Abstract
Background/Objectives:
Since 2007, our institution has used validated guidelines for the insertion of proactive gastrostomy feeding tubes in patients with head and neck cancer. Helical intensity-modulated radiotherapy (H-IMRT) delivered by Tomotherapy, is an advanced radiotherapy technique introduced at our centre in 2010. This form of therapy reduces long-term treatment-related toxicity to normal tissues. The aim of this study is to compare weight change and need for tube feeding following H-IMRT (n=53) with patients that would have previously been treated with three-dimensional conformal radiotherapy (n=134).
Subjects/Methods:
Patients with head and neck cancer assessed as high nutritional risk with recommendation for proactive gastrostomy were identified from cohorts from 2007 to 2008 and 2010 to 2011. Retrospective data were collected on clinical factors, weight change from baseline to completion of treatment, incidence of severe weight loss (⩾10%) and tube feeding. Statistical analyses to compare outcomes between the two treatments included χ2-test, Fisher’s exact and two-sample Wilcoxon tests (P<0.05).
Results:
The H-IMRT cohort had higher proportions of patients with definitive chemoradiotherapy (P=0.032) and more advanced N stage (P<0.001). Nutrition outcomes were not significantly different between H-IMRT and conformal radiotherapy, respectively: need for proactive gastrostomy (n=49, 92% versus n=115, 86%, P=0.213), median percentage weight change (−7.2% versus −7.3%, P=0.573) and severe weight loss incidence (28% versus 27%, P=0.843).
Conclusions:
Both groups had median weight loss >5% and high incidences of tube feeding and severe weight loss. Nutrition intervention remains critical in this patient population, despite advances in radiotherapy techniques, and no changes to current management are recommended.
Similar content being viewed by others
Introduction
Patients with mucosal squamous cell carcinoma cancer of the head and neck have a high incidence of malnutrition and frequently require enteral tube feeding. Since 2007, our institution has used validated local hospital guidelines: the RBWH Swallowing and Nutrition Management Guidelines for Patients with Head and Neck Cancer (S&N Guidelines), for a proactive approach to the insertion of enteral feeding tubes.1 Implementation of the S&N Guidelines has reduced unplanned hospital admissions and length of stay,2 and adherence to the S&N Guidelines has improved nutrition outcomes.3 There is no international consensus for the optimal method of tube feeding4 and centres have adapted either a proactive or reactive approach. The majority of studies supporting prophylactic gastrostomy insertion have been undertaken in patients receiving treatment with conformal radiotherapy or radiotherapy alone.5, 6, 7 As radiotherapy techniques and treatment regimens evolve, nutrition support recommendations also require ongoing review.
Intensity-modulated radiotherapy (IMRT) is a targeted form of radiotherapy. When compared with three-dimensional (3D) conformal radiotherapy, IMRT allows better preservation of organs and tissues in close proximity to the cancer being treated (for example, parotid glands), and so reduces late side effects such as xerostomia and thereby improves quality of life.8 Although, some authors have postulated this may lead to a reduced need for a gastrostomy,9 there are studies that continue to support the role of a prophylactic gastrostomy with IMRT, in particular with concurrent treatment.10 There have been concerns that prophylactic gastrostomy insertion increases the risk of gastrostomy dependency, with longer duration of tube usage and increased dysphagia post treatment,11, 12, 13 although some studies with IMRT have not found this to be of concern.14, 15, 16
Since 2010, the majority of patients with squamous cell carcinoma of the head and neck in our centre have been treated with helical-IMRT (H-IMRT) using Tomotherapy (TomoTherapy Inc., Madison, WI, USA). Several studies have suggested H-IMRT can achieve superior dose sparing to organs at risk versus other forms of IMRT.17, 18, 19, 20 This has strengthened the hypothesis that intensive nutrition support with a feeding tube may no longer be warranted. However, the extent of nutrition outcomes and requirement for tube feeding following H-IMRT has not been widely reported. Therefore, the aim of this study was to investigate weight change and the requirement for tube feeding in a cohort of high-risk patients receiving H-IMRT compared with a high-risk cohort receiving standard conformal radiotherapy to see whether any change to nutrition management is warranted.
Subjects and methods
Study population
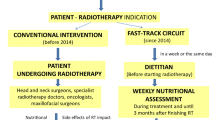
Patients attending the multidisciplinary Combined Head and Neck Clinic for cancer treatment over two time periods at a large metropolitan tertiary referral hospital were screened for inclusion in the study. The first cohort (January 2007 to December 2008) was treated with 3D conformal radiotherapy and the second cohort (July 2010 to June 2011) received either 3D conformal radiotherapy or H-IMRT. Patients were excluded if they had the following: benign disease, a non-head and neck tumour, palliative intent treatment, refused treatment, treatment at another hospital, incomplete/missing data or no access to the medical chart. The remaining eligible patients were classified as high risk or non-high risk according to the S&N Guidelines (see Figure 1). For the purposes of this study, only high-risk patients receiving definitive or adjuvant radiotherapy as part of their treatment were included, to provide a final comparative sample of patients who received either H-IMRT or 3D conformal radiotherapy (see Figure 2).
Royal Brisbane and Women’s Hospital Swallowing and nutrition management guidelines for patients with head and neck cancer—revised version 2010.43 These guidelines have minor alterations to the high-risk definition compared with the original version used from 2007 to 2009. They previously included the diagnosis of dysphagia at baseline. This has now been removed and unknown primary tumours added.
Nutrition intervention
High-risk patients were recommended for gastrostomy placement before treatment (proactive gastrostomy tube placement). This guideline recommendation encompasses those who would benefit from immediate nutrition support, owing to poor nutritional status or significant dysphagia at diagnosis (a therapeutic gastrostomy), as well as those who would benefit from future nutrition support, owing to predicted treatment side effects (a prophylactic gastrostomy). All other patients who may require tube feeding during treatment have either a nasogastric or gastrostomy tube placed depending on predicted duration of need (reactive tube placement).
All patients were screened at baseline by the dietitian using the validated Malnutrition Screening Tool.21 Patients who were identified at risk of malnutrition (score 2–5) were provided with dietary advice or referred to their local dietitian service pre-treatment. Patients were referred routinely to the surgical dietitian and/or radiotherapy dietitian, respectively, according to their treatment plan. Outpatients were seen on a weekly basis during treatment and inpatients were seen daily to weekly as clinically indicated as part of standard care.
Weight was recorded at diagnosis and at the end of radiotherapy treatment and percentage weight change calculated. Nutrition requirements were calculated by the dietitian using the ratio method.22 Energy requirements (125 kJ/kg/day, 30 kcal/kg/day) and protein requirements (1.2 g/kg/day) were based on actual body weight, unless the patient was overweight (body mass index >25 kg/m2), and then adjusted body weight was used. Adjusted body weight was calculated using the following equation (ideal body weight (IBW) + ((actual body weight−IBW) × 25%)), whereby (IBW) was the weight at body mass index 25 kg/m2. At each dietetic review, weight was monitored, and energy and protein intakes were estimated using a 24-h recall method. The dietitian estimated actual intake against standard portion sizes and revised nutrition requirements and prescriptions as clinically indicated.
Initiation of tube feeding for all patients was recommended if oral intake fell to <60% of estimated energy requirements and was not anticipated to improve in the next 10 days. Patients continued on tube feeding until they were able to establish a minimum of 60% of their nutrition requirements orally and maintain their weight. All patients were referred to their local dietitian service on completion of treatment.
Study design and data collection
This was a retrospective comparative cohort study. Data collection was via retrospective chart audit and the use of existing clinical databases in the patient administration systems of the hospital. Independent variables included the following: gender, age, clinical factors (tumour site, tumour stage and treatment) and adherence to the S&N Guidelines’ recommendations for proactive gastrostomy insertion. Dependent variables included the following: percentage weight change from diagnosis to the end of radiotherapy treatment, the incidence and use of proactively placed gastrostomy tubes and the incidence, type and duration of use of reactive feeding tubes.
Outcomes
Percentage weight change was chosen as the primary nutrition outcome for this study, as it has been widely used and accepted in the literature. Unintentional weight loss of ⩾10% within the previous 6 months signifies a substantial nutritional deficit.23 It has been associated with moderate-to-severe malnutrition and therefore is considered a simple valuable measure to use for this purpose.24 Significant weight loss has also been shown to negatively impact on patient and clinical outcomes, such as quality of life25 and survival,26, 27 and thus is a clinically significant measure readily available from retrospective data collection.
The nutrition outcome data were used to retrospectively determine the validity of the S&N Guideline recommendation for proactive gastrostomy. For each patient, the outcome of whether they were deemed to ‘need or not need a proactive gastrostomy’ was calculated. A patient was deemed to truly ‘need a proactive gastrostomy’ if the following clinical outcomes occurred:
-
Patient had a proactive gastrostomy placed as per the S&N Guidelines and it was used for nutrition support
-
Patient had a reactive feeding tube placed and it was used for >4 weeks
-
Patient had an unused proactive gastrostomy or a reactive feeding tube for <4 weeks, or no feeding tube, and lost ⩾10% body weight
These outcome definitions are described fully elsewhere when they were used to originally validate the S&N Guidelines1 and are deemed to confirm the prediction that the patient required a proactive gastrostomy as per the S&N Guidelines.
Statistical analysis
Based on the sample size from the two cohorts, there was an approximate ratio of 1:2.5 patients in each treatment group. In a previous study, the response within each group had an s.d. of 5. If the true difference in the treatment groups’ mean weight loss is 2.3%, we will be able to reject the null hypothesis that the population means treatment groups are equal with probability (power) 0.804. The type I error probability associated with this test of this null hypothesis is 0.05.
Statistical analysis was performed to determine any baseline between the treatment groups. Categorical variables were collapsed when necessary for the χ2-test as per details in Table 1. Continuous variables were assessed for normal distribution using the Shapiro–Wilk test and non-parametric tests were used when the data were not normally distributed. To compare outcomes, the two-sample Wilcoxon test was used for continuous variables and the χ2-test or Fisher’s exact test for the categorical variables. Statistical significance was set at P<0.05 for all analyses. Data were analysed using R Commander Version 1.8-3 and R version 2.14.2 (2012-02-29) (Available from R Foundation for Statistical Computing, Vienna, Austria).
Ethics
The study was deemed a quality improvement study and exempt from full ethical review by the Human Research Ethical Committee at the hospital. Patients received standard nutritional care during their treatment and were not subject to any experimental intervention. All data used is routinely collected for ongoing quality assurance and available in the patient administration systems of the hospital.
Results
Sample population
There were 187 high-risk patients eligible for the study after applying inclusion and exclusion criteria (see Figure 2). Reasons for high-risk rating were as follows: oral cavity cancer and bilateral chemoradiotherapy (n=42), oropharyngeal cancer and bilateral chemoradiotherapy (n=108), nasopharyngeal cancer and chemoradiotherapy (n=6), hypopharyngeal cancer and chemoradiotherapy (n=13), unknown primary and chemoradiotherapy (n=6), severe malnutrition at presentation (n=12) and severe dysphagia at presentation (n=0).
Of those presenting with severe malnutrition (defined as either unintentional weight loss >10% in 6 months, body mass index <20 kg/m2 with unintentional weight loss 5%–10% in 6 months, or Subjective Global Assessment C), four patients had post-operative radiotherapy for oral cavity (n=1) or laryngeal (n=3) tumours; five patients had radiotherapy for oropharyngeal (n=3), hypopharyngeal (n=1) or laryngeal (n=1) tumours; and the remaining three patients had chemoradiotherapy for a laryngeal tumour.
High-risk patients who received H-IMRT (n=53) were compared with high-risk patients who received 3D conformal radiotherapy (n=134) (see Table 1). None of the patients had metastatic disease and all received curative intent treatment. Although there were no statistically significant differences for age, gender, site or T stage, the H-IMRT cohort had more advanced nodal disease (N2 or N3 stage), 85% versus 57% (P<0.001), as well as a higher proportion treated with definitive chemoradiotherapy, 94% versus 78% (P=0.017).
S&N Guideline adherence and method of tube feeding
Overall, adherence with the S&N Guidelines’ high-risk category recommendations was high with 157/187 patients (84%) receiving a proactive gastrostomy. Two patients in the H-IMRT group had a reactive tube placed versus 14 patients in the 3D conformal group. The overall method of tube feeding was not different between the two groups (P=0.172) (Table 2).
Nutrition outcomes: weight
The mean weight at baseline was not significantly different between the two groups (P=0.272). There were no significant differences between the two types of treatment with regards to the outcome of weight change from diagnosis to the end of radiotherapy treatment (Table 2). Median percentage weight change was −7.2% (range: −19.1, 8.5) in the H-IMRT group versus −7.3% (range: −20.1, 22.9) in the conformal group (P=0.573). Incidence of severe weight loss (⩾10%) was 28% in the H-IMRT group versus 27% in the conformal group (P=0.843).
Nutrition outcomes: ‘needed a proactive gastrostomy’
Both groups had a high proportion of patients who met the criteria for ‘needed a proactive gastrostomy’ based on their actual clinical outcomes, with 92% in the H-IMRT group (n=49) versus 86% in the 3D group (n=115; P=0.213) (Table 2). There were 9 unused proactive tubes overall, of which 3 patients had severe weight loss (⩾10%) and 14 patients who did not receive any form of tube feeding; however, 9 of these also had severe weight loss (⩾10%) (Table 3).
Discussion
The results from this study demonstrate that despite advances in radiotherapy techniques, which reduce long-term toxicity and side effects,8 this has not translated into improved early nutritional outcomes. We have found no statistical difference in the mean weight loss during treatment and in the need for tube feeding, with a large proportion of patients still meeting the criteria for proactive gastrostomy placement. Although acknowledging there were differences in clinical characteristics between the two groups (higher rates of advanced N stage disease and more patients receiving definitive chemoradiotherapy in the H-IMRT group), which could possibly be attributed to the increasing incidence of human papillomavirus-related oropharyngeal cancers,28 ultimately there was still a high incidence of weight loss and requirement for tube feeding in both groups.
Research relating to impact of H-IMRT on nutrition outcomes and tube feeding requirements is sparse,29 although there are some studies reporting on outcomes following linear accelerator-based IMRT.30, 31, 32 The current evidence indicates that weight loss is a recurring problem, despite advancing radiotherapy techniques, which supports the ongoing essential need for nutrition intervention. Maintaining and improving nutritional status has been shown to improve quality of life25, 33 and other clinical outcomes.34
Capelle et al.35 reported a median loss of 6% of pre-radiotherapy weight (with a maximum weight loss of 13.6%) in a small case series (n=20) of patients receiving definitive or adjuvant chemoradiotherapy.35 You et al.36 reported 23% of their patients (7/31) lost >5% of their body weight and these weight changes and anatomical contour changes impacted on severity of side effects such as xerostomia.36 Duma et al.37 were investigating the dosimetric effect of adaptive radiotherapy and they reported re-planning usually occurred by the end of the third week of treatment, at which point there was a median weight loss of 2.3 kg (range 0 to −10.7 kg); however, the overall weight change was not reported.37 There is even less data in the literature on the usage of feeding tubes with H-IMRT. In one small study (n=5), all patients had a proactive gastrostomy tube placed; however, nutritional outcomes or tube use were not reported.38 Another small study (n=17) reported that no patients in their case series received a gastrostomy (although the use of nasogastric tubes was not reported); however, 29% (n=5) had severe weight loss ⩾10%.39
Multidisciplinary team adherence to the S&N Guideline recommendations for high-risk patients improved over time, with adherence of 80% (2007–2008) increasing to 89% (2010–2011). Despite a high rate of tube feeding and therefore nutrition intervention in this patient group, the weight loss outcomes remain sub-optimal. Both groups had median weight loss ⩾5% and a high incidence of severe weight loss (⩾10%), which is consistent with the literature.35, 39, 40 Further research is required to investigate why patients continue to lose significant weight, despite intensive nutrition interventions, and investigate strategies to overcome this weight loss.41 The aetiology of patients’ weight loss is likely multi-factorial and not simply related to the radiotherapy dosimetry. Patients receiving concurrent chemoradiotherapy often experience additional chemotherapy-induced side effects such as nausea, vomiting, taste changes, loss of appetite and fatigue. Silander et al.40 demonstrated patients were not able to meet their recommended energy and protein intakes despite prophylactic gastrostomy, hypothesising treatment side effects as the main barrier.40 Patient adherence to recommendations is also an important consideration, as we have shown in this study that despite proactive gastrostomy insertion, there were three patients that chose not to use their tube when it was recommended to do so, resulting in clinically significant weight loss. Capuano et al.34 reported 47% of patients were deemed non-adherent—either not accepting nutritional counselling or refusing nasogastric or gastrostomy tubes during treatment, and this had a significant impact on their outcomes.34 Further research to develop our understanding of factors that have an impact on weight loss and adherence is required to enable the development of effective strategies to ultimately improve nutrition outcomes.
A retrospective study design results in limitations such as patient exclusions, owing to difficulties accessing charts and missing data. It also limits the ability to measure other clinical outcomes that are not part of routine practice, such as quality of life, blood results, body composition and toxicity profiles. Although reduced late toxicity has been demonstrated with IMRT,8 the research with H-IMRT remains limited with studies only reporting the reduction in doses to organs at risk compared with IMRT17, 18, 19, 20 A prospective observational study is currently in progress to determine acute and late toxicity profiles following H-IMRT and will be reported on separately. The duration of gastrostomy use should be more carefully considered in future studies. If duration of gastrostomy use is <4 weeks, a nasogastric tube may be more appropriate42 as long as there is no compromise to the ultimate nutrition outcome and degree of weight loss. Although the high-risk definition for the S&N Guidelines actually changed slightly over the period of data collection for the two cohorts,43 this had a negligible impact on results, owing to small numbers in the categories affected by change, (no patients classified as high risk owing to dysphagia alone and only six patients with an unknown primary treated with chemoradiotherapy). Additional outcome measures such as nutritional status using validated tools44 or a combination of standardised characteristics to diagnose malnutrition45 would have been useful to include in this study; however, the details required for these types of assessment were usually only routinely recorded at baseline. Therefore, percentage weight loss was used as the primary nutrition outcome, as this was a convenient measure available through retrospective chart audit. Given ⩾10% weight loss has been shown to have an impact on patient and clinical outcomes,25, 26, 27 this was considered a suitable nutrition outcome measure for this study design.
The strength of this study is that it is the largest cohort to date with adequate statistical power to report on nutrition outcomes following H-IMRT. We were fortunate to be able to compare patients receiving the two types of treatment over a similar period of time at one centre with no other contemporaneous changes in practice at our institution that may have confounded these results. Concurrent comparative cohort studies will become increasingly difficult to perform, as centres migrate to the use of advanced techniques as their new standard of care. Our study also benefits from minimal selection bias with the use of validated guidelines to clearly identify high-risk patients for proactive tube feeding, with a high rate of adherence by the multi disciplinary team.
In conclusion, although H-IMRT has been shown to deliver reduced doses to normal tissue, there are no significant differences in incidence of tube feeding or weight loss during treatment when compared with conformal 3D radiotherapy techniques. Therefore, the placement of a proactive gastrostomy tube is still warranted in high-risk patients and nutrition intervention remains critical.
References
Brown TE, Spurgin AL, Ross L, Tripcony L, Keller J, Hughes BG et al. Validated swallowing and nutrition guidelines for patients with head and neck cancer: Identification of high-risk patients for proactive gastrostomy. Head Neck 2012; 35: 1385–1391.
Hughes BG, Jain VK, Brown T, Spurgin AL, Hartnett G, Keller J et al. Decreased hospital stay and significant cost savings after routine use of prophylactic gastrostomy for high-risk patients with head and neck cancer receiving chemoradiotherapy at a tertiary cancer institution. Head Neck 2012; 35: 436–442.
Brown T, Ross L, Jones L, Hughes B, Banks M . Nutrition outcomes following implementation of validated swallowing and nutrition guidelines for patients with head and neck cancer. Support Care Cancer 2014; 22: 2381–2391.
Nugent B, Lewis S, O'Sullivan JM . Enteral feeding methods for nutritional management in patients with head and neck cancers being treated with radiotherapy and/or chemotherapy. Cochrane Database Syst Rev (Online) 2013; 1: CD007904.
Tyldesley S, Sheehan F, Munk P, Tsang V, Skarsgard D, Bowman CA et al. The use of radiologically placed gastrostomy tubes in head and neck cancer patients receiving radiotherapy. Int J Radiat Oncol Biol Phys 1996; 36: 1205–1209.
Senft M, Fietkau R, Iro H, Sailer D, Sauer R . The influence of supportive nutritional therapy via percutaneous endoscopically guided gastrostomy on the quality of life of cancer patients. Support Care Cancer 1993; 1: 272–275.
Lee JH, Machtay M, Unger LD, Weinstein GS, Weber RS, Chalian AA et al. Prophylactic gastrostomy tubes in patients undergoing intensive irradiation for cancer of the head and neck. Arch Otolaryngol Head Neck Surg 1998; 124: 871–875.
Vergeer MR, Doornaert PA, Rietveld DH, Leemans CR, Slotman BJ, Langendijk JA . Intensity-modulated radiotherapy reduces radiation-induced morbidity and improves health-related quality of life: results of a nonrandomized prospective study using a standardized follow-up program. Int J Radiat Oncol Biol Phys 2009; 74: 1–8.
Sanguineti G, Gunn GB, Parker BC, Endres EJ, Zeng J, Fiorino C . Weekly dose-volume parameters of mucosa and constrictor muscles predict the use of percutaneous endoscopic gastrostomy during exclusive intensity-modulated radiotherapy for oropharyngeal cancer. Int J Radiat Oncol Biol Phys 2011; 79: 52–59.
Romesser PB, Romanyshyn JC, Schupak KD, Setton J, Riaz N, Wolden SL et al. Percutaneous endoscopic gastrostomy in oropharyngeal cancer patients treated with intensity-modulated radiotherapy with concurrent chemotherapy. Cancer 2012; 118: 6072–6078.
Corry J, Poon W, McPhee N, Milner AD, Cruickshank D, Porceddu SV et al. Randomized study of percutaneous endoscopic gastrostomy versus nasogastric tubes for enteral feeding in head and neck cancer patients treated with (chemo)radiation. J Med Imaging Radiat Oncol 2008; 52: 503–510.
Mekhail TM, Adelstein DJ, Rybicki LA, Larto MA, Saxton JP, Lavertu P . Enteral nutrition during the treatment of head and neck carcinoma: is a percutaneous endoscopic gastrostomy tube preferable to a nasogastric tube? Cancer 2001; 91: 1785–1790.
Kramer S, Newcomb M, Hessler J, Siddiqui F . Prophylactic versus reactive PEG tube placement in head and neck cancer. Otolaryngol Head Neck Surg 2014; 150: 407–412.
Amin N, Reddy K, Westerly D, Raben D, DeWitt P, Chen C . Sparing the larynx and esophageal inlet expedites feeding tube removal in patients with stage III-IV oropharyngeal squamous cell carcinoma treated with intensity-modulated radiotherapy. Laryngoscope 2012; 122: 2736–2742.
Rusthoven KE, Raben D, Ballonoff A, Kane M, Song JI, Chen C . Effect of radiation techniques in treatment of oropharynx cancer. Laryngoscope 2008; 118: 635–639.
de Arruda FF, Puri DR, Zhung J, Narayana A, Wolden S, Hunt M et al. Intensity-modulated radiation therapy for the treatment of oropharyngeal carcinoma: the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys 2006; 64: 363–373.
Ruchala KJ, Olivera GH, Schloesser EA, Mackie TR., Megavoltage CT . on a tomotherapy system. Phys Med Biol 1999; 44: 2597–2621.
Fiorino C, Dell'Oca I, Pierelli A, Broggi S, De Martin E, Di Muzio N et al. Significant improvement in normal tissue sparing and target coverage for head and neck cancer by means of helical tomotherapy. Radiother Oncol 2006; 78: 276–282.
Sheng K, Molloy JA, Read PW . Intensity-modulated radiation therapy (IMRT) dosimetry of the head and neck: a comparison of treatment plans using linear accelerator-based IMRT and helical tomotherapy. Int J Radiat Oncol Biol Phys 2006; 65: 917–923.
Lee TF, Fang FM, Chao PJ, Su TJ, Wang LK, Leung SW . Dosimetric comparisons of helical tomotherapy and step-and-shoot intensity-modulated radiotherapy in nasopharyngeal carcinoma. Radiother Oncol 2008; 89: 89–96.
Ferguson ML, Bauer J, Gallagher B, Capra S, Christie DR, Mason BR . Validation of a malnutrition screening tool for patients receiving radiotherapy. Australas Radiol 1999; 43: 325–327.
Isenring E, Zabel R, Bannister M, Brown T, Findlay M, Kiss N et al. Updated evidence-based practice guidelines for the nutritional management of patients receiving radiation therapy and/or chemotherapy. Nutr Diet 2013; 70: 312–324.
Rivadeneira DE, Evoy D, Fahey TJ, Lieberman MD, Daly JM . Nutritional support of the cancer patient. CA Cancer J Clin 1998; 48: 69–80.
Attar A, Malka D, Sabate JM, Bonnetain F, Lecomte T, Aparicio T et al. Malnutrition is high and underestimated during chemotherapy in gastrointestinal cancer: an AGEO prospective cross-sectional multicenter study. Nutr Cancer 2012; 64: 535–542.
Langius JA, van Dijk AM, Doornaert P, Kruizenga HM, Langendijk JA, Leemans CR et al. More than 10% weight loss in head and neck cancer patients during radiotherapy is independently associated with deterioration in quality of life. Nutr Cancer 2013; 65: 76–83.
Langius JA, Bakker S, Rietveld DH, Kruizenga HM, Langendijk JA, Weijs PJ et al. Critical weight loss is a major prognostic indicator for disease-specific survival in patients with head and neck cancer receiving radiotherapy. Br J Cancer 2013; 109: 1093–1099.
Martin L, Senesse P, Gioulbasanis I, Antoun S, Bozzetti F, Deans C et al. Diagnostic criteria for the classification of cancer-associated weight loss. J Clin Oncol. 2015; 33: 90–99.
Hocking JS, Stein A, Conway EL, Regan D, Grulich A, Law M et al. Head and neck cancer in Australia between 1982 and 2005 show increasing incidence of potentially HPV-associated oropharyngeal cancers. Br J Cancer 2011; 104: 886–891.
Chatterjee S, Mott JH, Smyth G, Dickson S, Dobrowsky W, Kelly CG . Clinical challenges in the implementation of a tomotherapy service for head and neck cancer patients in a regional UK radiotherapy centre. Br J Radiol 2011; 84: 358–366.
Caudell JJ, Schaner PE, Desmond RA, Meredith RF, Spencer SA, Bonner JA . Dosimetric factors associated with long-term dysphagia after definitive radiotherapy for squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 2010; 76: 403–409.
Gunn GB, Endres EJ, Parker B, Sormani MP, Sanguineti G . A phase I/II study of altered fractionated IMRT alone for intermediate T-stage oropharyngeal carcinoma. Strahlenther Onkol 2010; 186: 489–495.
Studer G, Peponi E, Kloeck S, Dossenbach T, Huber G, Glanzmann C . Surviving hypopharynx-larynx carcinoma in the era of IMRT. Int J Radiat Oncol Biol Phys 2010; 77: 1391–1396.
van den Berg MG, Rasmussen-Conrad EL, van Nispen L, van Binsbergen JJ, Merkx MA . A prospective study on malnutrition and quality of life in patients with head and neck cancer. Oral Oncol 2008; 44: 830–837.
Capuano G, Grosso A, Gentile PC, Battista M, Bianciardi F, Di Palma A et al. Influence of weight loss on outcomes in patients with head and neck cancer undergoing concomitant chemoradiotherapy. Head Neck 2008; 30: 503–508.
Capelle L, Mackenzie M, Field C, Parliament M, Ghosh S, Scrimger R . Adaptive radiotherapy using helical tomotherapy for head and neck cancer in definitive and postoperative settings: initial results. Clin Oncol 2012; 24: 208–215.
You SH, Kim SY, Lee CG, Keum KC, Kim JH, Lee IJ et al. Is there a clinical benefit to adaptive planning during tomotherapy in patients with head and neck cancer at risk for xerostomia? Am J Clin Oncol 2012; 35: 261–266.
Duma MN, Kampfer S, Schuster T, Winkler C, Geinitz H . Adaptive radiotherapy for soft tissue changes during helical tomotherapy for head and neck cancer. Strahlenther Onkol 2012; 188: 243–247.
Loo H, Fairfoul J, Chakrabarti A, Dean JC, Benson RJ, Jefferies SJ et al. Tumour shrinkage and contour change during radiotherapy increase the dose to organs at risk but not the target volumes for head and neck cancer patients treated on the TomoTherapy HiArt system. Clin Oncol 2011; 23: 40–47.
Chao KS, Low DA, Perez CA, Purdy JA . Intensity-modulated radiation therapy in head and neck cancers: The Mallinckrodt experience. Int J Cancer 2000; 90: 92–103.
Silander E, Jacobsson I, Berteus-Forslund H, Hammerlid E . Energy intake and sources of nutritional support in patients with head and neck cancer—a randomised longitudinal study. Eur J Clin Nutr 2013; 67: 47–52.
Brown T, Banks M, Hughes B, Kenny L, Lin C, Bauer J . Protocol for a randomized controlled trial of early prophylactic feeding via gastrostomy versus standard care in high risk patients with head and neck cancer. BMC Nurs 2014; 13: 17.
Arends J, Bodoky G, Bozzetti F, Fearon K, Muscaritoli M, Selga G et al. ESPEN Guidelines on Enteral Nutrition: non-surgical oncology. Clin Nutr 2006; 25: 245–259.
Brown T, Crombie J, Spurgin AL, Tripcony L, Keller J, Hughes B et al. Improving guideline sensitivity and specificity for the identification of proactive gastrostomy placement in patients with head and neck cancer. Head Neck 35: 1385–1391. in press.
Bauer J, Capra S, Ferguson M . Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr 2002; 56: 779–785.
White JV, Guenter P, Jensen G, Malone A, Schofield M . Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr 2012; 36: 275–283.
Acknowledgements
We thank Dr Tuan Ha and Vanessa Getliffe for their assistance in data collection, and the staff in medical records and the Combined Head and Neck Clinic at the Royal Brisbane and Women’s Hospital (RBWH) for their support. This study was supported by the Royal Brisbane and Women’s Hospital PhD Scholarship.
Author contributions
TB initiated the study concept. TB, JB, MB and BH contributed to study design. TB and CL participated in the acquisition of data. TB analysed the data and prepared the first draft of the manuscript. All the authors participated in the interpretation of the data, critical revision of the manuscript and the final approval of the submitted version. As corresponding author, TB has full access to all the data in the study and has final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
TB received a Royal Brisbane and Women’s Hospital PhD Scholarship. The funding body were not involved in the study design, data collection, analysis and interpretation of results, writing of the report or the decision to submit the article for publication. All other authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Brown, T., Banks, M., Hughes, B. et al. New radiotherapy techniques do not reduce the need for nutrition intervention in patients with head and neck cancer. Eur J Clin Nutr 69, 1119–1124 (2015). https://doi.org/10.1038/ejcn.2015.141
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.141
- Springer Nature Limited
This article is cited by
-
Nutritional parameters associated with hospital admissions in patients being treated for head and neck cancer
Supportive Care in Cancer (2020)
-
Randomised controlled trial of early prophylactic feeding vs standard care in patients with head and neck cancer
British Journal of Cancer (2017)
-
DARS: a phase III randomised multicentre study of dysphagia- optimised intensity- modulated radiotherapy (Do-IMRT) versus standard intensity- modulated radiotherapy (S-IMRT) in head and neck cancer
BMC Cancer (2016)
-
Validation of an updated evidence-based protocol for proactive gastrostomy tube insertion in patients with head and neck cancer
European Journal of Clinical Nutrition (2016)