Abstract
HLA 1-locus-mismatched unrelated donors (1MMUD) have been used in allogeneic hematopoietic stem cell transplantation (allo-HCT) for patients who lack an HLA-matched donor. We retrospectively analyzed 3313 patients with acute leukemia or myelodysplastic syndrome who underwent bone marrow transplantation from an HLA allele-matched unrelated donor (MUD) or 1MMUD between 2009 and 2014. We compared the outcomes of MUD (n=2089) and 1MMUD with antithymocyte globulin (ATG) (1MM-ATG(+); n=109) with those of 1MMUD without ATG (1MM-ATG(−); n=1115). The median total dose of ATG (thymoglobulin) was 2.5 mg/kg (range 1.0–11.0 mg/kg) in the 1MM-ATG(+) group. The rates of grade III–IV acute GvHD, non-relapse mortality (NRM) and overall mortality were significantly lower in the MUD group than in the 1MM-ATG(−) group (hazard ratio (HR) 0.77, P=0.016; HR 0.74; P<0.001; and HR 0.87, P=0.020, respectively). Likewise, the rates of grade III–IV acute GVHD, NRM and overall mortality were significantly lower in the 1MM-ATG(+) group than in the 1MM-ATG(−) group (HR 0.42, P=0.035; HR 0.35, P<0.001; and HR 0.71, P=0.042, respectively). The outcome of allo-HCT from 1MM-ATG(−) was inferior to that of allo-HCT from MUD even in the recent cohort. However, the negative impact of 1MMUD disappeared with the use of low-dose ATG without increasing the risk of relapse.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HCT) from unrelated donors has been established as a curative therapy for various malignant and nonmalignant hematological disorders in the absence of an HLA-identical sibling. The development of high-resolution HLA typing and GvHD prophylaxis has greatly contributed to this success. The transplant outcomes from an HLA-A, -B, -C and -DRB1 allele-matched unrelated donor (MUD) are now comparable to those from an HLA-matched related donor.1, 2, 3 However, it is difficult to find MUD for patients who have rare HLA haplotypes. Therefore, an HLA 1-locus-mismatched unrelated donor (1MMUD) has been considered as an alternative donor in allo-HCT when an HLA-matched related or unrelated donor is unavailable. However, the outcome has been shown to be inferior to that of allo-HCT from MUD mainly because of higher rates of GvHD and graft failure.4, 5, 6, 7 Therefore, an effective intervention is necessary to overcome this drawback.
Antithymocyte globulin (ATG) has been used as part of conditioning in allo-HCT to decrease the incidences of acute and chronic GvHD. Some previous studies reported that the use of ATG significantly reduced the incidence of GvHD,8, 9, 10, 11, 12, 13, 14 but a high dose of ATG increased the risks of relapse and infections.9, 15, 16, 17 Unfortunately, the optimal dose of ATG remains unclear. The optimal ATG dose should be determined based on a fine balance between the reduction of GvHD and the increase in relapse and infections. In addition, the optimal ATG dose may differ according to the number of HLA mismatches, donor source, conditioning regimen, disease type, disease stage and race. Therefore, the aims of the current study were to compare the transplant outcomes among 1MMUD without ATG, 1MMUD with ATG and MUD in allogeneic bone marrow transplantation (BMT) and to evaluate the effectiveness of ATG in BMT from 1MMUD using a recent cohort. Finally, we investigated the optimal dose of ATG for Japanese patients with acute leukemia or myelodysplastic syndrome who received BMT from 1MMUD.
Materials and methods
Patients
Patients aged at least 16 years with AML, ALL or myelodysplastic syndrome who underwent a first BMT from MUD or 1MMUD (one allele or Ag mismatch in the graft-versus-host direction) through the Japan Marrow Donor Program between 2009 and 2014 were included in this study. Clinical data for these patients were obtained from the Transplant Registry Unified Management Program (TRUMP),18, 19 which includes clinical data of HCT performed in Japan. Of the 3404 patients who fulfilled these selection criteria, the following patients were excluded: 56 patients who received ATG in BMT from MUD; 16 patients who received stem cells manipulated by ex vivo T-cell depletion or CD34 selection; 1 patient who lacked data on survival status; and 18 patients who lacked data on the brand or dose of ATG, or who received any brand of ATG other than thymoglobulin (Sanofi, Paris, France), which is the only brand of ATG approved for GvHD prophylaxis under the Japanese National Health Insurance system. Finally, 1115 patients who underwent BMT from 1MMUD without ATG (1MM-ATG(−)), 109 patients who did so from 1MMUD with ATG (1MM-ATG(+)) and 2089 patients who did so from MUD were included in the study. This study was planned by the HLA Working Group of the Japan Society for Hematopoietic Cell Transplantation and approved by the data management committees of TRUMP and the Institutional Review Board of Saitama Medical Center, Jichi Medical University.
Histocompatibility
Histocompatibility data for serological and genomic typing for the HLA-A, HLA-B, HLA-C and HLA-DR loci were obtained from the TRUMP database, which includes HLA allele data that were determined retrospectively by Japan Marrow Donor Program using frozen samples.20, 21 An HLA mismatch in the graft-versus-host direction was defined as when the recipient’s Ags or alleles were not shared by the donor, and an HLA mismatch in the host-versus-graft direction was defined as when the donor’s Ags or alleles were not shared by the recipient. In this study, patients who received BMT from an HLA 1MMUD in only the host-versus-graft direction were excluded.
End points and definitions
The primary end point was overall survival (OS) after BMT. Secondary end points were disease-free survival (DFS), GvHD-free, relapse-free survival (GRFS), and the cumulative incidences of neutrophil and platelet engraftment, acute and chronic GvHD, relapse and non-relapse mortality (NRM). Neutrophil recovery was defined as an absolute neutrophil count of at least 500 cells/mm3 for 3 consecutive days after transplantation. Platelet recovery was defined as an absolute platelet count of at least 5 × 104 cells/mm3 without platelet transfusion. Acute and chronic GvHD were graded according to previously published criteria.22, 23 The incidence of chronic GvHD was evaluated in patients who survived for at least 100 days. NRM was defined as death without relapse, DFS was defined as survival without disease progression or relapse, and GRFS was defined as survival without grade III–IV acute GvHD, chronic GvHD requiring systemic treatment, relapse or death from any cause.24 We classified the conditioning regimen as either myeloablative or reduced intensity according to the operational definitions of the National Marrow Donor Program/Center for International Blood and Marrow Transplant Research.25 Acute leukemia in first or second remission, and myelodysplastic syndrome excluding refractory anemia with excess blasts or leukemic transformation were defined as standard-risk diseases, and others were defined as high-risk diseases.
Statistical analysis
Categorical variables were compared between groups with the χ2-test or Fisher’s exact test, and continuous variables were compared with the Kruskal–Wallis test. The probabilities of DFS, GRFS and OS were estimated according to the Kaplan–Meier method, and compared among groups with the log-rank test. The probabilities of neutrophil and platelet engraftment, acute and chronic GvHD, relapse and NRM were estimated on the basis of cumulative incidence methods, and compared among groups with the Gray test, considering death without engraftment as a competing event for neutrophil and platelet engraftment, death or relapse without GvHD as a competing event for acute and chronic GvHD, death without relapse as a competing event for relapse, and relapse as a competing event for NRM.26, 27 Multivariate analyses for DFS, GRFS and OS were performed using the Cox proportional hazards model, whereas multivariate analyses for acute and chronic GvHD, relapse and NRM were performed using the Fine and Gray regression model.28 The following variables were considered; the patient’s age at transplantation (⩽50 years or >50 years), patient sex, disease type (AML, ALL or myelodysplastic syndrome), disease risk (standard risk or high risk), Eastern Cooperative Oncology Group Performance Status (0–1 or 2–4), HCT-Specific Comorbidity Index (0, 1–2 or ⩾3), intensity of the conditioning regimen (myeloablative or reduced intensity), GvHD prophylaxis (cyclosporine-based or tacrolimus-based), year of transplantation (2009–2011 or 2012–2014) and donor type (MUD, 1MM-ATG(−) or 1MM-ATG(+)). Factors other than donor type were deleted from the model in a stepwise manner to exclude factors with a P-value of 0.05 or higher. All P-values were two-sided and P-values of 0.05 or less were considered statistically significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University),29, 30 which is a graphical user interface for R (The R Foundation for Statistical Computing, version 3.0.2, Vienna, Austria). More precisely, it is a modified version of R commander (version 2.0-3) that was designed to add statistical functions that are frequently used in biostatistics.
Results
Patient characteristics
The characteristics of the patients in each group are shown in Table 1. The median ages of the recipients at transplantation were 49 (16–74), 53 (16–71) and 50 (16–77) years in the 1MM-ATG(−), 1MM-ATG(+) and MUD groups, respectively. The proportion of patients with performance status 2–4 in the 1MM-ATG(+) group (16.5%) was significantly higher than those in the 1MM-ATG(−) (7.5%) and MUD groups (6.5%). On the other hand, there were no significant differences among the three groups with respect to recipient sex, disease, disease risk, HCT-Specific Comorbidity Index or conditioning regimen. In the 1MM-ATG(+) group, 64 (5.7%), 12 (1.1%), 328 (29.4%) and 711 (63.8%) patients underwent single HLA-A, HLA-B, HLA-C and HLA-DR Ag-/allele-mismatched BMT, respectively, whereas 8 (7.3%), 3 (2.8%), 17 (15.6%) and 81(74.3%) patients in the 1MM-ATG(−) group, respectively (Supplementary Table 1). The median total dose of ATG (thymoglobulin) in the 1MM-ATG(+) group was 2.5 mg/kg (range 1.0–11.0 mg/kg) and about 96% of patients received ATG at a total dose of 5.0 mg/kg or lower.
OS, DFS and GRFS
The 3-year unadjusted OS, DFS and GRFS rates were 52.4% (95% CI, 49.0–55.6%), 47.3% (95% CI, 44.0–50.6%) and 28.2% (95% CI, 25.2–31.2%) in the 1MM-ATG(−) group; 56.3% (95% CI, 44.2–66.8%), 60.2% (95% CI, 49.1–69.6%) and 38.9% (95% CI, 28.3–49.4%) in the 1MM-ATG(+) group; and 55.7% (95% CI, 53.2–58.0%), 51.6% (95% CI, 49.2–54.0%) and 33.0% (95% CI, 30.8–35.2%) in the MUD group (P=0.020, Figure 1a; P=0.0092, Figure 1b; and P=0.0019, Figure 1c). In the multivariate analysis, OS, DFS and GRFS in the MUD group were significantly superior to those in the 1MM-ATG(−) group (HR 0.87, 95% CI, 0.78–0.98, P=0.020; HR 0.88, 95% CI, 0.79–0.98, P=0.021; and HR 0.89, 95% CI, 0.81–0.97, P=0.0088, respectively; Table 2). Likewise, OS, DFS and GRFS in the 1MM-ATG(+) group were also significantly superior to those in the 1MM-ATG(−) group (HR 0.71, 95% CI, 0.50–0.99, P=0.042; HR 0.67, 95% CI, 0.48–0.94, P=0.021; and HR 0.73, 95% CI, 0.56–0.96, P=0.023, respectively; Table 2).
NRM and relapse
The cumulative incidence of NRM at 3 years in the 1MM-ATG(−) group (26.6%; 95% confidence interval (CI), 23.7–29.5) was significantly higher than those in the 1MM-ATG(+) (11.9%; 95% CI, 5.9–20.2) and MUD groups (21.4%; 95% CI, 19.5–23.4; P<0.001; Figure 1d). A multivariate analysis confirmed that the risks of NRM in the 1MM-ATG(+) (HR, 0.35; 95% CI, 0.19–0.65; P<0.001) and MUD groups (HR, 0.74; 95% CI, 0.63–0.87; P<0.001) were lower than that in the 1MM-ATG(−) group (Table 2). On the other hand, there were no significant differences in relapse rate (Figure 1e), and the relapse risk was comparable among the three groups (Table 2). The relapse rate tended to be higher in the 1MM-ATG(+) group among standard-risk patients, but did not significantly differ among the three groups among high-risk patients (Supplementary Figure 1). The causes of death are summarized in Supplementary Table 2. Disease relapse was the most common cause of death, and accounted for 31%, 44% and 40% of all deaths in the 1MM-ATG(−), 1MM-ATG(+) and MUD groups, respectively. GvHD and infections accounted for 10% and 22%, 3% and 15%, and 8% and 18% of all deaths in the 1MM-ATG(−), 1MM-ATG(+) and MUD groups, respectively.
Engraftment and GvHD
The cumulative incidences of neutrophil engraftment at day 50 and platelet engraftment at day 150 in the MUD group (96.7%, 95% CI, 95.8–97.4%; and 80.4%, 95% CI, 78.6–82.0%) were both higher than those in the 1MM-ATG(−) group (95.0%, 95% CI, 93.5–96.1%; and 70.9%, 95% CI, 68.1–73.5%) or the 1MM-ATG(+) group (93.6%, 95% CI, 86.6–97.0%; and 75.3%, 95% CI, 65.9–82.4%; Figures 2a and b), although there was no statistically significant difference in the cumulative incidence of neutrophil engraftment between the 1MM-ATG(+) and MUD groups. There were no significant differences in chimerism after allo-HCT between the 1MM-ATG(−) and 1MM-ATG(+) groups (702 and 83 in the complete donor chimerism, 115 and 8 in dominant donor chimerism (⩾80%), 70 and 9 in mixed chimerism, 5 and 1 in the autologous recovery, and 223 and 8 in others/unknown, respectively, P=0.40).
The cumulative incidences of grade II–IV and III–IV acute GvHD at 100 days were 44.5% (95% CI, 41.5– 47.4%) and 13.1% (95% CI, 11.2–15.2%) in the 1MM-ATG(−) group, 33.4% (95% CI, 24.5–42.5%) and 5.8% (95% CI, 2.4–11.6%) in the 1MM-ATG(+) group, and 36.1% (95% CI, 34.1–38.2%) and 10.5% (95% CI, 9.2–11.9%) in the MUD group (P<0.001 and P=0.0085; Figures 3a and b). The risks of grade II–IV and III–IV acute GvHD in the 1MM-ATG(+) (hazard ratio (HR), 0.69; 95% CI, 0.49–0.98; P=0.040; and HR, 0.42; 95% CI, 0.19–0.94; P=0.035) and MUD groups (HR, 0.75; 95% CI, 0.67–0.84; P<0.001; and HR, 0.77; 95% CI, 0.63–0.95; P=0.016) were significantly lower than those in the 1MM-ATG(−) group, after adjusting for other significant factors in multivariate analyses (Table 2). The cumulative incidences of chronic and extensive chronic GvHD at 3 years were 38.1% (95% CI, 34.8–41.4%) and 21.5% (95% CI, 18.8–24.4%) in the 1MM-ATG(−) group; 34.0% (95% CI, 24.1–44.0%) and 16.3% (95% CI, 9.3–25.0%) in the 1MM-ATG(+) group; and 38.4% (95% CI, 36.1–40.8%) and 22.2% (95% CI, 20.2–24.2%) in the MUD group (P=0.85 and 0.44; Figures 3 and d). In a multivariate analysis, no significant difference was found among the three groups (Table 2).
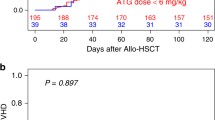
Impact of ATG dose in the 1MMUD-ATG(+) group
Next, we divided patients in the 1MM-ATG(+) group into three groups according to the total dose of ATG (b: <2 mg/kg; c: 2–4 mg/kg; and d: >4 mg/kg), and compared the outcomes in the three groups with those in the 1MM-ATG(−) group (a: 0 mg/kg). The patient characteristics of these groups are shown in Supplementary Table 3. The median total dose of ATG was 1.0 mg/kg (range 1.0–1.5 mg/kg), 2.5 mg/kg (range 2.0–3.75mg/kg) and 5.0 mg/kg (range 5.0–11.0 mg/kg) in the b: <2mg/kg, c: 2–4 mg/kg and d: >4 mg/kg groups, respectively. The cumulative incidences of grade III–IV acute GvHD at 100 days and extensive chronic GvHD at 2 years were 13.1% (95% CI, 11.2–15.2%) and 21.1% (95% CI, 18.5–23.9%) in the a: 0 mg/kg group; 5.3% (95% CI, 0.3–22.0%) and 52.1% (95% CI, 23.4–74.6%) in the b: <2 mg/kg group; 3.8% (95% CI, 0.7–11.6%) and 6.8% (95% CI, 1.7–16.8%) in the c: 2–4 mg/kg group; and 9.7% (95% CI, 2.4–23.2%) and 11.8% (95% CI, 2.8–28.0%) in the d: >4 mg/kg group (Figures 4a and b). The incidence of NRM at 2 years and the rate of 1-year GRFS were 24.1% (95% CI, 21.5–26.8%) and 38.8% (95% CI, 35.9–41.8%) in the a: 0 mg/kg group; 16.1% (95% CI, 3.7–36.3%) and 28.3% (95% CI, 10.4–49.6%) in the b: <2 mg/kg group; 6.4% (95% CI, 1.6–16.0%) and 52.6% (95% CI, 38.4–64.9%) in the c: 2–4 mg/kg group; and 12.7% (95% CI, 3.0–29.6%) and 49.4% (95% CI, 30.2–66.0%) in the d: >4 mg/kg group (P=0.014 and 0.055; Figures 4d and e).
Discussion
This study showed that OS in the 1MM-ATG(−) group was inferior to that in the MUD group even in a recent cohort (2009–2014). The difference in OS between the two groups was mainly due to the higher NRM in the 1MM-ATG(−) group, which was most likely associated with a higher incidence of acute GvHD. On the other hand, the risks of acute GvHD and NRM in the 1MM-ATG(+) group were significantly lower than those in the 1MM-ATG(−) group without an increase in relapse, although there was no statistically significant difference in chronic GvHD between the two groups. Accordingly, OS in the 1MM-ATG(+) group was significantly superior to that in the 1MM-ATG(−) group. In addition, most transplant outcomes in the 1MM-ATG(+) group were comparable to those in the MUD group. In fact, in a multivariate analysis using the MUD group as a reference, no significant differences in OS, DFS, GRFS or relapse rate were found between the two groups, and NRM in the 1MM-ATG(+) group was superior to that in the MUD group (data not shown). Therefore, the appropriate use of ATG as part of conditioning for GvHD prophylaxis should be considered in BMT from 1MMUD.
Most previous studies have reported that the use of ATG reduced the incidence of acute GvHD and/or chronic GvHD.8, 9, 10, 11, 12, 13, 14 On the other hand, several studies have noted the drawbacks of high doses of ATG, such as increased rates of relapse or infection.9, 15, 16, 17 In this study, however, the cumulative incidence of relapse and the proportion of infection-related mortality did not significantly differ between the 1MM-ATG(−) group and the 1MM-ATG(+) group. This difference might result from differences in the dose of ATG or differences in risk factors for GvHD and relapse, that is, the number of HLA mismatches, donor source, disease stage and so on. Finke et al.10 reported that the addition of ATG-Fresenius (total dose 60 mg/kg) to standard GvHD prophylaxis with cyclosporin and methotrexate reduced the incidences of acute and chronic GvHD without increasing the risk of relapse in patients who underwent allo-HCT from MUD. Likewise, Walker et al.31 showed that the use of thymoglobulin (total dose of 4.5 mg/kg) in allo-HCT from an MUD or 1MMUD markedly decreased both the need for immunosuppressive treatment and the symptoms of chronic GvHD in comparison with the no-ATG group. In these two large prospective, randomized trials, however, there were no significant differences in OS between the ATG group and the no-ATG group, although the follow-up duration in the latter trial might have been insufficient for the evaluation of OS.
The current study suggested that the use of ATG might improve OS in patients who received BMT from 1MMUD. The major difference between this study and previous studies, other than the presence or absence of HLA mismatch, was the dose of ATG. In the current study, most patients received a relatively lower dose of ATG (median 2.5 mg/kg). As shown by the comparison of ATG doses (Figure 4), a total dose of 2–4 mg/kg might be sufficient to prevent severe acute GvHD in BMT from 1MMUD, although it might be insufficient to decrease the incidence of chronic GvHD. Kim et al.12 also reported that a low dose of thymoglobulin (2.5 mg/kg) significantly decreased acute GvHD and NRM in allo-HCT from HLA-mismatched unrelated donors in Korea. Their results were quite similar to our findings. In contrast, in a randomized trial from an Italian group Gruppo Italiano Trapianti di Midollo Osseo (GITMO), thymoglobulin at 7.5 mg/kg did not significantly reduce acute GvHD compared with standard GvHD prophylaxis in allo-HCT from an unrelated donor, whereas a higher dose (15 mg/kg) reduced severe acute GvHD but increased the risk of infection, although this study was performed before the establishment of current criteria of HLA matching.9 Therefore, the suitable dose of ATG may be different between Asian and Caucasian patients. Several studies have shown that the incidence of GvHD in Asian patients is lower than that in Caucasian patients.32, 33, 34 Thus, race should also be considered when we examine the optimal dose of ATG.
The reduction of chronic GvHD may improve the quality of life (QOL) of the patients, as severe chronic GvHD is the leading cause of late morbidity and mortality in long-term survivors. However, there was no statistically significant difference in the incidence of chronic GvHD between the 1MM-ATG(−) and 1MM-ATG(+) groups in this study. This might be because of the lower dose of ATG or because there was insufficient statistical power to detect a difference. A lower dose of ATG might be able to significantly inhibit the proliferation of T cells, but not B cells. In addition, several studies have reported that another possible benefit of ATG is the early discontinuation of immunosuppressive drugs,14, 31, 35 which would also lead to improved QOL. A lower dose of ATG might allow patients to discontinue immunosuppressive drugs early even if there is no difference in the incidence of chronic GvHD, although we could not assess the duration of immunosuppressive drug use due to the lack of data. GRFS, which is considered to reflect QOL early after allo-HCT, in the 1MM-ATG(+) group was superior to that in the 1MM-ATG(−) group. Unfortunately, however, we could not precisely evaluate QOL because relevant data were not included in the database.
This study has several limitations. First, data on the timing of ATG infusion were unavailable. The duration between ATG infusion and allo-HCT may affect the degree of donor T-cell depletion and the incidence of GvHD. Second, data on cytogenetic or genetic abnormalities in hematological malignancies were insufficient, and therefore, it was impossible to accurately assess the impact of the use of ATG on relapse. Finally, there were fewer patients in the 1MM-ATG(+) group than in the other two groups, and therefore, the statistical power of the analysis of ATG dose was limited. In addition, according to the policy of the TRUMP database, we could not obtain information about the transplant center for each patient, and therefore, we could not directly assess a center effect. With regard to the factors that may be affected by the centers’ policy, there were no significant differences in the use of G-CSF in AML patients or the brand of calcineurin inhibitors among the groups, and, therefore, we suppose that there was not a strong center effect. However, it was impossible to completely deny the presence of a center effect.
In conclusion, the outcome of allo-HCT from 1MM-ATG(−) was inferior to that of allo-HCT from MUD even in a recent cohort. However, the negative impact of 1MMUD disappeared with the use of low-dose ATG without increasing the risk of relapse. A large prospective study is warranted to confirm the role of low-dose ATG in allo-HCT from 1MMUD.
References
Yakoub-Agha I, Mesnil F, Kuentz M, Boiron JM, Ifrah N, Milpied N et al. Allogeneic marrow stem-cell transplantation from human leukocyte antigen-identical siblings versus human leukocyte antigen-allelic-matched unrelated donors (10/10) in patients with standard-risk hematologic malignancy: a prospective study from the French Society of Bone Marrow Transplantation and Cell Therapy. J Clin Oncol 2006; 24: 5695–5702.
Schetelig J, Bornhauser M, Schmid C, Hertenstein B, Schwerdtfeger R, Martin H et al. Matched unrelated or matched sibling donors result in comparable survival after allogeneic stem-cell transplantation in elderly patients with acute myeloid leukemia: a report from the cooperative German Transplant Study Group. J Clin Oncol 2008; 26: 5183–5191.
Kanda J, Saji H, Fukuda T, Kobayashi T, Miyamura K, Eto T et al. Related transplantation with HLA-1 Ag mismatch in the GVH direction and HLA-8/8 allele-matched unrelated transplantation: a nationwide retrospective study. Blood 2012; 119: 2409–2416.
Flomenberg N, Baxter-Lowe LA, Confer D, Fernandez-Vina M, Filipovich A, Horowitz M et al. Impact of HLA class I and class II high-resolution matching on outcomes of unrelated donor bone marrow transplantation: HLA-C mismatching is associated with a strong adverse effect on transplantation outcome. Blood 2004; 104: 1923–1930.
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood 2007; 110: 4576–4583.
Kanda Y, Kanda J, Atsuta Y, Maeda Y, Ichinohe T, Ohashi K et al. Impact of a single human leucocyte antigen (HLA) allele mismatch on the outcome of unrelated bone marrow transplantation over two time periods. A retrospective analysis of 3003 patients from the HLA Working Group of the Japan Society for Blood and Marrow Transplantation. Br J Haematol 2013; 161: 566–577.
Kanda J, Ichinohe T, Fuji S, Maeda Y, Ohashi K, Fukuda T et al. Impact of HLA mismatch direction on the outcome of unrelated bone marrow transplantation: a retrospective analysis from the Japan Society for Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant 2015; 21: 305–311.
Bacigalupo A, Lamparelli T, Barisione G, Bruzzi P, Guidi S, Alessandrino PE et al. Thymoglobulin prevents chronic graft-versus-host disease, chronic lung dysfunction, and late transplant-related mortality: long-term follow-up of a randomized trial in patients undergoing unrelated donor transplantation. Biol Blood Marrow Transplant 2006; 12: 560–565.
Bacigalupo A, Lamparelli T, Bruzzi P, Guidi S, Alessandrino PE, di Bartolomeo P et al. Antithymocyte globulin for graft-versus-host disease prophylaxis in transplants from unrelated donors: 2 randomized studies from Gruppo Italiano Trapianti Midollo Osseo (GITMO). Blood 2001; 98: 2942–2947.
Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol 2009; 10: 855–864.
Socie G, Schmoor C, Bethge WA, Ottinger HD, Stelljes M, Zander AR et al. Chronic graft-versus-host disease: long-term results from a randomized trial on graft-versus-host disease prophylaxis with or without anti-T-cell globulin ATG-Fresenius. Blood 2011; 117: 6375–6382.
Kim HJ, Min WS, Cho BS, Eom KS, Kim YJ, Min CK et al. Successful prevention of acute graft-versus-host disease using low-dose antithymocyte globulin after mismatched, unrelated, hematopoietic stem cell transplantation for acute myelogenous leukemia. Biol Blood Marrow Transplant 2009; 15: 704–717.
Mohty M, Labopin M, Balere ML, Socie G, Milpied N, Tabrizi R et al. Antithymocyte globulins and chronic graft-vs-host disease after myeloablative allogeneic stem cell transplantation from HLA-matched unrelated donors: a report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Leukemia 2010; 24: 1867–1874.
Kuriyama K, Fuji S, Inamoto Y, Tajima K, Tanaka T, Inoue Y et al. Impact of low-dose rabbit anti-thymocyte globulin in unrelated hematopoietic stem cell transplantation. Int J Hematol 2016; 103: 453–460.
Hamadani M, Blum W, Phillips G, Elder P, Andritsos L, Hofmeister C et al. Improved nonrelapse mortality and infection rate with lower dose of antithymocyte globulin in patients undergoing reduced-intensity conditioning allogeneic transplantation for hematologic malignancies. Biol Blood Marrow Transplant 2009; 15: 1422–1430.
Soiffer RJ, Lerademacher J, Ho V, Kan F, Artz A, Champlin RE et al. Impact of immune modulation with anti-T-cell antibodies on the outcome of reduced-intensity allogeneic hematopoietic stem cell transplantation for hematologic malignancies. Blood 2011; 117: 6963–6970.
Baron F, Labopin M, Blaise D, Lopez-Corral L, Vigouroux S, Craddock C et al. Impact of in vivo T-cell depletion on outcome of AML patients in first CR given peripheral blood stem cells and reduced-intensity conditioning allo-SCT from a HLA-identical sibling donor: a report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant 2014; 49: 389–396.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol 2007; 86: 269–274.
Atsuta Y . Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol 2016; 103: 3–10.
Morishima Y, Sasazuki T, Inoko H, Juji T, Akaza T, Yamamoto K et al. The clinical significance of human leukocyte antigen (HLA) allele compatibility in patients receiving a marrow transplant from serologically HLA-A, HLA-B, and HLA-DR matched unrelated donors. Blood 2002; 99: 4200–4206.
Kawase T, Morishima Y, Matsuo K, Kashiwase K, Inoko H, Saji H et al. High-risk HLA allele mismatch combinations responsible for severe acute graft-versus-host disease and implication for its molecular mechanism. Blood 2007; 110: 2235–2241.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol 1991; 28: 250–259.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood 2015; 125: 1333–1338.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant 2009; 15: 367–369.
Gooley TA, Leisenring W, Crowley J, Storer BE . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Gray RJ . A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988; 16: 1141–1154.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Kanda Y . Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013; 48: 452–458.
Kanda J . Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol 2016; 103: 11–19.
Walker I, Panzarella T, Couban S, Couture F, Devins G, Elemary M et al. Pretreatment with anti-thymocyte globulin versus no anti-thymocyte globulin in patients with haematological malignancies undergoing haemopoietic cell transplantation from unrelated donors: a randomised, controlled, open-label, phase 3, multicentre trial. Lancet Oncol 2016; 17: 164–173.
Oh H, Loberiza FR Jr, Zhang MJ, Ringden O, Akiyama H, Asai T et al. Comparison of graft-versus-host-disease and survival after HLA-identical sibling bone marrow transplantation in ethnic populations. Blood 2005; 105: 1408–1416.
Morishima Y, Kawase T, Malkki M, Morishima S, Spellman S, Kashiwase K et al. Significance of ethnicity in the risk of acute graft-versus-host disease and leukemia relapse after unrelated donor hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2013; 19: 1197–1203.
Kanda J, Brazauskas R, Hu ZH, Kuwatsuka Y, Nagafuji K, Kanamori H et al. Graft-versus-host disease after HLA-matched sibling bone marrow or peripheral blood stem cell transplantation: comparison of North American Caucasian and Japanese populations. Biol Blood Marrow Transplant 2016; 22: 744–751.
Fuji S, Kim SW, Yano S, Hagiwara S, Nakamae H, Hidaka M et al. A prospective multicenter study of unrelated bone marrow transplants using a reduced-intensity conditioning regimen with low-dose ATG-F. Bone Marrow Transplant 2016; 51: 451–453.
Acknowledgements
We thank all of the physicians and staff members of the collaborating institutes of the Japan Society for Hematopoietic Stem Cell Transplantation.
Author contributions
KK, JK and YK designed the study and performed the statistical analysis; KK, JK, SF, MM, K Ikegame and YK interpreted the data and wrote the manuscript; KY, TF, TH, YO, NU, YK, K Iwato, TS, MH and HH provided the patient data; TF, TI and YA collected the patient data; and all of the authors interpreted the data, and reviewed and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Rights and permissions
About this article
Cite this article
Kawamura, K., Kanda, J., Fuji, S. et al. Impact of the presence of HLA 1-locus mismatch and the use of low-dose antithymocyte globulin in unrelated bone marrow transplantation. Bone Marrow Transplant 52, 1390–1398 (2017). https://doi.org/10.1038/bmt.2017.153
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.153
- Springer Nature Limited
This article is cited by
-
Human leukocyte antigen 7/8-matched unrelated bone marrow transplantation using anti-thymocyte globulin in children
International Journal of Hematology (2023)
-
Outcomes of patients with hematological malignancies who undergo unrelated donor hematopoietic stem cell transplantation with ATG-Fresenius versus ATG-Genzyme
Annals of Hematology (2023)
-
Personalizing rabbit anti-thymocyte globulin therapy for prevention of graft-versus-host disease after allogeneic hematopoietic cell transplantation: is there an optimal dose?
Bone Marrow Transplantation (2020)
-
Influence of HLA 1–3-locus mismatch and antithymocyte globulin administration in unrelated bone marrow transplantation
Annals of Hematology (2020)
-
Feasibility of salvage cord blood transplantation using a fludarabine, melphalan, and low-dose anti-thymocyte globulin conditioning regimen
International Journal of Hematology (2019)