, it did not reach statistical significance.
Discussion
Studies related to psycho-sexual therapy are quite heterogeneous, most dealing with psychogenic ED in young patients. Cognitive behavioral therapy is the most studied treatment modality. Treatment combining cognitive-behavioral therapy and PDE5is achieves improvements in ED, as well as a significant reduction in anxiety and depression compared to PDE5is monotherapy [12•, 13, 16, 18]. A pilot study [17], with a reduced number of patients (n = 10) and no control group, studied the use of mindfulness-based group therapy in situational ED. No significant improvements in ED or overall satisfaction were appreciated. According to the analyzed data, it seems that psycho-sexual therapy, and specifically cognitive behavioral therapy (CBT), may be a useful treatment for the treatment of psychogenic ED in young patients, improving the effect of oral therapies in some cases and reducing anxiety and depression associated with the disease.
Hormone replacement therapy, both in monotherapy [19–24] and in combination with PDE5is [25], has shown significant benefits in the treatment of EF in patients with hypogonadism. This represents a reminder of the need of requesting testosterone levels in the study of patients with ED and offers hormonal treatment if needed.
With regard to classical oral treatments of 5-phosphodiesterase inhibitors, there have been no major developments in the last 5 years. In fact, we have only found in this review a single study on a new molecule: mirodenafil [26]. Sildenafil, vardenafil, tadalafil, and avanafil are still the most used PDE5is. Trials comparing the efficacy and safety of PDE5is are still lacking, with available data suggesting similar efficacy and safety profiles [27, 58]. Many publications report the effectiveness of daily tadalafil therapy, but there is still little published evidence comparing its efficacy versus on-demand use for the treatment of erectile dysfunction [56]. We found quite a few publications that study the recent new formulations: orodispersible tablets (ODT) [65], orodispersible films (ODF) [26, 33, 38, 61], and orally disintegrating strips [29]. These may be an advantage for patients who have difficulty swallowing tablets and for those who will benefit of a rapid onset of action, because of the more discreet route of administration which some patients may prefer.
The application of alprostadil inside the urethra has shown greater efficacy compared to classic topical administration with a similar safety profile [66, 67]. In addition, the combination therapy of alprostadil administered intraurethral together with 5-phosphodiesterase inhibitors [67] showed better results in the treatment of ED compared to inhibitors in monotherapy.
Regarding low-intensity shockwave therapy (Li-ESWT), there are very heterogeneous studies, even if they study the same treatment modality. This is due to several factors such as the diversity of treatment protocols (energy, type of focus, duration of sessions, number of sessions, etc.), the different devices used, the combination or not of other therapies, and the different evaluation methods. Due to this great heterogeneity regarding different energies and administration protocols, several articles strive to compare different treatment modalities [78, 81, 86, 87, 105]. The results proved to be comparable in the different evaluators’ treatment methods, without statistically significant differences. Li-ESWT is a clinically effective and safe treatment for erectile dysfunction regardless of generator type, source, emitted shock wave morphology, and treatment protocol [105, 107, 110, 113]. Most common inhibitor included in the Li-ESWT protocol is tadalafil [92, 93, 95, 104]. The preferred dose is 5 mg daily. Most of the studies showed a significant improvement in EF and penile rigidity, which was greater when the use of Li-ESWT was combined with PDEis, without reporting significant changes in its safety profile. Several publications [76, 104, 111] conclude that Li-ESWT is also effective in patients refractory to PDE5is, being able to directly improve their EF in some and make them respond to oral treatment in others. Results are better in younger patients, with ED of vascular origin, with fewer comorbidities, and with mild or moderate ED [107, 108, 111]. Long-term loss of efficacy has been reported, suggesting the need for follow-up and the possibility of repeating therapy [71•, 88, 107]. Li-ESWT appears to be an effective and safe method for the treatment of erectile dysfunction in diabetic patients [100, 101, 109]. Other studies demonstrated the efficacy and safety of Li-ESWT treating ED in patients with chronic pelvic pain syndrome [97], post-prostatectomy [99], pelvic fractures with urethral damage [104], and renal transplant patients [103].
The vast majority of available studies on stem cell therapy (SCT) had a small sample size, had no control group, and had other relevant methodological limitations. Due to the heterogeneity present in the studies regarding the type, the optimal dose, or the route of administration of SCT, the comparison of results is very difficult. Despite encouraging initial results in terms of efficacy and safety, these issues do not yet allow firm conclusions to be drawn.
The use of nutraceuticals as a treatment for erectile dysfunction is controversial. Patients may perceive this type of therapy as more natural and safer. In addition, they can be obtained without a prescription and bought online and lack adequate health controls [187]. The use of nutraceuticals in erectile dysfunction has a very ancient history and has its roots in traditional Chinese medicine and Ayurvedic medicine [188]. Promising improvements in EF have recently been described with different nutraceuticals: l-arginine [143–145], Tribulus terrestris [146, 147], vitamin D [148, 149], panax ginseng [126], l-citrulline [127, 128], muira puama [133], and Ginkgo biloba [125]. However, the available studies on the subject are methodologically heterogeneous and generally of low quality, often reporting contradictory results, so recommendations on its use have not yet been established [9, 10].
We found 6 papers that analyze the effect of intracavernous injections PRP for the treatment of erectile dysfunction. Only one of the papers [153•] is a double-blind, randomized, placebo-controlled clinical trial. It is also the one that analyzes a greater number of patients (n = 60), obtaining a significant improvement in EF and patient satisfaction. Most studies [150, 151, 154, 155] reported statistically and clinically significant improvements in EF. In addition, smoking status, HbA1C, and severity of ED before treatment were strengthened as negative predictors of response to treatment [150, 154]. In general, no significant adverse effects were reported in any of the studies, the most frequent being mild pain at the injection site and mild penile bruising [151]. Therefore, analyzing the limited data available, it suggests that PRP can be used successfully for the treatment of ED. However, the available data is limited by its small sample size, short follow-up, and/or lack of controls. We also do not have standardized methods to prepare PRP or standardized treatment protocols.
In the last 5 years, the effect on EF of several drugs used for the treatment of other pathologies has been studied. Published papers include mirabegron [156, 157], aspirin [159, 160], bupropion [161, 162], cabergoline [163], and levothyroxine [164]. Most of the studies, although they analyzed different and special populations, found a significant difference in the improvement of ED. Only a few works did not find significant differences [160, 165]. It remains to be determined and it can be discussed whether the improvement in EF in some cases is due directly to the effect of the molecule or to the improvement of the underlying pathology of the patient (e.g., LUTS, hypothyroidism).
The use of intracavernous injections of botulinum toxin for the treatment of ED has recently been studied. We found three retrospective studies [166, 167, 171], and three double-blind randomized clinical trials [168, 169, 170•]. An improvement in the EF of patients was demonstrated, improving the results at high doses [168, 170•]. However, this therapy, although promising, still lacks long-term results, unlike the classic vaso-active drugs for the treatment of ED [174].
We have found five studies evaluating the effect of CPAP on EF [175, 176, 178–180]. In total, they include 318 patients with a follow-up time of between 3 and 12 months. Only one of the works is a clinical trial against placebo [180]. The correct use of CPAP improved both EF, sexual desire, general sexual satisfaction, self-esteem, relationship, and treatment, as well as drowsiness and quality of life. This improvement in EF was clinically significant in all but one study [176]. In addition, a trend of correlation between improvement in EF and hours of CPAP use was reported [175, 179].
Three papers have also been published [177, 181, 182] that evaluate the efficacy of hyperbaric therapy on EF. Significant improvements in IIEF and absence of adverse effects were reported. Unfortunately, all three are prospective pilot studies with a very short follow-up time (5-6 weeks). Innovatively, one of the works also demonstrates a significant improvement in angiogenesis measured by perfusion magnetic resonance imaging [182]. Therapies based on improving tissue oxygenation also seem promising therapies for the treatment of ED; however, the evidence is still scarce and long-term follow-up studies are lacking.
Conclusion
Numerous publications related to the conservative treatment of ED have been carried out. The significant rate of discontinuation of available therapies and the paucity of curative options prompted research on possible new treatments. In some cases, we must take into account the type of patient, their comorbidities, the origin of their ED, and its severity in order to reproduce effective results using these therapies. Some of these new treatments show good results with a good level of evidence (new PDE5i formulations, intracavernous injections, Li-ESWT, hormonal therapy). However, others (some new molecules, SCT, PRP, oxygenation-based therapies), although they present promising results, require better quality studies to establish firm recommendations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270(1):83–90.
Alwaal A, Awad M, Boggs N, Kuzbel J, Snoad B. Sexual Health Inventory for Men Questionnaire as a Screening Method for Erectile Dysfunction in a General Urology Clinic. Sex Med. 2020;8(4):660–3.
Nguyen HMT, Gabrielson AT, Hellstrom WJG. Erectile Dysfunction in Young Men-A Review of the Prevalence and Risk Factors. Sex Med Rev. 2017;5(4):508–20.
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151(1):54–61.
Bacon CG, Mittleman MA, Kawachi I, Giovannucci E, Glasser DB, Rimm EB. Sexual function in men older than 50 years of age: results from the health professionals follow-up study. Ann Intern Med. 2003;139(3):161–8.
Capogrosso P, Colicchia M, Ventimiglia E, Castagna G, Clementi MC, Suardi N, et al. One patient out of four with newly diagnosed erectile dysfunction is a young man–worrisome picture from the everyday clinical practice. J Sex Med. 2013;10(7):1833–41.
Islam MM, Naveen NR, Anitha P, Goudanavar PS, Rao GSNK, Fattepur S, et al. The Race to Replace PDE5i: Recent Advances and Interventions to Treat or Manage Erectile Dysfunction: Evidence from Patent Landscape (2016–2021). J Clin Med. 2022;11(11):3140.
Goldstein I, Lue TF, Padma-Nathan H, Rosen RC, Steers WD, Wicker PA. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338(20):1397–404.
Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, Hakim LS, et al. Erectile Dysfunction: AUA Guideline. J Urol. 2018;200(3):633–41.
Professionals SO. EAU Guidelines: Male Sexual Dysfunction [Internet]. Uroweb. [cited 2019 Apr 27]. Available from: https://uroweb.org/guideline/male-sexual-dysfunction/
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg Lond Engl. 2010;8(5):336–41.
• Bilal A, Abbasi NUH. Randomized Placebo Controlled Trial of Sildenafil Citrate, Cognitive Behavior Sex Therapy and Integrated Treatment in Men Diagnosed With Non Organic Erectile Dysfunction. Sex Med. 2022;10(1):100464. Cognitive behavioral therapy is the most studied treatment modality, comprising 5 of the 7 articles on psychosexual therapies. Of these, only this one article is a randomized clinical trial with placebo (Ahmad Bilal et al.) and it is also the one that includes the largest number of patients and the most recent.
Zhang Z, Gao X, Zhou Y, Yu C, Pimolsettapun J, Yang L, et al. Study on the combination of brief psychodynamic psychotherapy with Viagra in the treatment of non-organic ED. Gen Psychiatry. 2020;33(5):e100184.
Bilal A, Abbasi NUH. Cognitive Behavioral Sex Therapy: An Emerging Treatment Option for Nonorganic Erectile Dysfunction in Young Men: A Feasibility Pilot Study. Sex Med. 2020;8(3):396–407.
Wang Z, Tan H, Liu S, Zhang G. Effect of cognitive behavior intervention on improving psychological emotion and erectile dysfunction of chronic prostatitis patients. Acta Medica Mediterr. 2020;36(4):2507–13.
Khan S, Amjad A, Rowland D. Potential for Long-Term Benefit of Cognitive Behavioral Therapy as an Adjunct Treatment for Men with Erectile Dysfunction. J Sex Med. 2019;16(2):300–6.
Bossio JA, Basson R, Driscoll M, Correia S, Brotto LA. Mindfulness-Based Group Therapy for Men With Situational Erectile Dysfunction: A Mixed-Methods Feasibility Analysis and Pilot Study. J Sex Med. 2018;15(10):1478–90.
Khan S, Amjad A, Rowland D. Cognitive behavioral therapy as an adjunct treatment for Pakistani men with ED. Int J Impot Res. 2017 Sep;29(5):202–6.
Alwani M, Yassin A, Talib R, Al-Qudimat A, Aboumarzouk O, Al-Zoubi RM, et al. Cardiovascular Disease, Hypogonadism and Erectile Dysfunction: Early Detection, Prevention and the Positive Effects of Long-Term Testosterone Treatment: Prospective Observational. Real-Life Data Vasc Health Risk Manag. 2021;17:497–508.
Saad F, Caliber M, Doros G, Haider KS, Haider A. Long-term treatment with testosterone undecanoate injections in men with hypogonadism alleviates erectile dysfunction and reduces risk of major adverse cardiovascular events, prostate cancer, and mortality. Aging Male Off J Int Soc Study Aging Male. 2020;23(1):81–92.
Efesoy O, Çayan S, Akbay E. The Effect of Testosterone Replacement Therapy on Penile Hemodynamics in Hypogonadal Men With Erectile Dysfunction, Having Veno-Occlusive Dysfunction. Am J Mens Health. 2018;12(3):634–8.
Haider KS, Haider A, Doros G, Traish A. Long-Term Testosterone Therapy Improves Urinary and Sexual Function, and Quality of Life in Men with Hypogonadism: Results from a Propensity Matched Subgroup of a Controlled Registry Study. J Urol. 2018;199(1):257–65.
Yucel C, Keskin MZ, Peskircioglu CL. The Effect of Transdermal Testosterone Administration on Lower Urinary Tract Symptoms and Erectile Dysfunction: A Prospective, Randomized. Placebo-Controlled Trial Curr Urol. 2017;11(1):4–8.
Hackett G, Cole N, Saghir A, Jones P, Strange RC, Ramachandran S. Testosterone replacement therapy: improved sexual desire and erectile function in men with type 2 diabetes following a 30-week randomized placebo-controlled study. Andrology. 2017;5(5):905–13.
Narukawa T, Soh J, Kanemitsu N, Harikai S, Fujihara A, Ukimura O. Efficacy of testosterone replacement therapy plus alternate-day tadalafil for patients with late-onset hypogonadism: An open-label, randomized, crossover study. Int J Urol Off J Jpn Urol Assoc. 2021;28(4):376–81.
Lee SW, Son H, Lee SW, Cho KS, Moon DG, Yang DY, et al. Efficacy and Safety of Mirodenafil Oro-Dispersible Film in Korean Patients with Erectile Dysfunction: A Double-Blind, Randomized, Placebo-Controlled, Parallel-Group, Multicenter, Phase IV Study. World J Mens Health. 2022;40(2):280–9.
Kumar M, Pathade AD, Gupta SV, Goyal S, Rath D, Thakre M, et al. Efficacy and safety of avanafil as compared with sildenafil in the treatment of erectile dysfunction: A randomized, double blind, multicenter clinical trial. Int J Urol Off J Jpn Urol Assoc. 2022;29(4):351–9.
Cui WS, Guan RL, Lei HE, Liu JH, Wang T, Zhu SN, et al. Efficacy and safety of aildenafil citrate in Chinese men with erectile dysfunction: a multicenter, randomized, double-blind, placebo-controlled crossover trial. Transl Androl Urol. 2021;10(8):3358–67.
Sangkum P, Sirisopana K, Matang W, Phengsalae Y, Lertsithichai P, Ketsuwan C, et al. Efficacy of the Orally Disintegrating Strip Sildenafil for the Treatment of Erectile Dysfunction: A Prospective, Randomized Trial. Sex Med. 2021;9(6):100453.
Jiang H, Lin H, Li F, Dai Y, Zhang X, Jiang T, et al. Efficacy and Safety of Avanafil in Chinese Subjects With Erectile Dysfunction: A Multi-Center, Randomized, Double-Blinded, Placebo-Controlled Phase III Clinical Trial. Sex Med. 2021;9(3):100337.
Elkamshoushi AM, Badae NM, Kabary MG, Omar SI. Evaluation of daily avanafil efficacy in improving the endothelial function in Egyptian males with erectile dysfunction. Andrologia. 2021;53(1):e13833.
Law YXT, Tai BC, Tan YQ, Lata RNM, Lee KCJ. A Small Group Randomized Double-Blind Placebo-Controlled Study to Evaluate the Efficacy of Daily Pentoxifylline in the Management of Patients With Erectile Dysfunction with Suboptimal Treatment Response to Sildenafil. Sex Med. 2020;8(1):14–20.
Pavone C, Abrate A, Agiato S, Billeci S, Tulone G, Vella M, et al. Sildenafil orodispersible film in the treatment of erectile dysfunction after radical prostatectomy: A single-centre open-label uncontrolled trial. Andrologia. 2020;52(9):e13705.
Demirci A, Ozgur BC. The effect of using tadalafil 5 mg/day on neutrophil-lymphocyte and platelet-lymphocyte ratios in mild-medium and severe erectile dysfunction patients; and comparison of clinical response. Andrologia. 2019;51(9):e13347.
Pattanaik S, Kaundal P, Mavuduru RS, Singh SK, Mandal AK. Endothelial Dysfunction in Patients With Erectile Dysfunction: A Double-Blind, Randomized-Control Trial Using Tadalafil. Sex Med. 2019;7(1):41–7.
Jiang H, Zhao LM, Lin HC, Yan S, Liu JH, Zhu ZH, et al. Evaluation of the long-term safety and effectiveness of tadalafil once daily in Chinese men with erectile dysfunction: interim results of a multicenter, randomized, open-label trial. Asian J Androl. 2018;20(6):587–92.
Lee JG, Kim BD, Han CH, Lee KK, Yum KS. Evaluation of the effectiveness and safety of a daily dose of 5 mg of tadalafil, over an 8-week period, for improving quality of life among Korean men with andropause symptoms, including erectile dysfunction: A pilot study. Medicine (Baltimore). 2018;97(51):e13827.
Cocci A, Capece M, Cito G, Russo GI, Falcone M, Timpano M, et al. Effectiveness and Safety of Oro-Dispersible Sildenafil in a New Film Formulation for the Treatment of Erectile Dysfunction: Comparison Between Sildenafil 100-mg Film-Coated Tablet and 75-mg Oro-Dispersible Film. J Sex Med. 2017;14(12):1606–11.
Park HJ, Kim SW, Kim JJ, Lee SW, Paick JS, Ahn TY, et al. A Randomized, Placebo-Controlled, Double-Blind, Multi-Center Therapeutic Confirmatory Study to Evaluate the Safety and Efficacy of Avanafil in Korean Patients with Erectile Dysfunction. J Korean Med Sci. 2017;32(6):1016–23.
Li H, Bai G, Zhang X, Shi B, Liu D, Jiang H, et al. Effects of Two Different Dosages of Sildenafil on Patients With Erectile Dysfunction. Am J Mens Health. 2017;11(3):525–30.
Li G, Lan H, Liang J, Zhang C, Huang C. Efficacy of Tadalafil De-Escalation in the Treatment of Psychogenic Erectile Dysfunction. Urol Int. 2017;98(2):205–9.
Mohamed Gharib T, Abdel-Al I, Elatreisy A, Kandeel W, El-Shaer W, Abdrabuh AM, et al. Short- and long-term follow-up results of daily 5-mg tadalafil as a treatment for erectile dysfunction and premature ejaculation. Arab J Urol. 2022;20(1):49–53.
Tuken M, Culha MG, Serefoglu EC. Efficacy and safety of dapoxetine/sildenafil combination tablets in the treatment of men with premature ejaculation and concomitant erectile dysfunction-DAP-SPEED Study. Int J Impot Res. 2019;31(2):92–6.
Sebastianelli A, Morselli S, Spatafora P, Liaci A, Gemma L, Zaccaro C, et al. Outcomes of combination therapy with daily tadalafil 5 mg plus tamsulosin 0.4 mg to treat lower urinary tract symptoms and erectile dysfunction in men with or without metabolic syndrome. Minerva Urol Nephrol. 2021;73(6):836–44.
Sebastianelli A, Spatafora P, Frizzi J, Saleh O, De Nunzio C, Tubaro A, et al. Which Drug to Discontinue 3 Months After Combination Therapy of Tadalafil plus Tamsulosin for Men with Lower Urinary Tract Symptom and Erectile Dysfunction? Results of a Prospective Observational Trial. Eur Urol Focus. 2021;7(2):432–9.
Sebastianelli A, Spatafora P, Frizzi J, Saleh O, Sessa M, De Nunzio C, et al. Tadalafil 5 mg Alone or in Combination with Tamsulosin 0.4 mg for the Management of Men with Lower Urinary Tract Symptoms and Erectile Dysfunction: Results of a Prospective Observational Trial. J Clin Med. 2019;8(8):E1126.
Zhang Z, Li H, Zhang X, Dai Y, Park HJ, Jiann BP, et al. Efficacy and safety of tadalafil 5 mg once-daily in Asian men with both lower urinary tract symptoms associated with benign prostatic hyperplasia and erectile dysfunction: A phase 3, randomized, double-blind, parallel, placebo- and tamsulosin-controlled study. Int J Urol Off J Jpn Urol Assoc. 2019;26(2):192–200.
Amano T, Earle C, Imao T, Matsumoto Y, Kishikage T. Administration of daily 5 mg tadalafil improves endothelial function in patients with benign prostatic hyperplasia. Aging Male Off J Int Soc Study Aging Male. 2018;21(1):77–82.
Özkıdık M, Gökce Mİ, Yaman Ö. Efficacy of tadalafil treatment on erectile dysfunction in patients under dutasteride treatment: A prospective non-randomized comparative study. Turk J Urol. 2018;44(4):294–7.
Kim SW, Park NC, Lee SW, Yang DY, Park JK, Moon DG, et al. Efficacy and Safety of a Fixed-Dose Combination Therapy of Tamsulosin and Tadalafil for Patients With Lower Urinary Tract Symptoms and Erectile Dysfunction: Results of a Randomized, Double-Blinded. Active-Controlled Trial J Sex Med. 2017;14(8):1018–27.
Lee MK, Lee JH, Sohn SY, Lee SY, Jeong TY, Kim SC. Effect of low-dose tadalafil once daily on glycemic control in patients with type 2 diabetes and erectile dysfunction: a randomized, double-blind, placebo-controlled pilot study. Diabetol Metab Syndr. 2022;14(1):56.
Du L, Jia JH, Xue WY, Qi JC. Effect of tadalafil combined with atorvastatin on hemodynamics and sexual function in middle-aged and elderly patients with hyperlipidemia complicated with erectile dysfunction. Pak J Med Sci. 2021;37(7):1965–71.
Jagdish RK, Kamaal A, Shasthry SM, Benjamin J, Maiwall R, Jindal A, et al. Tadalafil improves erectile dysfunction and quality of life in men with cirrhosis: a randomized double blind placebo controlled trial. Hepatol Int. 2021 Nov 14;
Verri V, Nascimento AR, Brandao AA, Tibirica E. Effects of chronic type 5 phosphodiesterase inhibition on penile microvascular reactivity in hypertensive patients with erectile dysfunction: a randomized crossover placebo-controlled trial. J Hum Hypertens. 2021;35(4):360–70.
Thakur J, Rathi S, Grover S, Chopra M, Agrawal S, Taneja S, et al. Tadalafil, a Phosphodiesterase-5 Inhibitor, Improves Erectile Dysfunction in Patients With Liver Cirrhosis. J Clin Exp Hepatol. 2019;9(3):312–7.
Bolat MS, Cinar O, Akdeniz E, Aşcı R. Low dose daily versus on-demand high dose tadalafil in diabetic patients with erectile and ejaculatory dysfunction. Int J Impot Res. 2018;30(3):102–7.
Bolat MS, Özer İ, Cinar O, Akdeniz E, Aşcı R. The efficacy of low-dose tadalafil in patients undergoing hemodialysis with end-stage renal disease. Ren Fail. 2017;39(1):582–7.
Wang J, Wang YL, He Y, Li S, Zhang YP, Cheng YB, et al. Influencing Factors for Erectile Dysfunction of Young Adults with No Response to PDE5i. Curr Med Sci. 2021;41(3):529–34.
Zhang Y, Zhou W, Wu X, Liu G, Dai Y, Jiang H, et al. Cavernous artery intima-media thickness predicts the response to sildenafil in erectile dysfunction patients as a morphological parameter. Andrologia. 2021;53(8):e14149.
Boeri L, Capogrosso P, Ventimiglia E, Pozzi E, Chierigo F, Belladelli F, et al. Undiagnosed prediabetes status is associated with a reduced effectiveness of phosphodiesterase type 5 inhibitors in men with erectile dysfunction. Int J Impot Res. 2020;32(4):393–400.
Rocca MS, Vignoli A, Tenori L, Ghezzi M, De Rocco PM, Vatsellas G, et al. Evaluation of Serum/Urine Genomic and Metabolomic Profiles to Improve the Adherence to Sildenafil Therapy in Patients with Erectile Dysfunction. Front Pharmacol. 2020;11:602369.
Kızılay F, Kalemci S, Şimşir A, Altay B. Predisposing factors for erectile dysfunction and response to treatment in younger males: Are they different from those of older men? An observational-comparative study. Andrologia. 2020;52(2):e13495.
Jamaluddin null, Bansal M, Srivastava GK, Gupta NP. Role of Serum High-Sensitivity C-Reactive Protein as a Predictor of Therapeutic Response to Tadalafil in Patients With Erectile Dysfunction: A Prospective Observational Study. J Sex Med. 2019;16(12):1912–21.
Lacchini R, Muniz JJ, Nobre YTDA, Cologna AJ, Martins ACP, Tanus-Santos JE. Influence of arginase polymorphisms and arginase levels/activity on the response to erectile dysfunction therapy with sildenafil. Pharmacogenomics J. 2018;18(2):238–44.
Ogreden E, Oğuz U, Demirelli E, Tosun A, Yalçın O. Relationship between Response to PDE5 Inhibitors and Penile Duplex Doppler Ultrasound in Erectile Dysfunction. Med Sci Basel Switz. 2018;6(2):E28.
Cai T, Palumbo F, Liguori G, Mondaini N, Scroppo FI, Di Trapani D, et al. The intra-meatal application of alprostadil cream (Vitaros®) improves drug efficacy and patient’s satisfaction: results from a randomized, two-administration route, cross-over clinical trial. Int J Impot Res. 2019;31(2):119–25.
Garrido-Abad P, Senra-Bravo I, Manfredi C, Fernández-Pascual E, Linares-Espinós E, Fernández-Arjona M, et al. Combination therapy with topical alprostadil and phosphodiesterase-5 inhibitors after failure of oral therapy in patients with erectile dysfunction: a prospective, two-arm, open-label, non-randomized study. Int J Impot Res. 2022;34(2):164–71.
Ralph DJ, Eardley I, Taubel J, Terrill P, Holland T. Efficacy and Safety of MED2005, a Topical Glyceryl Trinitrate Formulation, in the Treatment of Erectile Dysfunction: A Randomized Crossover Study. J Sex Med. 2018;15(2):167–75.
Chung E, Bailey W, Wang J. A Prospective, Randomized, Double-Blinded, Clinical Trial Using a Second-Generation Duolith SD1 Low-Intensity Shockwave Machine in Males with Vascular Erectile Dysfunction. World J Mens Health. 2022 Jan 2;
Geyik S. A single-centre result of two courses of low-intensity shockwave therapy (Li-SWT) in erectile dysfunction. Andrologia. 2022;54(2):e14324.
• Chung E, Cartmill R. Evaluation of Long-Term Clinical Outcomes and Patient Satisfaction Rate Following Low Intensity Shock Wave Therapy in Men With Erectile Dysfunction: A Minimum 5-Year Follow-Up on a Prospective Open-Label Single-Arm Clinical Study. Sex Med. 2021;9(4):100384. It is a recent prospective study that differs from others due to its long follow-up time. This allows us to extract different results regarding the efficacy of shock wave therapy over time. The short follow-up time is one of the main weaknesses of the rest of the studies.
Akande TO, Akinwunmi OM, Adebayo SA, Akinyinka AO, Shittu OB. EFFICACY AND SAFETY OF LOW-INTENSITY EXTRACORPOREAL SHOCKWAVE THERAPY FOR TREATMENT OF VASCULAR ERECTILE DYSFUNCTION IN NIGERIAN MEN: REPORT OF A STUDY IN IBADAN, SOUTH-WEST NIGERIA. Ann Ib Postgrad Med. 2021;19(1):8–14.
Lei Q, Wang D, Liu C, Ji Z, Yan S. Comparison of the efficacy and safety of low-intensity extracorporeal shock wave therapy versus on-demand sildenafil for erectile dysfunction. Transl Androl Urol. 2021;10(2):860–8.
Ortac M, Özmez A, Cilesiz NC, Demirelli E, Kadıoğlu A. The impact of extracorporeal shock wave therapy for the treatment of young patients with vasculogenic mild erectile dysfunction: A prospective randomized single-blind, sham controlled study. Andrology. 2021;9(5):1571–8.
Palmieri A, Arcaniolo D, Palumbo F, Verze P, Liguori G, Mondaini N, et al. Low intensity shockwave therapy in combination with phosphodiesterase-5 inhibitors is an effective and safe treatment option in patients with vasculogenic ED who are PDE5i non-responders: a multicenter single-arm clinical trial. Int J Impot Res. 2021;33(6):634–40.
Vinay J, Moreno D, Rajmil O, Ruiz-Castañe E, Sanchez-Curbelo J. Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: a randomized double-blind sham-controlled clinical trial. World J Urol. 2021;39(6):2217–22.
Huang YP, Liu W, Liu YD, Zhang M, Xu SR, Lu MJ. Effect of low-intensity extracorporeal shockwave therapy on nocturnal penile tumescence and rigidity and penile haemodynamics. Andrologia. 2020;52(10):e13745.
Kalyvianakis D, Mykoniatis I, Memmos E, Kapoteli P, Memmos D, Hatzichristou D. Low-intensity shockwave therapy (LiST) for erectile dysfunction: a randomized clinical trial assessing the impact of energy flux density (EFD) and frequency of sessions. Int J Impot Res. 2020;32(3):329–37.
Kim KS, Jeong HC, Choi SW, Choi YS, Cho HJ, Ha US, et al. Electromagnetic Low-Intensity Extracorporeal Shock Wave Therapy in Patients with Erectile Dysfunction: A Sham-Controlled, Double-Blind, Randomized Prospective Study. World J Mens Health. 2020;38(2):236–42.
Lurz K, Dreher P, Levy J, McGreen B, Piraino J, Brevik A, et al. Low-Intensity Shockwave Therapy in the Treatment of Erectile Dysfunction. Cureus. 2020;12(11):e11286.
Patel P, Katz J, Lokeshwar SD, Molina M, Reis IM, Clavijo R, et al. Phase II Randomized, Clinical Trial Evaluating 2 Schedules of Low-Intensity Shockwave Therapy for the Treatment of Erectile Dysfunction. Sex Med. 2020;8(2):214–22.
Sramkova T, Motil I, Jarkovsky J, Sramkova K. Erectile Dysfunction Treatment Using Focused Linear Low-Intensity Extracorporeal Shockwaves: Single-Blind, Sham-Controlled, Randomized Clinical Trial. Urol Int. 2020;104(5–6):417–24.
Wang J, Luo L, Zhao S, Liu Y, Zhu Z, Zhao Z. Low intensity extracorporeal shockwave Therapy shifts PDE5i nonresponders to responders. Int Braz J Urol Off J Braz Soc Urol. 2020;46(6):934–42.
Wu SS, Ericson KJ, Shoskes DA. Retrospective comparison of focused shockwave therapy and radial wave therapy for men with erectile dysfunction. Transl Androl Urol. 2020;9(5):2122–8.
Fojecki GL, Tiessen S, Osther PJS. Effect of Linear Low-Intensity Extracorporeal Shockwave Therapy for Erectile Dysfunction-12-Month Follow-Up of a Randomized, Double-Blinded, Sham-Controlled. Study Sex Med. 2018;6(1):1–7.
Kalyvianakis D, Memmos E, Mykoniatis I, Kapoteli P, Memmos D, Hatzichristou D. Low-Intensity Shockwave Therapy for Erectile Dysfunction: A Randomized Clinical Trial Comparing 2 Treatment Protocols and the Impact of Repeating Treatment. J Sex Med. 2018;15(3):334–45.
Katz JE, Molina ML, Clavijo R, Prakash NS, Ramasamy R. A Phase 2 Randomized Trial To Evaluate Different Dose Regimens of Low-intensity Extracorporeal Shockwave Therapy for Erectile Dysfunction: Clinical Trial Update. Eur Urol Focus. 2018;4(3):336–7.
Kitrey ND, Vardi Y, Appel B, Shechter A, Massarwi O, Abu-Ghanem Y, et al. Low Intensity Shock Wave Treatment for Erectile Dysfunction-How Long Does the Effect Last? J Urol. 2018;200(1):167–70.
Ayala HAC, Cuartas JPS, Cleves DC. Impact on the Quality of Erections after Completing a Low-Intensity Extracorporeal Shock Wave Treatment Cycle on a Group of 710 Patients. Adv Urol. 2017;2017:1843687.
Tsai CC, Wang CJ, Lee YC, Kuo YT, Lin HH, Li CC, et al. Low-Intensity Extracorporeal Shockwave Therapy Can Improve Erectile Function in Patients Who Failed to Respond to Phosphodiesterase Type 5 Inhibitors. Am J Mens Health. 2017;11(6):1781–90.
Kalyvianakis D, Hatzichristou D. Low-Intensity Shockwave Therapy Improves Hemodynamic Parameters in Patients With Vasculogenic Erectile Dysfunction: A Triplex Ultrasonography-Based Sham-Controlled Trial. J Sex Med. 2017;14(7):891–7.
Gallo L, Pecoraro S, Sarnacchiaro P. Adjuvant daily therapy with L-arginine 2,500 mg and tadalafil 5 mg increases efficacy and duration of benefits of low-intensity extracorporeal shock wave therapy for erectile dysfunction: A prospective, randomized, single-blinded study with 1-year follow-up. Investig Clin Urol. 2022;63(1):83–91.
Mykoniatis I, Pyrgidis N, Zilotis F, Kapoteli P, Fournaraki A, Kalyvianakis D, et al. The Effect of Combination Treatment With Low-Intensity Shockwave Therapy and Tadalafil on Mild and Mild-To-Moderate Erectile Dysfunction: A Double-Blind, Randomized, Placebo-Controlled Clinical. Trial J Sex Med. 2022;19(1):106–15.
Sandoval-Salinas C, Saffon JP, Martínez JM, Corredor HA, Gallego A. Are Radial Pressure Waves Effective for the Treatment of Moderate or Mild to Moderate Erectile Dysfunction? A Randomized Sham Therapy Controlled Clinical Trial. J Sex Med. 2022;19(5):738–44.
Vena W, Vaccalluzzo L, LA Vignera S, Morenghi E, D’Agostino C, Perri A, et al. Low-intensity shockwave treatment (liswt) improves penile rigidity in eugonadal subjects with erectile dysfunction: a pilot study. Minerva Endocrinol. 2021 Dec 21;
Lau W, Shum CF, Lua HCA, Teo CPC. Low-intensity shockwave therapy in the management of erectile dysfunction in Singapore. Ann Acad Med Singapore. 2021;50(8):652–4.
Daneshwar D, Nordin A. Low intensity extracorporeal shockwave therapy for chronic pelvic pain syndrome patients with erectile dysfunction. Medicine (Baltimore). 2022;101(2):e28546.
Ergün M, Akyüz O. Is Li-ESWT effective in diabetic patients with severe erectile dysfunction? Asian J Androl. 2022;24(5):521–4.
Ladegaard PBJ, Mortensen J, Skov-Jeppesen SM, Lund L. Erectile Dysfunction A Prospective Randomized Placebo-Controlled Study Evaluating the Effect of Low-Intensity Extracorporeal Shockwave Therapy (LI-ESWT) in Men With Erectile Dysfunction Following Radical Prostatectomy. Sex Med. 2021;9(3):100338.
Shendy WS, Elsoghier OM, El Semary MM, Ahmed AA, Ali AF, Saber-Khalaf M. Effect of low-intensity extracorporeal shock wave therapy on diabetic erectile dysfunction: Randomised control trial. Andrologia. 2021;53(4):e13997.
Verze P, Capece M, Creta M, La Rocca R, Persico F, Spirito L, et al. Efficacy and safety of low-intensity shockwave therapy plus tadalafil 5 mg once daily in men with type 2 diabetes mellitus and erectile dysfunction: a matched-pair comparison study. Asian J Androl. 2020;22(4):379–82.
Zasieda Y. Combined treatment with focused low-intensity shock-wave therapy and androgen-stimulation therapy in men with corporal veno-occlusive erectile dysfunction on the background of hypogonadotropic hypogonadism. Georgian Med News. 2020;307:49–53.
Yamaçake KGR, Carneiro F, Cury J, Lourenço R, Françolin PC, Piovesan AC, et al. Low-intensity shockwave therapy for erectile dysfunction in kidney transplant recipients. A prospective, randomized, double blinded, sham-controlled study with evaluation by penile Doppler ultrasonography. Int J Impot Res. 2019;31(3):195–203.
Wang CJ, Lu YM, Li CC, Wu WJ, Chien TM. Low-intensity shock wave therapy ameliorates erectile dysfunction in men with pelvic fractures associated with urethral injury. Int J Impot Res. 2019;31(3):218–22.
Ghahhari J, De Nunzio C, Lombardo R, Ferrari R, Gatti L, Ghidini N, et al. Shockwave Therapy for Erectile Dysfunction: Which Gives the Best Results? A Retrospective National, Multi-Institutional Comparative Study of Different Shockwave Technologies. Surg Technol Int. 2022;19(40):213–8.
Oginski N, Apel H, Richterstetter M, Lieb V, Fiebig C, Goebell PJ, et al. Analysis of the Impact of Clinical Factors on Low-Intensity Extracorporeal Shockwave Therapy for Erectile Dysfunction. Urol Int. 2022;10:1–9.
Adeldaeim HM, Abouyoussif T, Gebaly OE, Assem A, Wahab MMA, Rashad H, et al. Prognostic Indicators for Successful Low-intensity Extracorporeal Shock Wave Therapy Treatment of Erectile Dysfunction. Urology. 2021;149:133–9.
Caretta N, De Rocco PM, Minicuci N, De Santis I, Palego P, Garolla A, et al. Efficacy of penile low-intensity shockwave treatment for erectile dysfunction: correlation with the severity of cavernous artery disease. Asian J Androl. 2021;23(5):462–7.
Geyik S. Comparison of the efficacy of low-intensity shock wave therapy and its combination with platelet-rich plasma in patients with erectile dysfunction. Andrologia. 2021;53(10):e14197.
Tzou KY, Hu SW, Bamodu OA, Wang YH, Wu WL, Wu CC. Efficacy of Penile Low-Intensity Shockwave Therapy and Determinants of Treatment Response in Taiwanese Patients with Erectile Dysfunction. Biomedicines. 2021;9(11):1670.
Musa ZS, El-Assmy A, Shokry AM, Shokeir AA, Zween T, Al-Kenawy MR. Long-term effectiveness and predictors of success of low-intensity shockwave therapy in phosphodiesterase type 5 inhibitors non-responders. Arab J Urol. 2020;18(1):54–8.
De Oliveira PS, De Oliveira TR, Nunes Á, Martins F, Lopes T. Low-intensity shock wave therapy for erectile dysfunction and the influence of disease duration. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol. 2019;90(4):276–82.
Vita R, Benvenga S, Giammusso B, La Vignera S. Determinants of Early Response to Low-Intensity Extracorporeal Shockwaves for the Treatment of Vasculogenic Erectile Dysfunction: An Open-Label, Prospective Study. J Clin Med. 2019;8(7):E1017.
Bieri M, Said E, Antonini G, Dickerson D, Tuma J, Bartlett CE, et al. Phase I and registry study of autologous bone marrow concentrate evaluated in PDE5 inhibitor refractory erectile dysfunction. J Transl Med. 2020;18(1):24.
You D, Jang MJ, Song G, Shin HC, Suh N, Kim YM, et al. Safety of autologous bone marrow-derived mesenchymal stem cells in erectile dysfunction: an open-label phase 1 clinical trial. Cytotherapy. 2021;23(10):931–8.
Al Demour S, Jafar H, Adwan S, AlSharif A, Alhawari H, Alrabadi A, et al. Safety and Potential Therapeutic Effect of Two Intracavernous Autologous Bone Marrow Derived Mesenchymal Stem Cells injections in Diabetic Patients with Erectile Dysfunction: An Open Label Phase I Clinical Trial. Urol Int. 2018;101(3):358–65.
Yiou R, Hamidou L, Birebent B, Bitari D, Le Corvoisier P, Contremoulins I, et al. Intracavernous Injections of Bone Marrow Mononucleated Cells for Postradical Prostatectomy Erectile Dysfunction: Final Results of the INSTIN Clinical Trial. Eur Urol Focus. 2017;3(6):643–5.
Koga S, Horiguchi Y. Efficacy of a cultured conditioned medium of exfoliated deciduous dental pulp stem cells in erectile dysfunction patients. J Cell Mol Med. 2022;26(1):195–201.
Mirzaei M, Bagherinasabsarab M, Pakmanesh H, Mohammadi R, Teimourian M, Jahani Y, et al. The Effect of Intracavernosal Injection of Stem Cell in the Treatment of Erectile Dysfunction in Diabetic Patients: A Randomized Single-blinded Clinical Trial. Urol J. 2021;18(6):675–81.
Al Demour S, Adwan S, Jafar H, Rahmeh R, Alhawari H, Awidi A. Safety and Efficacy of 2 Intracavernous Injections of Allogeneic Wharton’s Jelly-Derived Mesenchymal Stem Cells in Diabetic Patients with Erectile Dysfunction: Phase 1/2 Clinical Trial. Urol Int. 2021;105(11–12):935–43.
Protogerou V, Beshari SE, Michalopoulos E, Mallis P, Chrysikos D, Samolis AA, et al. The Combined Use of Stem Cells and Platelet Lysate Plasma for the Treatment of Erectile Dysfunction: A Pilot Study-6 Months Results. Med Basel Switz. 2020;7(3):E14.
Protogerou V, Michalopoulos E, Mallis P, Gontika I, Dimou Z, Liakouras C, et al. Administration of Adipose Derived Mesenchymal Stem Cells and Platelet Lysate in Erectile Dysfunction: A Single Center Pilot Study. Bioeng Basel Switz. 2019;6(1):E21.
Haahr MK, Harken Jensen C, Toyserkani NM, Andersen DC, Damkier P, Sørensen JA, et al. A 12-Month Follow-up After a Single Intracavernous Injection of Autologous Adipose-Derived Regenerative Cells in Patients with Erectile Dysfunction Following Radical Prostatectomy: An Open-Label Phase I Clinical Trial. Urology. 2018;121:203.e6-203.e13.
von Schwarz ER, Busse N, Angelus KM, Omair A, von Schwarz AA, Bogaardt PC. Intracavernous injection of stem cell-derived bioactive molecules for erectile dysfunction—a pilot phase non-randomized controlled trial. JOMH. 2021;17(4):99–108.
Derosa G, D’Angelo A, Preti PS, Maffioli P. Evaluation of the Effect on Sexual Performance of a Nutraceutical Combination Containing Alpha Lipoic Acid, Vitis vinifera L. and Ginkgo biloba, Compared to Placebo, Avanafil or a Combination of Nutraceutical Plus Avanafil in Males With Type 2 Diabetes Mellitus With Erectile Dysfunction. Front Endocrinol. 2022;13:847240.
Mirone V, Napolitano L, D’Emmanuele di Villa Bianca R, Mitidieri E, Sorrentino R, Vanelli A, et al. A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol. 2021;93(2):221–6.
Shirai M, Miyoshi Y, Ogasa T, Miyoshi M, Ishikawa K, Hiramatsu I, et al. Oral Testofen, L-Citrulline, Resveratrol, and Caffeine Supplement Drink Improves Sexual Function in Men with Phosphodiesterase 5 Inhibitors: Randomized, Double-Blind, Placebo-Controlled Crossover Pilot Study. World J Mens Health. 2021;39(4):733–9.
Shirai M, Hiramatsu I, Aoki Y, Shimoyama H, Mizuno T, Nozaki T, et al. Oral L-citrulline and Transresveratrol Supplementation Improves Erectile Function in Men With Phosphodiesterase 5 Inhibitors: A Randomized, Double-Blind. Placebo-Controlled Crossover Pilot Study Sex Med. 2018;6(4):291–6.
Shankhwar SN, Mahdi AA, Sharma AV, Pv K. A Prospective Clinical Study of a Prosexual Nutrient: Nano Leo for Evaluation of Libido, Erection, and Orgasm in Indian Men with Erectile Dysfunction. Evid-Based Complement. Altern Med ECAM. 2020;2020:4598217.
Park NC, Kim SW, Hwang SY, Park HJ. Efficacy and safety of an herbal formula (KBMSI-2) in the treatment of erectile dysfunction: A preliminary clinical study. Investig Clin Urol. 2019;60(4):275–84.
Elshahid ARM, Shahein IM, Mohammed YF, Ismail NF, Zakarria HBAER, GamalEl Din SF. Folic acid supplementation improves erectile function in patients with idiopathic vasculogenic erectile dysfunction by lowering peripheral and penile homocysteine plasma levels: a case-control study. Andrology. 2020;8(1):148–53.
Stein RA, Schmid K, Bolivar J, Swick AG, Joyal SV, Hirsh SP. Kaempferia parviflora ethanol extract improves self-assessed sexual health in men: a pilot study. J Integr Med. 2018;16(4):249–54.
Nguyen S, Rajfer J, Shaheen M. Safety and efficacy of daily Revactin® in men with erectile dysfunction: a 3-month pilot study. Transl Androl Urol. 2018;7(2):266–73.
Quarto G, Cola A, Perdonà S. Efficacy of a formulation containing Serenoa repens, Crocus sativus and Pinus massoniana extracts in men with concomitant LUTS and erectile dysfunction. Minerva Urol E Nefrol Ital J Urol Nephrol. 2017;69(3):300–6.
Sharma T, Ramamurthy A, Nathani S, Anand P. A comparative clinical study of black and white seeds of Kapikacchu with special reference to Vrishya Karma. Int J Res Ayurveda Pharm. 2017;8:121–6.
Lin C, Pattraraachachai J, Pawa KK, Wongyai S. A preliminary study of the efficacy of the polyherbal preparation Sao Thong Tai for erectile dysfunction among elderly men: a double-blind, randomized controlled trial. Clin Phytoscience. 2022;8(1):9.
Hussain MA, Alam MN, Ahmed N, Said H, Afrin SF, Hassan Z, et al. Investigation of efficacy of an herbal product (Habb-E-Munish) in the treatment of ED Using IIEF-5 scores and its effect on liver and renal functions. Bangladesh J Med Sci. 2019;19(1):176–9.
Tadayon Najafabadi B, Jafarinia M, Ghamari K, Shokraee K, Tadayyon F, Akhondzadeh S. Vitamin E and ginseng combined supplement for treatment of male erectile dysfunction: A double-blind, placebo-controlled, randomized, clinical trial. Adv Integr Med. 2021;8(1):44–9.
Farnia V, Tatari F, Alikhani M, Shakeri J, Taghizadeh M, Karbasizadeh H, et al. Rosa Damascena oil improved sexual function and testosterone in male patients with opium use disorder under methadone maintenance therapy-results from a double-blind, randomized, placebo-controlled clinical trial. Drug Alcohol Depend. 2017;1(176):117–25.
Kulkarni O, Agarwal A, Khare P, Ganu G. Randomized, double blind, placebo controlled clinical study to assess efficacy and safety of nrl/mw/201901 in subjects suffering from erectile dysfunction. Int J Res Pharm Sci. 2020;11(3):2790–801.
Najafabadi BT, Farsinejad M, Shokraee K, Momtazmanesh S, Violette PD, Esalatmanesh S, et al. Possible effects of Saffron (Crocus sativus) in the treatment of erectile dysfunction: A randomized, double-blind, placebo-controlled trial. J Herb Med. 2022;1(32): 100551.
Trebaticky B, Muchova J, Ziaran S, Bujdak P, Breza J, Durackova Z. Natural polyphenols improve erectile function and lipid profile in patients suffering from erectile dysfunction. Bratisl Lek Listy. 2019;120(12):941–4.
Gallo L, Pecoraro S, Sarnacchiaro P, Silvani M, Antonini G. The Daily Therapy With L-Arginine 2,500 mg and Tadalafil 5 mg in Combination and in Monotherapy for the Treatment of Erectile Dysfunction: A Prospective. Randomized Multicentre Study Sex Med. 2020;8(2):178–85.
Abu El-Hamd M, Hegazy EM. Comparison of the clinical efficacy of daily use of L-arginine, tadalafil and combined L-arginine with tadalafil in the treatment of elderly patients with erectile dysfunction. Andrologia. 2020;52(7):e13640.
Menafra D, de Angelis C, Garifalos F, Mazzella M, Galdiero G, Piscopo M, et al. Long-term high-dose L-arginine supplementation in patients with vasculogenic erectile dysfunction: a multicentre, double-blind, randomized, placebo-controlled clinical trial. J Endocrinol Invest. 2022;45(5):941–61.
GamalEl Din SF, Abdel Salam MA, Mohamed MS, Ahmed AR, Motawaa AT, Saadeldin OA, et al. Tribulus terrestris versus placebo in the treatment of erectile dysfunction and lower urinary tract symptoms in patients with late-onset hypogonadism: A placebo-controlled study. Urologia. 2019;86(2):74–8.
Kamenov Z, Fileva S, Kalinov K, Jannini EA. Evaluation of the efficacy and safety of Tribulus terrestris in male sexual dysfunction-A prospective, randomized, double-blind, placebo-controlled clinical trial. Maturitas. 2017;99:20–6.
Demirci A, Çakan M, Topçuoğlu M. Whether Adding Vitamin D to Tadalafil 5 mg Treatment Is Useful in Patients with Erectile Dysfunction and Vitamin D Deficiency? Urol Int. 2021;105(5–6):514–9.
Ali DA, Ranjan DP, Priyadarshi DS, Pandey DR. Evaluation Of Safety And Efficacy Of Vitamin D Supplementation Inerectile Dysfunction Patients With Vitamin D Deficiency. Clin Med. 2021;08(04):6.
Zaghloul AS, El-Nashaar AM, Said SZ, Osman IA, Mostafa T. Assessment of the intracavernosal injection platelet-rich plasma in addition to daily oral tadalafil intake in diabetic patients with erectile dysfunction non-responding to on-demand oral PDE5 inhibitors. Andrologia. 2022;54(6):e14421.
Wong SM, Chiang BJ, Chen HC, Wu YN, Lin YH, Liao CH. A short term follow up for intracavernosal injection of platelet rich plasma for the treatment of erectile dysfunction [Internet]. Vol. 32, Urological Science. 2021. p. 171–6. Available from: https://www.e-urol-sci.com/article.asp?issn=1879-5226;year=2021;volume=32;issue=4;spage=171;epage=176;aulast=Wong
Taş T, Çakıroğlu B, Arda E, Onuk Ö, Nuhoğlu B. Early Clinical Results of the Tolerability, Safety, and Efficacy of Autologous Platelet-Rich Plasma Administration in Erectile Dysfunction. Sex Med. 2021;9(2):100313.
• Poulios E, Mykoniatis I, Pyrgidis N, Zilotis F, Kapoteli P, Kotsiris D, et al. Platelet-Rich Plasma (PRP) Improves Erectile Function: A Double-Blind, Randomized, Placebo-Controlled Clinical Trial. J Sex Med. 2021;18(5):926–35. It is the only paper on PRP therapy that is a randomized clinical trial. It also presents the largest number of patients and the one of the longest follow-up time.
Zaghloul AS, Mahmoud ElNashar AER, GamalEl Din SF, Zaki Said S, Saad HM, Refaat Eldebs H, et al. Smoking status and the baseline international index of erectile function score can predict satisfactory response to platelet-rich plasma in patients with erectile dysfunction: A prospective pilot study. Andrologia. 2021;53(9):e14162.
Matz EL, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59(1):61–5.
Cirino G, Sorrentino R, di Villa Bianca R d’Emmanuele, Popolo A, Palmieri A, Imbimbo C, et al. Involvement of beta 3-adrenergic receptor activation via cyclic GMP- but not NO-dependent mechanisms in human corpus cavernosum function. Proc Natl Acad Sci U S A. 2003;100(9):5531–6.
Karakus S, Musicki B, Burnett AL. Mirabegron improves erectile function in men with overactive bladder and erectile dysfunction: a 12-week pilot study. Int J Impot Res. 2021 Jul 2;
Elbaz R, El-Assmy A, Zahran MH, Hashem A, Shokeir AA. Mirabegron for treatment of erectile dysfunction concomitant with lower urinary tract symptoms in patients with benign prostatic obstruction: A randomized controlled trial. Int J Urol Off J Jpn Urol Assoc. 2022;29(5):390–6.
Bayraktar Z, Albayrak S. Antiplatelet (aspirin) therapy as a new option in the treatment of vasculogenic erectile dysfunction: a prospective randomized double-blind placebo-controlled study. Int Urol Nephrol. 2018;50(3):411–8.
Bayraktar Z, Albayrak S. Efficacy and safety of combination of tadalafil and aspirin versus tadalafil or aspirin alone in patients with vascular erectile dysfunction: a comparative randomized prospective study. Int Urol Nephrol. 2019;51(9):1491–9.
Ghoreishi A, Dashtaki L, Hajisalimi B. Bupropion as a Treatment for Sexual Dysfunction Among Chronic Kidney Disease Patients. Acta Med Iran [Internet]. 2019 Sep 30 [cited 2022 Aug 29];57(5). Available from: https://acta.tums.ac.ir/index.php/acta/article/view/7649
Yee A, Loh HS, Ong TA, Ng CG, Sulaiman AH. Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Trial of Bupropion as Treatment for Methadone-Emergent Sexual Dysfunction in Men. Am J Mens Health. 2018;12(5):1705–18.
Mohammad EJ, Jaffal WN, Abbas KM. The Efficacy of Using Cabergoline in Psychogenic Erectile Dysfunction Treatment (A Local Study) -. Syst Rev Pharm. 2020;11(3):702–4.
Cannarella R, Calogero AE, Aversa A, Condorelli RA, La Vignera S. Is There a Role for Levo-Thyroxine for the Treatment of Arterial Erectile Dysfunction? The Clinical Relevance of the Mean Platelet Volume. J Clin Med. 2020;9(3):E742.
Foy CG, Newman JC, Russell GB, Berlowitz DR, Bates JT, Burgner AM, et al. Effect of Intensive vs Standard Blood Pressure Treatment Upon Erectile Function in Hypertensive Men: Findings From the Systolic Blood Pressure Intervention Trial. J Sex Med. 2020;17(2):238–48.
Giuliano F, Denys P, Joussain C. Effectiveness and Safety of Intracavernosal IncobotulinumtoxinA (Xeomin®) 100 U as an Add-on Therapy to Standard Pharmacological Treatment for Difficult-to-Treat Erectile Dysfunction: A Case Series. Toxins. 2022;14(4):286.
Giuliano F, Joussain C, Denys P. Long Term Effectiveness and Safety of Intracavernosal Botulinum Toxin A as an Add-on Therapy to Phosphosdiesterase Type 5 Inhibitors or Prostaglandin E1 Injections for Erectile Dysfunction. J Sex Med. 2022;19(1):83–9.
Moradi S, Khazaeli D, Dadfar M, Bakhtiari N. Efficacy of Intracavernosal Injections of 50-Unit Versus 100-Unit Doses of AbobotulinumtoxinA (Masport®) in Vasculogenic Erectile Dysfunction with Phosphodiesterase Type 5 Inhibitors Resistant. Nephro-Urol Mon. 2022;14(1):e119131.
Abdelrahman IFS, Raheem AA, Elkhiat Y, Aburahma AA, Abdel-Raheem T, Ghanem H. Safety and efficacy of botulinum neurotoxin in the treatment of erectile dysfunction refractory to phosphodiesterase inhibitors: Results of a randomized controlled trial. Andrology. 2022;10(2):254–61.
• El-Shaer W, Ghanem H, Diab T, Abo-Taleb A, Kandeel W. Intra-cavernous injection of BOTOX® (50 and 100 Units) for treatment of vasculogenic erectile dysfunction: Randomized controlled trial. Andrology. 2021;9(4):1166–75. It is the randomized clinical trial for the treatment of ED with botulinum toxin injections with the largest number of patients with a great difference compared to the rest. In addition to comparing treatment with placebo, it also has the longest follow-up time.
Giuliano F, Joussain C, Denys P. Safety and Efficacy of Intracavernosal Injections of AbobotulinumtoxinA (Dysport®) as Add on Therapy to Phosphosdiesterase Type 5 Inhibitors or Prostaglandin E1 for Erectile Dysfunction-Case Studies. Toxins. 2019;11(5):E283.
Taşkapu HH, Sönmez MG, Kılınç MT, Altınkaya N, Aydın A, Balasar M. Efficiency of intracavernosal alprostadil and oral clomiphene citrate combination treatment in penile vasculogenic erectile dysfunction patients accompanied by late-onset hypogonadism. Andrologia. 2020;52(10): e13759.
Bernie HL, Segal R, Le B, Burnett A, Bivalacqua TJ. An Empirical vs Risk-Based Approach Algorithm to Intracavernosal Injection Therapy: A Prospective Study. Sex Med. 2017;5(1):e31–6.
Bearelly P, Phillips EA, Pan S, O’Brien K, Asher K, Martinez D, et al. Long-term intracavernosal injection therapy: treatment efficacy and patient satisfaction. Int J Impot Res. 2020;32(3):345–51.
Apergis N, Gounidis A, Filippou DK, Papadopoulos VP. The Use of CPAP Independently Improves Nocturia, Erectile Function, and Depression Symptoms in Obstructive Sleep Apnea Male Patients: an Observational Study. SN Compr Clin Med. 2021;3(7):1575–85.
Coban S, Gunes A, Gul A, Turkoglu AR, Guzelsoy M, Ozturk M, et al. Can continuous positive airway pressure improve lower urinary tract symptoms and erectile dysfunction in male patients with severe obstructive sleep apnea syndrome? Investig Clin Urol. 2020;61(6):607–12.
Sen V, Sahin MO, Irer B, Koc E, Yildiz G. The impact of hyperbaric oxygen therapy on erectile functions and serum testosterone levels in patients with erectile dysfunction. Aging Male Off J Int Soc Study Aging Male. 2020;23(1):66–70.
Schulz R, Bischof F, Galetke W, Gall H, Heitmann J, Hetzenecker A, et al. CPAP therapy improves erectile function in patients with severe obstructive sleep apnea. Sleep Med. 2019;53:189–94.
Pascual M, de Batlle J, Barbé F, Castro-Grattoni AL, Auguet JM, Pascual L, et al. Erectile dysfunction in obstructive sleep apnea patients: A randomized trial on the effects of Continuous Positive Airway Pressure (CPAP). PLoS ONE. 2018;13(8):e0201930.
Melehan KL, Hoyos CM, Hamilton GS, Wong KK, Yee BJ, McLachlan RI, et al. Randomized Trial of CPAP and Vardenafil on Erectile and Arterial Function in Men With Obstructive Sleep Apnea and Erectile Dysfunction. J Clin Endocrinol Metab. 2018;103(4):1601–11.
Sahin MO, Sen V, Eser E, Koc E, Gumus U, Karakuzu C, et al. The Effect of Hyperbaric Oxygen Therapy on Erectile Functions: A Prospective Clinical Study. Urol Int. 2018;101(2):206–11.
Hadanny A, Lang E, Copel L, Meir O, Bechor Y, Fishlev G, et al. Hyperbaric oxygen can induce angiogenesis and recover erectile function. Int J Impot Res. 2018;30(6):292–9.
Rislanu A, Auwal H, Musa D, Auwal A. Comparative Effectiveness of Electrical Stimulation and Aerobic Exercise in the Management of Erectile Dysfunction: A Randomized Clinical Trial. Ethiop J Health Sci. 2020;30(6):961–70.
Carboni C, Fornari A, Bragante KC, Averbeck MA, Vianna da Rosa P, Mea Plentz RD. An initial study on the effect of functional electrical stimulation in erectile dysfunction: a randomized controlled trial. Int J Impot Res. 2018;30(3):97–101.
Cui W, Li H, Guan R, Li M, Yang B, Xu Z, et al. Efficacy and safety of novel low-intensity pulsed ultrasound (LIPUS) in treating mild to moderate erectile dysfunction: a multicenter, randomized, double-blind, sham-controlled clinical study. Transl Androl Urol. 2019;8(4):307–19.
Juho YC, Tang SH, Lin YH, Lin CX, Liang T, Cherng JH, et al. Germanium-Titanium-π Polymer Composites as Functional Textiles for Clinical Strategy to Evaluate Blood Circulation Improvement and Sexual Satisfaction. Polymers. 2021;13(23):4154.
Srivatsav A, Balasubramanian A, Pathak UI, Rivera-Mirabal J, Thirumavalavan N, Hotaling JM, et al. Efficacy and Safety of Common Ingredients in Aphrodisiacs Used for Erectile Dysfunction: A Review. Sex Med Rev. 2020;8(3):431–42.
Leisegang K, Finelli R. Alternative medicine and herbal remedies in the treatment of erectile dysfunction: A systematic review. Arab J Urol. 2021;19(3):323–39.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have existing conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors were performed in accordance with all applicable ethical standards including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Men’s Health
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alonso-Isa, M., García-Gómez, B., González-Ginel, I. et al. Conservative Non-surgical Options for Erectile Dysfunction. Curr Urol Rep 24, 75–104 (2023). https://doi.org/10.1007/s11934-022-01137-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-022-01137-2