Abstract
Purpose
The goal of surgical residency is to produce technically competent surgeons who can safely operate autonomously. This study aimed to explore residents’ perception of intraoperative autonomy across post-graduate years (PGY).
Methods
General surgery residents at a single academic institution were invited to participate in focus groups divided by PGY to explore their opinions on operative autonomy. Focus groups were audio recorded, transcribed, and analyzed using constant comparative technique. Thematic analysis was performed using an inductive approach.
Results
Thirty-nine residents participated in five focus groups. Five themes emerged from the data. Residents distinguished between autonomy of thought representing graduated decision-making and autonomy of action representing technical maneuvers in the operating room. Residents vocalized a respect for the balance of autonomy and patient safety and stated a desire to have clear expectations to minimize the impact of external factors on autonomy.
Conclusions
Residents differentiated autonomy as a parallel of autonomy of thought and autonomy of action and were empathetic to the responsibility of faculty to balance patient safety and autonomy. Surgical educators can improve resident autonomy by clearly managing expectations and minimizing external factors negatively affecting intraoperative autonomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The purpose of general surgery residency is to develop technically competent surgeons who can operate safely and independently upon completion of training. With the implementation of duty hour restrictions and regulations requiring more direct oversight of residents, there has been a persistent perception among practicing surgeons that graduating trainees are less prepared to perform at this level of independence [1,2,3,4,5].
It has been hypothesized that one cause for this failure to meet expectations is due to inadequate autonomy granted to residents during training. Several studies examining intraoperative autonomy and entrustment have shown that residents are consistently receiving lower levels of autonomy than expected [1, 6]. Furthermore, residents frequently report receiving less autonomy in a case than faculty perceive they are giving [7].
Several survey-based studies have been performed in an attempt to determine factors contributing to faculty decisions pertaining to the granting of resident autonomy. These factors include but are not limited to a resident’s observed clinical skill, patient safety, medicolegal considerations, or a desire to expedite case completion [8, 9]. While these studies have examined the perspectives of attendings with regard to autonomy provision, there remains a paucity of data relating to resident perspectives. Therefore, the objective of this study was to explore resident perceptions of operative autonomy across training years to better characterize resident perceptions of operative autonomy.
Methods
Participants
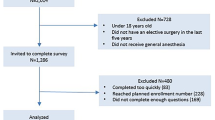
Categorical general surgery residents at a single large academic institution were invited to participate in focus groups from June to August of 2021. Participants were separated based on post-graduate year (PGY), with a dedicated focus group session held for each of the five PGY classes. This was done to maximize participants’ comfort in sharing their viewpoints. Resident recruitment was achieved through email, and participation was voluntary. The focus group sessions were held during a protected resident education hour. The training paradigm of the participants involves rotating at several large teaching hospitals, including a county hospital, several university-affiliated hospitals, and a VA hospital. The study was determined to be exempt from the Institutional Review Board and conducted in accordance with institutional ethical standards.
Data collection
Focus group facilitator guide questions were developed by two of the authors (DLD and ATC and piloted with a multi-disciplinary surgical education research group, which included surgical residents, education researchers, and surgeon faculty with expertise in education. Revisions to the questions were made based on feedback from the group.
Focus group sessions were held in-person and led by two of the authors (DLD and ATC) who received formal training in qualitative methods and focus group facilitation. The facilitators were general surgery residents completing dedicated surgical education research fellowships. Bias of the facilitators was minimized through the close following of the facilitator guide created by the multi-disciplinary research group. Study participants were oriented to the aims of the study and informed that the sessions would be recorded and transcribed, with all data de-identified to maintain confidentiality. Verbal consent from the focus group participants was obtained prior to initiating recording. The sessions were recorded using ZOOM™ (Zoom Video Communications, Inc, San Jose, CA) and transcribed.
Data analysis
The focus group recordings underwent transcript-based analysis. Of note, the transcript was corrected for any grammar or syntax to improve readability and ensure anonymity. Two focus group transcriptions were initially coded by a single author. Primary codes were condensed in a collaborative fashion between DLD and ATC into secondary codes and all five transcripts were coded by a single author using this consensus codebook. Codes were grouped into themes by DLD and ATC through an iterative process. Inductive thematic analysis was employed. Investigator triangulation was used, and themes were refined through several working group sessions involving all of the authors.
Results
In total, 39 categorical general surgery residents participated in five focus groups, representing an 80% overall participation rate. Nineteen of the participants were female (48.7%). The PGY5 class had 89% participation, the PGY4 class had 60% participation, the PGY3 class had 80% participation, the PGY2 class had 100% participation and the PGY1 class had 73% participation. Residents missing from the groups included those who were on scheduled vacations and those who were excused due to duty hour regulations relating to night float service rotations. None of the residents withdrew from participation upon initiation of the focus group sessions. Focus group sessions ranged from 38 to 63 min in length. Five themes emerged from the data. Representative quotes for the themes can be found in Table 1.
Theme 1: autonomy of thought
The first two themes differentiated autonomy as a parallel of autonomy of thought and autonomy of action. Autonomy of thought represented the graduated decision-making that takes place during any given operation, whereas autonomy of action referred to technically completing the various components of the case.
"There’s a very big difference between learning the steps of a case and deciding which steps to do." (PGY1)
Junior residents recognized autonomy of thought as a means to build confidence through simple decisions, such as deciding how to drape the patient or which instrument to use. Senior residents noted autonomy of thought to be deciding how to approach a case or mitigate divergences in operative plans; they highlighted autonomy of thought as a critical part of transitioning to independent practice. Residents noted that while autonomy of action is what autonomy in the literature is generally referring to, autonomy of thought is equally important when a resident reflects on the amount of autonomy they receive during a case, as this form of autonomy is crucial to their transition to independent practice. Residents in our study, particularly chiefs, were astutely aware of when they were being granted autonomy of thought versus when they were simply functioning as a technician. They expressed that autonomy of thought and open communication made them feel more like a colleague during a case and resulted in a greater sense of patient ownership.
Theme 2: autonomy of action
While the residents revealed the importance of autonomy of thought, they also emphasized autonomy of action as critical to developing one’s own technical abilities.
"It doesn't matter how phenomenal they are at teaching if they're not letting me practice [the technique]. At some point we need to be practicing. They're not only teaching you how it should be done, they're teaching you how to [physically] do it." (PGY3)
“If you're throwing a stitch in the portal vein and it pulls through, instead of just doing it themselves, they just hold suction. To be able to fix something you broke builds confidence." (PGY5)
Not only was autonomy of action critical to the development of necessary technical abilities, but it was also crucial to the development of resident confidence in being able to handle unforeseen complications. Building this confidence in higher stress situations was particularly important to chief residents who noted autonomy of action in routine parts of cases was typically granted to them, but autonomy of action when things were not going according to plan was often rescinded.
Theme 3: autonomy in the context of patient safety
The third theme identified from the data was a recognition of the importance of patient safety in autonomy determinations. Residents expressed an understanding that the attending’s primary role was to get a patient safely through an operation, even if this means sacrificing resident autonomy of action.
"Autonomy depends directly on the attending's ability to risk stratify patients and certain decisions. The attending should be there so you don't mess up, they should be able to fix your mistakes. They should be there to provide a safe environment for the patient to get better." (PGY3)
They suggested that engaging a resident’s autonomy of thought by asking them questions about decision-making portions of the case (e.g. where to divide a structure for an oncologic resection, what type of device to use for a particular step) could help bridge the autonomy gap that can occur due to the attendings foremost dedication to patient safety.
Theme 4: external factors influencing autonomy
The fourth theme encompassed the impact external factors have on resident operative autonomy. These factors included time pressures, a resident’s prior experience, particularly challenging technical components of an operation, and the character compatibility between the resident and the attending.
“I've had attendings ask, 'Have you done this?' And I say no, because I haven't, and they're like, 'Well not this time then, next time.'" (PGY1)
Residents expressed a desire for these external factors to be minimized as they most often negatively impact resident autonomy. For junior residents, mitigating time constraints is vital to allowing them the opportunity to try something new for the first time. The longer a resident is deprived of the opportunity to try something for the first time, the greater the gap in proficiency expectations in senior years of training.
Theme 5: importance of setting autonomy expectations
The fifth theme, setting expectations, was noted to be of utmost importance to residents, particularly in the later years of training. Residents were most frustrated when autonomy provision did not meet their expectations.
"The worst type of teacher, I think, is the one who lets you lead for the noncritical parts of the case but then takes over during the critical portions, and then tries to convince you that you did the case. It's almost insulting to the resident's level- like the attending thinks the chief is dumb enough to believe they did a case because the attending says so, when in actuality they did none of it." (PGY5)
While residents were frustrated when autonomy provision did not meet their expectations, they appreciated when faculty were up front and honest about how much they were going to be able to do in a case, even if that meant less autonomy of action.
"Some people don't like operating with Dr. X because she's new and doesn't give a lot of autonomy, but at least she is very explicit, 'I am a new faculty, I am just not comfortable yet with this.'" (PGY3)
Managing expectations through a pre-brief discussion of the autonomy plan is one practical way residents suggested attendings could ameliorate some of the disconnect that occurs between faculty and resident autonomy expectations.
Discussion
Surgical resident operative autonomy is a critical part of training technically competent and safe surgeons. This study outlines resident perspectives of intraoperative autonomy and identifies a distinction in autonomy of thought from autonomy of action. Residents acknowledged the challenge faculty face in balancing patient safety and external pressures in the context of granting residents operative autonomy. They highlighted the importance of setting autonomy expectations before a case.
This study highlights the importance of autonomy of thought from the resident perspective, which is well-supported in the literature. In a study by Cassidy et al., residents alluded to the concept of autonomy of thought when describing low autonomy as the absence of decision-making [10]. Similar to our resident participants, they described distant supervision over decision-making throughout a case to be pivotal to transitioning from training to independent practice. Hill and colleagues noted several facilitators and barriers to resident decision-making in the operating room [11]. While residents in their study endorsed maintaining an open dialog as key to facilitating autonomy of thought, they recognized case complexity and time pressures as barriers to not only autonomy of thought, but also autonomy of action. Nonetheless, open dialog and consistent engagement of autonomy of thought could serve as the bridge between an attending’s utmost duty to patient safety and the equipoise of resident autonomy of action.
The distinction of autonomy as a paradigm of thought and action could also provide an explanation for the high rate of discrepancy in resident perception of autonomy received compared to faculty perception of autonomy granted. The Zwisch scale [12] is one of the most studied tools for assessing autonomy, particularly in the context of the SIMPL app. It delineates the progression of autonomy from show and tell (no autonomy), to active and passive help from the attending, and concludes with supervision only where the attending is only present to ensure patient safety. On review of over 7000 trainee-faculty performance assessments using the Zwisch autonomy scale, residents and faculty performance ratings were discrepant almost half of the time, with 80% of the discrepancies involving residents rating themselves lower than faculty [7]. This finding has also been appreciated, particularly for chief residents, in several smaller scale, single institution studies [13, 14]. This divergence in autonomy perceptions will need to be addressed as programs more widely adopt this autonomy scale for intraoperative performance assessment, and we postulate this could also be contributing to the perception among practicing surgeons that recent graduates are less prepared to practice independently.
Foundational studies outlining the validity evidence for the Zwisch scale as a tool to measure resident operative autonomy incorporated faculty and observer raters but did not include resident self-rating [15]. With the growing evidence highlighting the discrepancy between faculty and resident autonomy scoring, questions can be raised around the interrater reliability of the Zwisch scale and, theoretically, the validity evidence supporting its internal structure. The largest study highlighting the discrepancy between faculty and resident autonomy ratings implied the gap was due to trainee underestimation of the amount of autonomy they were provided [7]. Kendrick and colleagues suggested the divergence, particularly with chief residents, was due to the psychological learning theory that postulates more skilled learners underrate performance with increased task complexity [7]. However, initial studies evaluating faculty and resident expectations for autonomy provision according to the Zwisch scale found that actual intraoperative autonomy provision rated by faculty for the most commonly performed general surgery cases was discernably lower than both resident and faculty expectations, suggesting that the problem lies in the actual autonomy provided [16]. In light of our results, we postulate that the discrepancy is not due to an over or underestimation of autonomy provision, but rather an incomplete assessment of autonomy, raising additional concerns for construct underrepresentation in the Zwisch scale. By integrating both autonomy of thought and autonomy of action into autonomy provision and assessment, faculty and residents may be able to ameliorate the autonomy gap.
The theme of resident operative autonomy and its delicate interplay with patient safety is supported by the literature. The general public perceives surgical resident autonomy as being associated with an increase in complications, leading to a resistance in patients to allow a resident to perform any portion of a procedure [17]. However, multiple studies evaluating patient outcomes for cases matched according to risk stratification and performed autonomously by residents have demonstrated no discernible difference in morbidity or mortality compared to those performed by attending surgeons alone or attending-resident dyads [18, 19]. Fieber and colleagues demonstrated that when residents perceived greater autonomy in a case, patient outcomes, as measured by death or serious morbidity and 30-day readmission rates, were discernibly improved [20]. These data demonstrate that enhancing a resident’s autonomy of action and thought is not only pivotal to training technically competent surgeons who are ready for autonomous practice, but it is also safe.
While residents in our focus groups noted the importance of having an attending available to ensure the safety of the patient, they expressed frustration when limitations to autonomy were not due to patient safety issues, but rather external factors. These external factors described by our participants aligned with the literature outlining different external factors impacting resident autonomy, including time constraints [8, 21], prior experience, character compatibility and attendings’ comfort level [22]. Residents during the focus groups also emphasized the value of feeling like a colleague during a case and expressed a greater sense of patient ownership when open communication and shared decision-making were maintained. Upon review of resident evaluations of teaching faculty, Rivard et al. noted that attendings who promoted resident autonomy utilized preoperative goal setting, fostered a collaborative operating room environment and committed to providing postoperative feedback [23].
In the context of our focus group results, one potential framework faculty and residents could employ to enhance resident autonomy and overall learning experience is the BID model: Briefing, Intraoperative teaching, and Debriefing [24]. The first component, briefing, would involve a short preoperative interaction in which the faculty gages the resident’s autonomy goals and establishes an autonomy plan. The second step, intraoperative teaching, would be focused on the autonomy goals established during the briefing. This step is where the interplay of autonomy of thought and action is critical. When a given moment in a case does not facilitate the previously established autonomy plan due to patient safety concerns, faculty should engage the resident’s autonomy of thought through open dialog. The final step, debriefing, can take place either while closing or shortly after case completion and should involve a mutual dialog reflecting on autonomy provision, whether it was adequate, and what the resident and faculty can do moving forward to enhance resident operative autonomy. Utilizing the BID framework in the context of resident autonomy could help bridge the gap between resident and faculty perceptions, safely expedite increased resident operative autonomy earlier in training, and ameliorate several concerns regarding readiness for independent practice.
One limitation to the study is that the focus groups were comprised of residents from a single, large academic institution so this reflects the experience of one particular training program. Future work should encompass focus groups comprised of residents from different training programs (e.g. community, hybrid, small academic). Focus groups involving fellows should also be studied to evaluate if our findings persist among more advanced trainees. Another potential limitation is that both focus group facilitators were surgical residents, potentially introducing biases based on their personal experience, however, this may also have allowed the participants to be more comfortable discussing their experiences with their peers instead of their superiors.
In conclusion, residents brought to light the important distinction of autonomy of thought from autonomy of action and acknowledged the ever-present challenge attendings face in balancing patient safety and resident autonomy. Surgeon educators can improve a resident’s autonomy perception and overall learning experience by minimizing the impact external factors have on intraoperative autonomy allocation and clearly managing resident expectations. Faculty can optimize resident autonomy by employing the BID framework to (1) establish autonomy expectations during the preoperative Brief, (2) engage a resident’s autonomy of thought during Intraoperative teaching portions of a case where allowing the resident autonomy of action could potentially compromise patient safety, and (3) Debrief autonomy provision after the case to enhance opportunities for resident autonomy moving forward.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
George BC, et al. Readiness of US General Surgery Residents for Independent Practice. Ann Surg. 2017;266(4):582–94.
Bell RH Jr. Why Johnny cannot operate. Surgery. 2009;146(4):533–42.
Lewis FR, Klingensmith ME. Issues in general surgery residency training–2012. Ann Surg. 2012;256(4):553–9.
Elfenbein DM. Confidence crisis among general surgery residents: a systematic review and qualitative discourse analysis. JAMA Surg. 2016;151(12):1166–75.
Napolitano LM, et al. Are general surgery residents ready to practice? A survey of the American College of Surgeons Board of Governors and Young Fellows Association. J Am Coll Surg. 2014;218(5):1063-1072.e31.
Meyerson SL, et al. Resident autonomy in the operating room: expectations versus reality. Ann Thorac Surg. 2017;104(3):1062–8.
Kendrick DE, et al. The reliability of resident self-evaluation of operative performance. Am J Surg. 2021;222(2):341–6.
Teman NR, et al. Entrustment of general surgery residents in the operating room: factors contributing to provision of resident autonomy. J Am Coll Surg. 2014;219(4):778–87.
Thiels CA, et al. Medical malpractice lawsuits involving surgical residents. JAMA Surg. 2018;153(1):8–13.
Cassidy DJ, et al. Surgical autonomy: a resident perspective and the balance of teacher development with operative independence. Am J Surg. 2021;221(2):336–44.
Hill KA, et al. How can surgeons facilitate resident intraoperative decision-making? Am J Surg. 2017;214(4):583–8.
DaRosa DA, et al. A theory-based model for teaching and assessing residents in the operating room. J Surg Educ. 2013;70(1):24–30.
Young KA, et al. Characterizing the relationship between surgical resident and faculty perceptions of autonomy in the operating room. J Surg Educ. 2017;74(6):e31–8.
Senders ZJ, et al. Factors influencing the entrustment of resident operative autonomy: comparing perceptions of general surgery residents and attending surgeons. J Grad Med Educ. 2021;13(5):675–81.
George BC, et al. Reliability, validity, and feasibility of the Zwisch scale for the assessment of intraoperative performance. J Surg Educ. 2014;71(6):e90–6.
Meyerson SL, et al. Defining the autonomy gap: when expectations do not meet reality in the operating room. J Surg Educ. 2014;71(6):e64-72.
Dickinson KJ, et al. Public perception of general surgery resident autonomy and supervision. j Am Coll Surg. 2021;232(1):8-15.e1.
Oliver JB, et al. Association between operative autonomy of surgical residents and patient outcomes. JAMA Surg. 2022;157(3):211–9.
Siam B, et al. Comparison of appendectomy outcomes between senior general surgeons and general surgery residents. JAMA Surg. 2017;152(7):679–85.
Fieber JH, et al. Does perceived resident operative autonomy impact patient outcomes? J Surg Educ. 2019;76(6):e182–8.
Bohnen JD, Chang DC, George BC. Operating room times for teaching and nonteaching cases are converging: less time for learning? J Surg Educ. 2021;78(1):148–59.
Park J, et al. Improving the intraoperative educational experience: understanding the role of confidence in the resident-attending relationship. J Surg Educ. 2019;76(5):1187–99.
Rivard SJ, et al. Resident perceptions of faculty behaviors promoting learner operative skills and autonomy. J Surg Educ. 2022;79(2):431–40.
Roberts NK, et al. The briefing, intraoperative teaching, debriefing model for teaching in the operating room. J Am Coll Surg. 2009;208(2):299–303.
Acknowledgements
This project was made possible by Indiana University Health and the Indiana Clinical and Translational Sciences Institute, funded in part by grant #ULITR002529 from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award and The Advanced in Medicine (AIM) grant from Cook Medical. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Cook Medical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts to disclose relevant to this work.
Appendix A: Focus Group Facilitator Guide
Appendix A: Focus Group Facilitator Guide
Intro:
Thank you everyone for taking the time to meet with us today. The goal of this session is to explore resident perspectives of intraoperative autonomy. This may mean different things to different people, so I would like to hear from everybody. It’s ok if you disagree or have different opinions than someone else in the group. We all have different personalities, learning styles, and histories that we bring to our experiences, so the more perspectives I can hear from, the more comprehensive our knowledge will be.
Questions:
-
1.
Describe what intraoperative autonomy means to you?
-
a.
Describe what it looks like.
-
b.
How does autonomy impact your intraoperative learning experience?
-
c.
How did you feel while working with someone who optimized autonomy?
-
a.
-
2.
When is intraoperative autonomy appropriate vs. inappropriate?
-
a.
What makes that autonomy provision appropriate vs. inappropriate?
-
b.
What could an attending do to recognize and/or mitigate inappropriate autonomy provision?
-
a.
-
3.
How can an attending optimize intraoperative autonomy for residents?
-
a.
Describe what optimized autonomy looks like to you.
-
b.
Does this look different based on a resident’s PGY?
-
a.
-
4.
How can a resident optimize intraoperative autonomy received?
-
a.
What external factors facilitate autonomy?
-
b.
What have you done to seek out more autonomy in a case?
-
c.
How often did you discuss specific goals for the case with the attending before you started?
-
a.
-
5.
Is there anything else about operative autonomy from the resident perspective that you feel has not yet been covered?
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Doster, D.L., Collings, A.T., Thomas, C. et al. Balancing autonomy of thought and action in the context of patient safety: resident perspectives on intraoperative autonomy. Global Surg Educ 1, 62 (2022). https://doi.org/10.1007/s44186-022-00039-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-022-00039-8