Abstract
Biomimetic nanoparticles (BioM NPs) feature functionalization that imitates the biological surroundings, endowing them with biological structure and functioning. BioM NPs could be covered with biologically sourced materials and could contain synthetic antigen-presenting cells and structures. Whenever used in cancer diagnostics, BioM NPs outperform standard medications and comparable non-BioM NPs, particularly regarding circulation time, tissue penetration, delivery, and toxicity. The particles achieved extraordinary results by using cell material for BioM NPs, which avoids difficult bottom-up synthetic approaches that aim to emulate such intricate and diverse biological components. One area of this rapidly developing research that has gotten a lot of interest is the use of BioM NPs in the treatment of different cancers. However, to the best of our knowledge, no published study has primarily analysed current improvements in BioM NPs for cancer therapy, taking into account the most common tumours and processes. As a result, the purpose of our present review study is to address this gap first. The discussion will next go to the numerous recent advances in BioM NPs for cancer therapy. This will cover the mechanics and procedures of BioM NPs, as well as their utilization in therapeutics. This paper then summarizes existing knowledge and investigates the numerous limitations and promise of synthetic BioM NPs for cancer therapy. This review aims to provide researchers with an overview of the current research and technological development of BioM NPs for cancer therapy. It serves as a guide for integrating BioM NPs into cancer research and future nanomedicine applications.
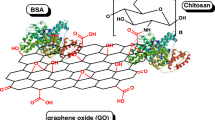
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancers are currently considered among the more costly diseases, with severe and long-lasting health, standard of life, and financial effects due to disease diversity and intricacy [1]. The various drawbacks and serious adverse reactions of conventional chemotherapeutic medications, in addition to different and variable therapeutic results, contribute to this [2]. The difficulty of medications to penetrate deep into tumour tissues and kill malignant cells selectively is a key barrier to pharmacotherapy [3]. Furthermore, many anticancer medications have a lack of solubility, making them unsuitable for intravenous administration, resulting in inefficient biodistribution and pharmacokinetic profiles [2], low drug concentrations at the tumour site, and larger drug concentrations in normal tissues resulting in serious adverse consequences [4, 5].
Nanoparticles (NPs), which range in size from 1 to 100 nm [6], have several benefits and uses in a variety of sectors [7]. NPs are used in a variety of biological applications, including drug delivery [8], imaging, diagnostics [4], regenerative medicine, and therapy [9]. Smart NPs have emerged as a possible alternative to traditional NPs in cancer treatment [10]. Besides, because of their large surface area and distinct catalytic characteristics [11], NPs perform as effective catalysts for chemical processes [12]. They are utilized in catalytic converters, fuel cells, and hydrogen generation [11]. Furthermore, NPs are employed in a variety of environmental applications [13], including water purification, gas sensing [14], pollution detection and removal, and site rehabilitation [15]. Because of the many applications of NPs, Cimen et al. [16] created metal-chelated magnetic NPs for protein C purification. Besides, BioM NPs have demonstrated potential in wastewater treatment technologies such as anaerobic ammonium oxidation (anammox); BioM NPs can function as catalysts, accelerating the anammox reaction kinetics [17]. BioM NPs accelerate the anammox process by providing active sites for the conversion of ammonium and nitrite to nitrogen gas, resulting in quicker nitrogen removal rates and increased treatment efficiency [18].
There is an increase in the number of manufactured NPs being explored for various uses in cancer [4]. NPs have been designed with an appropriate nano-ranged size for tumour-targeting characteristics and the decrease of unwanted off-target effects of medicines and immunological treatments [9]. They involve medication protection from biological circumstances in addition to the crossing of biological barriers. This provides medications with stability until they are released in a regulated way [4, 9]. Some of the most prevalent types include solid lipid NPs and metal-based NPs [19]. The size, charge, shape, and surface changes of NP drug delivery systems allow for intratumoral trafficking. To address the issue of tumour heterogeneity, NPs with optimised physicochemical characteristics and biological components are employed to increase blood circulation time, tumour penetration, and tumour accumulation, consequently enhancing the therapeutic index of these formulations [20]. The improved porosity and retaining impact have been seen as critical to the therapeutic effectiveness of nanomedicines, in which particles may enter and be kept inside tumour tissue because of fenestrations in quickly developed vasculature and inadequate lymph drainage, both of which are common in solid tumours [21]. However, reliance on this phenomenon has begun to decrease as a result of recurrent inconsistencies, tumour heterogeneity, and poor translation from in vivo research to the clinical scenario [22]. As a result, active NP targeting is predicted to play a key role in medication delivery and controlled release in future treatments [23]. This can be accomplished with externally conjugated peptides for active targeting, better binding, and increased drug accumulation at the tumour location [22, 24].
Given the peculiarities of the tumour environment in malignancies [25], which restrict the delivery and efficiency of both chemo- and immunotherapies, new research has embraced the distinct benefits of nanotechnology-based methods to address these obstacles [26]. Several nano-biomaterials are exploited as drug delivery methods targeting malignancies due to their enhanced permeability and retention (EPR) impact [27]. Additionally, there nevertheless exists an absence of targeting. Furthermore, surface decorating of NPs with targeted ligands is an efficient strategy for improving delivery efficiency [28], but the difficult procedure and potential for immune system activation may limit their applicability [1]. To compensate for the drawbacks of the previous two delivery technologies, the biomimetic (BioM) delivery system based on multifunctional cell membranes has been devised to incorporate the properties of a highly targeted nano platform and biocompatibility. The circulation period of medications can be extended, their biocompatibility and targeting increased, and their harmful and side effects decreased by encapsulating them with biofilms to produce BioM nanocarriers. The BioM NPs-based therapy of various malignancies is one area of this fast-emerging research that has received a lot of attention. However, to the best of our knowledge, no published study has reviewed solely the recent advancements of BioM NPs for cancer therapy; taking into account the most prominent cancers and their mechanisms. Hence, our current review paper seeks to first fill this gap. Then continue by discussing the various current breakthroughs in BioM NPs for effective cancer treatment. This will include mechanisms of BioM NPs and methods, as well as the use of BioM NPs in their therapies. This study then summarises existing knowledge and examines the multiple challenges and potential of synthesised BioM NPs for cancer treatment.
Cancers and Mechanisms of Cancer Tumours
Cancers are a diverse collection of illnesses distinguished by uncontrolled cell development and the capacity of these cells to infect surrounding tissues [29]. The prevalence of various forms of cancer varies by geography, population, and period. Numerous cancer types cause havoc the world over. However, as of February 2022, the WHO identifies breast, lung, colon, rectum, and prostate cancers are the most prevalent [30]. Breast cancer is the most frequent cancer in women, with a high global incidence. Many individuals’ outcomes have improved as a result of early discovery through screening and breakthroughs in therapy [31]; lung cancer develops in the lungs and is frequently connected with tobacco smoke [32]; however, nonsmokers can also acquire lung cancer; colorectal cancer affects the colon or rectum and typically begins as polyps that can progress to cancer over time [33]; furthermore, one of the most frequent malignancies in males is prostate cancer [34]; it usually begins in the prostate gland and progresses slowly [30].
It is crucial to remember that cancer statistics are subject to change, and the prevalence of individual malignancies can be altered by variables including way of life, exposure to pollutants, genetics, and advances in cancer detection and therapy. The latest data on cancer incidence and prevalence are provided via regular updates from health organisations and cancer registries.
Cancer tumours form as a result of a set of events that include genetic abnormalities [35], aberrant cell signalling [36], and evasion of the body’s normal regulatory processes [35, 36]. They are frequently caused by genetic mutations that accumulate in a cell’s DNA [37]. These mutations may be induced by a variety of circumstances [38], such as cancer-causing chemicals [39], genetic predisposition, or faults in DNA replication [38]. Unregulated division of cells can result from mutations in genes that govern cell-cycle regulation. Cancer cells can circumvent the usual regulatory checkpoints, resulting in rapid and uncontrolled multiplication [40]. Apoptosis, also known as programmed cell death, is a natural process that rids the body of damaged or superfluous cells. Cancer cells can have mutations that allow them to resist apoptosis, allowing them to live and multiply over time [41]. Tumours require blood to survive and develop. Cancer cells can induce the development of new blood vessels to deliver nutrients and oxygen to the developing tumour. Cancer cells can infect tissues that surround them and travel to distant organs via the bloodstream or lymphatic system. This process, known as metastasis [42], is a characteristic of cancer and contributes greatly to its lethality [29]. Cancer cells may acquire mechanisms that allow them to avoid identification and elimination by the immune system. This may entail suppressing immune responses or establishing an immunosuppressive milieu within the tumour. Cancer cells frequently demonstrate genomic instability [43], in which the DNA repair systems are compromised, resulting in additional mutation accumulation. This adds to cancer cell heterogeneity inside a tumour. The tumour’s surrounding environment, which includes immune cells, fibroblasts [44], and blood arteries [35, 36], is critical to tumour growth [45]. Cancer cells can modify their surroundings to encourage their proliferation and avoid detection by the immune system [46, 47].
Identifying these pathways is critical for creating successful cancer therapies that target particular vulnerabilities in cancer cells while causing the least amount of harm to healthy organs. It is vital to remember that cancer is a diverse illness with distinct processes for different forms of cancer.
Biomimetic Nanoparticles (BioM NPs) Mechanisms in Cancer Treatment
Before determining possibilities for improvement feasibility of BioM NPs through nanomedicine, it is vital to understand present treatment approaches and their inadequacies. According to a variety of information, methods of therapy for cancers could profit from the incorporation of nanomaterials [48, 49]. NPs can be used in surgery to improve imaging and for nanotechnology-based identification of residual or metastasized malignant material within draining lymph nodes [50]. The storage and targeting capacity of nanomedicine has also increased the effectiveness of chemotherapy. NPs have dramatically higher targeting, circulation time [4], and volume of distribution while exhibiting lower toxicity to normal tissues [1]. Radiotherapy and hyperthermia, in addition to conventional mAb- and non-mAb-based immunotherapies, have improved when aided by NPs [51]. Aside from these treatments, cervical and breast cancers stand to profit from improvements in NP-enabled gene editing and immune therapy, which are continually being developed and enhanced [5].
Biomimetic Nanoparticles (BioM NPs) for Passive Targeting of Cancer Cells
Biomimetic NPs (BioM NPs) for cancer cell passive targeting are a potential strategy in cancer treatment. Passive targeting makes use of tumour tissues’ inherent properties, including leaky vasculature [52] and limited lymphatic drainage, which enable NPs to aggregate preferentially in the tumour without actively targeting particular molecules on cancer cells [53]. BioM NPs imitate biological structures or properties to increase medication delivery effectiveness and interaction with cancer cells [52, 54]. The Enhanced Permeability and Retention (EPR) effect [53], particularly based on the leaky nature of tumour blood vessels, is used in passive targeting. NPs could extravasate from the circulation into the tumour interstitium with greater ease than normal tissues, resulting in tumour accumulation [55]. Figure 1 depicts a crucial process of EPR effect for the tumour buildup of potential nanocarriers.
A crucial process of the EPR effect for the tumour buildup of potential BioM NP nanocarriers for passive targeting of cancerous cells [62]. Reproduced with permission under the terms and conditions of the Creative Commons Attribution (CC BY) licence
Passive targeting’s efficacy is determined by tumour biology, which includes characteristics like degree of vascular and lymphatic vessel development [56], perivascular tumour invasion, and intra-tumour pressure [57]. These features, in addition to the physicochemical properties of BioM NPs, impact the success of passive nanomedicine targeting [54, 58]. Furthermore, blood circulation time has a substantial influence on targeting effectiveness; owing to the vascular barriers, systemically injected designed BioM NPs as medication carriers require a significantly longer circulation time to increase the likelihood of passing through the vascular wall [59, 60]. The quick clearance of nanomedicine by the reticuloendothelial system is one of the major impediments to extended blood circulation. Shi et al. addressed the use of steric stabilisation strategies such as PEGylation to address this problem. PEG is utilised to create covert drug carriers that have a longer circulation lifespan and are less detectable and cleared by the mononuclear phagocyte system (MPS). PEG is found in the majority of clinically authorised nanomedicines and investigational nanotherapeutics. The widespread use of PEG in over-the-counter (OTC) drugs, as well as medical products and vaccinations, sparked research that revealed PEG is not as immunologically inactive as previously thought [61].
BioM NPs can be used for imaging as well as medication administration, assisting in the diagnosis and monitoring of cancer development. Integrating medicinal and imaging functions in a single NP is a current research topic. However, issues include guaranteeing BioM NP stability, scalability, and repeatability. More study is needed to improve their in vivo performance and address any immunogenicity problems. BioM NPs for passive targeting represent a novel method with the potential to improve cancer therapy efficacy while minimising off-target consequences. The current study is aimed at refining and translating these advances from the lab to clinical applications. Bigaj-Józefowska et al. created multipurpose iron-modified mesoporous polydopamine NPs (MPDAFe NPs). Findings show significant promise for integrating effective medication administration with magnetic resonance imaging (MRI) and highlight the benefits of BioM coating with tumour cell-derived membranes. The resulting coating increased the targeting abilities of the NPs and extended their circulation. Also, rigorous biosafety assessments show that the combination chemo- and phototherapy displayed substantial cytotoxicity against cancer cells. The photothermal impact evaluation revealed increased cytotoxicity from laser irradiation, demonstrating the synergistic impacts of nanomaterials and photothermal treatment. A chemotherapeutic impact study revealed that cancer cell membrane-coated MPDAFe NPs outperformed free doxorubicin in suppressing cancer cell survival and proliferation [63]. Besides, Yin et al. described a BioM camouflage system for targeted drug administration and MRI, as well as macrophage membrane-coated iron-poly(tannic acid) NPs (Fe-PTA NPs). The surface protein profiles of macrophage cells were inherited by the macrophage membrane, allowing them to bypass the reticuloendothelial system and target homotypic cells. Doxorubicin (DOX), an anticancer medication, was loaded into macrophage membrane-Fe-PTA NPs and displayed pH-responsive release capabilities. Furthermore, the macrophage membrane-Fe-PTA NPs have the potential to be employed as T1-weighted MRI contrast agents for targeted MRI. This cell membrane camouflage approach holds enormous promise and presents a significant obstacle for clinic-based targeted treatment [64].
Tong et al. created a nedaplatin-encapsulated PEGylated liposomal cocktail. Employing high-performance liquid chromatography (HPLC), they discovered the incompatible nature of NDP with natural phospholipids. The orthogonal approach was used to optimise the parameters for making nedaplatin-encapsulated PEGylated liposomal, with the effectiveness of encapsulation serving as the criterion. The physicochemical features of optimised nedaplatin-encapsulated PEGylated liposomal, such as particle size, zeta potential, encapsulation efficacy, delivery patterns, and others, are extensively characterised. The findings indicated that nedaplatin-encapsulated PEGylated liposomal had a considerably sustained release profile, and the releasing time of nedaplatin might be as long as 8 days. Nedaplatin incorporated in PEGylated liposomes increased cellular absorption and demonstrated significant cytotoxic action. Nedaplatin-encapsulated PEGylated liposomal may accumulate at tumour locations after intravenous administration and successfully prevent tumour development in mice without noticeable side effects. The findings suggested that PEGylated liposomes might be a potential carrier for enhancing the therapeutic benefits of nedaplatin [65].
As illustrated by Fig. 2, Waghule et al. created and tested PEGylated liposomes and lyotropic liquid crystals to extend the plasma circulation duration of temozolomide. Throughout the manufacturing process, economically practicable membrane extrusion and improved hot melt emulsification procedures were used. Liposomes and lyotropic liquid crystals in the nanoscale were created. The BioM NP nanocarriers were discovered to have a longer release time. The cytotoxicity of temozolomide in glioblastoma cell lines was found to be tenfold higher than that of free temozolomide. PEGylated liposomes and PEGylated lyotropic liquid crystals have been shown to have a multiple-fold lower cell uptake in macrophage cell lines than uncoated liposomes and lyotropic liquid crystals, as well as a twofold increase in plasma when contrasted with Temozolomide when injected via the vein. Enhancing temozolomide plasma circulation duration resulted in a considerable improvement in brain bioavailability. The enhanced pharmacokinetics and biodistribution of temozolomide demonstrated the promise of these PEGylated BioM NP nanocarriers in the therapy of glioblastoma [66].
PEGylated liposomes and PEGylated lyotropic liquid crystals for glioblastoma therapy [66]. Reproduced with permission; Licence Number 5706910124252
This method has the potential to maintain the therapeutic effectiveness of PEGylated liposomes, particularly when administered repeatedly. As a result, academics are actively investigating creative approaches to addressing these increasing difficulties. Such approaches represent a possible avenue for reducing the immunogenicity of NP-enhanced cancer medication release, hence increasing its treatment perspective.
Biomimetic Nanoparticles (BioM NPs) for Active Targeting of Cancer Cells
BioM NPs developed for active cancer cell targeting have unique targeting ligands on their surfaces to increase their attraction for cancer cells [67]. This active targeting technique attempts to increase medication delivery precision and effectiveness to malignant cells, possibly minimising adverse impacts and enhancing the effectiveness of treatment. This method entails designing BioM NPs with specialised ligands that can recognise and bind to receptors specific to target cells (Fig. 3). Antibodies, amino acids [68], and aptamers [69] having a high selectivity for cancer cell receptors are frequently employed [70]. These ligands may be selected based on the unique molecular features of the malignancy being treated [70, 71]. The surface of NPs can be coated with monoclonal antibodies, enabling them to recognise and attach to particular antigens on cancer cells. This method is especially effective when targeting cell surface receptors that are overexpressed in specific cancers [71]. Active targeting improves NP absorption by promoting receptor-mediated endocytosis [72]. This can boost therapeutic chemical distribution into cancer cells while reducing absorption by healthy cells. Multifunctional BioM NPs for active targeting are frequently created [73]. They can transport therapeutic molecules like chemotherapeutic medicines [74], RNA [73], or imaging [64, 75] agents as well as targeting ligands and other capabilities [76].
A crucial process for the tumour buildup of potential nanocarriers. Active targeting: the application of ligands to tumorous cells’ surface receptors [62]. Reproduced with permission under the terms and conditions of the Creative Commons Attribution (CC BY) licence
Chen et al. used ZIF-8 as the carrier to design and produce a trastuzumab-coupled drug delivery framework (Fig. 4) with pH response properties. The drug loading and biocompatibility of the targeted drug delivery device were both high. At neutral pH circumstances, the cumulative curve of drug delivery showed minimal early leakage levels. There was an efficient augmentation in drug delivery at acidic pH conditions, confirming the existence of a specific pH-triggered drug delivery strategy. Because they can deliver the loaded medication in a regulated way, the created BioM NPs can function as drug delivery systems. Cellular uptake studies revealed that the internalisation induced by the HER2 antibody significantly increased NP uptake. This discovery suggests that the BioM NPs can specifically target cancer cells that overexpress HER2. The platform was tested for therapeutic effectiveness in BALB/c nude mice to verify its promise as an efficient drug delivery method for tumour inhibition in vivo. The results illustrate the smart drug delivery system’s specificity-targeted and pH-responsive characteristics, showing its great potential for effective and controlled cancer therapy usage [77].
Antibody-targeted ZIF-8 framework drug delivery mechanism in Her2 receptor-positive cells as an effective in vivo tumour inhibition drug delivery method [77]. Reproduced with permission; Licence Number 5706910546921
The work [78] looked at the preparation, physiochemical characterization, and in vitro and in vivo impacts of sialic acid and cetuximab decorated chitosan NPs loaded with gemcitabine and targeted to glycan and epidermal growth factor receptor overexpressing non-small-cell lung cancer cells. Chitosan was coupled with sialic acid using EDC/NHS chemistry and then gemcitabine-loaded sialic acid-conjugated chitosan NPs were produced using an ionic gelation technique and electrostatically adorned with cetuximab. In vitro, cytotoxicity of NPs determined with cell-based apoptosis tests revealed that targeted nanoformulations outperformed non-targeted nanoformulations in antiproliferative activity versus non-small-cell lung cancer cells. In vivo pharmacokinetic studies revealed that glycan and epidermal growth factor receptor-targeted NPs had higher absorption, and in vivo clinical effectiveness studies revealed that they have the strongest anticancer potential. By focussing on glycan and epidermal growth factor receptors on non-small-cell lung cancer cells and an induced lung cancer mouse model, the platform showed improved cellular internalisation and therapeutic perspective, suggesting that it could be an effective replacement for non-targeted, traditional chemotherapy [78].
Rajana et al. used a quality-by-design method to create Folic acid-adorned Palbociclib-loaded lipid-polymer hybrid NPs and tested their anticancer effectiveness in folate receptor-positive breast cancer cell lines. The synthesis of the as-prepared ligand was confirmed using spectroscopic methods. The optimised recipe had a satisfactory particle size distribution and effective entrapment. The framework has an 11-fold lower IC50 value than free Palbociclib. A receptor-blocking experiment was used to investigate the effect of folic acid in targeting breast cancer, and it was shown that the framework was internalised into cancer cells via folate receptor-mediated endocytosis. The framework was more effective against cancer, causing increased reactive oxygen species creation, apoptosis, decreased cell motility, and colony formation. As a result, the Palbociclib-loaded folic acid-conjugated lipid-polymer hybrid NPs created might serve as a viable BioM NP nanocarrier in the therapy of breast cancer [79]. Also, as indicated by Fig. 5, for cancer-specific medication delivery and treatment, a folate-targeted pH-sensitive bortezomib conjugate can be created. In folate receptor overexpressing cancer cells and 3D spheroids, the compound prepared by Liu et al. demonstrated better cellular uptake, penetration, and anticancer activity compared to free bortezomib, a bortezomib-mannitol derivative, and a PEGylated bortezomib conjugation [80].
A diagram depicting folate-targeted pH-sensitive bortezomib conjugates for cancer therapy [80]. Reproduced with permission under the terms and conditions of the Creative Commons Attribution (CC BY) licence
Under the particular molecular characteristics of every tumour, the targeted ligands may be customised for particular kinds of cancer. This personalisation improves the NPs’ selectivity for a certain malignancy. Off-target effects, diversity in receptor expression across individuals, and the necessity for efficient ligand conjugation techniques are all challenges. Furthermore, questions of NP stability, circulation time, and immune response must be tackled. Active targeting employing BioM NPs is an emerging subject that has an opportunity to transform cancer therapy. The current studies seek to enhance cancer therapy results by optimising the design, production, and clinical translation of these NPs.
Biomimetic Nanoparticles (BioM NPs) for Stimuli-Responsive Cancer Drug Release
BioM NPs created for stimulus-responsive cancer medication deliver therapeutic drugs in response to specific stimuli observed in the tumour microenvironment (TME) [81]. These stimuli can include changes in pH [80], temperature, enzyme activity [82], or other cancer-specific variables [83]. The objective is to improve medication delivery accuracy and control while minimising off-target effects and boosting therapeutic effectiveness [84]. By adding stimuli-responsive features into the nanocarrier system, functional BioM medication delivery may be realised by bypassing biological barriers and arriving at the targeted location [85]. BioM NPs may be programmed to react to particular stimuli in the TME. Amid these stimuli, responsive materials experience structural modifications, resulting in drug release. Tumour tissues frequently have lower pH values than normal tissues [86]. pH-responsive NPs can be programmed to release medications in reaction to the tumour’s acidic environment, enhancing drug delivery and lowering systemic toxicity [84]. Temperature fluctuations within the body, especially in the tumour site, can be used to facilitate medication release. When exposed to the increased temperatures seen in tumours, thermoresponsive NPs can deliver their payload [87]. In the TME, some enzymes are overexpressed [88]. Enzyme-responsive NPs can be programmed to release medications in response to enzyme activity [88], allowing for tailored drug delivery.
Packing bupivacaine nanocrystals (BNCs) into thermoresponsive oligo(ethylene glycol) methyl ether methacrylate (OEGMA) nanogels and coupling them to NIR-absorbing biodegradable copper sulphide NPs (CuS NPs) resulted in the formation of a hybrid nanomaterial (Fig. 6) [87]. These materials were surface-enhanced with polyelectrolytes using layer-by-layer processes, allowing them to easily cling to the surface of nanogels via supramolecular interactions. Because bupivacaine was encapsulated in nanocrystals, CuS@BNC-nanogels with drug loading efficiency were created. The nanocrystals acted as long-lasting drug reservoirs, leading to higher localised drug content, which proved advantageous for the application in long-term pain control. When exposed to NIR light, the platform demonstrated favourable photothermal transducing capabilities. The photothermal action of the CuS NPs caused the nano-crystallized drug delivery to be accelerated by the breakdown of the thermoresponsive nanogels upon heating. Remote control of on-demand delivery at a given time and location was accomplished, showing their possible application as an externally operated triggerable drug delivery device. Also, in the dose-ranging investigation, cell viability assessments and flow cytometry analysis revealed acceptable cytocompatibility. This remotely actuated nano platform is a viable technique for long-term regulated analgesia and a viable therapeutic pain treatment option [87].
Packed bupivacaine nanocrystals (BNCs) into thermoresponsive oligo(ethylene glycol) methyl ether methacrylate (OEGMA) nanogels and coupling them to NIR-absorbing biodegradable copper sulphide NPs (CuS NPs) resulted in the formation of a hybrid nanomaterial [87]. Reproduced with permission; Licence Number 5706911048512
Previously, thermoresponsive drug delivery devices were employed to administer chemotherapeutic drugs to tumours in a hyperthermic milieu [89, 90]. As illustrated by Fig. 7, Shah et al. created and characterised cisplatin-packed thermoresponsive liposomes (CDDP@TSLs) for improved anticancer effectiveness. A thin-film hydration process was used to create CDDP@TSLs with variable ratios of dipalmitoyl phosphatidylcholine and hydrogenated soy phosphatidylcholine and fixed quantities of distearyl phosphoethanolamine polyethene glycol and cisplatin. The produced platform had small particle sizes, a reasonable surface charge, good cisplatin encapsulation efficacy, and ideal thermoresponsive characteristics. The CDDP@TSLs were examined for cytotoxicity against lung cancer cells, ovarian cancer cells, and breast cancer cells in vitro at room temperature ranges because tumorous sites might have greater temperatures than normal locations. At 39 °C, the cytotoxicity of CDDP@TSLs was higher. Cellular uptake tests revealed a multiplication of particle absorption by numerous cell types, as well as greater internalisation at tumour locations. The prepare framework’s therapy demonstrated the effectiveness of the thermoresponsive liposomal formulation in lung cancer cells produced in mice by diethylnitrosamine. Furthermore, the platform may have increased anticancer activity, and maximised therapeutic benefit while minimising systemic off-site toxicity [91].
Cisplatin-loaded thermoresponsive liposomes demonstrate improved antitumour effectiveness [89]. Reproduced with permission; Licence Number 5706911325407
The high concentration of reactive oxygen species (ROS) in tumour tissues is one of the distinguishing hallmarks of tumour longevity, proliferation, and metastasis [92]. Nevertheless, ROS-responsive NPs are seldom used in cancer cell ROS-responsive functions because inherent ROS concentrations in cancer cells cannot be elevated to a level at which the created BioM NP framework can respond. Besides, to remedy this obstacle, palmitoyl ascorbate was strategically incorporated by Li et al. as a prooxidant for H2O2. The H2O2 generation in cancer cells investigated H2O2-responsive camptothecin polymer, endowing the nanocarriers with the self-sufficiency of H2O2 stimuli in cancerous cells. Molecular oncology exhibits tumoral physiology’s markers, including a declining proclivity to eliminate harmful ROS. The generation of H2O2 selectively triggered cancer cell demise by increased oxidative stress. It also acted as an autochthonous H2O2 resource to stimulate camptothecin delivery for chemotherapy. Excess H2O2 and camptothecin were released and easily infiltrated cancer cells resulting in their cooperative cytotoxicity. A complete treatment study indicated that the suggested combination suppressed tumours effectively by cooperative oxidation-chemotherapy; describing a unique BioM NPs-based platform that combines tumoral H2O2 for H2O2-responsive drug delivery [93].
Enzyme-responsive BioM NPs are intended to take advantage of the overexpression of particular enzymes in the TME [88], allowing for tailored medication delivery [83]. These enzymes may encompass those that are uniquely connected with cancer cells as well as those that are engaged in pathological processes related to tumour development and progression [84]. The idea behind employing enzyme responsiveness is to take advantage of the distinct biochemical properties of cancer cells and their environment. As illustrated by Fig. 8, Liu et al. described a tiny molecular amphiphile prodrug that may self-assemble to create a multipurpose nano-prodrug for increased anticancer efficacy via chemotherapy and phototherapy. The easy incorporation of quinone propionate into Irinotecan provides adequate amphiphiles that equip the prodrug with good self-assembly behaviour and turn the compound into a firm and homogeneous NP. Surprisingly, this outstanding self-assembly behaviour may pack phototherapy agents to construct a multipurpose nano-prodrug, improving the chemotherapeutic impact of both chemotherapy and phototherapy. Notably, the prodrug’s quinone propionic acid moiety was highly sensitive to overexpressed quinone oxidoreductase-1 in non-small cell lung cancer cells, allowing for nano-prodrug deconstruction and effective quinone oxidoreductase-1-responsive drug delivery. A BioM nano-prodrug was effectively investigated to improve drug accumulation on tumour tissue and relocate blood clearance by covering the hybrid membrane on the above nano-prodrug, which shows higher particular inhibition of tumour growth and metastasis in non-small cell lung cancer mice model. The results add to the logical structure of tumour-overexpressed enzyme-responsive nano-prodrugs for cancer combination treatment [88].
Schematic illustration of tumour-overexpressed enzyme sensitive amphiphiles tiny molecular self-assembly nano-prodrug for non-small-cell lung cancer chemo-phototherapy [88]. Reproduced with permission; Licence Number 5706920023812
Imaging agents can be incorporated into some stimuli-responsive BioM NPs. This allows for real-time tracking of medication release and distribution inside the tumour, which aids in therapy evaluation and optimisation. The challenges of stimuli-responsive BioM NPs include gaining precise control over the stimuli-responsive mechanisms, optimising release kinetics, and maintaining nanoparticle stability in physiological circumstances. Clinical translation also takes into account biocompatibility, possible immunogenicity, and scalability. Stimuli-responsive BioM NPs are a promising new approach in cancer therapy, with the promise of enhanced therapeutic results and decreased side effects via targeted and regulated drug release. Current studies are aimed at improving these NP designs and moving them closer to therapeutic applications.
Applications of Biomimetic Nanoparticles (BioM NPs) for Cancer Therapy
BioM NPs have shown tremendous promise in a variety of cancer therapeutic applications [94], owing to their unique features and designs inspired by natural biological systems. Several technologies seek to enhance medication delivery [71], imaging [95], and diagnostics [27] while reducing adverse effects and increasing the ultimate effectiveness of cancer therapies. Utilising improved permeability and retention (EPR) impacts, BioM NPss, like NPs coated with cell membranes, can passively target tumours. This permits therapeutic medicines to accumulate selectively in the TME, decreasing exposure to healthy tissues. Adding specific ligands on the surface of biomimetic NPs allows for active targeting of particular cancer cells, boosting drug delivery accuracy. Concentrating medications at the desired site of action can improve the therapeutic index.
Lu et al. produced BioM NPs that provided medicines for lactate metabolism-based synergistic treatment using the discovery of increased lactate in resected Glioblastoma multiforme (GBM) (Fig. 9). Owing to the self-assembling NPs being enclosed in glioma cell membranes, they easily crossed the blood–brain barrier and targeted GBM via homotypic identification. Lactate oxidase in the NPs turns LA into pyruvic acid and H2O2 once it reaches the tumours. By inhibiting histone expression and producing cell-cycle arrest, PA suppressed cancer cell proliferation. A synergistic impact like this provides potent therapeutic efficacy against both glioma cell-line-derived and patient-derived xenograft models [96]. Further, a pro-nano drug combination with GSH and NIR-sensitive mode has been shown to improve gamabufotalin-induced chemo-photothermal treatment with the help of indomethacin-reprogrammed [97] TME. Furthermore, a hybrid cell membrane was employed to give nano complexes with the ability to prolong circulation duration and increase drug buildup in tumour tissue. Indomethacin triggered by elevated levels of GSH can reduce tumour inflammation in the TME and sensitise tumour cells to gamabufotalin by decreasing PGE2 release. The newly introduced low-dose gamabufotalin, which has few adverse reactions, may successfully destroy tumour cells through ROS generation and low COX-2 expression. In vitro and in vivo studies indicated that nanocomplexes had high antitumour efficacy in tumour-bearing mice via chemo-photothermal treatment, as evidenced by the eradication of cervical tumours and significant extension of mouse survival time [97].
Clinical and mouse glioma studies, as well as M@HLPC building for tumour inhibition, are depicted schematically [96]. Reproduced with permission under the terms and conditions of the Creative Commons Attribution (CC BY) licence
Through a mechanism known as cell membrane cloaking, BioM NPs may be capable of self-recognition and source-targeting [98]. The method increases their circulation time and assists them in avoiding immunological capture. As a consequence, BioM NPs coated with natural cell membranes derived from various sources [99], such as leukocytes, platelets, cancer cells [100], and red blood cells (RBCs), have gained popularity [101]. NPs coated in RBC membranes have a remarkably long circulation duration [102]; NPs coated with bacterial membranes, on the other hand, can readily access neutrophil locations and travel to inflamed tumour areas [103]. The tumour cell membrane is particularly attractive among these sources owing to its various surface molecular features [101], which give several potentials for BioM functionalization of NPs. Furthermore, the tumour cell membrane allows for membrane antigen-mediated homologous binding, which increases the uniqueness and efficiency of the NPs [98]. BioM NPs have considerable potential for targeted drug administration and better cancer therapy, owing to the characteristic properties such as cell membrane cloaking and leveraging the benefits conferred by their varied cell sources [100]. The purpose of tumour cell membrane-camouflaged NPs, especially the versatile BioM core–shell nanosystem, is to improve standard chemotherapy’s targeting capability and immune system evasion capability, resulting in improved drug administration and enhanced therapeutic results. Li et al. built MPCONPs to verify the idea (Fig. 10). To build a shell for the NPs, autologous tumour cell membrane fragments were collected and employed. A trypsin-sensitive cationic polylysine framework is created and integrated with l-OHP and Ce6-AuNDs. These components are assembled to make the MPCONPs. MPCONPs, which are NPs disguised as tumour cell membranes, have increased cellular absorption in cancer cells and the efficiency of photodynamic treatment and chemotherapy. This opens up a lot of possibilities for them to be used as individualised therapeutic agents in clinical cancer treatment [100].
Nanosystem of MPCONPs for homologous targeted dual-mode imaging and combination treatment [100]. Reproduced with permission; Licence Number 5706930401725
Peng et al. presented the artesunate-chloroquine conjunction and created a BioM NP based on poly (d,l-lactide-co-glycolide) (PLGA) for dual-targeting drug delivery. To produce a ROS-sensitive core of BioM NPs, hydroxymethyl phenylboronic acid linked poly (d,l-lactide-co-glycolide) was synthesised. To receive a BioM NP-Hydroxymethyl phenylboronic acid/artesunate/chloroquine@mannose-modified erythrocyte membrane, a mannose-modified erythrocyte membrane is cloaked on the artesunate and chloroquine-loaded poly (d,l-lactide-co-glycolide) (PLGA)-based BioM NP core. It shows great potential in reducing colorectal cancer cell growth and correcting the phenotypes of tumour-associated macrophages by targeting both tumour cells and M2-like tumour-associated macrophages. The BioM NPs demonstrated enhanced aggregation at tumour tissues and efficiently inhibited tumour development via both reductions of tumour cell proliferation and repolarization of tumour-associated macrophages in an orthotopic colorectal cancer animal model. Notably, the key to achieving outstanding antitumour effects is uneven distribution to cancer cells and tumour-associated macrophages. This study presented a biomimetic nanocarrier that is beneficial in the treatment of colorectal cancer [104]. Furthermore, Miao et al. announced the development of RBC membrane-camouflaged nanocarriers that could imitate RBCs at various stages of life and researched how the deformability of RBC-derived nanocarriers impacted their biological behaviours, influenced by the significant impact of the stiffness and deformability of natural RBCs on their life span and flowing through narrow vessels (Fig. 11). RBC membrane-coated elastic poly(ethylene glycol) diacrylate hydrogel NPs (RBC-ENPs) imitating dynamic RBCs demonstrated great immunocompatibility with little immunoglobulin binding on the surface protein corona, leading to decreased opsonization in macrophages and ultralong circulation. RBC-ENPs may also deform like RBCs and achieve great diffusion in the tumour extracellular matrix, resulting in increased multicellular spheroid penetration and tumour tissue accumulation. In animal cancer models, doxorubicin-loaded RBC-ENPs outperformed the first-line chemotherapy medication PEGylated doxorubicin liposomes. Tuning the physical characteristics of cell membrane-derived nanocarriers may give an alternate strategy for the bionic design of nanomedicines in the future, according to this study [105]. Cao et al. used naive neutrophil membrane-coated poly(ethylene glycol) methyl ether-block-poly(lactic-co-glycolic acid) (PEG-PLGA) NPs to demonstrate the therapeutic effectiveness of celastrol as a potential candidate chemical for the treatment of pancreatic cancer. Neutrophil membrane-coated NPs (NNPs) have been shown to cross the blood-pancreas barrier and deliver pancreas-specific drugs in vivo. NNPs accumulated selectively at the tumour site after systemic treatment in a tumour-bearing mouse xenograft model, in contrast to NPs lacking neutrophil membrane coating. Celastrol-loaded NNPs dramatically improved tumour inhibition in both orthotopic and ectopic tumour models, extending the longevity of tumour-bearing mice and reducing liver metastases. The findings indicate that celastrol-loaded NNPs are a realistic and successful therapy choice for pancreatic cancer [106].
Cell membrane-camouflaged nanocarriers with erythrocyte BioM deformability for ultralong circulation and enhanced cancer therapy [105]. Reproduced with permission under the terms and conditions of the Creative Commons Attribution (CC BY) licence
Camouflaging synthetic NPs with hybrid cell membranes has received a lot of attention lately. The resulting BioM NPs retain the physicochemical features of the artificial NPs while acquiring the biological functionalities of the parent cells [107]. In comparison to single-cell membranes, hybrid cell membranes can equip synthetic NPs with a variety of bio functions obtained from the original parent cells. By covering cancer cell-mitochondria hybrid membrane (HM) on the surface of Gboxin-loaded NPs, Zou et al. demonstrated a BioM nanomedicine (HM-NPs@G). A reactive oxygen species-sensitive polymer is used in another design aspect to promote at-site Gboxin release. The HM camouflaging gives HM-NPs@G unique properties such as high biocompatibility, an enhanced pharmacokinetic profile, efficient blood–brain barrier penetration, and homotypic dual cancer cell and mitochondria targeting. The findings indicate that HM-NPs@G enhance blood circulation and tumour accumulation. Female mice with orthotopic U87MG GBM and patient-derived X01 glioblastoma stem cell xenografts show effective tumour suppression with a longer lifetime and minor adverse effects. We think that the biomimetic Gboxin nanomedicine has promise as a therapy for brain tumours [108].
The nano-delivery system’s hybrid cell membrane camouflage boosted solubility and targeting capabilities to tumour locations with higher immune evasion. This Prussian blue NP-based BioM formulation was verified as an effective PA delivery vehicle for suppressing the development of breast cancer xenografts in nude mice by tail vein injection. Molecular tests demonstrated that the anticancer efficacy was achieved by inhibiting cell growth and inducing apoptosis. Results showed that combining PA with nanomaterials can be a successful technique for treating breast cancer in vivo [109]. Also, Evers et al. produced and analysed EV-liposome hybrid NPs (hybrids) as an alternate delivery strategy incorporating the features of both liposomes and EVs. It has been demonstrated that hybrids are spherical particles that encapsulate siRNA, include EV-surface producers, and functionally transport siRNA to many cell types. The functional behaviour of hybrids in terms of cellular absorption, toxicity, and gene-silencing efficiency differs from liposomes and varies depending on the recipient cell type. Furthermore, hybrids created with cardiac progenitor cell (CPC) derived EVs preserve functional features associated with CPC-EVs, such as endothelial signalling activation and motility. To summarise, hybrids combine the advantages of synthetic and biological drug delivery methods and might be used as future therapeutic carriers of siRNA [110]. Besides, Wang et al. effectively coated hollow polydopamine (HPDA) NPs with an outer membrane vesicle (OMV)-cancer cell cancer cells hybrid membrane composed of OMV and B16-F10 cancer cells membrane (Fig. 12). They used OMV immunotherapy in conjunction with HPDA-mediated PTT to increase antitumour effectiveness against melanoma. When administered intravenously through the tail vein, HPDA@[OMV-cancer cells] NPs homogeneously targeted melanoma and activated the immune response in vaccinated mice by quickly promoting dendritic cell (DC) maturation in lymph nodes. The findings revealed that the antitumour immune response and PTT mutually enhance the potential for therapy and eliminate melanoma with no adverse reactions. Through combining payload with application-specific capabilities, the homogeneous-target and immune activation hybrid BioM membrane adapts to numerous synergistic medicinal and imaging uses [111].
Membrane-coated bacterial vesicle-cancer cell Hybrid NPs for tumour specific Immune activation and photothermal therapy [111]. Reproduced with permission under the terms and conditions of the Creative Commons Attribution (CC BY) licence
Macrophages have a large impact on tissue development [112], homeostasis, and remodelling [113]. The TME is defined by several physiological mechanisms, which ultimately impact cancer growth and spread. When inflammatory chemokines attract macrophages to the site of inflammation, they engage with particular ligands and become “resident” in the endothelium or pannus of inflammatory arteries [112]. NPs are coated with diverse membrane coatings in a top-down method, including membranes from hybrid membranes that combine the capabilities of several types of macrophages. By merging membrane components generated from RAW264.7 and 4T1 cells, hybrid membrane-coated doxorubicin (PLGA) NPs (DPLGA@ NPs) were created [114]. These NPs were utilised to treat lung metastases caused by breast cancer. The coupling of NPs with a hybrid membrane derived from macrophage and cancer cells has several advantages, including the ability to target specific metastasis, homogenous tumour-targeting abilities in vitro, and significantly enhanced multi-target capability in a lung metastasis model in vivo. After treatment of breast cancer-derived lung metastases, the DPLGA@NPs demonstrated remarkable chemotherapeutic capability, with around 88.9% anti-metastasis effectiveness. These NPs were strong and demonstrated the multi-targeting properties of hybrid membranes. This research suggests a viable BioM nano platform for treating breast cancer metastasis [114].
Through communicating with the environment via translocated surface membrane components, the cell membrane “disguise” permits the particles to be regarded as the source cell by the body. The membrane-coated NP’s newly conferred properties can be used for biological interfacing in the body, giving natural answers to numerous biomedical challenges.
Challenges Associated with Biomimetic Nanoparticles (BioM NPs) for Cancer Therapy
The biological systems’ complexity presents substantial challenges for cancer cell targeting and therapy. When nanocarriers are added to biological fluids, they attract proteins to their surfaces, generating an adsorption layer known as the protein corona [115]. This protein layer has a substantial impact on the biological behaviour of nanocarriers by affecting their physicochemical characteristics and can ultimately regulate their fate in vivo. This procedure has a substantial influence on the stability, targeting capability, pharmacokinetics, and toxicity of nanocarriers. As a result, the physiological activity of NPs is strongly reliant on the characterisation of the proteins that make up the corona. Furthermore, protein corona is a Janus-like phenomenon that can have both good and negative effects on NP-based treatments [116]. On the one hand, protein corona can affect blood circulation, protein accumulation and penetration at target areas, cellular absorption in tumour-targeting delivery, and interactions between NPs and immune cells for immunotherapy. Protein corona, on the other hand, might generate unanticipated in vivo behaviours owing to biomolecule absorption on BioM NPs [1, 116]. Protein corona, for example, might impair NP-cell membrane contacts by covering the first changed ligands or presenting an unfavourable steric impact, which reduces cellular absorption. To summarise, creating successful nanocarrier systems for therapeutic delivery requires a thorough understanding of the protein corona and its intricate interactions with NPs. Furthermore, biological barriers that prevent nanomedicine from accumulating and penetrating tumours, from blood and tissue to the cellular level [117], are a substantial impediment. The principal barriers to medication delivery at the blood level are strongly related to the endothelial cells that line the blood arteries [118]. Inflammation and cancer are common causes of decreased blood flow, which might impede medicine delivery. Furthermore, the permeability of tumour vasculature and its dependency on vascular endothelial growth factor (VEGF) might make medication administration difficult [20]. Obstacles may include poor vascularization at the tissue level [60], which may lead to hypoxic zones that can impair medication efficacy and delivery. Raised interstitial fluid pressures inside the TME may prevent medicines from reaching tissues efficiently. Furthermore, the variability of tissue features between and within tumours complicates medication administration even more [119]. This heterogeneity can take the form of differences in cell types, genetic mutations, or vasculature, all of which might affect medication delivery and efficiency. The fundamental issue at the cellular level derives from the passive nature of the majority of drug delivery techniques, which depend on transfer and concentration gradients to transfer medication from high-concentration parts to low-concentration areas, limiting the quantity of medicine reaching tumour cells. Besides, concerns concerning nanomedicine’s toxicity and safety, particularly its effects on organs and reproductive systems, are critical for long-term therapeutic usage [120]. For maximum therapeutic efficiency, nanocarrier drug loading and release control must be refined [121]. Adoption barriers such as difficult production, high prices, low biocompatibility, and the limited stability of BioM NPs prevent their widespread use in clinical settings.
Summary of Challenges
It is a difficult undertaking to create and synthesise BioM NPs that successfully combine biological elements while retaining stability and repeatability. To guarantee the safety of NPs for clinical application, the possible immunogenic response to NPs, particularly those generated from biological sources, must be carefully considered. The transition from laboratory-scale to large-scale manufacturing raises issues in preserving BioM NP uniformity and quality. BioM NPs may have low storage stability, necessitating the use of specific settings to prevent deterioration or loss of effectiveness over time. The variety of cancer types and tumour heterogeneity make it difficult to discover universal biomarkers for effective and precise targeting. Getting BioM NPs to the target location might be difficult due to physiological obstacles such as the reticuloendothelial system and the blood–brain barrier. Achieving regulatory requirements for clinical translation necessitates extensive testing and validation, and BioM NPs have to satisfy safety and effectiveness criteria.
To address the issues connected with BioM NPs for cancer treatment, scientists, engineers, and doctors must work together across disciplines. Continuous R&D efforts are required to realise the full potential of these novel nanocarriers in enhancing cancer treatment results.
Prospects Associated with Biomimetic Nanoparticles (BioM NPs) for Cancer Therapy
Transcytosis nanomedicine goes beyond the traditional active targeting technique, which primarily includes the binding of nanomedicine to cell surface receptors. It is intended to be moved across cells by utilising cellular machinery to move nanomedicine from one side of the cell to the other. This mechanism is useful for bypassing biological barriers that are ordinarily difficult to permeate, such as the blood–brain barrier or thick tumoral tissues. Transcytosis nanomedicine is notably useful in cancer therapy since the TME frequently provides a strong hurdle to traditional drug delivery strategies. We can improve treatment efficacy while minimising systemic toxicity by using transcytosis nanomedicine to increase the buildup of therapeutic molecules in tumour tissues [122]. For the creation of transcytosable nanomedicines, multiple approaches can be used, such as the employing of targeting ligands that bind to specific cell surface receptors, triggering endocytosis [81], and the development of nanocarriers that can avoid endosomal entrapment to reach the cytosol [123], encouraging exocytosis on the other side of the cell [1].
Summary of Prospects
BioM NPs have the promise of personalised cancer therapy since they can be tailored to particular patient profiles, allowing for more focussed and successful therapies. The adaptability of BioM NPs enables the inclusion of numerous therapeutic drugs, enabling combination treatments to attack diverse elements of cancer development at the same time. They can increase medication stability, lengthen circulation time, and improve drug penetration into tumour tissues, resulting in more efficient drug administration. BioM NPs may lessen the risk of adverse effects associated with standard cancer therapy by using biocompatible materials and replicating natural biological processes. Imaging agents can be included with BIoM NPs for real-time monitoring of therapy response, giving useful data for altering therapeutic tactics. Creating BioM NPs that react to particular environmental signals inside the TME can allow for regulated and targeted medication release. They can be designed to modify the immune response, thereby increasing the efficacy of cancer immunotherapies. Investigating environmentally friendly ways for the manufacture of BioM NPs might help to ensure the long-term viability of nanomedicine.
By appropriately evoking the immune system or controlling the TME in the immune system, the inclusion of BioM NPs into cancer vaccines represents a possible advance in cancer immunotherapy. Despite being intensively investigated in preclinical and clinical studies, the intricacy of biomaterials could present various hurdles for clinical translation. Significant research is needed to gain a thorough knowledge of their utilisation in cancer therapies, with an emphasis on immunology, biodistribution, and therapeutic processes. Additional research ought to delve further into these issues to accomplish clinical translation.
Concluding Remarks
Nanomedicine has the potential to revolutionise cancer therapy by addressing the limitations of existing medicines. It uses NP-mediated drug delivery to improve tumour-targeting and medication effectiveness, and it has potential in a variety of treatments. While there are hurdles, such as improving biocompatibility, regulating drug delivery, streamlining nano-design, and developing appropriate assessment models, the future of nanomedicine in cancer therapies looks prospective. Persistent innovation will assist it in reaching its maximum potential, opening the way for personalised and efficient therapies that will enhance patient outcomes and have a substantial influence on the cancer battle. This study thus focuses on recently prominent cancer types, their mechanisms and breakthroughs in BioM NPs for successful cancer therapy. Our study includes BioM NP mechanisms and techniques, and also the application of BioM NPs in cancer therapies. The remainder of this work gathers available data and explores the multiple challenges and promise of BioM NPs for cancer treatment.
Data Availability
Not applicable.
References
M. Chehelgerdi, M. Chehelgerdi, O.Q.B. Allela, R.D.C. Pecho, N. Jayasankar, D.P. Rao, T. Thamaraikani, M. Vasanthan, P. Viktor, N. Lakshmaiya, M.J. Saadh, A. Amajd, M.A. Abo-Zaid, R.Y. Castillo-Acobo, A.H. Ismail, A.H. Amin, R. Akhavan-Sigari, Progressing nanotechnology to improve targeted cancer treatment: overcoming hurdles in its clinical implementation. Mol. Cancer (2023). https://doi.org/10.1186/S12943-023-01865-0
E.T. Bin, A. Shahriar, A.R. Mahmud, T. Rahman, M.H. Abir, M.F.R. Siddiquee, H. Ahmed, N. Rahman, F. Nainu, E. Wahyudin, S. Mitra, K. Dhama, M.M. Habiballah, S. Haque, A. Islam, M.M. Hassan, Multidrug resistance in cancer: understanding molecular mechanisms, immunoprevention and therapeutic approaches. Front. Oncol. (2022). https://doi.org/10.3389/FONC.2022.891652
U. Anand, A. Dey, A.K.S. Chandel, R. Sanyal, A. Mishra, D.K. Pandey, V. De Falco, A. Upadhyay, R. Kandimalla, A. Chaudhary, J.K. Dhanjal, S. Dewanjee, J. Vallamkondu, J.M. Pérez de la Lastra, Cancer chemotherapy and beyond: current status, drug candidates, associated risks and progress in targeted therapeutics. Genes Dis. 10, 1367 (2023). https://doi.org/10.1016/J.GENDIS.2022.02.007
E. Issaka, M.A. Wariboko, E.A. Agyekum, Synergy and coordination between biomimetic nanoparticles and biological cells/tissues/organs/systems: applications in nanomedicine and prospect. Biomed. Mater. Dev. (2023). https://doi.org/10.1007/s44174-023-00084-x
J.A. Hess, M.K. Khasawneh, Cancer metabolism and oxidative stress: insights into carcinogenesis and chemotherapy via the non-dihydrofolate reductase effects of methotrexate. BBA Clin. 3, 152–161 (2015). https://doi.org/10.1016/j.bbacli.2015.01.006
N. Hossain, M.H. Mobarak, M.A. Mimona, M.A. Islam, A. Hossain, F.T. Zohura, M.A. Chowdhury, Advances and significances of nanoparticles in semiconductor applications—a review. Res. Eng. (2023). https://doi.org/10.1016/j.rineng.2023.101347
G. Naga Mallikarjun Rao, M.R.K. Vakkalagadda, A review on synthesis, characterization and applications of nanoparticles in polymer nanocomposites. Mater. Today Proc. (2023). https://doi.org/10.1016/j.matpr.2023.09.135
R. Liu, C. Luo, Z. Pang, J. Zhang, S. Ruan, M. Wu, L. Wang, T. Sun, N. Li, L. Han, J. Shi, Y. Huang, W. Guo, S. Peng, W. Zhou, H. Gao, Advances of nanoparticles as drug delivery systems for disease diagnosis and treatment. Chin. Chem. Lett. 34, 107518 (2023). https://doi.org/10.1016/j.cclet.2022.05.032
E. Issaka, State-of-the-art of synthesized exosomes and NPs-based biomimetic nanoparticles for wound rehabilitation: a review. Biomed. Mater. Dev. (2023). https://doi.org/10.1007/s44174-023-00112-w
L. Sun, H. Liu, Y. Ye, Y. Lei, R. Islam, S. Tan, R. Tong, Y.-B. Miao, L. Cai, Smart nanoparticles for cancer therapy. Signal Transduct. Target. Ther. 8, 418 (2023). https://doi.org/10.1038/s41392-023-01642-x
E. Issaka, J.N.-O. Amu-Darko, S. Yakubu, F.O. Fapohunda, N. Ali, M. Bilal, Advanced catalytic ozonation for degradation of pharmaceutical pollutants—a review. Chemosphere 289, 133208 (2022). https://doi.org/10.1016/j.chemosphere.2021.133208
E. Issaka, J.N.O. Amu-Darko, M. Adams, S. Yakubu, E. Gyimah, N. Ali, J. Cui, M. Bilal, Zinc imidazolate metal-organic frameworks-8-encapsulated enzymes/nanoenzymes for biocatalytic and biomedical applications. Catal. Lett. 153, 2083–2106 (2022). https://doi.org/10.1007/s10562-022-04140-x
E. Issaka, M.A. Wariboko, A. Mohammed, M. Enyan, S. Aguree, Trends in enzyme mimics for enhanced catalytic cascade systems for bio-sensing of environmental pollutants—a review. Chem. Eng. J. Adv. 15, 100510 (2023). https://doi.org/10.1016/j.ceja.2023.100510
J.N.O. Amu-Darko, S. Hussain, X. Zhang, M. Ouladsmane, E. Issaka, S. Ali, M. Wang, G. Qiao, Exploring the gas-sensing properties of MOF-derived TiN@CuO as a hydrogen sulfide sensor. Chemosphere 337, 139401 (2023). https://doi.org/10.1016/j.chemosphere.2023.139401
E. Issaka, M.A. Wariboko, N.A.N. Johnson, O.N. Aniagyei, Advanced visual sensing techniques for on-site detection of pesticide residue in water environments. Heliyon 9, e13986 (2023). https://doi.org/10.1016/j.heliyon.2023.e13986
D. Çimen, N. Bereli, A. Denizli, Metal-chelated magnetic nanoparticles for protein C purification. Sep. Sci. Technol. 55, 2259–2268 (2020). https://doi.org/10.1080/01496395.2019.1618327
M. Adams, E. Issaka, C. Chen, Anammox-based technologies: a review of recent advances, mechanism, and bottlenecks. J. Environ. Sci. 148, 151–173 (2025). https://doi.org/10.1016/j.jes.2024.01.015
E.A. Redina, O.A. Kirichenko, Mono- and bimetallic nanoparticles in catalysis. Catalysts 14, 68 (2024). https://doi.org/10.3390/catal14010068
W. Najahi-Missaoui, R.D. Arnold, B.S. Cummings, Safe nanoparticles: are we there yet? Int. J. Mol. Sci. 22, 1–22 (2021). https://doi.org/10.3390/IJMS22010385
M.J. Mitchell, M.M. Billingsley, R.M. Haley, M.E. Wechsler, N.A. Peppas, R. Langer, Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discovery 20, 101–124 (2020). https://doi.org/10.1038/s41573-020-0090-8
D. Fan, Y. Cao, M. Cao, Y. Wang, Y. Cao, T. Gong, Nanomedicine in cancer therapy. Signal Transduct. Targeted Ther. 8, 1–34 (2023). https://doi.org/10.1038/s41392-023-01536-y
Q. Liu, J. Cai, Y. Zheng, Y. Tan, Y. Wang, Z. Zhang, C. Zheng, Y. Zhao, C. Liu, Y. An, C. Jiang, L. Shi, C. Kang, Y. Liu, NanoRNP overcomes tumor heterogeneity in cancer treatment. Nano Lett. 19, 7662–7672 (2019)
M. Raatz, S. Shah, G. Chitadze, M. Brüggemann, A. Traulsen, The impact of phenotypic heterogeneity of tumour cells on treatment and relapse dynamics. PLoS Comput. Biol. (2021). https://doi.org/10.1371/JOURNAL.PCBI.1008702
L.J. Marshall, J. Bailey, M. Cassotta, K. Herrmann, F. Pistollato, Poor translatability of biomedical research using animals—a narrative review. Altern. Lab. Anim. 51, 102–135 (2023). https://doi.org/10.1177/02611929231157756
C. Wang, S. Zhang, Advantages of nanomedicine in cancer therapy: a review. ACS Appl. Nano Mater. (2023). https://doi.org/10.1021/ACSANM.3C04487
M. Chehelgerdi, M. Chehelgerdi, The use of RNA-based treatments in the field of cancer immunotherapy. Mol. Cancer (2023). https://doi.org/10.1186/S12943-023-01807-W
Q. Wang, Z. Wang, Z. Li, D. Li, F. He, K. Wang, J. Tian, X. Zhao, Biomimetic camouflaged nanoparticle-based folfirinox platform for optimizing clinical pancreatic cancer treatment. Nano Today 48, 101733 (2023). https://doi.org/10.1016/J.NANTOD.2022.101733
J. Verma, C. Warsame, R.K. Seenivasagam, N.K. Katiyar, E. Aleem, S. Goel, Nanoparticle-mediated cancer cell therapy: basic science to clinical applications. Cancer Metastasis Rev. 42, 601–627 (2023). https://doi.org/10.1007/S10555-023-10086-2
M.A.D. Machado, T.F. Moraes, B.H.L. Anjos, N.R.G. Alencar, T.-M.C. Chang, B.C.R.F. Santana, V.O. Menezes, L.O. Vieira, S.C.S. Brandão, M.A. Salvino, E.M. Netto, Association between increased subcutaneous adipose tissue radiodensity and cancer mortality: automated computation, comparison of cancer types, gender, and scanner bias. Appl. Radiat. Isotopes (2024). https://doi.org/10.1016/J.APRADISO.2024.111181
WHO (2022) Cancers. In: World Health Organization. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed 12 Jan 2024
L. Costa, R. Kumar, C. Villarreal-Garza, S. Sinha, S. Saini, J. Semwal, V. Saxsena, V. Zamre, M. Ray, C. Shimizu, L.H. Gusic, M. Toi, A. Lipton, Diagnostic delays in breast cancer among young women: an emphasis on healthcare providers. Breast (2023). https://doi.org/10.1016/J.BREAST.2023.103623
J. Xue, Z. Li, X. Li, C. Hua, P. Shang, J. Zhao, K. Liu, F. Xie, Evaluation of cigarette smoke-induced oxidative stress and inflammation in BEAS-2B cells based on a lung microfluidic chip. Food Chem. Toxicol. 176, 113787 (2023). https://doi.org/10.1016/J.FCT.2023.113787
I. Haq, T. Mazhar, R.N. Asif, Y.Y. Ghadi, N. Ullah, M.A. Khan, A. Al-Rasheed, YOLO and residual network for colorectal cancer cell detection and counting. Heliyon (2024). https://doi.org/10.1016/J.HELIYON.2024.E24403
J.L. Harcha, M. Tohme, J. Abraham, S. Vazhappilly, E.W. Walder, P. Kudalkar, A common malignancy with an uncommon behavior: prostate cancer with isolated pulmonary metastasis. Chest 164, A4373–A4374 (2023). https://doi.org/10.1016/j.chest.2023.07.2845
J.D. Mitchell, M. Laurie, Q. Xia, B. Dreyfus, N. Jain, A. Jain, D. Lane, D.J. Lenihan, Risk profiles and incidence of cardiovascular events across different cancer types. ESMO Open (2023). https://doi.org/10.1016/j.esmoop.2023.101830
M.S. Hussain, G. Gupta, M. Afzal, S.M. Alqahtani, V.P. Samuel, W. Hassan Almalki, I. Kazmi, S.I. Alzarea, S. Saleem, H. Dureja, S.K. Singh, K. Dua, L. Thangavelu, Exploring the role of lncrna neat1 knockdown in regulating apoptosis across multiple cancer types: a review. Pathol. Res. Pract. (2023). https://doi.org/10.1016/j.prp.2023.154908
İ Gül, İ Toygar, Ö. Usta Yeşilbalkan, Support needs of carers of cancer patients and the effects of the patient’s age and cancer type on their needs. Eur. J. Oncol. Nurs. (2024). https://doi.org/10.1016/j.ejon.2023.102468
K. Jorgensen, C. Denham, A. Kanbergs, C.F. Wu, R. Nitecki, N. Agusti, C. Meernik, A. Melamed, J.A. Rauh-Hain, All-cause and cancer-specific mortality after fertility-sparing surgery for stage IA and IC epithelial ovarian cancer. Gynecol. Oncol. 178, 60–68 (2023). https://doi.org/10.1016/j.ygyno.2023.09.015
X. Sun, S. Chen, G. Zhou, H. Cheng, Association between the dietary inflammatory index and all-cause mortality in the U.S. cancer survivors: a prospective cohort study using the national health and nutrition examination survey database. Prev. Med. Rep. (2023). https://doi.org/10.1016/j.pmedr.2023.102582
Y. Shionoya, M. Katsumata, H. Kasai, K. Shikano, A. Hino, M. Suzuki, M. Abe, T. Suzuki, Radiation-induced organizing pneumonia caused by carbon-ion radiotherapy for lung cancer. Radiol. Case Rep. 19, 567–571 (2024). https://doi.org/10.1016/j.radcr.2023.11.012
M.G. Akakpo, E. Owusu Roberts, R. Annobil, A.S. Aboagye, Perceptions about the causes and treatment of cancer—a cross-sectional survey of university students in Ghana. Prev. Med. Rep. (2023). https://doi.org/10.1016/j.pmedr.2023.102160
C. Fan, W. Zhu, Y. He, M. Da, The association between life’s essential 8 and all-cause, cancer and non-cancer mortality in US cancer survivors: a retrospective cohort study of NHANES. Prev. Med. (2024). https://doi.org/10.1016/J.YPMED.2024.107853
I. Gupta, O. Hussein, K.S. Sastry, S. Bougarn, N. Gopinath, E. Chin-Smith, Y. Sinha, H.M. Korashy, C. Maccalli, Deciphering the complexities of cancer cell immune evasion: mechanisms and therapeutic implications. Adv. Cancer Biol. Metastasis (2023). https://doi.org/10.1016/j.adcanc.2023.100107
Y. Chhabra, A.T. Weeraratna, Fibroblasts in cancer: unity in heterogeneity. Cell 186, 1580–1609 (2023). https://doi.org/10.1016/j.cell.2023.03.016
B.X. Wu, Z. Wu, Y.Y. Hou, Z.X. Fang, Y. Deng, H.T. Wu, J. Liu, Application of three-dimensional (3D) bioprinting in anti-cancer therapy. Heliyon (2023). https://doi.org/10.1016/j.heliyon.2023.e20475
W.M. Ciszewski, L.A. Wozniak, K. Sobierajska, SARS-CoV-2 S and N protein peptides drive invasion abilities of colon cancer cells through TGF-β1 regulation. Biochim. Biophys. Acta Mol. Cell Res. (2023). https://doi.org/10.1016/j.bbamcr.2023.119541
W.R. Kadhum, P. Ramaiah, N.A. Tayyib, A. Hjazi, A.J. Kahhharov, A.T. Alkhafaji, F.H. Al-Dami, B.M. Ridha, A.H. Alsalamy, M. Alwave, Novel and potential therapy options for a range of cancer diseases: using flavonoid. Pathol. Res. Pract. (2023). https://doi.org/10.1016/j.prp.2023.154997
Z. Cheng, M. Li, R. Dey, Y. Chen, Nanomaterials for cancer therapy: current progress and perspectives. J. Hematol. Oncol. (2021). https://doi.org/10.1186/S13045-021-01096-0
J.K. Patra, G. Das, L.F. Fraceto, E.V.R. Campos, M.D.P. Rodriguez-Torres, L.S. Acosta-Torres, L.A. Diaz-Torres, R. Grillo, M.K. Swamy, S. Sharma, S. Habtemariam, H.S. Shin, Nano based drug delivery systems: recent developments and future prospects. J. Nanobiotechnol. (2018). https://doi.org/10.1186/S12951-018-0392-8
B.K. Kashyap, V.V. Singh, M.K. Solanki, A. Kumar, J. Ruokolainen, K.K. Kesari, Smart nanomaterials in cancer theranostics: challenges and opportunities. ACS Omega 8, 14290–14320 (2023). https://doi.org/10.1021/ACSOMEGA.2C07840
M. Zhang, S. Gao, D. Yang, Y. Fang, X. Lin, X. Jin, Y. Liu, X. Liu, K. Su, K. Shi, Influencing factors and strategies of enhancing nanoparticles into tumors in vivo. Acta Pharm. Sin. B 11, 2265–2285 (2021). https://doi.org/10.1016/j.apsb.2021.03.033
N.S. Awad, N.M. Salkho, W.H. Abuwatfa, V. Paul, N.M. AlSawaftah, G.A. Husseini, Tumor vasculature vs tumor cell targeting: understanding the latest trends in using functional nanoparticles for cancer treatment. OpenNano (2023). https://doi.org/10.1016/j.onano.2023.100136
Y. Zi, K. Yang, J. He, Z. Wu, J. Liu, W. Zhang, Strategies to enhance drug delivery to solid tumors by harnessing the EPR effects and alternative targeting mechanisms. Adv. Drug Deliv. Rev. (2022). https://doi.org/10.1016/j.addr.2022.114449
M.F. Attia, N. Anton, J. Wallyn, Z. Omran, T.F. Vandamme, An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J. Pharm. Pharmacol. 71, 1185–1198 (2019). https://doi.org/10.1111/JPHP.13098
X. Shen, D. Pan, Q. Gong, Z. Gu, K. Luo, Enhancing drug penetration in solid tumors via nanomedicine: evaluation models, strategies and perspectives. Bioact. Mater. 32, 445–472 (2024). https://doi.org/10.1016/j.bioactmat.2023.10.017
J. Choi, E. Choi, D. Choi, The ambivalent nature of the relationship between lymphatics and cancer. Front. Cell Dev. Biol. (2022). https://doi.org/10.3389/FCELL.2022.931335
R. Baghban, L. Roshangar, R. Jahanban-Esfahlan, K. Seidi, A. Ebrahimi-Kalan, M. Jaymand, S. Kolahian, T. Javaheri, P. Zare, Tumor microenvironment complexity and therapeutic implications at a glance. Cell Commun. Signal. (2020). https://doi.org/10.1186/S12964-020-0530-4
L. Garnier, A.O. Gkountidi, S. Hugues, Tumor-associated lymphatic vessel features and immunomodulatory functions. Front. Immunol. (2019). https://doi.org/10.3389/FIMMU.2019.00720
S. Rajput, P. Kumar Sharma, R. Malviya, Fluid mechanics in circulating tumour cells: role in metastasis and treatment strategies. Med. Drug Discov. (2023). https://doi.org/10.1016/j.medidd.2023.100158
S. Waheed, Z. Li, F. Zhang, A. Chiarini, U. Armato, J. Wu, Engineering nano-drug biointerface to overcome biological barriers toward precision drug delivery. J. Nanobiotechnol. (2022). https://doi.org/10.1186/S12951-022-01605-4
D. Shi, D. Beasock, A. Fessler, J. Szebeni, J.Y. Ljubimova, K.A. Afonin, M.A. Dobrovolskaia, To PEGylate or not to PEGylate: immunological properties of nanomedicine’s most popular component, polyethylene glycol and its alternatives. Adv. Drug Deliv. Rev. 180, 114079 (2022). https://doi.org/10.1016/j.addr.2021.114079
M. Xu, X. Han, H. Xiong, Y. Gao, B. Xu, G. Zhu, J. Li, Cancer nanomedicine: emerging strategies and therapeutic potentials. Molecules 28, 5145 (2023). https://doi.org/10.3390/molecules28135145
M.J. Bigaj-Józefowska, E. Coy, K. Załęski, T. Zalewski, M. Grabowska, K. Jaskot, P. Perrigue, R. Mrówczyński, B.F. Grześkowiak, Biomimetic theranostic nanoparticles for effective anticancer therapy and MRI imaging. J. Photochem. Photobiol. B. 249, 112813 (2023). https://doi.org/10.1016/j.jphotobiol.2023.112813
T. Yin, Z. Chen, Z. Wei, Y. Lu, R. Aikebaier, Y. Chen, Iron-poly(tannic acid) biomimetic nanoparticles for targeted magnetic resonance imaging and drug delivery. Chin. J. Anal. Chem. 51, 100331 (2023). https://doi.org/10.1016/J.CJAC.2023.100331
J. Tang, Z. Yang, Y. Zhang, R. Huang, C. Yu, C. Yu, Preparation of PEGylated nedaplatin liposomes with sustained release behavior for enhancing the antitumor efficacy of non-small cell lung cancer. Int. J. Pharm. 635, 122708 (2023). https://doi.org/10.1016/j.ijpharm.2023.122708
T. Waghule, K. Laxmi Swetha, A. Roy, R. Narayan Saha, G. Singhvi, Exploring temozolomide encapsulated PEGylated liposomes and lyotropic liquid crystals for effective treatment of glioblastoma: in-vitro, cell line, and pharmacokinetic studies. Eur. J. Pharm. Biopharm. 186, 18–29 (2023). https://doi.org/10.1016/J.EJPB.2023.03.004
N. Thakur, S. Thakur, S. Chatterjee, J. Das, P.C. Sil, Nanoparticles as smart carriers for enhanced cancer immunotherapy. Front. Chem. (2020). https://doi.org/10.3389/FCHEM.2020.597806
N.T. Trac, E.J. Chung, Peptide-based targeting of immunosuppressive cells in cancer. Bioact. Mater. 5, 92–101 (2020). https://doi.org/10.1016/j.bioactmat.2020.01.006
J. Zhang, J. Shang, X. Tang, X. Xu, TfR Aptamer-functionalized MSNs for enhancing targeted cellular uptake and therapy of cancer cells. ACS Omega (2023). https://doi.org/10.1021/ACSOMEGA.3C06562
A.A.H. Abdellatif, H.A. Mohammed, R.A. Khan, V. Singh, A. Bouazzaoui, M. Yusuf, N. Akhtar, M. Khan, A. Al-Subaiyel, S.A.A. Mohammed, M.S. Al-Omar, Nano-scale delivery: a comprehensive review of nano-structured devices, preparative techniques, site-specificity designs, biomedical applications, commercial products, and references to safety, cellular uptake, and organ toxicity. Nanotechnol. Rev. 10, 1493–1559 (2021). https://doi.org/10.1515/NTREV-2021-0096/PDF
D. Dehaini, R.H. Fang, L. Zhang, Biomimetic strategies for targeted nanoparticle delivery. Bioeng. Transl. Med. 1, 30–46 (2016). https://doi.org/10.1002/BTM2.10004
L.D. Di Filippo, S.G. de Carvalho, J.L. Duarte, M.T. Luiz, J.A. Paes Dutra, G.A. de Paula, M. Chorilli, J. Conde, A receptor-mediated landscape of druggable and targeted nanomaterials for gliomas. Mater. Today Bio (2023). https://doi.org/10.1016/j.mtbio.2023.100671
P. Shi, Z. Cheng, K. Zhao, Y. Chen, A. Zhang, W. Gan, Y. Zhang, Active targeting schemes for nano-drug delivery systems in osteosarcoma therapeutics. J. Nanobiotechnol. (2023). https://doi.org/10.1186/S12951-023-01826-1
T.D. Clemons, R. Singh, A. Sorolla, N. Chaudhari, A. Hubbard, K.S. Iyer, Distinction between active and passive targeting of nanoparticles dictate their overall therapeutic efficacy. Langmuir 34, 15343–15349 (2018)
D. Zheng, P. Yu, Z. Wei, C. Zhong, M. Wu, X. Liu, RBC membrane camouflaged semiconducting polymer nanoparticles for near-infrared photoacoustic imaging and photothermal therapy. Nanomicro. Lett. (2020). https://doi.org/10.1007/S40820-020-00429-X
P. Ebrahimnejad, A. Sodagar Taleghani, K. Asare-Addo, A. Nokhodchi, An updated review of folate-functionalized nanocarriers: a promising ligand in cancer. Drug Discov. Today 27, 471–489 (2022). https://doi.org/10.1016/j.drudis.2021.11.011
Q. Chen, X. Zhang, G. Ding, Y. Ma, M. Zhou, Y. Zhang, Preparation and biological evaluation of antibody targeted metal-organic framework drug delivery system (TDDS) in Her2 receptor-positive cells. Talanta 269, 125380 (2024). https://doi.org/10.1016/j.talanta.2023.125380
K. Kumar, S.G. Rawat, M.M. Manjit, K.A. Priya, R. Chawla, Dual targeting pH responsive chitosan nanoparticles for enhanced active cellular internalization of gemcitabine in non-small cell lung cancer. Int. J. Biol. Macromol. 249, 126057 (2023). https://doi.org/10.1016/j.ijbiomac.2023.126057
N. Rajana, P. Sandeep Chary, V. Bhavana, R. Deshmukh, K. Dukka, A. Sharma, N. Kumar Mehra, Targeted delivery and apoptosis induction of CDK-4/6 inhibitor loaded folic acid decorated lipid-polymer hybrid nanoparticles in breast cancer cells. Int. J. Pharm. 651, 123787 (2024). https://doi.org/10.1016/j.ijpharm.2024.123787
Y. Liu, Z. Dai, J. Wang, Y. Tu, L. Zhu, Folate-targeted pH-sensitive bortezomib conjugates for cancer treatment. Chem. Commun. 55, 4254–4257 (2019). https://doi.org/10.1039/C9CC01344J
W. Xiao, L. Zhao, Y. Sun, X. Yang, Q. Fu, Stimuli-responsive nanoradiosensitizers for enhanced cancer radiotherapy. Small Methods (2023). https://doi.org/10.1002/SMTD.202301131
N. Khanna, T. Chatterji, S. Singh, S. Pandey, Application of stimuli responsive nanocomposites in drug delivery and theranostics to counter cancer proliferation and drug resistance. J. Drug Deliv. Sci. Technol. 88, 104958 (2023). https://doi.org/10.1016/j.jddst.2023.104958
M. Zhang, W. Hu, C. Cai, Y. Wu, J. Li, S. Dong, Advanced application of stimuli-responsive drug delivery system for inflammatory arthritis treatment. Mater. Today Bio (2022). https://doi.org/10.1016/j.mtbio.2022.100223
S. Bhattacharya, B.G. Prajapati, S. Singh, A critical review on the dissemination of PH and stimuli-responsive polymeric nanoparticular systems to improve drug delivery in cancer therapy. Crit. Rev. Oncol. Hematol. 185, 103961 (2023). https://doi.org/10.1016/j.critrevonc.2023.103961
L. Li, J. Wang, H. Kong, Y. Zeng, G. Liu, Functional biomimetic nanoparticles for drug delivery and theranostic applications in cancer treatment. Sci. Technol. Adv. Mater. 19, 771–790 (2018). https://doi.org/10.1080/14686996.2018.1528850
D. Mandal, K. Kushwaha, J. Gupta, Emerging nano-strategies against tumour microenvironment (TME): a review. OpenNano (2023). https://doi.org/10.1016/j.onano.2022.100112
T. Alejo, V. Sebastian, G. Mendoza, M. Arruebo, Hybrid thermoresponsive nanoparticles containing drug nanocrystals for NIR-triggered remote release. J. Colloid Interface Sci. 607, 1466–1477 (2022). https://doi.org/10.1016/j.jcis.2021.09.064
P. Liu, Y. Huang, C. Zhan, F. Zhang, C. Deng, Y. Jia, T. Wan, S. Wang, B. Li, Tumor-overexpressed enzyme responsive amphiphiles small molecular self-assembly nano-prodrug for the chemo-phototherapy against non-small-cell lung cancer. Mater. Today Bio 21, 100722 (2023). https://doi.org/10.1016/j.mtbio.2023.100722
H. Shah, A. Madni, N. Filipczak, N. Jan, M.M. Khan, S. Khan, A. Basit, A. Shafiq, N. Rai, S.S.K. Yalamarty, V. Torchilin, Cisplatin-loaded thermoresponsive liposomes for enhanced anticancer efficacy. J. Drug Deliv. Sci. Technol. (2023). https://doi.org/10.1016/j.jddst.2023.104509
A. Valizadeh, S. Asghari, S. Abbaspoor, A. Jafari, M. Raeisi, Y. Pilehvar, Implantable smart hyperthermia nanofibers for cancer therapy: challenges and opportunities. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. (2023). https://doi.org/10.1002/WNAN.1909
H. Shah, A. Madni, N. Filipczak, N. Jan, M.M. Khan, S. Khan, A. Basit, A. Shafiq, N. Rai, S.S.K. Yalamarty, V. Torchilin, Cisplatin-loaded thermoresponsive liposomes for enhanced anticancer efficacy. J. Drug Deliv. Sci. Technol. 84, 104509 (2023). https://doi.org/10.1016/J.JDDST.2023.104509
B. El Hassouni, C. Granchi, A. Vallés-Martí, I.G.P. Supadmanaba, G. Bononi, T. Tuccinardi, N. Funel, C.R. Jimenez, G.J. Peters, E. Giovannetti, F. Minutolo, The dichotomous role of the glycolytic metabolism pathway in cancer metastasis: interplay with the complex tumor microenvironment and novel therapeutic strategies. Semin. Cancer Biol. 60, 238–248 (2020). https://doi.org/10.1016/J.SEMCANCER.2019.08.025
J. Li, W. Ke, L. Wang, M. Huang, W. Yin, P. Zhang, Q. Chen, Z. Ge, Self-sufficing H2O2-responsive nanocarriers through tumor-specific H2O2 production for synergistic oxidation-chemotherapy. J. Control. Release 225, 64–74 (2016). https://doi.org/10.1016/j.jconrel.2016.01.029
E. Issaka, J.N.O. Amu-Darko, M. Adams, S. Yakubu, E. Gyimah, N. Ali, J. Cui, M. Bilal, Zinc imidazolate metal-organic frameworks-8-encapsulated enzymes/nanoenzymes for biocatalytic and biomedical applications. Catal. Lett. 153, 2083–2106 (2022). https://doi.org/10.1007/S10562-022-04140-X
W. Li, T. Ma, T. He, Y. Li, S. Yin, Cancer cell membrane–encapsulated biomimetic nanoparticles for tumor immuno-photothermal therapy. Chem. Eng. J. 463, 142495 (2023). https://doi.org/10.1016/J.CEJ.2023.142495
G. Lu, X. Wang, F. Li, S. Wang, J. Zhao, J. Wang, J. Liu, C. Lyu, P. Ye, H. Tan, W. Li, G. Ma, W. Wei, Engineered biomimetic nanoparticles achieve targeted delivery and efficient metabolism-based synergistic therapy against glioblastoma. Nat. Commun. 13, 4214 (2022). https://doi.org/10.1038/s41467-022-31799-y
C. Xiao, C. Tong, J. Fan, Z. Wang, Q. Xie, Y. Long, P. You, W. Wang, B. Liu, Biomimetic nanoparticles loading with gamabutolin-indomethacin for chemo/photothermal therapy of cervical cancer and anti-inflammation. J. Control. Release 339, 259–273 (2021). https://doi.org/10.1016/j.jconrel.2021.09.034
J. Lopes, D. Lopes, M. Pereira-Silva, D. Peixoto, F. Veiga, M.R. Hamblin, J. Conde, C. Corbo, E.N. Zare, M. Ashrafizadeh, F.R. Tay, C. Chen, R.F. Donnelly, X. Wang, P. Makvandi, A.C. Paiva-Santos, Macrophage cell membrane-cloaked nanoplatforms for biomedical applications. Small Methods (2022). https://doi.org/10.1002/SMTD.202200289
Y. Wu, S. Wan, S. Yang, H. Hu, C. Zhang, J. Lai, J. Zhou, W. Chen, X. Tang, J. Luo, X. Zhou, L. Yu, L. Wang, A. Wu, Q. Fan, J. Wu, Macrophage cell membrane-based nanoparticles: a new promising biomimetic platform for targeted delivery and treatment. J. Nanobiotechnol. (2022). https://doi.org/10.1186/S12951-022-01746-6
X. Li, Y. Lin, Z. Yang, L. Guan, Z. Wang, A. Liu, B. Yang, L. Tang, Q. Lin, Cancer cell membrane biomimetic nanosystem for homologous targeted dual-mode imaging and combined therapy. J. Colloid Interface Sci. 652, 770–779 (2023). https://doi.org/10.1016/j.jcis.2023.08.109
M. Li, Q. Guo, C. Zhong, Z. Zhang, Multifunctional cell membranes-based nano-carriers for targeted therapies: a review of recent trends and future perspective. Drug Deliv. (2023). https://doi.org/10.1080/10717544.2023.2288797
H. Lu, Y. Wang, R. Yu, Immune cell membrane-coated nanoparticles for targeted myocardial ischemia/reperfusion injury therapy. Innov. Med. 1, 100015 (2023). https://doi.org/10.59717/J.XINN-MED.2023.100015
H. Han, R. Bártolo, J. Li, M.A. Shahbazi, H.A. Santos, Biomimetic platelet membrane-coated nanoparticles for targeted therapy. Eur. J. Pharm. Biopharm. 172, 1–15 (2022). https://doi.org/10.1016/j.ejpb.2022.01.004
J. Peng, J. Zhou, R. Sun, Y. Chen, D. Pan, Q. Wang, Y. Chen, Z. Gong, Q. Du, Dual-targeting of artesunate and chloroquine to tumor cells and tumor-associated macrophages by a biomimetic PLGA nanoparticle for colorectal cancer treatment. Int. J. Biol. Macromol. 244, 125163 (2023). https://doi.org/10.1016/j.ijbiomac.2023.125163
Y. Miao, Y. Yang, L. Guo, M. Chen, X. Zhou, Y. Zhao, D. Nie, Y. Gan, X. Zhang, Cell membrane-camouflaged nanocarriers with biomimetic deformability of erythrocytes for ultralong circulation and enhanced cancer therapy. ACS Nano 16, 6527–6540 (2022)
X. Cao, Y. Hu, S. Luo, Y. Wang, T. Gong, X. Sun, Y. Fu, Z. Zhang, Neutrophil-mimicking therapeutic nanoparticles for targeted chemotherapy of pancreatic carcinoma. Acta Pharm. Sin. B 9, 575–589 (2019). https://doi.org/10.1016/J.APSB.2018.12.009
H.-Y. Chen, J. Deng, Y. Wang, C.-Q. Wu, X. Li, H.-W. Dai, Hybrid cell membrane-coated nanoparticles: a multifunctional biomimetic platform for cancer diagnosis and therapy. Acta Biomater. 112, 1–13 (2020). https://doi.org/10.1016/j.actbio.2020.05.028
Y. Zou, Y. Sun, Y. Wang, D. Zhang, H. Yang, X. Wang, M. Zheng, B. Shi, Cancer cell-mitochondria hybrid membrane coated Gboxin loaded nanomedicines for glioblastoma treatment. Nat. Commun. 14, 4557 (2023). https://doi.org/10.1038/s41467-023-40280-3
Q. Xie, B. Li, J. Fan, J. Liang, S. Jiang, Y. Qin, L. Jiang, J. Cui, X. Nie, S. Sun, B. Liu, W. Wang, Biomimetic hybrid-cell membrane nanoparticles loaded with panaxytriol for breast cancer combinational therapy. Mater. Des. 223, 111219 (2022). https://doi.org/10.1016/J.MATDES.2022.111219
M.J.W. Evers, S.I. van de Wakker, E.M. de Groot, O.G. de Jong, J.J.J. Gitz-François, C.S. Seinen, J.P.G. Sluijter, R.M. Schiffelers, P. Vader, Functional siRNA delivery by extracellular vesicle-liposome hybrid nanoparticles. Adv. Healthc. Mater. (2022). https://doi.org/10.1002/ADHM.202101202
D. Wang, C. Liu, S. You, K. Zhang, M. Li, Y. Cao, C. Wang, H. Dong, X. Zhang, Bacterial vesicle-cancer cell hybrid membrane-coated nanoparticles for tumor specific immune activation and photothermal therapy. ACS Appl. Mater. Interfaces 12, 41138–41147 (2020). https://doi.org/10.1021/acsami.0c13169
M. Zhou, X. He, C. Mei, C. Ou, Exosome derived from tumor-associated macrophages: biogenesis, functions, and therapeutic implications in human cancers. Biomark Res. (2023). https://doi.org/10.1186/S40364-023-00538-W
K. Lou, S. Feng, H. Luo, J. Zou, G. Zhang, X. Zou, Extracellular vesicles derived from macrophages: current applications and prospects in tumors. Front. Bioeng. Biotechnol. (2022). https://doi.org/10.3389/FBIOE.2022.1097074
C. Gong, X. Yu, B. You, Y. Wu, R. Wang, L. Han, Y. Wang, S. Gao, Y. Yuan, Macrophage-cancer hybrid membrane-coated nanoparticles for targeting lung metastasis in breast cancer therapy. J. Nanobiotechnol. 18, 92 (2020). https://doi.org/10.1186/s12951-020-00649-8
R. Rampado, S. Crotti, P. Caliceti, S. Pucciarelli, M. Agostini, Recent Advances in understanding the protein corona of nanoparticles and in the formulation of “stealthy” nanomaterials. Front. Bioeng. Biotechnol. (2020). https://doi.org/10.3389/FBIOE.2020.00166
M. Heidarzadeh, A. Zarebkohan, R. Rahbarghazi, E. Sokullu, Protein corona and exosomes: new challenges and prospects. Cell Commun. Signal. (2023). https://doi.org/10.1186/S12964-023-01089-1
J.M. Metselaar, T. Lammers, Challenges in nanomedicine clinical translation. Drug Deliv. Transl. Res. 10, 721–725 (2020). https://doi.org/10.1007/S13346-020-00740-5
D. Huo, X. Jiang, Y. Hu, Recent advances in nanostrategies capable of overcoming biological barriers for tumor management. Adv. Mater. (2020). https://doi.org/10.1002/ADMA.201904337
P.M. Glassman, J.W. Myerson, L.T. Ferguson, R.Y. Kiseleva, V.V. Shuvaev, J.S. Brenner, V.R. Muzykantov, Targeting drug delivery in the vascular system: focus on endothelium. Adv. Drug Deliv. Rev. 157, 96–117 (2020). https://doi.org/10.1016/j.addr.2020.06.013
S.M. Neetika, P. Thakur, P. Gaur, G.M. Rani, S. Rustagi, R.K. Talreja, V. Chaudhary, Cancer treatment and toxicity outlook of nanoparticles. Environ. Res. 237, 116870 (2023). https://doi.org/10.1016/j.envres.2023.116870
Y. Cong, D. Baimanov, Y. Zhou, C. Chen, L. Wang, Penetration and translocation of functional inorganic nanomaterials into biological barriers. Adv. Drug Deliv. Rev. 191, 114615 (2022). https://doi.org/10.1016/j.addr.2022.114615
X. Cheng, Q. Xie, Y. Sun, Advances in nanomaterial-based targeted drug delivery systems. Front. Bioeng. Biotechnol. (2023). https://doi.org/10.3389/FBIOE.2023.1177151
Y. Wenqi, W. Lingxi, A. Mehmood, W. Shah, Nanotechnology-enabled therapies improve blood-brain barrier challenges in brain tumor. Int. J. Polym. Mater. Polym. Biomater. (2023). https://doi.org/10.1080/00914037.2023.2291105
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
EI contributed towards conceptualization, methodology, investigation, data curation, writing-original draft, writing- review, and supervision; JNOA-D contributed towards resources, formal analysis, writing-original draft, and writing- review.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Issaka, E., Amu-Darko, J.N.O. Biomimetic Nanoparticles for Cancer Therapy: A Review of Recent Advances, Applications, and Bottlenecks. Biomedical Materials & Devices (2024). https://doi.org/10.1007/s44174-024-00179-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44174-024-00179-z