Abstract
Nanostructured inorganic biomaterial emerged as the most essential platform to address traumatic and non-traumatic conditions of hard tissues in the current scenario. Synthetic inorganic biomaterials serve as an efficient and pathogen-free choice that overcomes the obstructions associated with autografts and allografts to promote new tissue regeneration, since nano-hydroxyapatite (nHAp) is a biomaterial that mimics the natural mineral composition of bones and teeth of human hard tissues, which is widely employed in orthopedics and dentistry. The nHAp-based materials exhibit bioactive, biocompatible, and osteoconductive features under in vitro and in vivo conditions. The brittle nature of synthetic nHAp leads to weak mechanical properties, which eventually confines the utility of nHAp in load-bearing applications. Hence, this review focuses on the recent trends in the fabrication and investigation of nHAp-based polymer nanocomposite scaffolds for bone regeneration. Employing different polymers and fabrication strategies would efficiently tailor the physicochemical properties, and tailor-made mechanical properties in competence with biodegradation, thereby enhancing their potential in biomedical utility, and exploring their efficacy under in vitro and in vivo conditions to make “HAp-based smart-biomaterials” for bone tissue engineering.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Restoration of osseous defects caused by traumatic and non-traumatic cases remains a major mission in orthopedic and dental surgery. The need for the restoration and replacement of injured and diseased bone tissue has been drastically amplified with the increasing average age of the population worldwide. Since there are plenty of conflicts associated with existing current “gold standard” routes and therapy, osseous repair necessitates instantaneous post-operative fixation to endorse and direct the healing of bone which has to be considered [1, 2]. In some cases, the bone healing process cannot be readily compromised by post-surgical microbial contamination (infection) or by foreign body response to the metal substitutes used for fixation. In certain cases, utilization of autografts for major bone defect repair, considerable morbidity at the donor site may occur [3, 4]. Moreover, autografts are associated with immune response, and certain osteomyelitis causes infectious diseases leading to complications in new bone formations. In the case of allografts or xenografts, it also encounters graft rejection, which further elicits the transfer of infection from the donor or elicits immunological reactions from the host [3, 4]. Hence, the need has been raised to regenerate damaged tissue with minimal pathogenic infections, and for successful tissue regeneration in a controlled manner.
Exploring the influence of HAp with biological systems paves the interesting initiative to acquire knowledge about its potential contribution to the growing economy worldwide. However, hydroxyapatite (HAp) has gained great attention in wide applications, such as bone tissue engineering (BTE), wound healing and management, drug delivery, bioimaging, and environmental remediation applications [5–11]. Among these, BTE is one such prominent field that is highly amazed by the biological performance of HAp. Based on this, hence, there is a rising demand for state-of-the-art reviews which consider predominantly current and emerging research on HAp in BTE. This article reviews the recent progress of nanostructured HAp-based nanocomposite scaffolds for bone tissue engineering. The review starts with highlighting the characteristics and properties of HAp, the importance of nanoscale HAp (nHAp), the significance of inorganic and organic composite scaffolds, the role of nHAp in BTE application, and the limitations of synthetic nHAp. In the next section, the development of varying combinations of natural polymers with nHAp and their potential outcomes, and shortcomings in BTE are discussed. A schematic representation of the outline of the review is illustrated in Fig. 1. The article concludes with the future outlook for bone regeneration, and so on.
Bone tissue engineering
BTE is an interdisciplinary area, which implies the ideology or principles of science and engineering to heal the defective site with its biochemical functionalities via restoration, maintenance, or improvement of the hard tissue [12, 13]. One of the major favorable approaches for controlled tissue regeneration is the utilization of structural support, which facilitates the healing and rejuvenation of damaged biological tissues. Indeed, biological cells can be implanted into a synthetic substrate, so-called scaffolds that assist the formation of three-dimensional (3D) tissue [12].
In this regard, the regeneration of complex hard tissue necessitates a material with remarkable features. Such inadequacies can come across the developments in synthetic biomaterials with admirable physicochemical and biological properties such as non-toxic, non-allergic, non-immunogenic, and non-inflammatory, and bio-functionality while implanted in vivo. Until now, several synthetic biomaterials like gypsum (calcium sulfates), calcium phosphates, bioactive glasses, polymers, etc., are being widely utilized in BTE [14–19]. Among them, varying types of calcium phosphates (especially HAp) have attracted much researchers’ attention [6, 12, 13].
Calcium phosphates
Calcium phosphates (CPs) are a privileged category of bioceramics due to their excellent biocompatible, bioactive, osteoconductive, and biodegradable properties [20, 21]. CPs can be classified into many types depending on their Ca/P ratio, which includes dicalcium phosphate (Ca/P = 1), tricalcium phosphate (Ca/P = 1.5), tetra-calcium phosphate (Ca/P = 2), octa-calcium phosphate (Ca/P = 1.33), hydroxyapatite (Ca/P = 1.67), etc., and are shown in Fig. 2. Calcium phosphates including tricalcium phosphate, tetra-calcium phosphates, and synthetic hydroxyapatite (HAp), etc., are of meticulous worth and bring forth a broad break in bone regeneration therapy [20–22].
Based on the resorption rate and dissolving behavior, CPs can be ordered while exposed to the physiological milieu as tetra-calcium phosphate > amorphous calcium phosphate > α-tri-calcium phosphate > β-tri-calcium phosphate > HAp [23, 24]. The solubility order revealed that HAp has minimal resorbability when compared to other CPs. Characteristics of HAp and other CPs are displayed in Table 1. Dissimilar to other CPs, HAp does not dissociate under physiological conditions, thus suggesting that it is thermodynamically stable in the physiological environment (pH) and so effectively contributes bioactivity through the strong chemical bond formation with surrounding host hard tissue. Moreover, HAp possesses a chemical resemblance with the natural inorganic phase, and the structure of HAp is shown in Fig. 3. Therefore, HAp is considered a prominent, gold-standard biomaterial for the regeneration of hard tissues like bones and teeth [23–25].
Need of nano-hydroxyapatite (nHAp)
Recently, nanoscale HAp (nHAp) had a great interest in biomedical research due to its admirable surface properties compared to its microscale and bulk counterpart [26]. In addition to BTE, nHAp has been employed in several rationales such as dental implant coatings, drug delivery, bioimaging, water decontamination, and soil treatment. Owing to its ample roles in the biomedical field, especially in BTE (osteogenesis), nHAp has been extensively investigated by several researchers [5–11]. Nanocrystalline HAp possesses enhanced sinterability and improved densification owing to its higher surface area, and thus may enhance fracture toughness and mechanical properties [27]. Furthermore, nHAp is expected to provide enhanced bioactivity compared to bulk/macro/microscale HAp [28]. When compared to conventional HAp, nHAp offers efficient osteoblast adhesion, differentiation, and proliferation that lead to bone regeneration within a short duration [29–31]. The nHAp has superior surface properties such as high surface area and surface roughness, which assist cell attachment and favor interaction host tissue for long-term utility and efficient BTE that is the necessary concern [32, 33]. One of the main factors of biomaterial is the high surface area that influences cellular adhesion and improved the density of cells. Another important characteristic is the surface roughness that is essential for host tissue interactions. It has been assumed that cell–matrix interactions are facilitated by surface properties and the essential interactions take place within 1 nm of the biomaterial surface [32, 33].
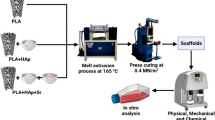
Preparation methods of HAp
So far, several routes were adopted to synthesize HAp with specific control of its structure, morphology, and size distribution. In agreement to Sadat-Shojai et al. [33], (i) dry methods, (ii) wet route, (iii) high-temperature routes, (iv) HAp derived from biogenic sources, and (v) combination methods were reported (Fig. 4). Among these, wet chemistry is one of the familiar routes followed using different solvents, varying temperatures, diverse chemical precursors, etc., that are being utilized in the wet chemical synthesis of HAp. Several additives are commonly applied to control parameters. Chemical precipitation is a simple and feasible route to produce fine-sized HAp nanoparticles [33]. In the sol–gel route, the sol is a form of a colloidal suspension of alkoxides, then forms gelation, aged, dried, and calcinated to remove by-products [34]. In hydrothermal synthesis, chemical precipitation occurs at higher temperatures along with pressure developed inside a closed environment. The sonochemical method takes place in the presence of ultrasound waves passed through chemical precursors, which allows the formation of the homogenous size distribution of HAp particles [35]. Inhibition of agglomeration and control over morphology and size of the particles are carried out in the emulsion route using different surfactants [36].
Schematic representation of different preparation methods of HAp [33]
Clinical demands for BTE
In most developed countries, osteoporosis condition and its associated consequences are taking up to 15% of the cost of health care services. Such disbursement is likely to rise due to fracture, which is caused by growing numbers of cases in load-bearing bones due to osteoporosis, obesity, falls, accidental situations, and so on [37]. Estimated hip fractures are 1.6 million worldwide, and it has been predicted to be 6.3 million by 2050 [38]. Fractures are majorly occurring in Asia, where around 50% of the patients may reside because of the population demographic changes. Specifically, India and China contain ~ 37% of the world’s population [39]. Such a situation consequently demands researchers’ attention on cost-effective treatments; therefore, the attention is not only to orthopedic surgeons but also to scientists.
Significance of inorganic–organic nanocomposite scaffolds
As the human bone tissue is a natural nanocomposite, the organic phase of collagen fibrils is infused with the inorganic phase nHAp [40, 41]. The nanocrystalline HAp offers stiffness and strength, whereas organic collagen fibrils provide flexibility to the bone. The amalgamation of both inorganic and organic phases collectively affords mechanical support and dynamic resilience to the skeleton of the body [40, 41]. Essentially, 70% of natural human bone comprised nanocrystalline hydroxyapatite (nHAp), which is around 20–80 nm in length and 2–5 nm in width ranges [41, 42]. However, synthetic HAp has a chemical resemblance to natural bone mineral; its usage is limited in clinical applications owing to its poor mechanical strength [6]. Hence, different forms of HAp-based nanocomposites have been developed to enhance their mechanical properties. The development of synthetic nHAp (inorganic)-polymer (organic) composite scaffolds is an excellent strategy to mimic the inorganic–organic phase of natural bone to achieve improved mechanical properties. Therefore, designing the combinatorial properties of both nHAp and polymer (either natural or synthetic) with controlled features may serve as suitable scaffolds to direct the regeneration of bone tissue at the defective site.
Design of scaffolds
Many fabrication strategies are employed for the preparation of nanocomposite scaffolds, which are stimulated by natural bone characteristics. A few important characteristics of scaffold materials are schematically displayed in Fig. 5. Among these, bioactivity is one of the necessary features to create a chemical bond with natural bone. The schematic representation (Fig. 6) depicts the in vitro apatite layer formation, which facilitates the chemical bonding of nHAp with host bone for efficient osteointegration [30, 31].
The flexibility of natural bone is due to its unique microstructure, since bone consists of both organic collagen fibrils and inorganic HAp, which provide flexibility and rigidity that maintain the dynamic functioning of bone [40, 41]. Similar principles can be taken into account during the designing of nanocomposite scaffolds that include parallel fibrillar arrays and lamination, therefore considering the vital biological characteristics of living bone and transformation of the strategy to engineer BTE scaffolds. Since the exclusive combination of organic and inorganic fractions affords stiffness with dynamic flexibility, and thus reduces the probability of fractures under normal loading situations, an analogous approach can be employed in BTE to obtain the essential resistance against compressive and tensile forces. Biological features like biocompatibility, bioactivity, and osteoconductivity are taken into account in addition to physical factors. Thus, the scaffold may have the potential to encourage the adhesion and differentiation of osteoblast cells for successful BTE [40, 41]. Several factors, which include functional groups, surface energy, surface area, hydrophilicity, and conjugants, may also have an impact on the BTE ability of scaffolds [42].
Scaffold architecture
The nanocomposite scaffolds should have porous architecture, and bioactive and biocompatible features to interact with the surrounding host environment. It is found that the characteristics of scaffolds include 3D architecture, enhanced biocompatibility, interconnected porosity, improved mechanical strength, and facile interactions with the surrounding environment which are highly desirable to aid the formation of new bone tissue [43, 44].
In BTE, the pore structure and pore size of the scaffolds play a crucial role. The cell adhesion, migration, and transfer of nutrients are solely dependent on the porous structure with an interconnected pore architecture. The scaffolds’ very small pore size obstructs the migration of the cell into its interior, thus consequently cells aggregated on the exterior of the scaffold’s surface. This causes essential nutrient depletion, which further leads to necrotic performance. In contrast, the very huge pore structure of the scaffold decreases surface area, eventually hindering the cell adhesion and spreading of cells to its interior [45–47]. Hence, the demand has been elevated to attain a balance between surface area and specific optimal pore size which is a crucial requirement for tissue regeneration [46, 47]. M. Sous et al. report 100–800 μm was the optimal pore diameter range for BTE [48]. Few reports recommended that a 100–250 μm range of pore size is necessary for BTE. Nonetheless, the nominal pore size of ~ 100 μm can be an essential requirement for efficient cellular adhesion and regeneration [48].
Fabrication of composite scaffolds
Different fabrication techniques have been adopted to fabricate HAp and other calcium phosphates (CaP) based polymer composite scaffolds. Among them, freeze drying, particulate leaching, electrospinning, gas foaming, biomimetic, solvent casting, selective laser sintering, 3D printing, etc., are common techniques to attain tailormade composite scaffolds [49–52].
Many scaffolds were prepared by freeze-drying or lyophilization route that offers small porous architecture with poor interconnectivity and poor mechanical property. Weak interfacial bonding between CaP particles and chitosan leads to deprived mechanical strength [53] and poor interaction of CaP with chitosan matrix results loosening of particles from the polymer matrix and further inflammation and tissue grievance [54]. In Zhang and Zhang’s report, lyophilized chitosan and β-tricalcium phosphate scaffold with a stronger compressive modulus 1–3 MPa than relative chitosan scaffolds but remarkably poorer than human cancellous bone [55]. However, lyophilized chitosan/nHAp composites achieved ~ 95% porosity with 20 to 60 μm pore size and higher proliferation rate osteoblasts compared to pure chitosan scaffolds [56]. Lei et al. developed natural bone ceramic (NBC)/collagen and HAp/collagen composites scaffolds via glutaraldehyde cross-linking and freeze-drying. NBC/collagen and HAp/collagen promoted the expression of early-stage and late-stage osteogenic genes respectively and also had varying influences on the duration of MC3T3-E1 cell mineralization. In terms of mechanical behavior, nHAp/collagen scaffolds showed 7.9 ± 0.2 MPa of Young’s modulus which was higher than NBC/collagen (5.1 ± 0.7 MPa). [57]
Significance of biodegradation
As biodegradability is the crucial factor for outstanding biocompatible scaffolds over time during in vivo implantation, however, the mechanical, biological, and physicochemical features determine the degradation rate of the material. Absorption kinetics of scaffolds is necessary and depends on the regeneration of tissues. If a scaffold is employed for bone regeneration application, deterioration of the scaffold takes place in a relatively gradual manner; still, the mechanical strength should be retained before the reconstruction of nearly new tissue completion [58]. For instance, scaffolds should not last more than 1 month in skin tissue regeneration. If the scaffolds last more than the required period, the retained material can retard rather than assists tissue regeneration. The gradual breakdown of biomaterial aided by specific biochemical activity implies the term biodegradation. Especially, if the breakdown is mediated by cells or tissue activity, the material is known as biodegradable. In the case of in vivo implantation, the term “biodegradation” often describes the material as slightly independent of the degradation activity, even though the fact those biodegradable products are necessary to be metabolized or eliminated from the body [50].
Owing to the minimal or lack of immune response and better overall interactions with a variety of cell types, polymers of natural origin were among the prime biodegradable scaffold materials to be attracted to clinical usage. Based on degradation behavior, biomaterials can be categorized into non-degradable and biodegradable. A non-degradable material does not decompose and the properties it reserves should be consistent with soft tissue [58]. The biodegradation rate solely depends on the polymer’s intrinsic properties such as hydrophobic/hydrophilic character, amorphous/crystalline quality, chemical structure, the association of hydrolytically unstable bonds, molecular weight, and glass transition temperature. Henceforth, a biomaterial with a wide range of hard and soft tissue applications can be tunable for weeks or months, or years of duration. In the case of an inflammatory response, the regulated macrophage is crucial; accordingly, degradation can occur besides the formation of new tissue. After which, the scaffold material is essential to break down on its own to restore it with new cell growth. While designing a bone tissue engineering scaffold, degradation mechanism and degradation rate are imperative to be investigated [50].
In polymers, the degradation mechanism is assisted via a non-biological route, i.e., erosion and hydrolysis, or a biological route, i.e., enzymatic action or involvement by microorganisms like bacteria, yeast, and fungi. Most natural polymers have undergone enzymatic degradation (Fig. 7). The protein-based polymers are acted upon enzymes like collagenases and metalloproteinases to break down their peptide bonds in vivo [58]. Polysaccharide-based biomaterials are degraded through amylases and lysosomes in the body. Conversely, major synthetic polymers of hydrolyzable linkages are broken down by hydrolytic processes such as urea, ester, and urethane linkages. In fact, polymers with a high number of hydrophilic groups simply undergo biodegradation. The whole biodegradation process can range from a few days to months to years based on the type of polymer. However, the cell biomass and other intermediate products can assume to be mineralized to CO2 over a long duration [59].
Schematic representation of biodegradation of polymers 58
In non-biological degradation, chemical splitting is highly accountable for deterioration, in addition to physical erosion. The amorphous blocks are liable to water molecular diffusion [60]. For instance, hydrolytic degradation begins initially in the amorphous region of the polymer leading to the splitting of the chain, followed by degradation occurring in crystalline regions. Considerably, the degree of hydrolysis is remarkably associated with relative hydrophilicity. Physical erosion alongside the hydrolysis reaction aids degradation. During physical erosion, the two processes such as bulk erosion and surface erosion head to the breakdown and resorption or dissolution of the scaffold material. However, the biodegradation should compromise the scaffold’s functional and mechanical potentials until the complete new tissue regeneration [60, 61].
Natural polymers in BTE
Natural polymers (NPs) have intrinsic biocompatible and biodegradable properties, thus readily suitable for BTE application. The NPs include chitosan (CS), collagen (Col), silk fibroin (SF), hyaluronic acid (Hyal), gelatin (Gel), etc., being widely used in BTE (Fig. 8). Polymers possess biocompatibility and are easy to engineer into desirable structures and sizes based on the requirement. The degradation characteristics and mechanical behaviors of the polymers can be managed and enable them to be tailormade, which is further targeted for a specific intention to subsequent in vivo implantation [62–64]. This section summarizes the amalgamation of nHAp with NPs like collagen, chitosan, gelatin, silk fibroin, hyaluronic acid, etc., and their efficiencies in in vitro and in vivo BTE circumstances.
HAp in combination with polymers of natural origin has excellent biocompatibility and superior osteogenesis but is associated with low osteoinductivity and mechanics, which could be dependent on the different types of bone defects. The BTE scaffolds should possess peculiar geometrical shapes and sizes resembling repaired sites. Besides their chemical composition, geometry, mechanical property, etc., adequate biological affinities encourage the migration/spreading of seeding cells to accelerate bone regeneration. Moreover, the location of bone defects necessitates the functionality or property of the scaffold. In the case of cortical bone, which requires tiny pores, the spongy bone demands the scaffold with a highly porous and resilient scaffold [12]. However, the scaffolds demand adequate mechanical strength and degradation behavior based on the need to replace with host natural tissue after a period of implantation. Murata et al. reported the refilling of HAp/collagen composite on an iliac crest defect assessment in 74 patients. Where bone defects are reduced in a time-dependent mode, cortical regeneration was noticed in 28.5% of the cases within 3 months, which was increased to 95.9% of the patients after 1 year. The cancellous bone repair was attained in 57.1% of the patients after 3 months which increased gradually to 95.9% after the year [65]. A study showed mineralized collagen fibrils and chitosan (CS/nHAC) composites with mesenchymal stem cells (MSCs) were implantation in cancellous bone defects in rabbit femurs. Inclusion of MSCs enhanced the formation of new bone at 12 weeks [66]. Chacon et al. investigated collagen/chitosan/HAp composite scaffolds for bone regeneration efficiency in healthy tibial and fragile bone (ovariectomy, i.e., gonadal hormone deficiency) rats. A thinner and incomplete defect closure was noted after 5 weeks. On the other hand, non-ovariectomized animals have a significant enhancement in new bone regeneration. New bone formation in the proximal tibial metaphysis of rats was noticed. The lacunae were filled with osteocytes which were organized in different directions. Moreover, the preservations of the medullary canal, hematopoietic tissue filling, and bone trabeculae were observed [67]. However, the differences in bone regeneration time and rate of osteogenesis were dependent on many factors such as the health condition of the patient, scaffold composition, and size and size of the defect. A few significant results of HAp-polymer composite scaffolds and their remarks are listed in Table 2.
Collagen-HAp nanocomposites
Collagen (Col) is the major constituent of bone that consists of a fibrous structure with a 50 to 500 nm in diameter range. The nano-sized architecture of Col assists the cellular adhesion, proliferation, and differentiation for the regeneration of bone tissue. Since the natural HAp nanocrystals are oriented to collagen fibrous molecules, [68, 69] the size of nHAp was found to be length around 50 nm, width around 25 nm, and thickness at 2–5 nm [68, 69]. Several investigations on Col-nHAp composites have been studied for BTE, where the majorly considered route is in situ precipitation [70]. Inclusion of collagen into porous sintered HAp scaffolds has shown enhanced mechanical strength while causing declined porosity [71]. The improvement in mechanical property ascribed that the formation of intermolecular H-bonds among HAp and Col, which eventually enhances the fracture toughness, therefore leads to improved resistance to failure [72]. The Col-nHAp scaffolds exhibit homogenous interconnected macro-porous structure with a compression strength up to 2.67 ± 0.37 MPa that was superior when compared to the control group (Relive® artificial bone) [73].
Varying ratios of Col-HAp scaffolds such as 70:30; 50:50; and 30:70 were fabricated by cryo-gelation method with the addition of 1-ethyl-3-(3-dimethyl aminopropyl) carbodiimide hydrochloride/N-hydroxysuccinimide used as cross-linkers. Col-nHAp scaffolds revealed better mechanical strength and enhanced cell proliferation when compared to pure Col sponges [75, 76]. Col-nHAp nanocomposites with layer-by-layer (multilayer) architecture were fabricated by Kim et al., which showed superior attachment, and differentiation of mesenchymal stem cells (MSCs) when seeded on scaffolds [77]. According to Yang et al. report, a biomimetic composite scaffold was prepared using Col, nHAp, and phosphatidylserine. The chemical composition of these scaffolds is analogous to that of natural bone [78]. J. Kozlowska et al. reported modified Col-nHAp composites fabricated by the freeze-drying method followed by dehydrothermal treatment [79]. The Col-nHAp showed a good response to the surrounding biological environment. Preliminary histological observation revealed minor local irritability, excellent biocompatibility, and vascularization on the 30th day post-implantation [79]. Dehydrothermally cross-linked Col-HAp composite for enhanced in vivo bone repair with a simplified preparative process without needed additional chemical reagents was reported by Zhang et al. [80] which demonstrated effectively induced osteoid tissue recovery in vivo. Yu et al. also prepared Col-HAp scaffolds by freeze-drying methods and investigated on rat calvarial model [74] and significant data is shown in Fig. 9. The Col-HAp composite scaffold with intrafibrillar mineralization (in cellular or lamellar microstructures) was achieved by biomimetic strategy. Iron and magnesium ions were incorporated in Col-HAp with lamellar scaffold architecture. Both in vitro and in vivo investigations confirmed the synergistic consequence of dual element incorporated lamellar scaffolds ion efficient bone regeneration.
(A) Fabrication of intrafibrillar mineralization of Fe/Mn embedded Col-HA composite scaffolds. (B) Pictorial representation of digital, photographic, and histological stained images of in vivo post-implantation [74]. Where A1-F1, A2-F2, and A3-F3 denote digital, X-ray, and histologic staining images respectively
Chitosan-nHAp nanocomposites
Chitosan (CS) is a versatile natural biopolymer that consists of glucosamine and N-acetyl glucosamine with β (1 → 4) glycosidic linkages [81]. The primary material chitin is a polysaccharide, which is rich in nitrogen. Chitin generally exists in hard exoskeletons of crustaceans and other invertebrates and it may be extracted from the cell walls of fungi and other marine sources [82, 83]. Chitin and its derivatives possess biodegradation, biocompatible, and intrinsic antibacterial properties that pave a crucial role in tissue engineering applications [84, 85]. CS acts as an important biopolymer in biomedical applications that include wound healing, antimicrobial, and tissue (hard and soft) regeneration. Moreover, in BTE, CS is exclusively applied to owe to its binding capacity with anionic molecules, pore-forming ability, antibacterial property, and biodegradability. Fabrication of CS into porous or hydrogel scaffolds facilitates improved inherent antibacterial properties when chelated with diverse metal ions [86, 87].
In situ prepared CS-nHAp composites exhibited a compression strength of 0.511 MPa, which was higher when compared to the CS scaffold. An elevated level of alkaline phosphatase (ALP) was noticed that was six times superior to pristine CS scaffolds [88, 89]. Freeze-drying method is one of the excellent routes to facilitate porous polymer structures through the nucleation of ice crystals, which emerged alongside the thermal gradient lines. However, the orientation of the pore can be restricted while freezing the molds by altering the geometry of the thermal gradients [88]. Silver (Ag) doped HAp and magnetite nanoparticles (NPs) were impregnated with CS providing excellent nanocomposite scaffolds with improved biocompatible, bioactive, and antibacterial qualities [90]. Improved integration and efficient bone tissue formation were achieved with CS-nHAp at varying bone defects in rat models, demonstrating their efficacy under in vivo conditions [91, 92]. The admirable benefits of CS-nHAp nanocomposite systems have been exploited as carriers to deliver numerous drugs, growth factors, and stem cells into targeted host tissue or cells [93, 94]. As coatings on substrates of titanium alloys, CS-HAp nanocomposites offered enhanced integration of implant materials to provide successful bone tissue formation in diabetic patients; however, the belated osseointegration may lead to numerous difficulties [95, 96].
Atak et al. reported amine group (NH2) modified CS-nHAp scaffolds for bone tissue engineering, revealing NH2-CS-nHAp scaffolds for better cellular attachment, survival, and differentiation of osteogenic process in hBM-MSCs when compared to pure CS and CS-nHAp [97]. Chatzipetros et al. investigated CS-nHAp scaffolds on rat calvarial critical-sized defect model (Fig. 10). This study suggests significant increase of the new bone tissue formation at the 4th week compared to the 2nd week implantation in euthanized rat models [98]. Jahan et al. developed guanosine 5′-diphosphate-crosslinked CS-nHAp scaffolds and investigated its osteogenic capability under in vitro and in vivo environments. The cells encapsulated composite scaffolds revealed a threefold increase in proliferation rate, double the rate of ALP levels, osterix expression, and further elevated calcium phosphate deposition in vitro, moreover the potential healing rate in tibial fractures at the 17th day in vivo post-implantation [99].
Right and left dorsal portions of parietal bones (A) two symmetrical bone defects in 5-mm diameter, (B) nHAp-CS composite implanted at right side defect, (C) allocation of rats shown in a timeline picture, (D) the nHAp-CS implanted at bone defects in rat models, and (E) final-stage digital analysis [98]
Alginate-nHAp nanocomposites
Alginate (Alg) is an important biopolymer, chiefly obtained from marine-sourced brown algae. The glucuronic acid and mannuronic acid copolymerized via α-1,4-glycosidic linkage to produce Alg biopolymer [100]. Hydrogels prepared from Alg tend to be moderately soluble in water when partially reacted with Ba2+ and Ca2+ divalent cations, which possess several biomedical applications, including drug delivery, BTE, and wound healing [101, 102]. Alg is a biodegradable, biocompatible material as represented by Becker et al., and also investigated their mechanical property [103, 104]. The correlation of biocompatibility with the purity of Alg was also noticed, whereas purified forms possess low adverse effects with surrounding tissues when compared to their poorly purified counterparts. The Alg purified at 40% exhibited compression strength around 22 kPa, although holding its elasticity, which was remarkably better than poorly purified Alg. Furthermore, the hydrogels with higher glucuronic acid substance provide better ductile properties and tensile strength as differing from the Alg with higher mannuronic acid concentration [104, 105]. Additionally, the enhanced mechanical strength of Alg can be attained by the reinforcement of ceramics such as nHAp. Upon introducing calcium (Ca) precursor ions for the synthesis of nHAp, Ca2+ can readily bind with carboxyl groups of sodium Alg (SA) via strong electrostatic interactions. Inclusion of phosphate (PO43−) precursors to the Ca-Alg complex leads to PO43− ions interacting with Ca2+ present in the Ca-Alg complex causing supersaturation and subsequent nucleation of nHAp occurs [106].
Nanocomposites containing carbonated nHAp with strontium and SA (SrCnHAp) spheres and without strontium (CnHAp) were used to perform in vitro and in vivo investigations. The cell viability of MC3T3-E1 osteoblasts on CnHAp and SrCnHAp composites explored its cytocompatibility under in vitro situations; however, the SrCnHAp composites revealed a higher rate of metabolic activity and cell membrane integrity when compared to CnHAp composite scaffolds [108]. Rabbit models were utilized for in vivo examinations, which endured sinus lift performance and demonstrated lesser amounts of SrCnHAp spheres in the 12th week. Thus, a prominent improvement of biocompatible, osteoconductive, and bioresorbable performances with the addition of strontium was noted when compared to CnHAp samples [108]. A study on Alg-Sr-nHAp microspheres laden with vancomycin was conducted to enhance the drug loading and sustained drug releasing efficiencies. By altering the pH (buffer solution), composite materials act as a promising vehicle for drug release [109]. The critical sized defects (i.e., even if the defect is small in size, but does not heal the bone itself by an animal) with the adequate mechanical strength of Alg-HAp scaffolds may fill the defect area in an animal model; however, its relevance to addressing the large defects should be scrutinized furthermore.
Regeneration of cartilage plays a crucial role in the success of osteochondral repair [110] because it offers a mechanical and biological transformation from unmineralized cartilage at the articulating surface to the underneath mineralized bone tissue. To address this, the Alg-HAp hydrogel scaffold was prepared using sodium citrate (SC) as a dispersing agent for HAp. The elevated levels of calcified cartilage markers such as ALP activity, Col X secretion, and mineral deposition were observed. The in vivo examination demonstrates that subcutaneous implantation of Alg-HAp scaffolds expressed predominant matrix mineralization, which has the potential for 3D bioprinting and osteochondral regeneration [111]. The biogenic scaffolds display enhanced biocompatibility and bioactive characteristics when compared to chemically derived scaffolds. Biogenic hydroxyapatite (bHAp) with porous features was prepared by the polymer infiltration way from the fishbone skeleton source and subsequently coated on Alg to fabricate Alg-bHAp composites. The better coating was achieved with 3% w/v Alg for about 10 min for porous bHAp scaffolds. Histological examination of 3Alg-nHAp (3% w/v Alg) scaffolds at the femur bone of rats signifies that the scaffolds assist both intramembranous and endochondral bone formation (Fig. 11) [107]. After 6 months, the femur defect was completely rejuvenated and filled with the mature lamellar bone with a Ca/P ratio that was analogous to the normal bone composition of the rat. R.C. Cuozzo et al. reported that a combination of zinc (Zn) with Alg-nHAp demonstrates a considerable quantity of bone formation notable in 6th month post-implanted rats when compared with the nHAp group [112].
Implantation of Alg-HAp scaffolds in the albino rat (male); surgical procedure (A and B), femur bone healing at 6 months of post-implantation (C) and SEM micrographs of bone defects grafted with Alg-nHAp composite scaffolds (D) [107]
Silk fibroin-nHAp nanocomposites
Silk fibroin (SF) has fascinated huge interest in tissue regeneration owing to its excellent biocompatible and minimal inflammatory reaction [113]. The SF-based biomaterials have been widely enhanced due to their ease of processing to make scaffolds with controlled parameters and their low degradation rate [114, 115]. Functional electrospun SF nano-fibrous scaffold functionalized with two-step HAp particle, by mussel adhesive encouraged polydopamine (PDA) chemistry [116], and a few significant results of this report are illustrated in Fig. 12. During electrospinning, the HAp particles were integrated into SF scaffolds, and immobilized onto HAp-impregnated electrospun SF nanofibrous scaffolds through PDA-assisted adhesion chemistry. Superior mechanical strength and microenvironment for physiological bone-specific were attained with double-stage functionalized SF nanofibrous scaffolds. To boost up the bone repair capability, hADMSCs were genetically tailored by transcriptional co-activator with PDZ binding motif (TAZ) through polymer nanoparticles-assisted gene delivery. The TAZ is a familiar transcriptional modulator, which triggers the osteogenic differentiation of MSCs [117, 118], and improved bone formation in a critical-sized calvarial defect model was obtained.
(A) Electrospun silk fibroin (SF) nanofibrous scaffolds engineered with two-stage hydroxyapatite (HAp) particle functionalization, (B) cross-view of the scaffolds, (C) Young’s modulus, (D) SEM micrographs and (E) immunofluorescence images and (F) quantification of osteopontin at 8 weeks of implantation in critical-sized calvarial bone defects in rat [116]
The consequence of SF and HAp fragmented coating on graft ligamentization and osseointegration of the artificial ligament; polyethylene terephthalate (PET) was explored by Cai et al. [119] The cell counting kit-8 (CCK-8) assessment demonstrates MC3T3-E1 osteoblasts and L929 fibroblasts with improved adhesion and proliferation rate on PET–HA and PET–SF fibers, respectively, compared to bare PET fibers. Furthermore, in vivo examination on a beagle anterior cruciate ligament (ACL) reconstruction model disclosed that the fragmented coating could efficiently persuade the osseointegration processes and graft ligamentization, which was perceived by excellent tissue infiltration in intra-articular part (IAP) and higher bone in-growth in intraosseous part (IOP) of the ligament [119]. Shang et al. developed a biomimetic bilayer membrane using SF-chondroitin sulfate-HAp that offered a promising approach for the defined repair of osteochondral tissue [120]. The biomimetic bilayer structure stimulated new cartilage formation and subchondral repair of the osteochondral defect model at the 12th week of implantation. In Behera et al. report, a comparative study of biochemical and biophysical characteristics was made on in situ reinforced SF-HAp composites and exterior deposition of HAp particles on a fibroin scaffold. In both cases (composite scaffolds), minimal immune responses were noticed in the co-culture model of osteoblast-macrophage [121].
Gelatin-nHAp nanocomposites
Gelatin (Gel) is a non-toxic natural biomacromolecule derived from collagen of numerous animal by-products, which is extensively utilized in food, cosmetic, and pharmaceutical industries [122, 123]. Gel has been utilized to enhance cell attachment; despite its biological properties, the mechanical strength and high degradation rates hinder its usage in hard tissue regeneration [124–126]. Hence, it has been amalgamated with HAp and other biomaterials to obtain the scaffolds with improved properties. Gel-nHAp-minocycline composite was developed and the composites were co-cultured with rat bone marrow stem cell proliferation [127]. Varying weight ratios of Gel-nHAp-TiO2 were developed using the phase separation method. The scaffolds with 77 to 82% of porosity were attained. Reinforcement of titania into nanocomposite scaffolds has shown 10.15 MPa compression strength compared to Gel-nHAp (94.87 MPa) scaffolds [128].
Nosrati et al. adopted a two-step strategy to develop Gel-HAp-3D graphene scaffolds, which includes hydrothermal autoclave by purging of hydrogen gas to prepare 3D graphene followed by employing hydrogel 3D printing technology [122, 129]. The interface analysis revealed that two phases (HAp-Graphene) are together held coherently and further improved mechanical properties, and higher accuracy of dimensionality was achieved (Fig. 13). A. A. Salifu et al. investigated human fetal osteoblasts (hFOBs) embedded scaffolds of 25 wt% HAp-Gel, and pristine Gel fibers (by electrospinning), which were heaped into 3-stack (3-S) and 4-stack (4-S) three-dimensional (by 3D printing technology) bone graft models under static cell culture conditions [130]. The interfaces of 3-S with regular cell seeding were merged with cross-interface migration of embedded cells; on the other hand, the middle interface layer of 4-S was retained separately because the cells were not seeded in the middle layers. Therefore, migration has not arrived at the center region of the 4-S layer. These findings agree with Papenburg et al., which revealed augmented cell adjoining layers and partial bonding existed in the 4-S model, with the interface between two-center layers with unseeded sides [131].
(A) Fabrication of Gel-HAp-rGO scaffolds: (a) hydrothermal (HT) processing conditions, (b) powders prepared by HT, (c) hydrogels, (d, e) setup of hydrogel 3D printing, and (f) 3D scaffolds. (B) SEM micrographs of Gel-HAp-rGO 3D scaffolds [129]
Hyaluronic acid-nHAp composites
Hyaluronic acid (HylA) have linear unbranched hydrophilic glycosaminoglycans, which are composed of repeated N-acetyl glucosamine and glucuronic acid: disaccharide parts [133]. HyAl has excellent bone regeneration properties owing to its biocompatible, elastic, antimicrobial, and osteoconductive features [134]. HyAl plays a crucial role in cell signaling pathways and assists essential function in cell proliferation and differentiation. The histological investigation was performed on rat models about 8 weeks of post-implantation that demonstrates the defects filled with calcium sulfate-nHAp-HyAl-collagenase nanocomposite scaffolds confirmed noteworthy and consistent regeneration of the alveolar bones, in which a greater number of osteocytes on the defective site was noticed [135].
Dennis et al. designed self-assembled and shear–responsive injectable colloidal gels for bone defect fillers [132]. The viscoelastic colloidal gel consists of microparticles of extracellular matrix (ECM), i.e., demineralized bone matrix (DBM), decellularized cartilage (DCC), and with HyAl and HAp nanoparticles as shown in Fig. 14. Rheological behavior of HyAl-ECM suspensions and HAp-HyAl-ECM gels ascribed identical or considerably higher storage moduli; G′ ≈ 100–10,000 Pa, viscoelastic recoveries; G′recovery ≥ 87%, and yield stresses; Ʈy ≈ 100–10,000 Pa, when compared with controls (without ECM).
Live/dead assay of hUCMSCs (human umbilical cord mesenchymal stromal cells) cultured on HyAl-HAp-ECM colloidal gels. Where green and red fluorescence denotes the viable and non-viable cells respectively. Where Ф refers to the volume fraction of ECM in each formulation. All scale bars are 100 μm [132]
Conclusion and future perspectives
Though several researchers have been focused on the development of scaffolds based on several polymer-HAp composite scaffolds, each composite is associated with certain kinds of pros and cons in terms of its mechanical stability, control over porosity, and interaction with the biological environment in vitro and in vivo. This is mainly because polymers are extremely sensitive to many factors like pH, temperature, solvents, etc., based on chemical composition, especially with the processing of natural polymers. In BTE, the production of composite scaffolds of polymers-nHAp is still required to be considered to determine the equilibrium between mechanical strength and biological performance, which may vary and is solely dependent on the choice of polymer selection. The development of patient-specific scaffold materials is an immense challenge for scientists and researchers. Fabrication of critical biological shapes, degree porosity, and mechanical stability is very difficult.
However, each fabrication technique has its advantage and disadvantages; hence, there are still various disputes that must be explored further in detail on BTE shortly to attain suitable nHAp-based composite scaffolds with tunable properties. Many reports on composite scaffolds have been deprived of insights from fabrication strategies to in vitro and in vivo aspects. More to the point, most of the studies have been mainly concentrated on fabrication and physicochemical characterization but not in vivo investigation. When bridging the gap between fabrications to in vivo studies with its clear intermediate mechanical stability and porosity alterations, this may sound like the future research avenue in clinical trials in the field of bone tissue engineering.
Data availability
Data will be made available on reasonable request.
References
Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468(11):3070–6. https://doi.org/10.1007/s11999-010-1399-0.
Hartman CW, Garvin KL. Femoral fixation in revision total hip arthroplasty. Instr Course Lect. 2012;61:313–25.
Nandi SK, Roy S, Mukherjee P, Kundu B, De DK, Basu D. Orthopaedic applications of bone graft & graft substitutes: a review. Indian J Med Res. 2010;132:15–30.
Greenwald AS, Boden SD, Goldberg VM, Khan Y, Laurencin CT, Rosier RN. American Academy of Orthopaedic Surgeons. The Committee on Biological Implants. Bone-graft substitutes: facts, fictions, and applications. J Bone Joint Surg Am. 2001;83-A(2):98–103. https://doi.org/10.2106/00004623-200100022-00007.
Burg KJ, Porter S, Kellam JF. Biomaterial developments for bone tissue engineering. Biomaterials. 2000;21(23):2347–59. https://doi.org/10.1016/s0142-9612(00)00102-2.
Zhou H, Lee J. Nanoscale hydroxyapatite particles for bone tissue engineering. Acta Biomater. 2011;7(7):2769–81. https://doi.org/10.1016/j.actbio.2011.03.019.
Kantharia N, Naik S, Apte S, Kheur M, Kheur S, Kale B. Nano-hydroxyapatite and its contemporary applications. J Dent Res Sci Develop. 2014;1:15.
Palazzo B, Iafisco M, Laforgia M, Margiotta N, Natile G, Bianchi CL, Walsh D, Mann S, Roveri N. Biomimetic hydroxyapatite–drug nanocrystals as potential bone substitutes with antitumor drug delivery properties. Adv Func Mater. 2007;17(13):2180–8. https://doi.org/10.1002/adfm.200600361.
Deshmukh K, Shaik MM, Ramanan SR, Kowshik M. Self-activated fluorescent hydroxyapatite nanoparticles: a promising agent for bioimaging and biolabeling. ACS Biomater Sci Eng. 2016;2(8):1257–64. https://doi.org/10.1021/acsbiomaterials.6b00169.
Verwilghen C, Rio S, Nzihou A, Gauthier D, Flamant G, Sharrock PJ. Preparation of high specific surface area hydroxyapatite for environmental applications. J Mater Sci. 2007;42(15):6062–6. https://doi.org/10.1007/s10853-006-1160-y.
Elsayed MT, Hassan AA, Abdelaal SA, Taher MM, Ahmed M, Khalaf M, Shoueir KR. Morphological, antibacterial, and cell attachment of cellulose acetate nanofibers containing modified hydroxyapatite for wound healing utilizations. J Mater Res Technol. 2020;9(6):13927–36. https://doi.org/10.1016/j.jmrt.2020.09.094.
Mondal S, Pal U. 3D hydroxyapatite scaffold for bone regeneration and local drug delivery applications. J Drug Deliv Sci Technol. 2019;53:101131. https://doi.org/10.1016/j.jddst.2019.101131.
Amini AR, Laurencin CT, Nukavarapu SP. Bone tissue engineering: recent advances and challenges. Crit Rev Biomed Eng. 2012;40(5):363–408.
He W, Wu Z, Wu Y, Zhong Z, Hong Y. Construction of the gypsum-coated scaffolds for in situ bone regeneration. ACS Appl Mater Interfaces. 2021;13(27):31527–41. https://doi.org/10.1021/acsami.1c08372.
Denry I, Kuhn LT. Design and characterization of calcium phosphate ceramic scaffolds for bone tissue engineering. Dent Mater. 2016;32(1):43–53. https://doi.org/10.1016/j.dental.2015.09.008.
Bose S, Tarafder S. Calcium phosphate ceramic systems in growth factor and drug delivery for bone tissue engineering: a review. Acta Biomater. 2012;8(4):1401–21. https://doi.org/10.1016/j.actbio.2011.11.017.
Liu X, Ma PX. Polymeric scaffolds for bone tissue engineering. Ann Biomed Eng. 2004;32(3):477–86. https://doi.org/10.1023/b:abme.0000017544.36001.8e.
Gerhardt L-C, Boccaccini AR. Bioactive glass and glass-ceramic scaffolds for bone tissue engineering. Materials (Basel). 2010;3(7):3867–910. https://doi.org/10.3390/ma3073867.
Baino F, Verné E, Vitale-Brovarone C. Feasibility, tailoring and properties of polyurethane/bioactive glass composite scaffolds for tissue engineering. J Mater Sci Mater Med. 2009;20(11):2189–95. https://doi.org/10.1007/s10856-009-3787-0.
Mondal S, Dorozhkin SV, Pal U. Recent progress on fabrication and drug delivery applications of nanostructured hydroxyapatite. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2018;10(4):e1504. https://doi.org/10.1002/wnan.1504.
Dorozhkin SV. Multiphasic calcium orthophosphate (CaPO4) bioceramics and their biomedical applications. Ceram Int. 2016;42(6):6529–54. https://doi.org/10.1016/j.ceramint.2016.01.062.
Ohura K, Bohner M, Hardouin P, Lemaître J, Pasquier G, Flautre B. Resorption of, and bone formation from, new beta-tricalcium phosphate-monocalcium phosphate cements: an in vivo study. J Biomed Mater Res. 1996;30(2):193–200. https://doi.org/10.1002/(SICI)1097-4636(199602)30:2%3c193::AID-JBM9%3e3.0.CO;2-M.
Suzuki O, Kamakura S, Katagiri T. Surface chemistry and biological responses to synthetic octacalcium phosphate. J Biomed Mater Res B Appl Biomater. 2006;77(1):201–12. https://doi.org/10.1002/jbm.b.30407.
Meyer JL, Fowler BO. Lattice defects in nonstoichiometric calcium hydroxylapatites. Chem Approach Inorg Chem. 1982;21(8):3029–35. https://doi.org/10.1021/ic00138a021.
Radha G, Balakumar S, Venkatesan B, Vellaichamy E. Evaluation of hemocompatibility and in vitro immersion on microwave-assisted hydroxyapatite–alumina nanocomposites. Mater Sci Eng, C. 2015;50:143–50. https://doi.org/10.1016/j.msec.2015.01.054.
Lowe B, Hardy JG, Walsh LJ. Optimizing nanohydroxyapatite nanocomposites for bone tissue engineering. ACS Omega. 2020;5(1):1–9. https://doi.org/10.1021/acsomega.9b02917.
LeGeros RZ. Biodegradation and bioresorption of calcium phosphate ceramics. Clin Mater. 1993;14(1):65–88. https://doi.org/10.1016/0267-6605(93)90049-d.
Stupp SI, Ciegler GW. Organoapatites: materials for artificial bone. I. Synthesis and Microstructure. J Biomed Mater Res. 1992;26(2):169–83. https://doi.org/10.1002/jbm.820260204.
Webster TJ, Ergun C, Doremus RH, Siegel RW, Bizios R. Enhanced functions of osteoblasts on nanophase ceramics. Biomaterials. 2000;21(17):1803–10. https://doi.org/10.1016/s0142-9612(00)00075-2.
Kim H-M, Himeno T, Kawashita M, Kokubo T, Nakamura T. The mechanism of biomineralization of bone-like apatite on synthetic hydroxyapatite: an in vitro assessment. J R Soc Interface. 2004;1(1):17–22. https://doi.org/10.1098/rsif.2004.0003.
Chavan PN, Bahir MM, Mene RU, Mahabole MP, Khairnar RS. Study of nanobiomaterial hydroxyapatite in simulated body fluid: formation and growth of apatite. Mater Sci Eng, B. 2010;168(1):224–30. https://doi.org/10.1016/j.mseb.2009.11.012.
Srivatsan TS. Biomaterials: a nano approach, by Sreeram Ramakrishna, Murugan Ramalingam, T S Sampath Kumar, and Winston O Soboyejo. Mater Manuf Process. 2014;29(11–12):1510–1. https://doi.org/10.1080/10426914.2014.950068.
Sadat-Shojai M, Khorasani M-T, Dinpanah-Khoshdargi E, Jamshidi A. Synthesis methods for nanosized hydroxyapatite with diverse structures. Acta Biomater. 2013;9(8):7591–621. https://doi.org/10.1016/j.actbio.2013.04.012.
AlHammad MS. Nanostructure hydroxyapatite based ceramics by sol gel method. J Alloy Compd. 2016;661:251–6. https://doi.org/10.1016/j.jallcom.2015.11.045.
Koirala MB, Nguyen TDT, Pitchaimani A, Choi S-O, Aryal S. Synthesis and characterization of biomimetic hydroxyapatite nanoconstruct using chemical gradient across lipid bilayer. ACS Appl Mater Interfaces. 2015;7(49):27382–90. https://doi.org/10.1021/acsami.5b09042.
Amin S, Siddique T, Mujahid M, Shah SS. Synthesis and characterization of nano hydroxyapatite using reverse micro emulsions as nano reactors. J Chem Soc Pak. 2015;37(1):79–85.
Henkel J, Woodruff MA, Epari DR, Steck R, Glatt V, Dickinson IC, Choong PFM, Schuetz MA, Hutmacher DW. Bone regeneration based on tissue engineering conceptions — a 21st century perspective. Bone Res. 2013;1(1):216–48. https://doi.org/10.4248/BR201303002.
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA. IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277–88. https://doi.org/10.1007/s00198-011-1601-6.
Cheung C-L, Ang SB, Chadha M, Chow ES-L, Chung Y-S, Hew FL, Jaisamrarn U, Ng H, Takeuchi Y, Wu C-H, Xia W, Yu J, Fujiwara S. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies Study. Osteoporos Sarcopenia. 2018;4(1):16–21. https://doi.org/10.1016/j.afos.2018.03.003.
Hellmich C, Ulm F-J. Micromechanical model for ultrastructural stiffness of mineralized tissues. J Eng Mech. 2002;128(8):898–908. https://doi.org/10.1061/(ASCE)0733-9399(2002)128:8(898).
Weiner S, Traub W. Organization of hydroxyapatite crystals within collagen fibrils. FEBS Lett. 1986;206(2):262–6. https://doi.org/10.1016/0014-5793(86)80993-0.
Munir MU, Salman S, Ihsan A, Elsaman T. Synthesis, characterization, functionalization and bio-applications of hydroxyapatite nanomaterials: an overview. Int J Nanomed. 2022;17:1903–25. https://doi.org/10.2147/IJN.S360670.
Thomas V, Dean DR, Jose MV, Mathew B, Chowdhury S, Vohra YK. Nanostructured biocomposite scaffolds based on collagen coelectrospun with nanohydroxyapatite. Biomacromol. 2007;8(2):631–7. https://doi.org/10.1021/bm060879w.
Murphy CM, O’Brien FJ. Understanding the effect of mean pore size on cell activity in collagen-glycosaminoglycan scaffolds. Cell Adh Migr. 2010;4(3):377–81. https://doi.org/10.4161/cam.4.3.11747.
Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials. 2005;26(27):5474–91. https://doi.org/10.1016/j.biomaterials.2005.02.002.
Kong L, Gao Y, Cao W, Gong Y, Zhao N, Zhang X. Preparation and characterization of nano-hydroxyapatite/chitosan composite scaffolds. J Biomed Mater Res A. 2005;75(2):275–82. https://doi.org/10.1002/jbm.a.30414.
Kim H-W, Song J-H, Kim H-E. Nanofiber generation of gelatin–hydroxyapatite biomimetics for guided tissue regeneration. Adv Func Mater. 2005;15(12):1988–94. https://doi.org/10.1002/adfm.200500116.
Sous M, Bareille R, Rouais F, Clément D, Amédée J, Dupuy B, Baquey C. Cellular biocompatibility and resistance to compression of macroporous beta-tricalcium phosphate ceramics. Biomaterials. 1998;19(23):2147–53. https://doi.org/10.1016/s0142-9612(98)00118-5.
Reddy MS, Ponnamma D, Choudhary R, Sadasivuni KK. A comparative review of natural and synthetic biopolymer composite scaffolds. Polymers. 2021;13(7):1105. https://doi.org/10.3390/polym13071105.
Song R, Murphy M, Li C, Ting K, Soo C, Zheng Z. Current development of biodegradable polymeric materials for biomedical applications. Drug Des Dev Ther. 2018;12:3117. https://doi.org/10.2147/DDDT.S165440.
Avanzi IR, Parisi JR, Souza A, Cruz MA, Martignago CC, Ribeiro DA, Braga AR, Renno AC. 3D‐printed hydroxyapatite scaffolds for bone tissue engineering: A systematic review in experimental animal studies. J Biomed Mater Res B Appl Biomater. 2023;111(1):203–19. https://doi.org/10.1002/jbm.b.35134.
Milazzo M, Contessi Negrini N, Scialla S, Marelli B, Farè S, Danti S, Buehler MJ. Additive manufacturing approaches for hydroxyapatite-reinforced composites. Adv Func Mater. 2019;29(35):1903055. https://doi.org/10.1002/adfm.201903055.
Hu Q, Li B, Wang M, Shen J. Preparation and characterization of biodegradable chitosan/hydroxyapatite nanocomposite rods via in situ hybridization: a potential material as internal fixation of bone fracture. Biomaterials. 2004;25(5):779–85. https://doi.org/10.1016/S0142-9612(03)00582-9.
Li X, Chang J. Preparation and characterization of bioactive collagen/wollastonite composite scaffolds. J Mater Sci Mater Med. 2005;16(4):361. https://doi.org/10.1002/jbm.a.30414.
Zhang Y, Zhang M. Synthesis and characterization of macroporous chitosan/calcium phosphate composite scaffolds for tissue engineering. J Biomed Mater Res. 2001;55(3):304–12. https://doi.org/10.1002/1097-4636(20010605)55:3%3c304::AID-JBM1018%3e3.0.CO;2-J.
Li X, Nan K, Shi S, Chen H. Preparation and characterization of nano-hydroxyapatite/chitosan cross-linking composite membrane intended for tissue engineering. Int J Biol Macromol. 2012;50(1):43–9. https://doi.org/10.1016/j.ijbiomac.2011.09.021.
Lei X, Gao J, Xing F, Zhang Y, Ma Y, Zhang G. Comparative evaluation of the physicochemical properties of nano-hydroxyapatite/collagen and natural bone ceramic/collagen scaffolds and their osteogenesis-promoting effect on MC3T3-E1 cells. Regen Biomaterials. 2019;6(6):361–71. https://doi.org/10.1093/rb/rbz026.
Reddy MSB, Ponnamma D, Choudhary R, Sadasivuni KK. A comparative review of natural and synthetic biopolymer composite scaffolds. Polymers. 2021;13(7):1105. https://doi.org/10.3390/polym13071105.
Puls J, Wilson SA, Hölter D. Degradation of cellulose acetate-based materials: a review. J Polym Environ. 2011;19(1):152–65. https://doi.org/10.1007/s10924-010-0258-0.
Samantaray PK, Little A, Haddleton DM, McNally T, Tan B, Sun Z, Huang W, Ji Y, Wan C. Poly(glycolic acid) (PGA): a versatile building block expanding high performance and sustainable bioplastic applications. Green Chem. 2020;22(13):4055–81. https://doi.org/10.1039/D0GC01394C.
Hsu S, Hung K-C, Chen C-W. Biodegradable polymer scaffolds. J Mater Chem B. 2016;4(47):7493–505. https://doi.org/10.1039/C6TB02176J.
Mo X, Zhang D, Liu K, Zhao X, Li X, Wang W. Nano-hydroxyapatite composite scaffolds loaded with bioactive factors and drugs for bone tissue engineering. Int J Mol Sci. 2023;24(2):1291. https://doi.org/10.3390/ijms24021291.
Venkatesan J, Kim S-K. Nano-hydroxyapatite composite biomaterials for bone tissue engineering—a review. J Biomed Nanotechnol. 2014;10(10):3124–40. https://doi.org/10.1166/jbn.2014.1893.
Ramesh N, Moratti SC, Dias GJ. Hydroxyapatite–polymer biocomposites for bone regeneration: a review of current trends. J Biomed Mater Res B Appl Biomater. 2018;106(5):2046–57. https://doi.org/10.1002/jbm.b.33950.
Murata K, Fujibayashi S, Otsuki B, Shimizu T, Matsuda S. Repair of iliac crest defects with a hydroxyapatite/collagen composite. Asian Spine J. 2020;14(6):808–13. https://doi.org/10.31616/asj.2019.0310.
Huang Z, Chen Y, Feng Q-L, Zhao W, Yu B, Tian J, Li S-J, Lin B-M. In vivo bone regeneration with injectable chitosan/hydroxyapatite/collagen composites and mesenchymal stem cells. Front Mater Sci. 2011;5(3):301–10. https://doi.org/10.1007/s11706-011-0142-4.
Chacon EL, Bertolo MR, de Guzzi Plepis AM, da Conceição Amaro Martins V, Dos Santos GR, Pinto CA, Pelegrine AA, et al. Collagen-chitosan-hydroxyapatite composite scaffolds for bone repair in ovariectomized rats. Sci Rep. 2023;13(1):28. https://doi.org/10.1038/s41598-022-24424-x.
Venugopal J, Prabhakaran MP, Zhang Y, Low S, Choon AT, Ramakrishna S. Biomimetic hydroxyapatite-containing composite nanofibrous substrates for bone tissue engineering. Philos Trans A Math Phys Eng Sci. 1917;2010(368):2065–81. https://doi.org/10.1098/rsta.2010.0012.
Boland ED, Matthews JA, Pawlowski KJ, Simpson DG, Wnek GE, Bowlin GL. Electrospinning collagen and elastin: preliminary vascular tissue engineering. Front Biosci. 2004;9:1422–32. https://doi.org/10.2741/1313.
Peng C, Zhu ZA, Li GL, Sun DC, Li JG, Qiu ZY, Hu CL, Liu ZH, Sheng HB, Cui FZ. Enhancement of bone healing in rabbit ulnar critical bone defect by injectable nano-hydroxyapatite/collagen/(calcium sulfate hemihydrate) mixed with autogenous bone marrow. Journal of Biomaterials and Tissue Engineering 2013;3(5):534–41. https://doi.org/10.1166/jbt.2013.1117.
Islam MdS, Todo M. Effects of sintering temperature on the compressive mechanical properties of collagen/hydroxyapatite composite scaffolds for bone tissue engineering. Mater Lett. 2016;173:231–4. https://doi.org/10.1016/j.matlet.2016.03.028.
Libonati F, Nair AK, Vergani L, Buehler MJ. Mechanics of collagen–hydroxyapatite model nanocomposites. Mech Res Commun. 2014;58:17–23. https://doi.org/10.1016/j.mechrescom.2013.08.008.
Jia L, Duan Z, Fan D, Mi Y, Hui J, Chang L. Human-like collagen/nano-hydroxyapatite scaffolds for the culture of chondrocytes. Mater Sci Eng, C. 2013;33(2):727–34. https://doi.org/10.1016/j.msec.2012.10.025.
Yu L, Rowe DW, Perera IP, Zhang J, Suib SL, Xin X, Wei M. Intrafibrillar mineralized collagen-hydroxyapatite-based scaffolds for bone regeneration. ACS Appl Mater Interfaces. 2020;12(16):18235–49. https://doi.org/10.1021/acsami.0c00275.
Rodrigues SC, Salgado CL, Sahu A, Garcia MP, Fernandes MH, Monteiro FJ. Preparation and characterization of collagen-nanohydroxyapatite biocomposite scaffolds by cryogelation method for bone tissue engineering applications. J Biomed Mater Res A. 2013;101(4):1080–94. https://doi.org/10.1002/jbm.a.34394.
Cunniffe GM, Dickson GR, Partap S, Stanton KT, O’Brien FJ. Development and characterisation of a collagen nano-hydroxyapatite composite scaffold for bone tissue engineering. J Mater Sci: Mater Med. 2010;21(8):2293–8. https://doi.org/10.1007/s10856-009-3964-1.
Kim TG, Park S-H, Chung HJ, Yang D-Y, Park TG. Microstructured scaffold coated with hydroxyapatite/collagen nanocomposite multilayer for enhanced osteogenic induction of human mesenchymal stem cells. J Mater Chem. 2010;20(40):8927–33. https://doi.org/10.1039/C0JM01062F.
Yang C, Wang Y, Chen X. Preparation and evaluation of biomimetric nano-hydroxyapatite-based composite scaffolds for bone-tissue engineering. Chin Sci Bull. 2012;57(21):2787–92. https://doi.org/10.1007/s11434-012-5201-4.
Kozlowska J, Jundzill A, Bajek A, Bodnar M, Marszalek A, Witmanowski H, Sionkowska A. Preliminary in vitro and in vivo assessment of modified collagen/hydroxyapatite composite. Mater Lett. 2018;221:74–6. https://doi.org/10.1016/j.matlet.2018.03.122.
Zhang Z, Ma Z, Zhang Y, Chen F, Zhou Y, An Q. Dehydrothermally crosslinked collagen/hydroxyapatite composite for enhanced in vivo bone repair. Colloids Surf B Biointerfaces. 2018;163:394–401. https://doi.org/10.1016/j.colsurfb.2018.01.011.
Khor E. Chitin: fulfilling a biomaterials promise. Elsevier; 2014.
Abdou ES, Nagy KSA, Elsabee MZ. Extraction and characterization of chitin and chitosan from local sources. Biores Technol. 2008;99(5):1359–67. https://doi.org/10.1016/j.biortech.2007.01.051.
Teli MD, Sheikh J. Extraction of chitosan from shrimp shells waste and application in antibacterial finishing of bamboo rayon. Int J Biol Macromol. 2012;50(5):1195–200. https://doi.org/10.1016/j.ijbiomac.2012.04.003.
Freier T, Koh HS, Kazazian K, Shoichet MS. Controlling cell adhesion and degradation of chitosan films by N-acetylation. Biomaterials. 2005;26(29):5872–8. https://doi.org/10.1016/j.biomaterials.2005.02.033.
Sarasam AR, Brown P, Khajotia SS, Dmytryk JJ, Madihally SV. Antibacterial activity of chitosan-based matrices on oral pathogens. J Mater Sci: Mater Med. 2008;19(3):1083–90. https://doi.org/10.1007/s10856-007-3072-z.
Wang X, Du Y, Fan L, Liu H, Hu Y. Chitosan- metal complexes as antimicrobial agent: synthesis, characterization and structure-activity study. Polym Bull. 2005;55(1):105–13. https://doi.org/10.1007/s00289-005-0414-1.
Madihally SV, Matthew HWT. Porous chitosan scaffolds for tissue engineering. Biomaterials. 1999;20(12):1133–42. https://doi.org/10.1016/S0142-9612(99)00011-3.
Zhang J, Nie J, Zhang Q, Li Y, Wang Z, Hu Q. Preparation and characterization of bionic bone structure chitosan/hydroxyapatite scaffold for bone tissue engineering. J Biomater Sci Polym Ed. 2014;25(1):61–74. https://doi.org/10.1080/09205063.2013.836950.
Nikpour MR, Rabiee SM, Jahanshahi M. Synthesis and characterization of hydroxyapatite/chitosan nanocomposite materials for medical engineering applications. Compos B Eng. 2012;43(4):1881–6. https://doi.org/10.1016/j.compositesb.2012.01.056.
Anjaneyulu U, Swaroop VK, Vijayalakshmi U. Preparation and characterization of novel Ag doped hydroxyapatite–Fe3O4–chitosan hybrid composites and in vitro biological evaluations for orthopaedic applications. RSC Adv. 2016;6(13):10997–1007. https://doi.org/10.1039/C5RA21479C.
Danilchenko SN, Kalinkevich OV, Pogorelov MV, Kalinkevich AN, Sklyar AM, Kalinichenko TG, Ilyashenko VY, Starikov VV, Bumeyster VI, Sikora VZ, Sukhodub LF. Characterization and in vivo evaluation of chitosan-hydroxyapatite bone scaffolds made by one step coprecipitation method. J Biomed Mater Res, Part A. 2011;96A(4):639–47. https://doi.org/10.1002/jbm.a.33017.
Dhivya S, Saravanan S, Sastry TP, Selvamurugan N. Nanohydroxyapatite-reinforced chitosan composite hydrogel for bone tissue repair in vitro and in vivo. J Nanobiotechnol. 2015;13(1):40. https://doi.org/10.1186/s12951-015-0099-z.
Yang J, Liu A, Han Y, Li Q, Tian J, Zhou C. Osteodifferentiation of mesenchymal stem cells on chitosan/hydroxyapatite composite films. J Biomed Mater Res, Part A. 2014;102(4):1202–9. https://doi.org/10.1002/jbm.a.34756.
Della Porta G, Campardelli R, Cricchio V, Oliva F, Maffulli N, Reverchon E. Injectable PLGA/hydroxyapatite/chitosan microcapsules produced by supercritical emulsion extraction technology: an in vitro study on teriparatide/gentamicin controlled release. J Pharm Sci. 2016;105(7):2164–72. https://doi.org/10.1016/j.xphs.2016.05.002.
Shi YY, Li M, Liu Q, Jia ZJ, Xu XC, Cheng Y, Zheng YF. Electrophoretic deposition of graphene oxide reinforced chitosan–hydroxyapatite nanocomposite coatings on Ti substrate. J Mater Sci: Mater Med. 2016;27(3):48. https://doi.org/10.1007/s10856-015-5634-9.
Ma X-Y, Feng Y-F, Ma Z-S, Li X, Wang J, Wang L, Lei W. The promotion of osteointegration under diabetic conditions using chitosan/hydroxyapatite composite coating on porous titanium surfaces. Biomaterials. 2014;35(26):7259–70. https://doi.org/10.1016/j.biomaterials.2014.05.028.
Atak BH, Buyuk B, Huysal M, Isik S, Senel M, Metzger W, Cetin G. Preparation and characterization of amine functional nano-hydroxyapatite/chitosan bionanocomposite for bone tissue engineering applications. Carbohyd Polym. 2017;164:200–13. https://doi.org/10.1016/j.carbpol.2017.01.100.
Chatzipetros E, Christopoulos P, Donta C, Tosios KI, Tsiambas E, Tsiourvas D, Kalogirou E-M, Tsiklakis K. Application of nano-hydroxyapatite/chitosan scaffolds on rat calvarial critical-sized defects: a pilot study. Med Oral Patol Oral Cir Bucal. 2018;23(5):e625–32. https://doi.org/10.4317/medoral.22455.
Jahan K, Manickam G, Tabrizian M, Murshed M. In vitro and in vivo investigation of osteogenic properties of self-contained phosphate-releasing injectable purine-crosslinked chitosan-hydroxyapatite constructs. Sci Rep. 2020;10(1):11603. https://doi.org/10.1038/s41598-020-67886-7.
Gombotz WR, Wee S. Protein release from alginate matrices. Adv Drug Deliv Rev. 1998;31(3):267–85. https://doi.org/10.1016/S0169-409X(97)00124-5.
Kuo CK, Ma PX. Ionically crosslinked alginate hydrogels as scaffolds for tissue engineering: part 1 Structure, gelation rate and mechanical properties. Biomaterials. 2001;22(6):511–21. https://doi.org/10.1016/S0142-9612(00)00201-5.
Tampieri A, Sandri M, Landi E, Celotti G, Roveri N, Mattioli-Belmonte M, Virgili L, Gabbanelli F, Biagini G. HA/alginate hybrid composites prepared through bio-inspired nucleation. Acta Biomater. 2005;1(3):343–51. https://doi.org/10.1016/j.actbio.2005.01.001.
Gutowska A, Jeong B, Jasionowski M. Injectable gels for tissue engineering. Anat Rec. 2001;263(4):342–9. https://doi.org/10.1002/ar.1115.
Becker TA, Kipke DR, Brandon T. Calcium alginate gel: a biocompatible and mechanically stable polymer for endovascular embolization. J Biomed Mater Res. 2001;54(1):76–86. https://doi.org/10.1002/1097-4636(200101)54:1%3c76::AID-JBM9%3e3.0.CO;2-V.
Drury JL, Dennis RG, Mooney DJ. The tensile properties of alginate hydrogels. Biomaterials. 2004;25(16):3187–99. https://doi.org/10.1016/j.biomaterials.2003.10.002.
Rajkumar M, Meenakshisundaram N, Rajendran V. Development of nanocomposites based on hydroxyapatite/sodium alginate: synthesis and characterisation. Mater Charact. 2011;62(5):469–79. https://doi.org/10.1016/j.matchar.2011.02.008.
Mahmoud EM, Sayed M, El-Kady AM, Elsayed H, Naga SM. In vitro and in vivo study of naturally derived alginate/hydroxyapatite bio composite scaffolds. Int J Biol Macromol. 2020;165:1346–60. https://doi.org/10.1016/j.ijbiomac.2020.10.014.
Valiense H, Barreto M, Resende RF, Alves AT, Rossi AM, Mavropoulos E, Granjeiro JM, Calasans-Maia MD. In vitro and in vivo evaluation of strontium-containing nanostructured carbonated hydroxyapatite/sodium alginate for sinus lift in rabbits. J Biomed Mater Res B Appl Biomater. 2016;104(2):274–82. https://doi.org/10.1002/jbm.b.33392.
Li H, Jiang F, Ye S, Wu Y, Zhu K, Wang D. Bioactive apatite incorporated alginate microspheres with sustained drug-delivery for bone regeneration application. Mater Sci Eng, C. 2016;62:779–86. https://doi.org/10.1016/j.msec.2016.02.012.
Hunziker EB. Articular cartilage repair: basic science and clinical progress. a review of the current status and prospects. Osteoarthr Cartil. 2002;10(6):432–63.
You F, Chen X, Cooper DML, Chang T, Eames BF. Homogeneous hydroxyapatite/alginate composite hydrogel promotes calcified cartilage matrix deposition with potential for three-dimensional bioprinting. Biofabrication. 2018;11(1):015015. https://doi.org/10.1088/1758-5090/aaf44a.
Cuozzo RC, Sartoretto SC, Resende RFB, Alves ATNN, Mavropoulos E, Prado da Silva MH, Calasans-Maia MD. Biological evaluation of zinc-containing calcium alginate-hydroxyapatite composite microspheres for bone regeneration. J Biomed Mater Res Part B: Appl Biomater. 2020;108(6):2610–20.
Vepari C, Kaplan DL. Silk as a biomaterial. Prog Polym Sci. 2007;32(8):991–1007. https://doi.org/10.1016/j.progpolymsci.2007.05.013.
Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J, Lu H, Richmond J, Kaplan DL. Silk-based biomaterials. Biomaterials. 2003;24(3):401–16. https://doi.org/10.1016/S0142-9612(02)00353-8.
Yoshimoto H, Shin YM, Terai H, Vacanti JP. A biodegradable nanofiber scaffold by electrospinning and its potential for bone tissue engineering. Biomaterials. 2003;24(12):2077–82. https://doi.org/10.1016/S0142-9612(02)00635-X.
Ko E, Lee JS, Kim H, Yang SY, Yang D, Yang K, Lee J, Shin J, Yang HS, Ryu W, Cho S-W. Electrospun silk fibroin nanofibrous scaffolds with two-stage hydroxyapatite functionalization for enhancing the osteogenic differentiation of human adipose-derived mesenchymal stem cells. ACS Appl Mater Interfaces. 2018;10(9):7614–25. https://doi.org/10.1021/acsami.7b03328.
Hong J-H, Yaffe MB. TAZ: A β-catenin-like molecule that regulates mesenchymal stem cell differentiation. Cell Cycle. 2006;5(2):176–9. https://doi.org/10.4161/cc.5.2.2362.
Kim KM, Choi YJ, Hwang J-H, Kim AR, Cho HJ, Hwang ES, Park JY, Lee S-H, Hong J-H. Shear stress induced by an interstitial level of slow flow increases the osteogenic differentiation of mesenchymal stem cells through TAZ activation. Plos One. 2014;9(3):e92427. https://doi.org/10.1371/journal.pone.0092427.
Cai J, Wan F, Dong Q, Jiang J, Ai C, Sheng D, Jin W, Liu X, Zhi Y, Wang S, Sun Y, Chen J, Shao Z, Chen S. Silk fibroin and hydroxyapatite segmented coating enhances graft ligamentization and osseointegration processes of the polyethylene terephthalate artificial ligament in vitro and in vivo. J Mater Chem B. 2018;6(36):5738–49. https://doi.org/10.1039/C8TB01310A.
Shang L, Ma B, Wang F, Li J, Shen S, Li X, Liu H, Ge S. Nanotextured silk fibroin/hydroxyapatite biomimetic bilayer tough structure regulated osteogenic/chondrogenic differentiation of mesenchymal stem cells for osteochondral repair. Cell Prolif. 2020;53(11):e12917. https://doi.org/10.1111/cpr.12917.
Behera S, Naskar D, Sapru S, Bhattacharjee P, Dey T, Ghosh AK, Mandal M, Kundu SC. Hydroxyapatite reinforced inherent RGD containing silk fibroin composite scaffolds: promising platform for bone tissue engineering. Nanomed: Nanotechnol, Biol Med. 2017;13(5):1745–59.
Kang H-W, Tabata Y, Ikada Y. Fabrication of porous gelatin scaffolds for tissue engineering. Biomaterials. 1999;20(14):1339–44. https://doi.org/10.1016/S0142-9612(99)00036-8.
Djagny VB, Wang Z, Xu S. Gelatin: a valuable protein for food and pharmaceutical industries: review. Crit Rev Food Sci Nutr. 2001;41(6):481–92. https://doi.org/10.1080/20014091091904.
Piao Y, Chen B. Synthesis and mechanical properties of double cross-linked gelatin-graphene oxide hydrogels. Int J Biol Macromol. 2017;101:791–8. https://doi.org/10.1016/j.ijbiomac.2017.03.155.
Mehedi Hasan M, Nuruzzaman Khan M, Haque P, Rahman MM. Novel alginate-Di-aldehyde cross-linked gelatin/nano-hydroxyapatite bioscaffolds for soft tissue regeneration. Int J Biol Macromol. 2018;117:1110–7. https://doi.org/10.1016/j.ijbiomac.2018.06.020.
Nabavinia M, Khoshfetrat AB, Naderi-Meshkin H. Nano-hydroxyapatite-alginate-gelatin microcapsule as a potential osteogenic building block for modular bone tissue engineering. Mater Sci Eng, C. 2019;97:67–77. https://doi.org/10.1016/j.msec.2018.12.033.
Dou X-C, Zhu X-P, Zhou J, Cai H-Q, Tang J, Li Q-L. Minocycline-released hydroxyapatite–gelatin nanocomposite and its cytocompatibility in vitro. Biomed Mater. 2011;6(2):025002. https://doi.org/10.1088/1748-6041/6/2/025002.
Kailasanathan C, Selvakumar N, Naidu V. Structure and properties of titania reinforced nano-hydroxyapatite/gelatin bio-composites for bone graft materials. Ceram Int. 2012;38(1):571–9. https://doi.org/10.1016/j.ceramint.2011.07.045.
Nosrati H, Sarraf Mamoory R, Le Svend DQ, Bünger CE. Fabrication of gelatin/hydroxyapatite/3D-graphene scaffolds by a hydrogel 3D-printing method. Mater Chem Physics. 2020;239:122305. https://doi.org/10.1016/j.matchemphys.2019.122305.
Salifu AA, Lekakou C, Labeed F. Multilayer cellular stacks of gelatin-hydroxyapatite fiber scaffolds for bone tissue engineering. J Biomed Mater Res Part A. 2017;105(3):779–89. https://doi.org/10.1002/jbm.a.35954.
Papenburg BJ, Liu J, Higuera GA, Barradas AMC, de Boer J, van Blitterswijk CA, Wessling M, Stamatialis D. Development and analysis of multi-layer scaffolds for tissue engineering. Biomaterials. 2009;30(31):6228–39. https://doi.org/10.1016/j.biomaterials.2009.07.057.
Dennis SC, Whitlow J, Detamore MS, Kieweg SL, Berkland CJ. Hyaluronic-acid–hydroxyapatite colloidal gels combined with micronized native ECM as potential bone defect fillers. Langmuir. 2017;33(1):206–18. https://doi.org/10.1021/acs.langmuir.6b03529.
Zhao N, Wang X, Qin L, Zhai M, Yuan J, Chen J, Li D. Effect of hyaluronic acid in bone formation and its applications in dentistry. J Biomed Mater Res, Part A. 2016;104(6):1560–9. https://doi.org/10.1002/jbm.a.35681.
Toole BP. Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer. 2004;4(7):528–39. https://doi.org/10.1038/nrc1391.
Subramaniam S, Fang Y-H, Sivasubramanian S, Lin F-H, Lin C. Hydroxyapatite-calcium sulfate-hyaluronic acid composite encapsulated with collagenase as bone substitute for alveolar bone regeneration. Biomaterials. 2016;74:99–108. https://doi.org/10.1016/j.biomaterials.2015.09.044.
Song JE, Tian J, Kook YJ, Thangavelu M, Choi JH, Khang G. A BMSCs-Laden Quercetin/duck’s feet collagen/hydroxyapatite sponge for enhanced bone regeneration. J Biomed Mater Res, Part A. 2020;108(3):784–94. https://doi.org/10.1002/jbm.a.36857.
Yang X, Li Y, He W, Huang Q, Zhang R, Feng Q. Hydroxyapatite/collagen coating on PLGA electrospun fibers for osteogenic differentiation of bone marrow mesenchymal stem cells. J Biomed Mater Res, Part A. 2018;106(11):2863–70. https://doi.org/10.1002/jbm.a.36475.
Tampieri A, Iafisco M, Sandri M, Panseri S, Cunha C, Sprio S, Savini E, Uhlarz M, Herrmannsdörfer T. Magnetic bioinspired hybrid nanostructured collagen–hydroxyapatite scaffolds supporting cell proliferation and tuning regenerative process. ACS Appl Mater Interfaces. 2014;6(18):15697–707. https://doi.org/10.1021/am5050967.
Chen L, Wu Z, Zhou Y, Li L, Wang Y, Wang Z, Chen Y, Zhang P. Biomimetic porous collagen/hydroxyapatite scaffold for bone tissue engineering. J Appl Polym Sci. 2017;134(37):45271. https://doi.org/10.1002/app.45271.
Parisi C, Salvatore L, Veschini L, Serra MP, Hobbs C, Madaghiele M, Sannino A, Di Silvio L. Biomimetic gradient scaffold of collagen–hydroxyapatite for osteochondral regeneration. J Tissue Eng. 2020;11:2041731419896068. https://doi.org/10.1177/2041731419896068.
Soriente A, Fasolino I, Gomez-Sánchez A, Prokhorov E, Buonocore GG, Luna-Barcenas G, Ambrosio L, Raucci MG. Chitosan/hydroxyapatite nanocomposite scaffolds to modulate osteogenic and inflammatory response. J Biomed Mater Res, Part A. 2022;110(2):266–72. https://doi.org/10.1002/jbm.a.37283.
Nazeer MA, Yilgör E, Yilgör I. Intercalated chitosan/hydroxyapatite nanocomposites: promising materials for bone tissue engineering applications. Carbohyd Polym. 2017;175:38–46. https://doi.org/10.1016/j.carbpol.2017.07.054.
Gritsch L, Maqbool M, Mouriño V, Ciraldo EF, Cresswell M, Jackson PR, Lovell C, Boccaccini AR. Chitosan/hydroxyapatite composite bone tissue engineering scaffolds with dual and decoupled therapeutic ion delivery: copper and strontium. J Mater Chem B. 2019;7(40):6109–24. https://doi.org/10.1039/C9TB00897G.
Bendtsen ST, Quinnell SP, Wei M. Development of a novel alginate-polyvinyl alcohol-hydroxyapatite hydrogel for 3D bioprinting bone tissue engineered scaffolds. J Biomed Mater Res, Part A. 2017;105(5):1457–68. https://doi.org/10.1002/jbm.a.36036.
Liu S, Hu Y, Zhang J, Bao S, Xian L, Dong X, Zheng W, Li Y, Gao H, Zhou W. Bioactive and biocompatible macroporous scaffolds with tunable performances prepared based on 3D printing of the pre-crosslinked sodium alginate/hydroxyapatite hydrogel ink. Macromol Mater Eng. 2019;304(4):1800698. https://doi.org/10.1002/mame.201800698.
Ocando C, Dinescu S, Samoila I, Daniela Ghitulica C, Cucuruz A, Costache M, Averous L. Fabrication and properties of alginate-hydroxyapatite biocomposites as efficient biomaterials for bone regeneration. Eur Polymer J. 2021;151:110444. https://doi.org/10.1016/j.eurpolymj.2021.110444.
Raucci MG, Demitri C, Soriente A, Fasolino I, Sannino A, Ambrosio L. Gelatin/nano-hydroxyapatite hydrogel scaffold prepared by sol-gel technology as filler to repair bone defects. J Biomed Mater Res, Part A. 2018;106(7):2007–19. https://doi.org/10.1002/jbm.a.36395.
Huang T, Fan C, Zhu M, Zhu Y, Zhang W, Li L. 3D-printed scaffolds of biomineralized hydroxyapatite nanocomposite on silk fibroin for improving bone regeneration. Appl Surf Sci. 2019;467–468:345–53. https://doi.org/10.1016/j.apsusc.2018.10.166.
FathimaShahithaJahirHussain MA, Al Saadi A. Preparation and Characterization of Hyaluronic Acid/ Hydroxyapatite Composite (HA/HAp) Scaffolds for Bone Tissue Engineering. Annals of the Romanian Society for Cell Biology. 2021;25:412822–33.
Chocholata P, Kulda V, Dvorakova J, Kolaja Dobra J, Babuska V. Biological evaluation of polyvinyl alcohol hydrogels enriched by hyaluronic acid and hydroxyapatite. Int J Mol Sci. 2020;21(16):5719. https://doi.org/10.3390/ijms21165719.
Liu H, Wang C, Sun X, Zhan C, Li Z, Qiu L, Luo R, Liu H, Sun X, Li R, Zhang J. Silk fibroin/collagen/hydroxyapatite scaffolds obtained by 3D printing technology and loaded with recombinant human erythropoietin in the reconstruction of alveolar bone defects. ACS Biomater Sci Eng. 2022. https://doi.org/10.1021/acsbiomaterials.2c00690.
Acknowledgements
The author G. Radha would like to acknowledge the Indian Council of Medical Research (ICMR-RA – No.45/50/2020-Nan/BMS) for the support. The author also acknowledges the MHRD RUSA 2.0 scheme (C3/RI&QI/RUSA 2.0/Theme-2/Group-2/Award/2021/034), University of Madras, to carry out this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Radha, G., Manjubaashini, N. & Balakumar, S. Nano-hydroxyapatite/natural polymer composite scaffolds for bone tissue engineering: a brief review of recent trend. In vitro models 2, 125–151 (2023). https://doi.org/10.1007/s44164-023-00049-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44164-023-00049-w