Abstract
This phase II trial evaluates, for the first time, the safety and efficacy of bendamustine plus high-dose melphalan (HDM) as a conditioning regimen before the second autologous stem cell transplantation (ASCT) in previously untreated multiple myeloma (MM) patients. In total, 32 ASCT patients received HDM (200 mg/m2) as conditioning for the first ASCT. After 3–6 months from the first ASCT, responding patients underwent a second ASCT following bendamustine (200 mg/m2) and HDM (140 mg/m2). High-dose chemotherapy and ASCT were performed with complete neutrophil and platelet recovery in all patients. The median number of days to neutrophil and platelet engraftment was 11 (range 9–15) and 12 (range 10–19), respectively. Only one subject experienced grade 3 diarrhea; the rate of mucositis and vomiting was significantly lower with the bendamustine plus HDM regimen compared with the HDM-only regimen (81.2 vs 96.9%, P=0.025 and 78.1 vs 100%, P=0.008). Overall response rate (ORR) was 81.2% after the first transplant, and 90.6% after the second, while complete response rates were 46.8 and 62.5%, respectively (P=0.016). Actuarial 2-year PFS and OS were 79% (95% confidence interval (CI), 60–98) and 97% (95% CI, 91–100), respectively. Bendamustine+HDM is feasible as the conditioning regimen for second ASCT in MM patients. The present study may pave the way for phase III studies specifically aimed at further investigating this combination strategy. The role of this combination in MM for conditioning regimen in a first or single ASCT setting should be also investigated.
Similar content being viewed by others
Introduction
With the advent of modern therapies, as well as their integration into existing treatment approaches and the improved management of complications, the outcome of patients with multiple myeloma (MM) has dramatically improved in the past decade.1 Thanks to the unprecedented higher and deeper responses and the increasing number of treatment options, questions regarding existing treatment paradigms and optimal treatment have been raised.2 For almost 25 years, therapeutic intensification with high-dose chemotherapy (HDC) and autologous stem cell transplantation (ASCT) has been considered as the standard of care in MM patients without significant comorbidities.2, 3 Although this approach is currently being debated by some investigators in the modern therapy era,4 it still represents the standard treatment strategy;5 and the incorporation of novel agents into different phases of the transplant procedure, including induction,6, 7, 8, 9 consolidation,10, 11 and maintenance12, 13 has substantially improved outcomes.
Although many studies have been performed in the induction, consolidation and maintenance settings, few trials have been dedicated to conditioning regimens before ASCT;14, 15, 16, 17, 18, 19, 20, 21, 22 and the current standard conditioning regimen is considered high-dose melphalan (HDM).14
Bendamustine (BENDA) (Ribomustin/Levact; Mundipharma International Ltd, and Treanda; Cephalon) is a synthetic chemotherapeutic agent that combines the alkylating properties of a mustard group with the antimetabolic activity of a purine analog. It can induce responses in disease resistant to other alkylating agents via direct induction of apoptosis, inhibition of mitosis, and activation of an alternative DNA repair pathway distinct from standard alkylator mechanisms of action.23 BENDA has proven activity in both newly diagnosed and relapsed/refractory MM;24 and it has already been shown to be a feasible part of a modified BeEAM (bendamustine, etoposide, cytarabine, melphalan) ASCT conditioning regimen for non-Hodgkin lymphoma with acceptable safety and promising efficacy.25 Recently, Mark et al.19 published a phase I trial on escalating doses of BENDA added to the current standard conditioning of HDM at 200 mg/m2 in patients with MM at their first transplant. We report herein the results of a phase II trial evaluating the safety and efficacy of BENDA plus HDM as the conditioning regimen for ASCT after induction therapy in MM patients. This is the first study in transplant-eligible patients with newly diagnosed MM to use a BENDA-based conditioning regimen before the second ASCT in a tandem treatment strategy.
Patients and methods
Setting and design
This was a single-arm, prospective phase II study. Patients were recruited from three hematological centers in the South of Italy (Calabria Region); all patients were referred to the Stem Cell Transplantation Unit of the Azienda Ospedaliera BMM, Reggio Calabria (Italy) after response to induction therapy for PBSC collection and transplantation. The study was approved by the institutional review board of Azienda Ospedaliera BMM of Reggio Calabria (Italy) and was conducted according to the Declaration of Helsinki and the International Conference on Harmonisation Guidelines for Good Clinical Practice. All patients provided written informed consent before inclusion.
Patients
Inclusion criteria were as follows: transplant-eligible patients, aged 18–70 years, with de novo MM who after induction achieved a favorable response (International Myeloma Working Group (IMWG) criteria) and who presented International Staging System (ISS) stage 1–3 and World Health Organization (WHO) performance status 0–3 could be enrolled. A WHO performance of 3 was allowed only if it was caused by MM rather than a comorbid condition. Exclusion criteria were as follows: New York Heart Association class II to IV heart failure; abnormal pulmonary-function findings; systematic amyloid light-chain amyloidosis; non-secretory MM; Waldenstrom macroglobulinemia or IgM MM; history of active malignancy during the past 5 years with the exception of basal cell carcinoma or stage 0 cervical cancer. Laboratory exclusion criteria were creatinine clearance <15 mL/min; absolute neutrophil count <1.0 × 109/L and platelet count <75 × 109/L. Patients who had a refractory disease (progression or no response) to induction chemotherapy were also excluded.
Treatment
All patients received a bortezomib-based induction therapy (in association with corticosteroids with or without thalidomide). High-dose CY (3–4 g/m2) plus granulocyte CSF (G-CSF) were used to mobilize PBSCs. The minimum target dose of CD34+ cells to safely support two sequential courses of high-dose conditioning regimen was 5 × 106/kg (2.5 × 106/kg per transplant).
All patients received HDM (200 mg/m2) as conditioning regimen before the first ASCT. After 3–6 months from the first ASCT, patients who achieved a stable disease or a more favorable response (as defined below) underwent a second ASCT following BENDA (100 mg/m2 days −3 and −2) and HDM (140 mg/m2 day −1) as a conditioning regimen. No consolidation or maintenance therapies were permitted.
Supportive care
During the aplastic phase of both ASCT procedures, all patients received oral prophylaxis with ciprofloxacin at 500 mg twice-daily or levofloxacin at 500 mg/day from day 0 until neutrophil recovery, and with acyclovir at 800 mg twice-daily from day +3 post transplantation until approximately day +90. Pneumocystis jiroveci prophylaxis with trimethoprim/sulfamethoxazole (1 double-strength tablet 2 or 3 times weekly) was started after hematological recovery and was continued for 3 months. G-CSF (filgrastim or lenograstim) at 5 mcg/kg/day was started at day +5 and continued until neutrophil recovery. Red blood cell and platelet transfusions were administered in order to maintain hemoglobin levels ⩾8 g/dL and platelet counts ⩾10 × 109/L, or in case of symptomatic anemia and/or minimal mucocutaneous hemorrhagic syndrome. Patients also received i.v. hydration and electrolyte support.
Evaluations
The primary objective of this study was to evaluate: (i) treatment-related toxicity and TRM; (ii) time to neutrophil and platelet engraftment after BENDA plus HDM; and (iii) cumulative incidence of neutrophil and platelet recovery. Secondary objectives were to evaluate the complete response (CR) rate, the overall response rate (ORR; defined as the CR+very good partial response (VGPR)), PFS and OS. The evaluation of response was performed at enrollment and at day +30 and day +100 after both ASCTs. Moreover, toxicities and engraftment rates between the first and second transplants were compared.
Adverse events were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.0). TRM was defined as death from any cause other than disease progression within 100 days from transplantation. Time to neutrophil engraftment was defined as the duration between day 0 and the first of 3 consecutive days of ANC >0.5 × 109/L after transplant. Time to platelet engraftment was defined as the duration between day 0 and the first day of platelet count sustained at >20 × 109/L without any transfusion in the previous 7 days. Response and progression were reported by investigators according to revised uniform response criteria by the International Myeloma Working Group.26, 27 In particular, we considered as a CR a negative immunofixation of serum and urine, disappearance of any soft tissue plasmacytomas and <5% plasma cells in bone marrow. In patients for whom only measurable disease was by serum free light chains level, the normal free light chains ratio of 0.26–1.65 in addition to CR criteria was required. Two consecutive assessments were needed. Bone marrow biopsy and aspirate samples were collected at baseline and as needed to confirm CR. Patients with CR who lacked confirmation from bone marrow biopsy samples were downgraded to VGPR.
Statistical analysis
Data were summarized as median and range (continuous variables) or as absolute frequencies and percentages (binary variables), as appropriate. Within-patient comparisons were made by the Wilcoxon rank test (for continuous variables) and the McNemar test (binary data), as appropriate. Response rates, survival and toxicity were summarized by descriptive statistics. TRM was evaluated as cumulative incidence. PFS and OS were investigated by the Kaplan–Meier method. The response rate after BENDA plus HDM was calculated and compared with HDM (200 mg/m2) response rates. The degree of uncertainty (precision) around PFS and OS was expressed as point estimate and the corresponding 95% confidence interval (CI). Data analysis was performed using SPSS for Windows (version 20.0.0; IBM, Armonk, NY, USA).
Results
Study population
A total of 32 patients (median age 56 years; 56% males) were consecutively enrolled in the study between January 2013 and December 2014. Baseline demographic and disease characteristics are summarized in Table 1. Patients ranged in age from 40 to 66 years. Data on cytogenetic abnormalities, del(13q), t(4;14) and del(17p), detected by FISH on highly purified bone marrow plasma cells, were available for 25 patients. The isotype distribution of M-proteins reflected the typical MM population (IgG, 75.0%; IgA, 21.9%; free light chain only, 3.1%). All 32 registered patients started induction therapy and 16 (50%) received VTD (velcade, thalidomide and dexamethasone) (Table 1). All patients continued to receive CY priming and the tandem HDC because of responsive disease.
Stem cell engraftment
After the BENDA plus HDM conditioning regimen, a median of 5.0 (range 3.2–7.0) CD34+ cells × 106/kg was infused. HDC and ASCT were performed with complete neutrophil and platelet recovery in all patients. The median number of days to neutrophil and platelet engraftment was 11 (range 9–15) and 12 (range 10–19), respectively. The median number of days with ANC ⩽0.1, ⩽0.5 and ⩽1 × 109/L was 3 (range 2–8), 5 (range 3–10) and 6 (range 3–13), respectively. The median duration of hospitalization after stem cell infusion was 16 days (range 13–27). The engraftment kinetics observed for BENDA plus HDM conditioning at second transplant were similar to those reported previously with the first HDM (200 mg/m2) conditioning regimen (Table 2).
Treatment-related toxicity and TRM
Overall, the BENDA plus HDM regimen was well tolerated (Table 3). The majority of patients (n=26; 81.2%) experienced mucositis, but it was of grade 1–2 in all cases. Similarly, most patients reported nausea (n=25; 78.1%) and diarrhea (n=24; 75.0%), but only one subject experienced grade 3 diarrhea. The rate of mucositis and vomiting was significantly lower with the BENDA plus HDM regimen compared with the HDM-only regimen administered for the first ASCT (81.2 vs 96.9%, P=0.025 and 78.1 vs 100%, P=0.008). After complete hematologic recovery after the second transplant, one patient showed a skin rash after 40 days and two subjects experienced CMV infections, documented 30 days after the first transplant and 40 days after the second transplant, respectively. Both CMV infections were successfully eradicated with valacyclovir treatment (900 mg/day for 15 days).
Fever ⩾38.2 °C was reported in 15 patients (46.9%) during neutropenia. It was clinically documented in two patients (6.2%). In one case of E. coli infection was microbiogically documented. The median duration of fever was 3 days (range: 2–7).
No cases of TRM were reported. One patient died of brain hemorrhage 150 days after the second ASCT.
Response assessment
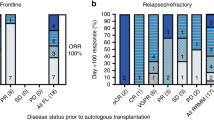
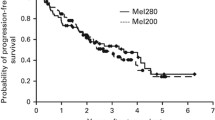
Clinical responses to treatment are shown in Figure 1. At the end of induction therapy, 25 and 37.5% of the patients had achieved a CR and a VGPR, respectively, with an ORR of 62.5%. After the first and second transplantation, the CR improved to 46.8 and 62.5%, respectively (P=0.016 and P<0.0001). ORR was 81.2% after the first transplant (P=0.031), and 90.6% after the second transplant (P=0.004). At a median follow-up of 16 months (range, 9–32) after the second ASCT, four patients (12.5%) had progressed and one (3.1%) died. The median PFS and OS were not reached. Actuarial 2-year PFS and OS were 79% (95% CI, 60–98) and 97% (95% CI, 91–100), respectively (Figures 2 and 3).
Discussion
In 1992, the IFM group published the first study where HDC combined with ASCT improved the response rate, PFS and OS of patients with MM.28 Several prospective randomized trials confirmed a benefit with HDC when compared with conventional chemotherapy,29, 30, 31, 32 and this procedure has been part of the standard of care for over two decades.33 In the 2000s, an improvement of clinical outcomes was observed with the advent of immunomodulatory drugs and proteasome inhibitors.34 The subsequent years have been characterized by studying the optimal combination of new agents, and questions regarding existing treatment paradigm and optimal treatment have been raised.
In the new era for MM treatment, transplant trials support the use of upfront ASCT in the context of novel agents.4, 6, 7, 8, 9, 29 The transplant may be single or tandem (that is, second course of HDC within 6 months of the first) and the optimal strategy that routinely incorporates a tandem transplant remains an open question.4, 35, 36 The IMWG suggests considering timely second ASCT in those patients who fail to achieve a VGPR or better after the first ASCT;37 this clinical outcome is often used in some centers as the criterion for planning the tandem procedure. Recent studies with the new induction regimens indicate that there is a role for tandem ASCT in MM in the presence of adverse cytogenetic abnormalities.38, 39 Results from an upcoming integrated analysis of four phase III European trials,40 in which one-third of patients have been randomized to a tandem ASCT procedure, could alter future transplantation algorithms.
Nowadays, there is no consensus regarding the best conditioning regimen.3, 14 HDM at a dose of 200 mg/m2 is considered to be the standard conditioning regimen.14, 17, 18, 30 However, a variety of strategies has been explored with the aim of improving the results of HDM 200 mg/m2, including dose escalation,22 addition of other agents such as busulfan, thiotepa or TBI14, 15, 17, 18, 19, 20, 21, 22 or, conversely, dose reduction as part of a tandem auto-SCT procedure,20 with overall mixed results. Further evidence is however necessary on the best conditioning regimen.
BENDA combines the alkylating activity of the mustard group with the antimetabolite activity of the purine analog structure and has activity in multiresistant cell lines that do not respond to treatment with other alkylating agents.23 Recently, Mark et al.19 conducted a phase I trial adding escalating doses of BENDA to HDM (200 mg/m2) as conditioning regimen in MM patients. In this study, a maximum tolerated dose was not achieved and the highest dose cohort of BENDA 225 mg/m2 plus HDM was expanded in order to further evaluate the safety. Overall, this combination regimen did not increase transplantation risk or toxicity, and was not associated with any TRM. Although preliminary, the efficacy results show an ORR of 80% at day +100 and a CR or improved rate of approximately 45% at 1 year after ASCT.
For the first time, in the present phase II study we evaluated the safety and feasibility of adding BENDA (200 mg/m2) to HDM (140 mg/m2) as a conditioning regimen before the second ASCT in de novo MM patients in a tandem transplant strategy. In our study, the choice of BENDA was based on the documented sensitivity of myeloma cells to the drug in the context of resistance to previous treatments;24, 41, 42 and the decision was made to explore the association between a pure alkylating agent (melphalan) with an agent (BENDA) that combines the alkylating properties of a mustard group with the antimetabolic activity of a purine analog and can induce responses in disease resistant in a distinct way from standard alkylator mechanisms of action.43
We believe that the use of a preparative regimen that combines two agents in the second ASCT could have a key role in long-term results. In this regard, when two conditioning regimens with alkylating agents were prospectively compared by a Spanish Group a higher response rate was found with busulfan/melphalan than with melphalan alone.17, 18, 44 We decided to use a fixed dose of 200 mg/m2 because of the reported cardiotoxicity in previous series at higher doses of BENDA42, 43 and to reduce the risk of synergistic toxicity between the BENDA and HDM and keeping in mind that all patients performed, in the previous 6 months, a first ASCT. Moreover, the association between BENDA at 200 mg/m2+plus HDM at 140 mg/m2 was investigated in lymphoma patients in the context of BeEAM chemotherapy regimen with an extremely low-toxicity profile.25 However, a formal phase I study is recommended to address the maximum tolerated dose of bendamustine with fixed-dose melphalan. Overall, our conditioning regimen showed a favorable tolerability profile, and no cases of TRM were reported. Although most patients experienced commonly-occurring adverse events such as mucositis, vomiting and diarrhea, these were mild in severity in almost all cases. Interestingly, a lower incidence of mucositis and vomiting was reported as compared with the first ASCT. Although this study was not specifically aimed at comparing tolerability between the former and the latter conditioning regimen, one may speculate that the use of a lower dose of HDM (140 mg/m2 instead of 200 mg/m2) combined with BENDA, a molecule with a different mechanism of action, could cause less adverse events. Importantly, stem cell engraftment was successful in all patients, and the BENDA plus HDM regimen was associated with an overall short hospital stay (16 days), with some potential advantages from a cost-saving perspective.
The evaluation of efficacy was a secondary end point of our study; and therefore, no definite conclusions on this issue can be drawn also due to the limited number of patients enrolled. Overall, the addition of BENDA to HDM determined a high incidence of response, with an ORR of about 91% and more than 60% of patients achieving CR; these rates, although not statistical significantly probably due to the small simple size of the study, are higher than those obtained after the first transplant, lending some further support to the feasibility and soundness of the combination regimen.
It must be acknowledged that our study has several limitations, mainly related to the limited number of recruited subjects and the absence of a true control arm; these issues should be taken into account when evaluating the safety, tolerability and efficacy of the new conditioning regimen. Indeed, although it may be appropriate to use a different conditioning regimen in patients not attaining a CR, it would probably not be appropriate to change the conditioning regimen in patients attaining a CR after the first transplant, as these patients have proven to be very sensitive to HDM. The capacity of the second, different, conditioning regimen to induce CR in patients attaining a suboptimal response after the first procedure is probably crucial to the efficacy of any strategy based on tandem transplants.
In conclusion, BENDA plus HDM is feasible as the conditioning regimen for second ASCT in patients with MM. The present study, despite its limitations, may pave the way for larger phase III studies specifically aimed at investigating safety, therapeutic activity and also the cost/efficacy ratio of this combination strategy and can give a contribute in the continuous debate about new conditioning regimen for ASCT as double alkylating agents, single alkylating agent or new alkylants that could include new formulation of HDM or adding new drugs different from chemotherapy. The role of this combination in MM for conditioning regimen in a first or single ASCT setting should be also investigated.
References
Röllig C, Knop S, Bornhäuser M . Multiple myeloma. Lancet 2015; 385: 2197–2208.
Ludwig H, Sonneveld P, Davies F, Bladé J, Boccadoro M, Cavo M et al. European perspective on multiple myeloma treatment strategies in 2014. Oncologist 2014; 19: 829–844.
Shah N, Callander N, Ganguly S, Gul Z, Hamadani M, Costa L et al. Hematopoietic stem cell transplantation for multiple myeloma: guidelines from the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant 2015; 21: 1155–1166.
Martino M, Morabito F . Autologous stem cell transplantation in multiple myeloma is not dead but alive and well. Expert Opin Biol Ther 2015; 15: 149–154.
van Rhee F, Giralt S, Barlogie B . The future of autologous stem cell transplantation in myeloma. Blood 2014; 124: 328–333.
Cavo M, Tacchetti P, Patriarca F, Petrucci MT, Pantani L, Galli M et alGIMEMA Italian Myeloma Network. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet 2010; 376: 2075–2085.
Rosiñol L, Oriol A, Teruel AI, Hernández D, López-Jiménez J, de la Rubia J et alProgramapara el Estudio y la Terapéutica de las Hemopatía Malignas/Grupo Español de Mieloma (PETHEMA/GEM) group. Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation therapy in multiple myeloma: a randomized phase 3 PETHEMA/GEM study. Blood 2012; 120: 1589–1596.
Palumbo A, Cavallo F, Gay F, Di Raimondo F, Ben Yehuda D, Petrucci MT et al. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med 2014; 371: 895–905.
Jakubowiak AJ, Dytfeld D, Griffith KA, Lebovic D, Vesole DH, Jagannath S et al. A phase 1/2 study of carfilzomib in combination with lenalidomide and low-dose dexamethasone as a frontline treatment for multiple myeloma. Blood 2012; 120: 1801–1809.
Cavo M, Pantani L, Petrucci MT, Patriarca F, Zamagni E, Donnarumma D et alGIMEMA (Gruppo Italiano Malattie Ematologiche dell'Adulto) Italian Myeloma Network. Bortezomib-thalidomide-dexamethasone is superior to thalidomide-dexamethasone as consolidation therapy after autologous hematopoietic stem cell transplantation in patients with newly diagnosed multiple myeloma. Blood 2012; 120: 9–19.
Roussel M, Lauwers-Cances V, Robillard N, Hulin C, Leleu X, Benboubker L et al. Front-line transplantation program with lenalidomide, bortezomib, and dexamethasone combination as induction and consolidation followed by lenalidomide maintenance in patients with multiple myeloma: a phase II study by the Intergroupe Francophone du Myélome. J Clin Oncol 2014; 32: 2712–2717.
McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1770–1781.
Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T et alIFM Investigators. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1782–1791.
Martino M, Olivieri A, Offidani M, Vigna E, Moscato T, Fedele R et al. Addressing the questions of tomorrow: melphalan and new combinations as conditioning regimens before autologous hematopoietic progenitor cell transplantation in multiple myeloma. Expert Opin Investig Drugs 2013; 22: 619–634.
Alegre A, Lamana M, Arranz R, Fernández-Villalta MJ, Tomás JF, Figuera et al. Busulfan and melphalan as conditioning regimen for autologous peripheral blood stem cell transplantation in multiple myeloma. Br J Haematol 1995; 91: 380–386.
Moreau P, Facon T, Attal M, Hulin C, Michallet M, Maloisel F et alIntergroupe Francophone du Myélome. Comparison of 200 mg/m2 melphalan and 8 Gy total body irradiation plus 140 mg/m2 melphalan as conditioning regimens for peripheral blood stem cell transplantation in patients with newly diagnosed multiple myeloma: final analysis of the Intergroupe Francophone du Myélome 9502 randomized trial. Blood 2002; 99: 731–735.
Lahuerta JJ, Mateos MV, Martínez-López J, Grande C, de la Rubia J, Rosiñol L et alGrupo Español de MM and Programa para el Estudio de la Terapéutica en Hemopatía Maligna Cooperative Study Groups. Busulfan 12 mg/kg plus melphalan 140 mg/m2 versus melphalan 200 mg/m2 as conditioning regimens for autologous transplantation in newly diagnosed multiple myeloma patients included in the PETHEMA/GEM2000 study. Haematologica 2010; 95: 1913–1920.
Blanes M, Lahuerta JJ, González JD, Ribas P, Solano C, Alegre et al. Intravenous busulfan and melphalan as a conditioning regimen for autologous stem cell transplantation in patients with newly diagnosed multiple myeloma: a matched comparison to a melphalan-only approach. Biol Blood Marrow Transplant 2013; 19: 69–74.
Mark TM, Reid W, Niesvizky R, Gergis U, Pearse R, Mayer S et al. A phase 1 study of bendamustine and melphalan conditioning for autologous stem cell transplantation in multiple myeloma. Biol Blood Marrow Transplant 2013; 19: 831–837.
Musso M, Messina G, Marcacci G, Crescimanno A, Console G, Donnarumma D et al. High-dose melphalan plus thiotepa as conditioning regimen before second autologous stem cell transplantation for ‘de novo’ multiple myeloma patients: a phase II study. Biol Blood Marrow Transplant 2015; 21: 1932–1938.
Roussel M, Moreau P, Huynh A, Mary JY, Danho C, Caillot D et alIntergroupe Francophone du Myélome (IFM). Bortezomib and high-dose melphalan as conditioning regimen before autologous stem cell transplantation in patients with de novo multiple myeloma: a phase 2 study of the Intergroupe Francophone du Myelome (IFM). Blood 2010; 115: 32–37.
Bensinger WI, Becker PS, Gooley TA, Chauncey TR, Maloney DG, Gopal AK et al. A randomized study of melphalan 200 mg/m2 vs 280 mg/m2 as a preparative regimen for patients with multiple myeloma undergoing auto-SCT. Bone Marrow Transplant 2015; 51: 67–71.
Leoni LM, Bailey B, Reifert J, Bendall HH, Zeller RW, Corbeil J et al. Bendamustine (Treanda) displaysa distinct pattern of cytotoxicity and unique mechanistic features compared with other alkylating agents. Clin Cancer Res 2008; 14: 309–317.
Palumbo A, Offidani M, Patriarca F, Petrucci MT, Cavo M . Bendamustine for the treatment of multiple myeloma in first-line and relapsed-refractory settings: a review of clinical trial data. Leuk Lymphoma 2015; 56: 559–6.
Visani G, Malerba L, Stefani PM, Capria S, Galieni P, Gaudio F et al. BeEAM (bendamustine, etoposide, cytarabine, melphalan) before autologous stem celltransplantation is safe and effective for resistant/relapsed lymphoma patients. Blood 2011; 118: 3419–3425.
Palumbo A, Rajkumar SV, San Miguel JF, Larocca A, Niesvizky R, Morgan G et al. International Myeloma Working Group consensus statement for the management, treatment, and supportive care of patients with myeloma not eligible for standard autologous stem-cell transplantation. J Clin Oncol 2014; 32: 587–600.
Durie BG, Harousseau JL, Miguel JS, Bladé J, Barlogie B, Anderson K et al. International uniform response criteria for multiple myeloma. Leukemia 2006; 20: 1467–1473.
Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Français du Myélome. N Engl J Med 1996; 335: 91–97.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883.
Bladé J, Rosiñol L, Sureda A, Ribera JM, Díaz-Mediavilla J, García-Laraña J et al. High-dose therapy intensification compared with continued standard chemotherapy in multiple myeloma patients responding to the initial chemotherapy: long-term results from a prospective randomized trial from the Spanish cooperative group PETHEMA. Blood 2005; 106: 3755–3759.
Fermand JP, Katsahian S, Divine M, Leblond V, Dreyfus F, Macro M et al. High-dose therapy and autologous blood stem-cell transplantation compared with conventional treatment in myeloma patients aged 55 to 65 years: long-term results of a randomized control trial from the Group Myelome-Autogreffe. J Clin Oncol 2005; 23: 9227–9233.
Barlogie B, Kyle RA, Anderson KC, Greipp PR, Lazarus HM, Hurd DD et al. Standard chemotherapy compared with high-dose chemo radiotherapy for multiple myeloma: final results of a phase III US Intergroup Trial S9321. J Clin Oncol 2006; 24: 929–936.
Passweg JR, Baldomero H, Bader P, Bonini C, Cesaro S, Dreger P et alEuropean Society for Blood and Marrow Transplantation (EBMT). Hematopoietic SCT in Europe 2013: recent trends in the use of alternative donors showing more haploidentical donors but fewer cord blood transplants. Bone Marrow Transplant 2015; 50: 476–482.
Bergsagel PL . Where we were, where we are, where we are going: progress in multiple myeloma. Am Soc Clin Oncol Educ Book 2014, 199–203.
Martino M, Montanari M, Ferrara F, Ciceri F, Scortechini I, Palmieri S et alGruppo Italiano per437 il Trapianto di Midollo Osseo, Cellule Staminali Emopoietiche e Terapia Cellulare (GITMO) – Sezione Trapianto Autologo. Very low rate of readmission after an early discharge outpatient model for autografting in multiple myeloma patients: an Italian multicenter retrospective study. Biol Blood Marrow Transplant 2014; 20: 1026–1032.
Attal M, Harousseau JL, Facon T, Guilhot F, Doyen C, Fuzibet JG et alInterGroupe Francophone du Myélome. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med 2003; 349: 2495–2502.
Cavo M, Rajkumar SV, Palumbo A, Moreau P, Orlowski R, Bladé J et alInternational Myeloma Working Group. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood 2011; 117: 6063–6073.
Rosiñol L, Oriol A, Teruel AI, Hernández D, López-Jiménez J, de la Rubia J et al. Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation therapy in multiple myeloma: a randomized phase 3 PETHEMA/GEM study. Blood 2012; 120: 1589–1596.
Neben K, Lokhorst HM, Jauch A, Bertsch U, Hielscher T, van der Holt B et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood 2012; 119: 940–948.
Cavo M, Salwender H, Rosinol L, Moreau P, Petrucci MT, Blau IW et al. Double vs single autologous stem cell transplantation after bortezomib-based induction regimens for multiple myeloma: an integrated analysis of patient-level data from phase III European studies. Blood (ASH Annual Meeting Abstracts) Blood 2013; 122 (21): 767.
Cavo M, Tosi P, Zamagni E, Cellini C, Tacchetti P, Patriarca F et al. Prospective, randomized study of single compared with double autologous stem-cell transplantation for multiple myeloma: Bologna 96 clinical study. J Clin Oncol 2007; 25: 2434–2441.
Rasschaert M, Schrijvers D, Van den Brande J, Dyck J, Bosmans J, Merkle K et al. A phase I study of bendamustine hydrochloride administered day 1+2 every 3 weeks in patients with solid tumours. Br J Cancer 2007; 96: 1692–1698.
Rasschaert M, Schrijvers D, Van den Brande J, Dyck J, Bosmans J, Merkle K et al. A phase I study of bendamustine hydrochloride administered once every 3 weeks in patients with solid tumors. Anticancer Drugs 2007; 18: 587–595.
Lahuerta JJ, Martinez-Lopez J, Grande C, Bladé J, de la Serna J, Alegre et al. Conditioning regimens in autologous stem cell transplantation for multiple myeloma: a comparative study of efficacy and toxicity from the Spanish Registry for Transplantation in Multiple Myeloma. Br J Haematol 2000; 109: 138–147.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
Study concepts by MM, GM and FM. Data acquisition by MM, GM, IDV, GC, MG and SM. Quality control of data and algorithms and statistical analysis by MM and GT. Data analysis and interpretation by MM, GT and FM. Statistical analysis by MM and GT. Manuscript preparation by MM, AGR and FM. Manuscript editing by MM, GT, AGR and FM. Manuscript review by MM, GT, GM, IDV, GC, AGR, MG, SM and FM. Editorial assistance for the preparation of this manuscript was provided by Luca Giacomelli, PhD, on behalf of Content Ed Net; this assistance was funded by Mundipharma.
Rights and permissions
About this article
Cite this article
Martino, M., Tripepi, G., Messina, G. et al. A phase II, single-arm, prospective study of bendamustine plus melphalan conditioning for second autologous stem cell transplantation in de novo multiple myeloma patients through a tandem transplant strategy. Bone Marrow Transplant 51, 1197–1203 (2016). https://doi.org/10.1038/bmt.2016.94
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.94
- Springer Nature Limited
This article is cited by
-
Bridging advanced myeloma patients to subsequent treatments and clinical trials with classical chemotherapy and stem cell support
Bone Marrow Transplantation (2023)
-
Effectiveness of biosimilar pegfilgrastim in patients with multiple myeloma after high-dose melphalan and autologous stem cell transplantation
Annals of Hematology (2023)
-
Adding bendamustine to melphalan before ASCT improves CR rate in myeloma vs. melphalan alone: A randomized phase-2 trial
Bone Marrow Transplantation (2022)
-
Tandem autologous hematopoietic cell transplantation with sequential use of total marrow irradiation and high-dose melphalan in multiple myeloma
Bone Marrow Transplantation (2021)
-
High incidence of reversible renal toxicity of dose-intensified bendamustine-based high-dose chemotherapy in lymphoma and myeloma patients
Bone Marrow Transplantation (2019)