Abstract
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disorder with phenotypic and genetic heterogeneity. Recent studies have suggested an oligogenic basis of ALS, in which the co-occurrence of two or more genetic variants has additive or synergistic deleterious effects. To assess the contribution of possible oligogenic inheritance, we profiled a panel of 43 relevant genes in 57 sporadic ALS (sALS) patients and eight familial ALS (fALS) patients from five pedigrees in east China. We filtered rare variants using the combination of the Exome Aggregation Consortium, the 1000 Genomes and the HuaBiao Project. We analyzed patients with multiple rare variants in 43 known ALS causative genes and the genotype–phenotype correlation. Overall, we detected 30 rare variants in 16 different genes and found that 16 of the sALS patients and all the fALS patients examined harbored at least one variant in the investigated genes, among which two sALS and four fALS patients harbored two or more variants. Of note, the sALS patients with one or more variants in ALS genes had worse survival than the patients with no variants. Typically, in one fALS pedigree with three variants, the family member with three variants (Superoxide dismutase 1 (SOD1) p.V48A, Optineurin (OPTN) p.A433V and TANK binding kinase 1 (TBK1) p.R573H) exhibited much more severe disease phenotype than the member carrying one variant (TBK1 p.R573H). Our findings suggest that rare variants could exert a negative prognostic effect, thereby supporting the oligogenic inheritance of ALS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disorder with a substantial heritable component (Goutman et al. 2022a). Mendelian familial ALS (fALS) accounts for 10–15% of individuals with the disease. Approximately, 90% of cases are sporadic and do not have any family history. The pathogenesis of ALS remains inadequately understood. Recent studies have raised a gene–time–environment hypothesis, which posits that genetic predisposition interacts with environmental exposures over time leading to ALS (Al-Chalabi and Hardiman 2013; Goutman et al. 2022b). Heredity plays an important role in the cause of ALS, even in sporadic ALS (sALS) patients. The heritability of sALS has been estimated to be 12–21% in genome-wide association studies (Fogh et al. 2014; Keller 2014) to as high as 61% in twin studies (Al-Chalabi et al. 2010). The first ALS gene, Superoxide dismutase 1 (SOD1), was discovered through linkage analysis in 1993 (Rosen et al. 1993). Moreover, over the past decade, the number of genes associated with ALS has increased dramatically. Currently, more than 150 genes have been identified to be related to ALS (http://alsod.iop.kcl.ac.uk); among them are approximately 20 genes are with high penetrance, such as SOD1, Chromosome 9 open reading frame 72 (C9ORF72), TAR DNA-binding protein (TARDBP) and Fused in sarcoma (FUS), whereas the rest are reported to increase the risk of ALS (Shatunov and Al-Chalabi 2021).
Accordingly, lines of evidence have proposed an oligogenic basis of ALS (Al-Chalabi et al. 2017; van Blitterswijk et al. 2012). The hypothesis was firstly developed from the fact that asymptomatic carriers are common even in pedigrees with variants in high-penetrant genes such as SOD1. We have reported p.Gly141Ala mutation in the SOD1 gene associated with incomplete penetrance (Dong et al. 2020). Description of compound heterozygous and recessive SOD1 mutations suggests that oligogenic inheritance may account for incomplete penetrance (Gentile et al. 2021; Kuuluvainen et al. 2019). Subsequently, a series of studies have reported the coexistence of multiple variants in ALS causal genes in both sALS and fALS patients (Cady et al. 2015; Dols-Icardo et al. 2018; Giannoccaro et al. 2017; McCann et al. 2020; Morgan et al. 2017; Naruse et al. 2019; Pang et al. 2017; Scarlino et al. 2020; Shepheard et al. 2021). Among them, several studies suggested that the additional variant in the ALS causative gene may influence ALS phenotypes such as the onset of age (Cady et al. 2015; Naruse et al. 2019; Shepheard et al. 2021), survival (Pang et al. 2017; Scarlino et al. 2020), and co-occurrence with dementia (Dols-Icardo et al. 2018; Giannoccaro et al. 2017) or parkinsonism (Giannoccaro et al. 2017).
Although oligogenic inheritance is reported in several studies, further studies in different ethnic populations are crucial. In this study, to assess the contribution of possible oligogenic inheritance, by profiling a panel of 43 relevant genes in 57 sALS patients and eight familial fALS patients from five pedigrees in east China, we have demonstrated that ALS patients can carry more than one variant in ALS causative genes, and that the presence of rare variants is associated with poorer survival in both sALS patients and an ALS pedigree. Our findings suggested that rare variants could exert a negative prognostic effect, supporting the oligogenic inheritance of ALS.
Materials and Methods
Subjects
Between 2011 and 2020, ALS patients who were diagnosed and followed up at Huashan Hospital, Shanghai were systematically enrolled. All subjects were evaluated by neuromuscular specialists and fulfilled the criteria for definite ALS, probable ALS, or probable ALS-laboratory-supported based on the revised El Escorial criteria (Brooks et al. 2000). Data on sex, age, site of onset, and treatment with riluzole were recorded and those on survival, defined as the time from symptom onset to permanent assisted ventilation (≥ 23 h per day noninvasive ventilation), tracheostomy, or death, whichever is earlier, were recorded. Written informed consent was obtained from all the participating subjects.
Controls
An exon database named "HuaBiao" (https://www.biosino.org/wepd), which contains deep sequencing (> 100 ×) of 5000 healthy samples collected mainly from three representative Han Chinese populations at Zhengzhou, Taizhou and Nanning, was used for case–control association tests (Hao et al. 2021). High-quality reads (mean Phred score > 30) and high sequencing depth of samples (mean depth > 100 ×) were processed by the same procedures as ALS subjects. Only protein-coding regions were included for downstream analyses.
Genotyping and Rare Variant Filtering
Genomic DNA was extracted from the whole blood of individual subjects according to standard protocols. Next-generation sequencing (NGS) library preparation and whole-exome sequencing (WES) was performed using commercial assay kits (NGS Library Prep kits and Nimblegen SeqCap EZ Human Exome Kit v3.0 kits, Roche). NGS was performed by Illumina HiSeq system with 140 bp of paired-end reads. The mean sequencing depth of the targeted exome region reached at least 60 × in both cases and controls. The WES data were processed through the Genome Analysis Toolkit best practice pipeline before variant calling, and HaplotypeCaller was used (www.biostars.org/) to call the variants in parallel. Variant annotation and filtering were performed by ANNOVAR with sorting intolerant from torelant (SIFT, http://sift.jcvi.org/) and PolyPhen2 (http://genetics.bwh.harvard.edu/pph2/), and by SnpEff with GENCODE (http://snpeff.sourceforge.net/) as an annotation database. Population frequencies for each variant were determined in dbSNP, the 1000 Genomes Project, and the Exome Aggregation Consortium (ExAC) (http://exac.broadinstitute.org). Under the "rare disease, rare mutation" criteria, only non-synonymous variants with minor allele frequency (MAF) of less than 0.01% across all populations in ExAC and 1000 Genomes Project datasets were selected. All of the variants had a sequencing quality score (Phred) of at least 50 and a mapping quality score of at least 20.
ALS Candidate Genes
Genes for the ALS panel were selected from the Amyotrophic Lateral Sclerosis online Database (ALSoD, http://alsod.iop.kcl.ac.uk/) and the Online Mendelian Inheritance in Man (OMIM, http://www.omim.org/) databases and two latest studies (Goutman et al. 2022b; Mohassel et al. 2021). Forty-one causative ALS genes (Amyotrophic lateral sclerosis 2 (ALS2), Angiogenin (ANG), Annexin A11 (ANXA11), Cilia and flagella associated protein 410 (C21orf2), Calmodulin binding transcription activator 1 (CAMTA1), Cyclin F (CCNF), Coiled-coil-helix-coiled-coil-helix domain containing 10 (CHCHD10), Charged multivesicular body protein 2B (CHMP2B), Cylindromatosis (CYLD), Dynactin subunit 1 (DCTN1), DnaJ heat shock protein family member C7 (DNAJC7), Elongator acetyltransferase complex subunit 3 (ELP3), Ephrin type-A receptor 4 (EPHA4), Erb-B2 receptor tyrosine kinase 4 (ERBB4), Fig4 phosphoinositide 5-phosphatase (FIG4), Fused in sarcoma (FUS), Glycosyltransferase 8 domain containing 1 (GLT8D1), Heterogeneous nuclear ribonucleoprotein A1 (HNRNPA1), Heterogeneous nuclear ribonucleoprotein A2/B1 (HNRNPA2B1), Kinesin family member 5A (KIF5A), Lectin galactoside binding like protein (LGALSL), Matrin 3 (MATR3), Neurofilament heavy chain (NEFH), NIMA related kinase 1 (NEK1), Optineurin (OPTN), Profilin 1 (PFN1), Peripherin (PRPH), Senataxin (SETX), Sigma non-opioid intracellular receptor 1 (SIGMAR1), Superoxide dismutase 1 (SOD1), Spastic paraplegia 11 (SPG11), Serine palmitoyltransferase long chain base subunit 1 (SPTLC1), Sequestosome 1 (SQSTM1), TAR DNA binding protein (TARDBP), TANK binding kinase 1 (TBK1), Cytotoxic granule associated RNA binding protein (TIA1), Tubulin alpha 4A (TUBA4A), Ubiquilin 2 (UBQLN2), Unc-13 homolog A (UNC13A), Vesicle-associated membrane protein associated protein B/C (VAPB), and Valosin containg protein (VCP)) were examined for rare variants. The Chromosome 9 open reading frame 72 (C9orf72) repeat expansion and Ataxin 2 (ATXN2) repeat expansion were analyzed in all the patients using repeat-primed polymerase chain reactions.
Statistical Analysis
Statistical analyses were performed in R v4.0.3 to identify any association between clinical variables including sex, age at disease onset, site of disease onset (bulbar or spinal), and disease duration. A χ2 analysis was performed between sex and site of onset, whereas Welch's t-tests were performed between the age of onset and both sex and site of onset. The Kaplan–Meier survival analyses were performed between disease duration and both sex and site of onset. Survival was defined as the time from symptom onset to permanent assisted ventilation (≥ 23 h per day noninvasive ventilation), tracheostomy, or death. In addition, a linear regression model was fitted between age of onset and duration.
Whether the number of ALS-implicated variants carried by individuals influenced their clinical presentation was also assessed. To identify rare and novel single-nucleotide polymorphisms (SNPs) that might be overrepresented in sALS subjects, Fisher's exact tests were used to compare each candidate SNV's allele frequency in sALS versus controls. One-way analysis of variance was used to assess the association between the number of rare non-synonymous variants (Non-syn RV) and age at onset. The Kaplan–Meier survival analyses were performed between disease duration and the presence of both non-synonymous rare variants (Non-syn RV) and synonymous rare variants (Syn RV). After adjustment for onset age, sex and site of onset, the hazard ratio between the number of rare variants and survival status was estimated by Cox regression. All the hazard ratios in this paper were estimated by penalized regression model using glmnet v4.1 to correct left-truncation bias that might arise from death before being able to undergo the genetic tests (McGough et al. 2021).
Results
Subject Phenotypic Characteristics
Demographic characteristics for all 57 sequenced sALS subjects and eight fALS subjects from five pedigrees are shown in Table 1. The mean (SD) age of onset was 55.0 ± 10.7 years in sALS patients and 43.1 ± 7.7 in eight fALS patients. Of sALS and fALS patients, 68.4% and 60% were male, respectively. Bulbar onset was present in 14 sALS patients (24.6%) but not in fALS patients. Riluzole was administered in 46 sALS patients and all fALS patients for at least one month. After a median of 29 (interquartile range 19–45) months, 53 sALS patients had reached the end point. The follow-up time of eight fALS patients (i.e., Pedigree A: III7 and IV4, Pedigree B:III1, Pedigree C: II7, Pedigree D: III18, three members of Pedigree E not shown) was short, thus, only two patients reached the end point, the survival time of which was 24 months (Pedigree A, III7) and 47 months (Pedigree E, III2) (Table 1, Fig. 1).
ALS pedigrees with multiple variants of interest. Examined subjects are indicated by the crosses above the pedigree symbol. The arrows indicate the probands. The age at onset and the age at death or current age are indicated at the top of the symbols. The variants harbored are indicated at the bottom of the symbols. ALS amyotrophic lateral sclerosis
Statistical analyses were performed to identify any association between clinical variables, namely sex, age at disease onset, site of disease onset and disease duration (Fig. 2a–f). There was no significant association between gender and any of the other three indicators (Fig. 2a–c); however, there was a high propensity for women to develop bulbar onset and for men to present with spinal onset (Fig. 2c). The cases with bulbar onset were more likely to have later age of onset (p = 0.0159, Fig. 2d) and reduced life expectancy (p = 0.031, Fig. 2e). There was also a tendency that patients with later onset present shorter disease duration (Fig. 2f).
Statistical analysis of clinical variables for 57 sALS cases. a Association between sex and age at onset. b Kaplan–Meier survival curves for ALS patients stratified by gender. c Association between sex and site of onset. d Association between the site of onset and age at onset. e Kaplan–Meier survival curves for ALS patients stratified by site of onset. f Association between survival and age at onset. ALS, amyotrophic lateral sclerosis; sALS, sporadic ALS
Rare Variant Identifications
Of the 43 causative genes examined, 43 missense variants with MAF < 0.01% in ExAC and 1000 Genomes were filtered, as shown in Table 2. The pathogenicity of each variant was evaluated according to the American College of Medical Genetics and Genomics (ACMG) standards (Richards et al. 2015). Considering the heterogeneity of common SNPs in different ethnic populations, the frequency of the loci found in the HuaBiao database was also explored, which consists of 5000 healthy Han Chinese. Fisher's exact tests were performed to calculate whether there was a significant difference in the frequency of these SNPs between the ALS cohort and the Chinese healthy population. We identified 13 of the variants with MAF < 0.01 in the ExAC and 1000 Genomes, which are relatively common (p > 0.05) in the Chinese population (Table 2, common variants in the Chinese population), whereas the other 30 variants in 16 different genes are rare in both Chinese and Caucasian populations (Table 2, rare variants in the Chinese population). Some synonymous variants of 30 genes were also found (Supplementary Table 1).
Patients with Multiple Rare Variants
After the exclusion of the 10 relatively common variants in the Chinese population, all eight fALS patients from five different pedigrees examined had at least one rare non-synonymous variant within the 30 causative ALS genes. Three fALS patients (37.5%) from different families harbored two variants (SOD1 p.G94R + SQSTM1 p.G262R; SOD1 p.F22G + FUS p.P151S; TARDBP p.G298V + SETX p.I1304W) and one patient (12.5%) harbored three variants (SOD1 p.V48A + OPTN p.A433V + TBK1 p.R573H). The four pedigrees with multiple rare variants are shown in Fig. 1.
Only one out of five pedigrees exhibited monogenic nature, albeit with incomplete penetrance, which we have reported before (Dong et al. 2020). Of the sALS patients, 18 (31.6%) had at least one rare non-synonymous variant within the 30 causative ALS genes; one (3.5%) harbored two variants (SETX p.I1520T + C21orf2 p.R172W), and one harbored three variants (ALS2 p.E697K + SPG11 p.C1734F + NEFH p.P933S).
Effect of Rare Variants on Survival
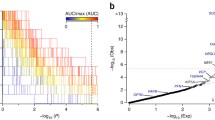
Within 43 causative ALS genes, we found that presence of non-synonymous variants is associated with lower survival probability in sALS patients (log-rank test, p = 0.007, Fig. 3b), whereas the presence of synonymous variants is not associated with lower survival probability (log-rank test, p = 0.59, Fig. 3c). After adjustment for age of onset, sex and bulbar onset, it was found that the presence of rare non-synonymous still remained associated with survival, increasing the risk of death/ventilator dependence (hazard ratio = 3.93, 95% CI = 1.53–79, p < 0.05). Patients with two or more variants did not exhibit reduced survival probability when compared with patients with one variant, which may be explained by the too-small sample size, as only two sALS patients harbored more than one rare variant, the duration of which was 24 and 31 months. Bulbar onset also increased the hazard risk of death/ventilator dependence when compared with spinal onset (hazard ratio = 2.43, 95% CI = 1.23–4.82, p < 0.05). However, there is no significance between the number of non-synonymous variants and age at onset (Fig. 3a).
Effect of rare variants on disease onset and survival. a Association between the number of rare non-synonymous variants (Non-syn RV) and age at onset. b Kaplan–Meier survival curves for ALS patients stratified by the presence of non-synonymous rare variants (Non-syn RV) in 43 ALS causative genes. c Kaplan–Meier survival curves for ALS patients stratified by the presence of synonymous rare variants (Syn RV) in 43 ALS causative genes. ALS, amyotrophic lateral sclerosis
Interestingly, although the fALS patients were not included in the survival analysis for insufficient sample size, we still observed significant heterogeneity of survival in Pedigree A (Fig. 1). Three family members, that is II1, III4 and III7 in Pedigree A, presented with a typical rapid ALS progression, whereas two other members, I1 and IV4, manifested a prolonged duration of disease. Whole-exome sequencing demonstrated a novel SOD1 p.V48A (c.T143 > C) variant in addition to the OPTN p.A433V (c.C1298 > T) and TBK1 p.R573H (c.G1718 > A) variants in III7, whereas only the TBK1 variant was detected in IV4. This finding suggests that the burden of rare variants is associated with survival, consistent with what we found in sALS patients.
Discussion
In this study, we profiled a panel of 43 relevant genes in 57 sALS patients and five ALS pedigrees from east China. Overall, we detected 30 rare variants in 16 different genes and found that the presence of rare variants is associated with poorer survival in both sALS patients and an ALS pedigree with three variants.
Considering the heterogeneity of common SNPs in different ethnic populations, we adopted the HuaBiao database, which consists of 5000 healthy Han Chinese as controls. Cases and control WES were performed by utilizing the same library preparation kits. However, we were unable to perform variant calling jointly in the case and control datasets. We identified 13 variants that were rare in the ExAC and 1000 Genomes but were relatively common (p > 0.05 by Fisher exact test) in the Chinese population. Interestingly, eight of the 13 variants have been reported before in other Amyorophic lateral slerosis and Frontotemporal dementia (ALS-FTD) studies (Kim et al. 2016, 2018; Nahm et al. 2020; Naruse et al. 2019; Pang et al. 2017; Zhang et al. 2018a, b), namely ERBB4 p.I658F, NEK1 p.287A, SETX p.1331L, SETX p.E756V, SETX p.E813D, ANXA11 p.T321N, SPG11 p.L1982S and NEFH p.A380T (Table 2, common variants in the Chinese population). Our study suggests that these variants may not be directly associated with the disease, whereas the other 30 variants that are rare in the ExAC, 1000 Genomes and HuaBiao database may be causally associated with the disease. Among them, 12 variants (TARDBP p.G298S, SQSTM1 p.G262R, SETX p.M1912T, TBK1 p.R573H, SPG11 p.H235fs, FUS p.P151S, FUS p.R520C, SOD1 p.E22G, SOD1 p.V48A, SOD1 p.G94R, SOD1 p.G142A, and NEFH p.T642M) have been reported in ALS-FTD studies (Cirulli et al. 2015; Dong et al. 2020; Elshafey et al. 1994; Fujisawa et al. 2012; Giau et al. 2019; Kim et al. 2018; Kwiatkowski et al. 2009; Narain et al. 2018; Siddique and Deng 1996; Stevanin et al. 2008; Tunca et al. 2020; Zhang et al. 2018a), and three variants (ALS2 p.E697K, OPTN p.D527fs, and C21orf2 p.R172W) were not reported, but recorded in ALS databases (ALSoD, ALSdb or Project MinE). Fifteen variants (DCTN1 p.R651Q, DCTN1 p.Y224F, ALS2 p.L385S, CHMP2B p.T156A, SETX p.I1520T, SETX p.L1304W, OPTN p.A433V, KIF5A p.P1024S, TBK1 p.S398P, SPG11 p.C1734F, SPG11 p.Q809P, SPG11 p.H86D, UNC13A p.P431L, SOD1 p.E134X, and NEFH p.P933S) were novel, which have not been reported in ALS-FTD studies or recorded in ALS databases. Our study provided support for the association of these variants with disease. However, because it is difficult to conclusively demonstrate pathogenicity without pedigree information, most of the rare variants we identified were classified as variants of uncertain significance according to the ACMG. Eight rare variants (TARDBP p.G298V, SPG11 p.H235fs, FUS p.R521C, SOD1 p.E22G, SOD1 p.V48A, SOD1 p.G94R, SOD1 p.E134X and SOD1 p.142A) are classified as pathogenic or likely pathogenic (Table 2). Apart from SOD1 p.E134X, all other variants have been reported. Of note, SPG11 p.H235fs was heterozygous, whereas SPG11 mutations are usually autosomal recessive. Resultantly, the clinical significance of SPG11 p.H235fs is uncertain.
We identified several patients who carry more than one variant, accounting for 3.51% of sALS and 50% of fALS patients who we examined, suggesting a possible oligogenic basis. Furthermore, we used a chord diagram to show patients with multiple rare variants (Fig. 4). ALS genes were divided into four categories based on previous literature (Nguyen et al. 2018), including "impaired autophagy/proteostasis", "cytoskeletal defect", "mitochondrial dysfunction and impaired DNA repair", and "disturbed RNA metabolism" (Fig. 4a). Patients harbored multiple rare variants discovered in our study are presented in Fig. 4b. SOD1 was the most detected gene, which was detected simultaneously with four other genes, three of which were related to autophagy. We also reviewed reported multiple gene rare variant carriers with ALS or ALS-FTD (Farhan et al. 2018; Keogh et al. 2018; Lamp et al. 2018; Lattante et al. 2021; Liu et al. 2021a, b; McCann et al. 2020; Müller et al. 2018; Narain et al. 2019; Naruse et al. 2019; Nguyen et al. 2018; Pang et al. 2017; Ross et al. 2020; Scarlino et al. 2020; Sghaier et al. 2022; Tripolszki et al. 2019; Vazquez-Costa et al. 2019; Yang et al. 2021; Yilmaz et al. 2022; Zhang et al. 2018a) (Supplementary Table 2, Fig. 3c). C9orf72 was the most detected gene, accounting for 112 times, which may be because C9orf72 mutation is the most common known cause of ALS. However, C9orf72 G4C2 expansion is extremely rare in the Chinese population (Zou et al. 2013) and was not detected in our cohort. Similarly, SOD1 accounted for a large proportion, which was 59 times. It is worth noting that several autophagy genes, including TBK1, OPTN and SQSTM1, the mutations of which were not common in ALS-FTD patients, account for a considerable proportion in multiple gene rare variant carriers, accounting for 38, 42 and 36 times, respectively. The co-occurrence of TBK1 and OPTN, TBK1 and SQSTM1 was frequently detected. In addition, these three genes frequently coexist with SOD1 and genes relating to RNA metabolism, such as C9orf72 and FUS.
Patients with multiple rare variants. a Biological process affected by mutations in ALS genes: different colors represent different biological processes, and illustrations are also applicable in panels b and c. b Chord diagram illustrating patients with multiple rare variants in our study. The x-axis represents the number of times one gene variant was detected alongside another; the width of the chord connecting the two genes represents the number of times they occur together. Different colors represent different biological processes. c Chord diagram illustrating reported multiple gene rare variant carriers with ALS or ALS-FTD. ALS, amyotrophic lateral sclerosis
Although a series of papers have reported the co-occurrence of variants in ALS genes (Cady et al. 2015; Dols-Icardo et al. 2018; McCann et al. 2020; Morgan et al. 2017; Naruse et al. 2019; Pang et al. 2017; Scarlino et al. 2020; Shepheard et al. 2021), the presence of the oligogenic nature of ALS remains debatable. Notably, the reported percentage of patients who harbored more than one variant varied much, from as low as 1% (Morgan et al. 2017) to as high as 19.5% (Pang et al. 2017). This difference is caused by the inconsistency in the selection of sequenced genes and criteria for filtering potentially pathogenic variants. Some studies adopted very rigorous filtering criteria that only include pathogenic or likely pathogenic variants in high-penetrant genes, whereas other studies, including ours, also had some variants of uncertain significance according to the ACMG standards (Richards et al. 2015). The ACMG standards are very practical for clinical use, but for non-strictly Mendelian diseases such as ALS, only including variants that are classified as pathogenic or likely pathogenic may lead to underestimation of the significance of some variants in low-penetrant or risk genes. Some other studies did not exclude SNPs that were relatively common in the control population, resulting in a falsely high proportion of patients with multiple rare variants. In our study and some other studies (Shepheard et al. 2021), population-matched WES data were adopted to avoid such flaws. In addition, Keogh et al. (2018) suggested that individuals with ALS are more likely to harbor a known genetic risk factor, and it is the burden of these variants in combination with rare benign alleles that is likely to be responsible for some oligogenic associations. Therefore, further mechanistic functional analyses or segregation studies are warranted to scrutinize the pathogenicity of each of the variants that we identified and the synergy of these variants.
Next, we explored whether the presence of rare variants was associated with the survival of ALS patients, and we found that sALS patients with one or more variants in ALS causative genes had worse survival than patients with no variants. In addition, in an ALS pedigree with three variants, the family member III7 with three variants (SOD1 p.V48A, OPTN p.A433V and TBK1 p.R573H) exhibited much more severe disease phenotype than IV4 who carries one variant (TBK1 p.R573H). This observation provides strong support for our conclusions in sALS patients. However, Pang and Scarlino reported that patients with two variants exhibited reduced survival probability when compared with patients with one variant (Pang et al. 2017; Scarlino et al. 2020). This phenomenon was not observed in our cohort, possibly because of our insufficient sample size, as only two sALS patients harbored more than one rare variant.
Few studies have examined genotype–phenotypic relationships within patients from the same family, where the genetic background is so uniform that the effects of oligogenic can be seen. Although here we have reported a possible genotype–phenotype correlation within Pedigree A, the pathogenicity of each variant needs to be investigated. The SOD1 p.V48A variant was recorded in the ALSoD and was reported in a Chinese cohort study (Tang et al. 2019). It was classified as pathogenic according to the ACMG standards. In contrast, the absence of the SOD1 variant in the proband who presented slow disease progression indicates that SOD1 is not the only pathogenic gene in this pedigree. We considered the TBK1 variant to contribute to the disease, as it was recorded in the ALSdb database, and was identified by a genome-wide association study (Cirulli et al. 2015). Patients carrying mutations in TBK1 and other ALS genes simultaneously have been frequently reported (Liu et al. 2021a), especially in the genes related to the autophagy pathway (OPTN and SQSTM1) (Black et al. 2017; Dols-Icardo et al. 2018; Lattante et al. 2019; Liu et al. 2021a; Pottier et al. 2015) or RNA homeostasis and trafficking (C9ORF72, FUS, and TARDBP) (Black et al. 2017; de Majo et al. 2018; Muller et al. 2018; van der Zee et al. 2017). These studies as well as ours have suggested that TBK1 belongs to the genes that might cause an increased risk of developing the disease or an earlier onset of the disease, supporting the oligogenic hypothesis.
Conclusions
In this study, we demonstrated that ALS patients can carry more than one variant in ALS causative genes, and that the presence of rare variants is associated with survival in both sALS patients and an ALS pedigree. Our findings suggested that rare variants could exert a negative prognostic effect, thereby supporting the oligogenic inheritance of ALS.
Data Availability
The datasets generated from the statistical analyses during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACMG:
-
The American College of Medical Genetics and Genomics
- ALS:
-
Amyotrophic lateral sclerosis
- ALS2:
-
Amyotrophic lateral sclerosis 2
- ALSdb:
-
ALS data browser
- ALSod:
-
Amyotrophic Lateral Sclerosis online Database
- ANG:
-
Angiogenin
- ANXA11:
-
Annexin A11
- ATXN2:
-
Ataxin 2
- C9orf72:
-
Chromosome 9 open reading frame 72
- C21orf2:
-
Cilia- and flagella-associated protein 410
- CAMTA1:
-
Calmodulin-binding transcription activator 1
- CCNF:
-
Cyclin F
- CHCHD10:
-
Coiled-coil-helix-coiled-coil-helix domain containing 10
- CHMP2B:
-
Charged multivesicular body protein 2B
- CYLD:
-
Cylindromatosis
- DCTN1:
-
Dynactin subunit 1
- DNAJC7:
-
DnaJ heat shock protein family (Hsp40) member C7
- ELP3:
-
Elongator acetyltransferase complex subunit 3
- EPHA4:
-
Ephrin type-A receptor 4
- ERBB4:
-
Erb-B2 receptor tyrosine kinase 4
- ExAC:
-
The Exome Aggregation Consortium
- fALS:
-
Familial amyotrophic lateral sclerosis
- FTD:
-
Frontotemporal dementia
- FIG4:
-
FIG4 phosphoinositide 5-phosphatase
- FUS:
-
Fused in sarcoma
- GLT8D1:
-
Glycosyltransferase 8 domain containing 1
- HNRNPA1:
-
Heterogeneous nuclear ribonucleoprotein A1
- HNRNPA2B1:
-
Heterogeneous nuclear ribonucleoprotein A2/B1
- KIF5A:
-
Kinesin family member 5A
- LGALSL:
-
Lectin galactoside-binding-like protein
- MATR3:
-
Matrin 3
- NEFH:
-
Neurofilament heavy chain
- NEK1:
-
NIMA-related kinase 1
- OMIM:
-
Online Mendelian inheritance in man
- OPTN:
-
Optineurin
- PFN1:
-
Profilin 1
- PRPH:
-
Peripherin
- sALS:
-
Sporadic amyotrophic lateral sclerosis
- SETX:
-
Senataxin
- SIGMAR1:
-
Sigma non-opioid intracellular receptor 1
- SNP:
-
Single-nucleotide polymorphisms
- SOD1:
-
Superoxide dismutase 1
- SPG11:
-
Spastic paraplegia 11
- SPTLC1:
-
Serine palmitoyltransferase long chain base subunit 1
- SQSTM1:
-
Sequestosome 1
- TARDBP:
-
TAR DNA-binding protein
- TBK1:
-
TANK-binding kinase 1
- TIA1:
-
Cytotoxic granule-associated RNA-binding protein
- TUBA4A:
-
Tubulin Alpha 4a
- UBQLN2:
-
Ubiquilin 2
- UNC13A:
-
Unc-13 Homolog A
- VAPB:
-
Vesicle-associated membrane protein-associated protein B/C
- VCP:
-
Valosin-containing protein
- WES:
-
Whole-exome sequencing
References
Al-Chalabi A, Fang F, Hanby MF, Leigh PN, Shaw CE, Ye W, Rijsdijk F (2010) An estimate of amyotrophic lateral sclerosis heritability using twin data. J Neurol Neurosur Ps 81(12):1324–1326. https://doi.org/10.1136/jnnp.2010.207464
Al-Chalabi A, van den Berg LH, Veldink J (2017) Gene discovery in amyotrophic lateral sclerosis: implications for clinical management. Nat Rev Neurol 13(2):96–104. https://doi.org/10.1038/nrneurol.2016.182
Al-Chalabi A, Hardiman O (2013) The epidemiology of ALS: a conspiracy of genes, environment and time. Nat Rev Neurol 9(11):617–628. https://doi.org/10.1038/nrneurol.2013.203
Black HA, Leighton DJ, Cleary EM, Rose E, Stephenson L, Colville S, Ross D, Warner J, Porteous M, Gorrie GH, Swingler R, Goldstein D, Harms MB, Connick P, Pal S, Aitman TJ, Chandran S (2017) Genetic epidemiology of motor neuron disease-associated variants in the Scottish population. Neurobiol Aging 51:178. https://doi.org/10.1016/j.neurobiolaging.2017.04.019
Brooks BR, Miller RG, Swash M, Munsat TL, World Federation of Neurology Research Group on Motor Neuron D (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1(5):293–299. https://doi.org/10.1080/146608200300079536
Cady J, Allred P, Bali T, Pestronk A, Goate A, Miller TM, Mitra RD, Ravits J, Harms MB, Baloh RH (2015) Amyotrophic lateral sclerosis onset is influenced by the burden of rare variants in known amyotrophic lateral sclerosis genes. Ann Neurol 77(1):100–113. https://doi.org/10.1002/ana.24306
Cirulli ET, Lasseigne BN, Petrovski S, Sapp PC, Dion PA, Leblond CS, Couthouis J, Lu YF, Wang QL, Krueger BJ, Ren Z, Keebler J, Han YJ, Levy SE, Boone BE, Wimbish JR, Waite LL, Jones AL, Carulli JP, Day-Williams AG, Staropoli JF, Xin WW, Chesi A, Raphael AR, McKenna-Yasek D, Cady J, de Jong JMBV, Kenna KP, Smith BN, Topp S, Miller J, Gkazi A, Al-Chalabi A, van den Berg LH, Veldink J, Silani V, Ticozzi N, Shaw CE, Baloh RH, Appel S, Simpson E, Lagier-Tourenne C, Pulst SM, Gibson S, Trojanowski JQ, Elman L, McCluskey L, Grossman M, Shneider NA, Chung WK, Ravits JM, Glass JD, Sims KB, Van Deerlin VM, Maniatis T, Hayes SD, Ordureau A, Swarup S, Landers J, Baas F, Allen AS, Bedlack RS, Harper JW, Gitler AD, Rouleau GA, Brown R, Harms MB, Cooper GM, Harris T, Myers RM, Goldstein DB, Consortium FS (2015) Exome sequencing in amyotrophic lateral sclerosis identifies risk genes and pathways. Science 347(6229):1436–1441. https://doi.org/10.1126/science.aaa3650
de Majo M, Topp SD, Smith BN, Nishimura AL, Chen HJ, Gkazi AS, Miller J, Wong CH, Vance C, Baas F, ten Asbroek ALMA, Kenna KP, Ticozzi N, Redondo AG, Esteban-Perez J, Tiloca C, Verde F, Duga S, Morrison KE, Shaw PJ, Kirby J, Turner MR, Talbot K, Hardiman O, Glass JD, de Belleroche J, Gellera C, Ratti A, Al-Chalabi A, Brown RH, Silani V, Landers JE, Shaw CE (2018) ALS-associated missense and nonsense TBK1 mutations can both cause loss of kinase function. Neurobiol Aging 71:266. https://doi.org/10.1016/j.neurobiolaging.2018.06.015
Dols-Icardo O, Garcia-Redondo A, Rojas-Garcia R, Borrego-Hernandez D, Illan-Gala I, Munoz-Blanco JL, Rabano A, Cervera-Carles L, Juarez-Rufian A, Spataro N, De Luna N, Galan L, Cortes-Vicente E, Fortea J, Blesa R, Grau-Rivera O, Lleo A, Esteban-Perez J, Gelpi E, Clarimon J (2018) Analysis of known amyotrophic lateral sclerosis and frontotemporal dementia genes reveals a substantial genetic burden in patients manifesting both diseases not carrying the C9orf72 expansion mutation. J Neurol Neurosur Ps 89(2):162–168. https://doi.org/10.1136/jnnp-2017-316820
Dong SQ, Liu XN, Yang WB, Zhou YN, Wang JC, Chen XJ (2020) An exon 5 mutation (c.425G > C, p.Gly141Ala) in the SOD1 gene in a Chinese family associated with incomplete penetrance. Amyotroph Lat Scl Fr 21(5–6):473–476. https://doi.org/10.1080/21678421.2020.1738496
Elshafey A, Lanyon WG, Connor JM (1994) Identification of a new missense point mutation in exon-4 of the Cu/Zn superoxide-dismutase (Sod-1) gene in a family with amyotrophic-lateral-sclerosis. Hum Mol Genet 3(2):363–364. https://doi.org/10.1093/hmg/3.2.363
Farhan SMK, Gendron TF, Petrucelli L, Hegele RA, Strong MJ (2018) OPTN p.Met468Arg and ATXN2 intermediate length polyQ extension in families with C9orf72 mediated amyotrophic lateral sclerosis and frontotemporal dementia. Am J Med Genet B 177(1):75–85. https://doi.org/10.1002/ajmg.b.32606
Fogh I, Ratti A, Gellera C, Lin K, Tiloca C, Moskvina V, Corrado L, Soraru G, Cereda C, Corti S, Gentilini D, Calini D, Castellotti B, Mazzini L, Querin G, Gagliardi S, Del Bo R, Conforti FL, Siciliano G, Inghilleri M, Sacca F, Bongioanni P, Penco S, Corbo M, Sorbi S, Filosto M, Ferlini A, Di Blasio AM, Signorini S, Shatunov A, Jones A, Shaw PJ, Morrison KE, Farmer AE, Van Damme P, Robberecht W, Chi A, Traynor BJ, Sendtner M, Melki J, Meininger V, Hardiman O, Andersen PM, Leigh NP, Glass JD, Overste D, Diekstra FP, Veldink JH, van Es MA, Shaw CE, Weale ME, Lewis CM, Williams J, Brown RH, Landers JE, Ticozzi N, Ceroni M, Pegoraro E, Comi GP, DAlfonso S S, van den Berg LH, Taroni F, Al-Chalabi A, Powell J, Silani V, Collaborators SC (2014) A genome-wide association meta-analysis identifies a novel locus at 17q11.2 associated with sporadic amyotrophic lateral sclerosis. Hum Mol Genet 23(8):2220–2231. https://doi.org/10.1093/hmg/ddt587
Fujisawa T, Homma K, Yamaguchi N, Kadowaki H, Tsuburaya N, Naguro I, Matsuzawa A, Takeda K, Takahashi Y, Goto J, Tsuji S, Nishitoh H, Ichijo H (2012) A novel monoclonal antibody reveals a conformational alteration shared by amyotrophic lateral sclerosis-linked SOD1 mutants. Ann Neurol 72(5):739–749. https://doi.org/10.1002/ana.23668
Gentile G, Perrone B, Morello G, Simone IL, Ando S, Cavallaro S, Conforti FL (2021) Individual oligogenic background in p.D91A-SOD1 amyotrophic lateral sclerosis patients. Genes (Basel) 12(12):1843. https://doi.org/10.3390/genes12121843
Giannoccaro MP, Bartoletti-Stella A, Piras S, Pession A, De Massis P, Oppi F, Stanzani-Maserati M, Pasini E, Baiardi S, Avoni P, Parchi P, Liguori R, Capellari S (2017) Multiple variants in families with amyotrophic lateral sclerosis and frontotemporal dementia related to C9orf72 repeat expansion: further observations on their oligogenic nature. J Neurol 264(7):1426–1433. https://doi.org/10.1007/s00415-017-8540-x
Giau VV, Bagyinszky E, Yang YS, Youn YC, An SSA, Kim SY (2019) Genetic analyses of early-onset Alzheimer’s disease using next generation sequencing. Sci Rep 9(1):8368. https://doi.org/10.1038/s41598-019-44848-2
Goutman SA, Hardiman O, Al-Chalabi A, Chio A, Savelieff MG, Kiernan MC, Feldman EL (2022a) Recent advances in the diagnosis and prognosis of amyotrophic lateral sclerosis. Lancet Neurol 21(5):480–493. https://doi.org/10.1016/S1474-4422(21)00465-8
Goutman SA, Hardiman O, Al-Chalabi A, Chio A, Savelieff MG, Kiernan MC, Feldman EL (2022b) Emerging insights into the complex genetics and pathophysiology of amyotrophic lateral sclerosis. Lancet Neurol 21(5):465–479. https://doi.org/10.1016/S1474-4422(21)00414-2
Hao M, Pu WL, Li Y, Wen SQ, Sun C, Ma YY, Zheng HX, Chen XD, Tan JZ, Zhang GQ, Zhang MH, Xu SH, Wang Y, Li H, Wang JC, Jin L (2021) The HuaBiao project: whole-exome sequencing of 5000 Han Chinese individuals. J Genet Genomics 48(11):1032–1035. https://doi.org/10.1016/j.jgg.2021.07.013
Keller MF, Ferrucci L, Singleton AB, Tienari PJ, Laaksovirta H, Restagno G, Chiò A, Traynor BJ, Nalls MA (2014) Genome-wide analysis of the heritability of amyotrophic lateral sclerosis. JAMA Neurol 71(10):1123–1134. https://doi.org/10.1001/jamaneurol.2014.2914
Keogh MJ, Wei W, Aryaman J, Wilson I, Talbot K, Turner MR, McKenzie CA, Troakes C, Attems J, Smith C, Al Sarraj S, Morris CM, Ansorge O, Pickering-Brown S, Jones N, Ironside JW, Chinnery PF (2018) Oligogenic genetic variation of neurodegenerative disease genes in 980 postmortem human brains. J Neurol Neurosurg Psychiatry 89(8):813–816. https://doi.org/10.1136/jnnp-2017-317234
Kim HJ, Oh KW, Kwon MJ, Oh SI, Park JS, Kim YE, Choi BO, Lee S, Ki CS, Kim SH (2016) Identification of mutations in Korean patients with amyotrophic lateral sclerosis using multigene panel testing. Neurobiol Aging 37:209. https://doi.org/10.1016/j.neurobiolaging.2015.09.012
Kim EJ, Kim YE, Jang JH, Cho EH, Na DL, Seo SW, Jung NY, Jeong JH, Kwon JC, Park KH, Park KW, Lee JH, Roh JH, Kim HJ, Yoon SJ, Choi SH, Jang JW, Ki CS, Kim SH (2018) Analysis of frontotemporal dementia, amyotrophic lateral sclerosis, and other dementia-related genes in 107 Korean patients with frontotemporal dementia. Neurobiol Aging 72:186. https://doi.org/10.1016/j.neurobiolaging.2018.06.031
Kuuluvainen L, Kaivola K, Monkare S, Laaksovirta H, Jokela M, Udd B, Valori M, Pasanen P, Paetau A, Traynor BJ, Stone DJ, Schleutker J, Poyhonen M, Tienari PJ, Myllykangas L (2019) Oligogenic basis of sporadic ALS: the example of SOD1 p.Ala90Val mutation. Neurol Genet 5(3):e335. https://doi.org/10.1212/NXG.0000000000000335
Kwiatkowski TJ, Bosco DA, LeClerc AL, Tamrazian E, Vanderburg CR, Russ C, Davis A, Gilchrist J, Kasarskis EJ, Munsat T, Valdmanis P, Rouleau GA, Hosler BA, Cortelli P, de Jong PJ, Yoshinaga Y, Haines JL, Pericak-Vance MA, Yan J, Ticozzi N, Siddique T, McKenna-Yasek D, Sapp PC, Horvitz HR, Landers JE, Brown RH (2009) Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science 323(5918):1205–1208. https://doi.org/10.1126/science.1166066
Lamp M, Origone P, Geroldi A, Verdiani S, Gotta F, Caponnetto C, Devigili G, Verriello L, Scialo C, Cabona C, Canosa A, Vanni I, Bellone E, Eleopra R, Mandich P (2018) Twenty years of molecular analyses in amyotrophic lateral sclerosis: genetic landscape of Italian patients. Neurobiol Aging 66:179. https://doi.org/10.1016/j.neurobiolaging.2018.01.013
Lattante S, Doronzio PN, Conte A, Marangi G, Martello F, Bisogni G, Meleo E, Colavito D, Del Giudice E, Patanella AK, Bernardo D, Romano A, Zollino M, Sabatelli M (2021) Novel variants and cellular studies on patients’ primary fibroblasts support a role for NEK1 missense variants in ALS pathogenesis. Hum Mol Genet 30(1):65–71. https://doi.org/10.1093/hmg/ddab015
Lattante S, Doronzio PN, Marangi G, Conte A, Bisogni G, Bernardo D, Russo T, Lamberti D, Patrizi S, Apollo FP, Lunetta C, Scarlino S, Pozzi L, Zollino M, Riva N, Sabatelli M (2019) Coexistence of variants in TBK1 and in other ALS-related genes elucidates an oligogenic model of pathogenesis in sporadic ALS. Neurobiol Aging 84:239. https://doi.org/10.1016/j.neurobiolaging.2019.03.010
Liu X, He J, Chen L, Zhang N, Tang L, Liu X, Ma Y, Fan D (2021a) TBK1 variants in Chinese patients with amyotrophic lateral sclerosis. Neurobiol Aging 97:149. https://doi.org/10.1016/j.neurobiolaging.2020.07.028
Liu Z, Yuan Y, Wang M, Ni J, Li W, Huang L, Hu Y, Liu P, Hou X, Hou X, Du J, Weng L, Zhang R, Niu Q, Tang J, Jiang H, Shen L, Tang B, Wang J (2021b) Mutation spectrum of amyotrophic lateral sclerosis in Central South China. Neurobiol Aging 107:181–188. https://doi.org/10.1016/j.neurobiolaging.2021.06.008
McCann EP, Henden L, Fifita JA, Zhang KY, Grima N, Bauer DC, Chan Moi Fat S, Twine NA, Pamphlett R, Kiernan MC, Rowe DB, Williams KL, Blair IP (2020) Evidence for polygenic and oligogenic basis of Australian sporadic amyotrophic lateral sclerosis. J Med Genet. https://doi.org/10.1136/jmedgenet-2020-106866
McGough SF, Incerti D, Lyalina S, Copping R, Narasimhan B, Tibshirani R (2021) Penalized regression for left-truncated and right-censored survival data. Stat Med 40(25):5487–5500. https://doi.org/10.1002/sim.9136
Morgan S, Shatunov A, Sproviero W, Jones AR, Shoai M, Hughes D, Al Khleifat A, Malaspina A, Morrison KE, Shaw PJ, Shaw CE, Sidle K, Orrell RW, Fratta P, Hardy J, Pittman A, Al-Chalabi A (2017) A comprehensive analysis of rare genetic variation in amyotrophic lateral sclerosis in the UK. Brain 140(6):1611–1618. https://doi.org/10.1093/brain/awx082
Mohassel P, Donkervoort S, Lone MA, Nalls M, Gable K, Gupta SD, Foley AR, Hu Y, Saute JAM, Moreira AL, Kok F, Introna A, Logroscino G, Grunseich C, Nickolls AR, Pourshafie N, Neuhaus SB, Saade D, Gangfuss A, Kolbel H, Piccus Z, Le Pichon CE, Fiorillo C, Ly CV, Topf A, Brady L, Specht S, Zidell A, Pedro H, Mittelmann E, Thomas FP, Chao KR, Konersman CG, Cho MT, Brandt T, Straub V, Connolly AM, Schara U, Roos A, Tarnopolsky M, Hoke A, Brown RH, Lee CH, Hornemann T, Dunn TM, Bonnemann CG (2021) Childhood amyotrophic lateral sclerosis caused by excess sphingolipid synthesis. Nat Med 27(7):1197–1204. https://doi.org/10.1038/s41591-021-01346-1
Muller K, Brenner D, Weydt P, Meyer T, Grehl T, Petri S, Grosskreutz J, Schuster J, Volk AE, Borck G, Kubisch C, Klopstock T, Zeller D, Jablonka S, Sendtner M, Klebe S, Knehr A, Gunther K, Weis J, Claeys KG, Schrank B, Sperfeld AD, Hubers A, Otto M, Dorst J, Meitinger T, Strom TM, Andersen PM, Ludolph AC, Weishaupt JH, German ALSnMNDNET (2018) Comprehensive analysis of the mutation spectrum in 301 German ALS families. J Neurol Neurosurg Psychiatry 89(8):817–827. https://doi.org/10.1136/jnnp-2017-317611
Nahm M, Lim SM, Kim YE, Park J, Noh MY, Lee S, Roh JE, Hwang SM, Park CK, Kim YH, Lim G, Lee J, Oh KW, Ki CS, Kim SH (2020) ANXA11 mutations in ALS cause dysregulation of calcium homeostasis and stress granule dynamics. Sci Transl Med 12(566):eaax3993. https://doi.org/10.1126/scitranslmed.aax3993
Narain P, Pandey A, Gupta S, Gomes J, Bhatia R, Vivekanandan P (2018) Targeted next-generation sequencing reveals novel and rare variants in Indian patients with amyotrophic lateral sclerosis. Neurobiol Aging 71:265. https://doi.org/10.1016/j.neurobiolaging.2018.05.012
Narain P, Padhi AK, Dave U, Mishra D, Bhatia R, Vivekanandan P, Gomes J (2019) Identification and characterization of novel and rare susceptible variants in Indian amyotrophic lateral sclerosis patients. Neurogenetics 20(4):197–208. https://doi.org/10.1007/s10048-019-00584-3
Naruse H, Ishiura H, Mitsui J, Takahashi Y, Matsukawa T, Tanaka M, Doi K, Yoshimura J, Morishita S, Goto J, Toda T, Tsuji S (2019) Burden of rare variants in causative genes for amyotrophic lateral sclerosis (ALS) accelerates age at onset of ALS. J Neurol Neurosurg Psychiatry 90(5):537–542. https://doi.org/10.1136/jnnp-2018-318568
Nguyen HP, Van Broeckhoven C, van der Zee J (2018) ALS genes in the genomic era and their implications for FTD. Trends Genet 34(6):404–423. https://doi.org/10.1016/j.tig.2018.03.001
Pang SY, Hsu JS, Teo KC, Li Y, Kung MHW, Cheah KSE, Chan D, Cheung KMC, Li M, Sham PC, Ho SL (2017) Burden of rare variants in ALS genes influences survival in familial and sporadic ALS. Neurobiol Aging 58:238. https://doi.org/10.1016/j.neurobiolaging.2017.06.007
Pottier C, Bieniek KF, Finch N, van de Vorst M, Baker M, Perkersen R, Brown P, Ravenscroft T, van Blitterswijk M, Nicholson AM, DeTure M, Knopman DS, Josephs KA, Parisi JE, Petersen RC, Boylan KB, Boeve BF, Graff-Radford NR, Veltman JA, Gilissen C, Murray ME, Dickson DW, Rademakers R (2015) Whole-genome sequencing reveals important role for TBK1 and OPTN mutations in frontotemporal lobar degeneration without motor neuron disease. Acta Neuropathol 130(1):77–92. https://doi.org/10.1007/s00401-015-1436-x
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, Committee ALQA (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, Donaldson D, Goto J, O’Regan JP, Deng HX et al (1993) Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362(6415):59–62. https://doi.org/10.1038/362059a0
Ross JP, Leblond CS, Laurent SB, Spiegelman D, Dionne-Laporte A, Camu W, Dupre N, Dion PA, Rouleau GA (2020) Oligogenicity, C9orf72 expansion, and variant severity in ALS. Neurogenetics 21(3):227–242. https://doi.org/10.1007/s10048-020-00612-7
Scarlino S, Domi T, Pozzi L, Romano A, Pipitone GB, Falzone YM, Mosca L, Penco S, Lunetta C, Sansone V, Tremolizzo L, Fazio R, Agosta F, Filippi M, Carrera P, Riva N, Quattrini A (2020) Burden of rare variants in ALS and axonal hereditary neuropathy genes influence survival in ALS: insights from a next generation sequencing study of an Italian ALS Cohort. Int J Mol Sci 21(9):3346. https://doi.org/10.3390/ijms21093346
Sghaier I, Kacem I, Ticozzi N, Mrabet S, Paverelli S, Abida Y, Ratti A, Silani V, Gouider R (2022) The oligogenic model of amyotrophic lateral sclerosis; phenotypes of three Tunisian families. Clin Genet 102(6):555–556. https://doi.org/10.1111/cge.14205
Shatunov A, Al-Chalabi A (2021) The genetic architecture of ALS. Neurobiol Dis 147:105156. https://doi.org/10.1016/j.nbd.2020.105156
Shepheard SR, Parker MD, Cooper-Knock J, Verber NS, Tuddenham L, Heath P, Beauchamp N, Place E, Sollars ESA, Turner MR, Malaspina A, Fratta P, Hewamadduma C, Jenkins TM, McDermott CJ, Wang D, Kirby J, Shaw PJ, Project MC, Min Project E (2021) Value of systematic genetic screening of patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 92(5):510–518. https://doi.org/10.1136/jnnp-2020-325014
Siddique T, Deng HX (1996) Genetics of amyotrophic lateral sclerosis. Hum Mol Genet 5:1465–1470. https://doi.org/10.1093/hmg/5.supplement_1.1465
Stevanin G, Azzedine H, Denora P, Boukhris A, Tazir M, Lossos A, Rosa AL, Lerer I, Hamri A, Alegria P, Loureiro J, Tada M, Hannequin D, Anheim M, Goizet C, Gonzalez-Martinez V, Le Ber I, Forlani S, Iwabuchi K, Meiner V, Uyanik G, Erichsen AK, Feki I, Pasquier F, Belarbi S, Cruz VT, Depienne C, Truchetto J, Garrigues G, Tallaksen C, Tranchant C, Nishizawa M, Vale J, Coutinho P, Santorelli FM, Mhiri C, Brice A, Durr A, consortium S (2008) Mutations in SPG11 are frequent in autosomal recessive spastic paraplegia with thin corpus callosum, cognitive decline and lower motor neuron degeneration. Brain 131(3):772–784. https://doi.org/10.1093/brain/awm293
Tang L, Ma Y, Liu XL, Chen L, Fan DS (2019) Better survival in female SOD1-mutant patients with ALS: a study of SOD1-related natural history. Transl Neurodegener 8:2. https://doi.org/10.1186/s40035-018-0142-8
Tripolszki K, Gampawar P, Schmidt H, Nagy ZF, Nagy D, Klivenyi P, Engelhardt JI, Szell M (2019) Comprehensive genetic analysis of a Hungarian amyotrophic lateral sclerosis cohort. Front Genet 10:732. https://doi.org/10.3389/fgene.2019.00732
Tunca C, Seker T, Akcimen F, Coskun C, Bayraktar E, Palvadeau R, Zor S, Kocoglu C, Kartal E, Sen NE, Hamzeiy H, Ozoguz Erimis A, Norman U, Karakahya O, Olgun G, Akgun T, Durmus H, Sahin E, Cakar A, Basar Gursoy E, Babacan Yildiz G, Isak B, Uluc K, Hanagasi H, Bilgic B, Turgut N, Aysal F, Ertas M, Boz C, Kotan D, Idrisoglu H, Soysal A, Uzun Adatepe N, Akalin MA, Koc F, Tan E, Oflazer P, Deymeer F, Tastan O, Cicek AE, Kavak E, Parman Y, Basak AN (2020) Revisiting the complex architecture of ALS in Turkey: expanding genotypes, shared phenotypes, molecular networks, and a public variant database. Hum Mutat 41(8):e7–e45. https://doi.org/10.1002/humu.24055
van Blitterswijk M, van Es MA, Hennekam EA, Dooijes D, van Rheenen W, Medic J, Bourque PR, Schelhaas HJ, van der Kooi AJ, de Visser M, de Bakker PI, Veldink JH, van den Berg LH (2012) Evidence for an oligogenic basis of amyotrophic lateral sclerosis. Hum Mol Genet 21(17):3776–3784. https://doi.org/10.1093/hmg/dds199
van der Zee J, Gijselinck I, Van Mossevelde S, Perrone F, Dillen L, Heeman B, Baumer V, Engelborghs S, De Bleecker J, Baets J, Gelpi E, Rojas-Garcia R, Clarimon J, Lleo A, Diehl-Schmid J, Alexopoulos P, Perneczky R, Synofzik M, Just J, Schols L, Graff C, Thonberg H, Borroni B, Padovani A, Jordanova A, Sarafov S, Tournev I, de Mendonca A, Miltenberger-Miltenyi G, Simoes do Couto F, Ramirez A, Jessen F, Heneka MT, Gomez-Tortosa E, Danek A, Cras P, Vandenberghe R, De Jonghe P, De Deyn PP, Sleegers K, Cruts M, Van Broeckhoven C, Goeman J, Nuytten D, Smets K, Robberecht W, Damme PV, Bleecker J, Santens P, Dermaut B, Versijpt J, Michotte A, Ivanoiu A, Deryck O, Bergmans B, Delbeck J, Bruyland M, Willems C, Salmon E, Pastor P, Ortega-Cubero S, Benussi L, Ghidoni R, Binetti G, Hernandez I, Boada M, Ruiz A, Sorbi S, Nacmias B, Bagnoli S, Sorbi S, Sanchez-Valle R, Llado A, Santana I, Rosario Almeida M, Frisoni GB, Maetzler W, Matej R, Fraidakis MJ, Kovacs GG, Fabrizi GM, Testi S (2017) TBK1 mutation spectrum in an extended european patient cohort with frontotemporal dementia and amyotrophic lateral sclerosis. Hum Mutat 38(3):297–309. https://doi.org/10.1002/humu.23161
Vazquez-Costa JF, Pedrola Vidal L, Moreau-Le Lan S, Teresi-Copovi I, Frasquet M, Chumillas MJ, Sevilla T (2019) Facial onset sensory and motor neuronopathy: a motor neuron disease with an oligogenic origin? Amyotroph Lateral Scler Frontotemporal Degener 20(3–4):172–175. https://doi.org/10.1080/21678421.2019.1582671
Yang L, Cheng Y, Jia X, Liu X, Li X, Zhang K, Shen D, Liu M, Guan Y, Liu Q, Cui L, Li X (2021) Four novel optineurin mutations in patients with sporadic amyotrophic lateral sclerosis in Mainland China. Neurobiol Aging 97:149. https://doi.org/10.1016/j.neurobiolaging.2020.08.002
Yilmaz R, Weishaupt K, Valkadinov I, Knehr A, Brenner D, Weishaupt JH (2022) Quadruple genetic variants in a sporadic ALS patient. Mol Genet Genomic Med 10(7):e1953. https://doi.org/10.1002/mgg3.1953
Zhang H, Cai W, Chen S, Liang J, Wang Z, Ren Y, Liu W, Zhang X, Sun Z, Huang X (2018a) Screening for possible oligogenic pathogenesis in Chinese sporadic ALS patients. Amyotroph Lateral Scler Frontotemporal Degener 19(5–6):419–425. https://doi.org/10.1080/21678421.2018.1432659
Zhang H, Liang JL, Chen SY, Wang ZJ, Yang F, Cui F, Ren YT, Liu WX, Sun ZS, Huang XS (2018b) Screening of the SETX gene in sporadic amyotrophic lateral sclerosis patients of Chinese origin. Zhonghua Yi Xue Za Zhi 98(33):2628–2631. https://doi.org/10.3760/cma.j.issn.0376-2491.2018.33.003
Zou ZY, Li XG, Liu MS, Cui LY (2013) Screening for C9orf72 repeat expansions in Chinese amyotrophic lateral sclerosis patients. Neurobiol Aging 34(6):1710. https://doi.org/10.1016/j.neurobiolaging.2012.11.018
Acknowledgements
The authors would like to give their gratitude to all the study participants and their families for their dedication to ALS research. The authors would like to thank HuaBiao Project: Whole-Exome Database of Han Chinese, for we use the database as control.
Funding
This work was supported by 2020 Central Transfer Payment Medical Siege Institutions Capacity Building Project (National and Provincial Multi-scientific Cooperation Diagnosis and Treatment of Major Diseases Capacity Building Project); Shanghai Fudan University Education Development Foundation and State Key Laboratory of Genetic Engineering, Human Phenome Institute, Zhangjiang Fudan International Innovation Center, Fudan University; Shanghai Municipal Science and Technology Major Project 2017HZDZX01.
Author information
Authors and Affiliations
Contributions
Included conception and study design (XC and JW), data collection or acquisition (SD, XY, KW, WY, JL, YZ and XL), statistical analysis (SD, XY, KW and YW), interpretation of results (SD, XY, KW, JW and XC), drafting the manuscript work (SD, XY, JW and XC) and approval of final version to be published and agreement to be accountable for the integrity and accuracy of all aspects of the work (all the authors).
Corresponding authors
Ethics declarations
Conflict of Interest
No potential conflict of interest was reported by the author(s).
Ethical Approval and Consent to Participate
The studies involving human participants were reviewed and approved by the Ethics Committee of Huashan Hospital, Fudan University. The patients/participants provided their written informed consent to participate in this study.
Consent for Publication
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, S., Yin, X., Wang, K. et al. Presence of Rare Variants is Associated with Poorer Survival in Chinese Patients with Amyotrophic Lateral Sclerosis. Phenomics 3, 167–181 (2023). https://doi.org/10.1007/s43657-022-00093-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43657-022-00093-8