Abstract
Background
This study aims to systematically compare the efficacy of two distinct approaches that is limb occlusion pressure (LOP) and systolic blood pressure (SBP) in determining the optimal tourniquet pressure for primary total knee arthroplasty. The overarching goal is to identify the method that yields superior outcomes in minimizing post-operative thigh pain while simultaneously reducing complications in our patient population.
Methods
311 patients scheduled for primary total knee replacement (TKR) were randomized in two groups. Group A (LOP) had 154 patients and group B had 157 patients. In group A, LOP was determined for all patients. After adding the safety margin, the tourniquet pressure was determined which was kept during the procedure. By adding 150 mm Hg to SBP in group B, the tourniquet inflation pressure was ascertained. Postoperatively, thigh pain was evaluated from day 1 to day 3 and at 6 weeks.
Results
The average tourniquet pressure in group A patients having thigh circumference between 40 and 50 cm was 223.8 mm + − 19.8 mm Hg and in group B it was 262.1 + − 15.9 mm Hg (P < .01). Patients having thigh circumference between 51 and 60 cm had average tourniquet pressure of 240.07 + − 20.1 mm Hg in group A and 264.5 + − 17.4 mm Hg in group B (P < .01). The average tourniquet pressure for patients with thigh circumference more than 60 cm was 296 + /15.3 mm Hg in group A and 267.3 + /19.2 mm Hg in group B (P < 0.01).
Conclusion
Tourniquet pressure determination based on the limb occlusion pressure (LOP) method provide less postoperative thigh pain and better range of motion.
Graphical Abstract
Optimizing Tourniquet Pressure in Primary Total Knee Replacement: Limb Occlusion Pressure vs Systolic blood pressure method to minimize thigh pain.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is one of the most often done orthopaedic procedures that seeks to reduce pain, rectify deformity, and enhance quality of life in patients with degenerative joint disease [1]. In the initial post-operative phase following TKA, development of thigh pain post tourniquet administration is still a prevalent complaint [2]. The orthopaedic literature has not yet determined the ideal method of tourniquet inflation pressure determination and its optimal duration of application. [1]. According to the current consensus, the tourniquet should be applied with a minimum possible pressure and time which provides a bloodless surgical field [2] yet, a standardized approach for determining the optimal inflation pressure remains elusive. For establishing the tourniquet inflation pressure in practice, orthopaedic surgeons consider several variables including age, body mass index (BMI), extremity girth and systolic blood pressure (SBP) [1]. When doing TKA, some surgeons arbitrary choose 280/300 mm Hg or SBP + (100–150) mm Hg as the tourniquet inflation pressure [3]. The limb occlusion pressure (LOP) represents the minimal tourniquet pressure necessary to halt arterial blood flow beyond the cuff. Its determination involves either manual or automated methods, achieved through gradual cuff inflation until pulse cessation, facilitated by diagnostic tools like pulse oximeters or Doppler flowmeters. In addition to the thigh pain that has been documented in the literature, other side effects of tourniquet use in TKA include skin ecchymosis, blebs, quadriceps weakness, decreased knee ROM, infection and venous thromboembolism (VTE) [4]. Most of these issues are pressure and time related and they can jeopardize TKA patients’ ability to recover and achieve their goals [5]. Tailoring tourniquet pressure according to limb occlusion pressure (LOP) enables a personalized approach for each patient, proving effective in optimizing cuff pressures and contributing to enhanced tourniquet management. In many studies [6, 7], the total knee arthroplasty performed without the use of a tourniquet and has produced results that are comparable to those achieved with the tourniquet. Although the use of a tourniquet during TKA is still debatable and has mixed effects, orthopaedic surgeons routinely employ it in their practices [8]. Furthermore, extra high-quality research is required, particularly among Indian populations to find out the ideal method of tourniquet pressure determination.
The primary aim of this study was to determine whether the limb occlusion pressure (LOP) method for determining optimal tourniquet pressure reduces the cuff pressure during TKA and if this results in less post-operative thigh pain when compared to the SBP method. The secondary aim was to determine whether these two techniques of calculating tourniquet pressure differed in terms of knee range of motion, the quality of the bloodless field, blood loss and wound complications.
Materials and Methods
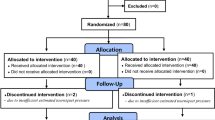
From November 2021 to June 2022, this prospective randomized controlled trial was conducted. All patients scheduled for primary TKA with the pneumatic tourniquet under spinal anaesthesia/combined spinal epidural anaesthesia gave their informed written consent after our institutional ethical board granted its clearance. In this study, patients who received TKA had degenerative knee conditions caused to primary osteoarthritis and rheumatoid arthritis were included. Patients who had extra articular deformities requiring specialized methods and implants, post-traumatic arthritis, a history of bleeding disorders, evidence of DVT/VTE and conditions that made tourniquet use contraindicated (peripheral vascular disease, peripheral neuropathy) were excluded from this study. Patients with excessive intraoperative blood pressure changes that resulted in bleeding in the surgical field and patients who were lost to follow-up were also excluded. The age, gender, BMI, preoperative haemoglobin level (Hb) and thigh circumference (15 cm from the superior pole of the patella with the knee extended) measured using the tape method were recorded. By computer-based randomization, patients were split into two groups. After skin drapes being set up, the senior surgeon lifted the lower limb at 45 degrees and maintained for 30 s, followed by inflation of the pneumatic tourniquet. No exsanguination done for any patient. The tourniquet inflation pressure in group A (LOP) was calculated by estimating the limb occlusion pressure. To measure LOP, a tourniquet cuff with its distal edge 15 cm from the proximal pole of the patella was wrapped around the thigh. The cuff was slowly inflated, and distal pulses (dorsalis pedis artery) were palpated. The pressure at which distal pulses ceased to exist was noted. The tourniquet cuff was inflated to the prescribed pressure in accordance with the Association of Perioperative Registered Nurses’ recommendations, which state that for adult patients, a safety margin of 40 mm Hg should be used if the LOP is less than 130 mm Hg, 60 mm Hg should be used for LOPs between 131 mm Hg and 190 mm Hg and 80 mm Hg should be used for LOPs above 190 mm Hg. In group B, the tourniquet pressure was based on SBP just before giving the skin incision. In this group SBP was added with 150 mm Hg, making our tourniquet cuff inflation pressure. All patients received tablet Pregabalin 75 mg and tablet Acetaminophen 650 mg stat dose a night before surgery. A bolus dose of preoperative antibiotic, Cefuroxime 1.5 g was given to all patients 1 h before tourniquet inflation. One layer of cotton padding was then stretched around the proximal thigh, 15 cm proximal to the superior pole of patella following SA/CSEA. For all patients with thighs smaller than 60 cm in circumference, a straight tourniquet measuring 15 cm wide by 61 cm long was employed. For patients having thigh circumference more than 60 cm, the tourniquet of length 81 cm and width 15 cm was used. The tourniquet cuff, source and tubing were checked in all patients before application. We used VBM Medizintechnik GmbH digital tourniquet system in all patients. After painting and draping, tourniquet was inflated based on LOP or SBP method depending upon the allotted group. The same surgical technique and implant (PFC sigma, Depuy) were used throughout all surgeries performed by a single skilled surgeon. After cement polymerization, the tourniquet was released, and the duration of the tourniquet was recorded. Haemostasis was established and the wound was then closed with an extraarticular drain. The Surgical field quality was rated by the operating surgeon as either blood mixed or clear after the procedure. In the recovery room, all patients received CPM up to 60 degrees which was raised to 90 degrees on day 1. The same postoperative pain relief treatment was given to all patients. The adductor canal block was given to all patients just after completion of surgery. In the postoperative ward, patient was given injection acetaminophen 6 hourly for first 24 h. Tablet Paracetamol 650 mg thrice a day and Aceclofenac 100 mg twice daily was given to all patients during the hospital stay till discharge. Patients were mobilized full weight bearing walk with walker along with knee ROM and quadriceps exercise, after 24 h of surgery. All patients received tablet Aspirin 150 mg for DVT prevention [26]. Mechanical DVT prophylaxis was given to both groups in the form of intermittent pneumatic compression device (IPCD). Thigh pain was evaluated with the rest pain scale of the hospital for special surgery knee score (no pain, mild pain, moderate pain, severe pain). The pain scale was applied on day 1 to day 3 after surgery. Knee ROM, postoperative haemoglobin level, wound complication, need of blood transfusion were evaluated in all patients. If the postoperative period went uneventful, patients were discharged from the hospital after 3 days. Knee ROM and thigh pain were again evaluated at the initial follow-up appointment at 6 weeks.
Statistical Analysis
Categorical variables were presented in numbers and percentage and continuous variable were presented as mean ± SD. Quantitative variables were compared using Student’s t test and chi square test was used for categorical data. A P value of < 0.05 was considered statistically significant. The data were entered in MS EXCEL spreadsheet, and the analysis was done using Statistical Package for Social Science (SPSS) version 25.0.
Results
Demographics
315 patients in all were enrolled in the study. Owing to intraoperative breakthrough bleeding and tourniquet failure, four patients had to be excluded. Therefore, using computer-based randomization, the remaining 311 patients were split into two groups, with 154 patients in group A and 157 patients in group B. The baseline demographic and clinical characteristics were not statistically different between the two groups, except for body mass index (BMI) (P = 0.01) and SBP (P = 0.0001) which was an incidental finding [Table 1]. Both groups’ average ages were 62.3 + − 5.04 years and 63.4 + − 8.02 years, respectively (P = 0.24). 22 patients (14.2%) were males, and 132 patients (85.7%) were females out of 154 patients in group A. Out of the 157 patients in group B, 35 patients (22.2%) were men, and 122 patients (77.7%) were women. The average BMI in group A was 30.5 + − 5.7 kg/m2 and in group B was 29.08 + − 5.3 kg/m2 (P = 0.01). The mean thigh circumference was 52.1 + − 7.03 cm in group A and 51.3 + − 6.7 cm in group B (P = 0.27). Average SBP in group A was 107.4 + − 13.2 mm Hg and in group B was 118 + − 20.0 mm Hg (P = 0.0001). The mean duration of tourniquet application was 45.1 + − 8.5 min in group A and 46.3 + − 8.1 min in group B (P = 0.19).
Primary Outcome
Patients having thigh circumference of 40–50 cm had mean tourniquet pressure of 223.8 + − 19.8 mm Hg in group A and 262.1 + − 15.9 mm Hg in group B (P = 0.0001) [Table 2]. Talking about thigh pain, 76.4% patients in group A of the above-mentioned thigh girth had “no to mild” intensity of pain while 51.6% patients in group B had “moderate to severe” grade of thigh pain. Likewise, the patients having thigh circumference of 51–60 cm had mean tourniquet pressure of 240.07 + − 20.1 mm Hg in group A and 264.5 + − 17.4 mm Hg in group B (P = 0.0001). In these patients, 72.05% had “no to mild” grade pain in group A and 53.3% had “mild to moderate” grade pain in group B. Similarly, Patients having thigh circumference > 60 cm had average tourniquet pressure of 296 + − 15.3 mm Hg in group A and 267.3 + − 19.2 mm Hg in group B (P = 0.0001). Their intensity of pain was “no to mild” grade in both group A (75%) and group B (62.5%). The above findings implies that the mean tourniquet pressure was less in group A patients leading to negligible thigh pain. However, the above statement was found contradictory in patients having thigh girth > 60 cm, still the intensity of pain did not change suggesting that LOP method of tourniquet pressure determination is more reliable.
Secondary Outcome
The mean knee flexion on day 3 post TKA was 82.3 degree in group A and 79.4 degree in group B (P = 0.02) [Table 3]. On day 3 following TKA, the average extensor lag was 18.0 degree in group A and 20.1 degree in group B (P = 0.0006). At six weeks, the average knee flexion in groups A and B patients was 104.9 and 104.7 degrees (P = 0.34) while, the average extensor lag was 1.07 and 2.01 degrees respectively (P = 0.21). The above findings indicate that LOP method cause less damage to the knee extensor mechanism leading to better ROM in these patients in the immediate post-operative period but at 6 weeks, the above disparity was not noticeable. The mean preoperative haemoglobin (Hb) levels in groups A and B were 11.6 g/dl and 11.9 g/dl respectively (p = 0.06). The average postoperative Hb level was 10.4 g/dl in group A and 10.5 g/dl in group B (P = 0.5) suggesting no difference in blood loss in both tourniquet pressure determination methods during the procedure. Following TKA, blood transfusions were needed for 10 patients in group A and 11 patients in group B (P = 0.8). Four patients in group A and seven patients in group B (P = 0.3) had thigh ecchymosis. 5 patients in group A and 12 patients in group B (P = 0.08) had unclear (bloody) surgical fields. Five patients in group A and six in group B (P = 0.7) required elevation in the pre-determined tourniquet pressure which was ascertained before commencing the surgery.
Discussion
The use of tourniquet during elective TKA is still debated in Orthopaedic literature [8] yet it is commonly used to provide bloodless operative field, decrease surgical error, reduced operative time and better visualization of anatomic structure [2]. Some authors have demonstrated that its use in limb procedures has had no appreciable negative effects [9, 10]. Regarding the impact of a tourniquet on perioperative blood loss, post-TKA functional result, and postoperative pain, there are still differences in opinion [8]. Tourniquet use, however, has been linked to both local and systemic issues [11]. Clinical and experimental research have demonstrated a clear relationship [12,13,14] between the amount and duration of tourniquet pressure and the severity of neuromuscular damage following TKA. A similar correlation exists for the total duration of the tourniquet application [5]. As a goal, the tourniquet should be applied at the lowest pressure and least time possible [15]. Although, the modern tourniquet and advances of tourniquet technology has resulted in the use of lower tourniquet inflation pressure yet there is still lack of standard consensus regarding minimal effective tourniquet pressure [16]. Most of the surgeons routinely apply fixed tourniquet pressure of 250–300 mm Hg or add fixed amount of pressure above SBP (100–150 mm Hg) in elective TKA and consider these pressures as safe neglecting the adverse effect associated with these high tourniquet pressure [17]. In our study, we have compared LOP method of tourniquet pressure determination with (SBP + 150 mm Hg) method. The most important factors affecting tourniquet pressure include thigh circumference and SBP of the patient [18]. We found reduced cuff pressure in LOP method of tourniquet pressure determination having direct correlation with thigh circumference. Olivecrona et al. [19] in their study demonstrated that LOP method reduces tourniquet cuff pressure but no difference was found in the postoperative pain between LOP and their control group. However, this can be due to low cuff pressure (mean 252 mm Hg) in their control group. In our study, the severity of thigh pain was less in LOP group when compared with (SBP + 150 mm Hg) group. This could be due to less tourniquet inflation pressure in the LOP group. Excessive tourniquet pressure causes axonal compression syndrome leading to delayed recovery of nerves and muscles under the tourniquet cuff [20]. Other authors believe that postoperative pain could be related to neuromuscular damage beneath the tourniquet along with compromised blood supply to the nerve fibres, muscles and skin [21]. Smaller thigh circumference increases postoperative thigh pain risk [2]. In our study, this was more evident in group B patients. Hong Yi et al. [2] in their study believe that applying excessive pressure causes local tissue compression which includes axial stretching force and local compressive force. Patients having smaller thigh circumference have less soft tissue covering and thus less neuromuscular protection from compression. Our study supported this inference. Worland et al. [5] compared high tourniquet pressure (350 mm Hg) with low tourniquet pressure (mean- 230 mm Hg). They found more thigh pain in high pressure group on day 1–3 but no difference was found at 6 weeks. In our study also, we got similar results. Thigh pain was more in group B patients initially but at 6 weeks, there was no difference. Bruner [22] noted that tourniquet time close to 60 min, some individuals showed significant adverse effect. Sherman et al. [23] have shown that risk of complication increases with tourniquet time longer than 40–60 min. However, we did not find any significant correlation between tourniquet time and thigh pain. This might be attributed to the fact that the mean tourniquet time was short in our study in both the groups.
There are conflicting reports regarding the use of tourniquet and postoperative knee ROM [24]. Pinsornsak P et al. [1] in their study showed no direct correlation of different tourniquet pressure and knee ROM. Our study showed that different tourniquet pressure affects knee ROM in the immediate postoperative period but not at 6 weeks. This might be because of thigh pain limiting quadriceps function leading to decreased ROM.
Our study found no difference in the preoperative and postoperative haemoglobin level between the two groups. We also found no difference in the need of blood transfusion between two groups. This was consistent with the study of Kim et al. [3]. There was no wound complication and infection in our study in both the groups which was contradictory from the study done by Clarke et al. [25] and Olivecrona et al. [19]. we only found thigh ecchymosis in few patients which was insignificant in both the groups. This might be attributed to the commencement of blood thinner from first postoperative day (POD1). We found statistically insignificant difference in the picture of surgical field between both the groups. Patients in group B, especially having thigh girth > 60 cm, had surgical field full of blood. This might be due to less tourniquet inflation pressure determined from SBP causing inadequate thigh compression. We found no difference regarding the need of elevation of tourniquet pressure in both the groups in our study. This might be due to addition of safety margin in group A and 150 mm Hg to SBP in group B considering hemodynamic fluctuation during surgery.
The two important variables that leads to failure in haemostasis using lower tourniquet pressure are thigh circumference and vessel compliance [5]. Worland et al. [5] found that in patients with adequate vascular function and thigh circumference between 46 and 76 cm, it is possible to get bloodless operative field with a tourniquet pressure of 100 mm Hg plus SBP. In our study, we found breakthrough bleeding and bloody surgical field when tourniquet pressure was determined by adding 100 mm Hg to the SBP. Therefore, we added 150 mm Hg to SBP in all patients of our study. Our study showed that SBP + 150 mm Hg gives optimum tourniquet pressure in patients having thigh circumference up-to 60 cm but with moderate to severe thigh pain. We believe that in patients with larger thigh girth, it is better to determine tourniquet pressure by Limb Occlusion Pressure (LOP) method.
The strength of this study is that it was a randomized controlled trial of a large number of study population with few exclusion criteria. Our study has certain limitations. First, pain is a subjective complaint and there are chances of intra-observer error even when the thigh pain is measured by a single technician. Second, due to the proximity of thigh pain and surgical site pain, it was difficult to differentiate between the two and they may have caused overestimation of thigh pain. Third, the evaluation of bloodless surgical field is subjective. Finally, our study has a smaller number of study population having thigh circumference > 60 cm. Therefore, further research is required to investigate the most effective method of tourniquet pressure determination especially in population having thigh circumference > 60 cm.
Conclusion
In primary TKR, limb occlusion pressure (LOP) method of tourniquet pressure determination provide optimal pressure with less post-operative thigh pain when compared with systolic blood pressure (SBP) method with better knee range of motion (ROM). The procedure time, wound complications, blood loss, and requirement for blood transfusion were unaffected by the LOP or SBP methods. Hence, we recommend limb occlusion pressure as a tourniquet pressure determination method for primary total knee arthroplasty.
Abbreviations
- TKA:
-
Total knee arthroplasty
- LOP:
-
Limb occlusion pressure
- SBP:
-
Systolic blood pressure
- ROM:
-
Range of motion
References
Pinsornsak, P., Pinitchanon, P., & Boontanapibul, K. (2021). Effect of Different tourniquet pressure on postoperative pain and complications after total knee arthroplasty: A prospective. Randomized Controlled Trial. J Arthroplasty., 36(5), 1638–1644.
Hong, P. Y., Chen, W. M., Wu, P. K., Chen, C. F., Su, Y. P., Lee, O. K. S., Chiang, C. C., Huang, C. K., Liu, C. L., & Chen, T. H. (2013). Thigh pain after total knee arthroplasty: Analysis of risk factors. Formosan Journal of Musculoskeletal Disorders, 4(1), 11–14.
Kim, T. K., Bamne, A. B., Sim, J. A., Park, J. H., & Na, Y. G. (2019). Is lower tourniquet pressure during total knee arthroplasty effective? A prospective randomized controlled trial. BMC Musculoskeletal Disorders, 20(1), 275.
Dennis, D. A., Kittelson, A. J., Yang, C. C., Miner, T. M., Kim, R. H., & Stevens-Lapsley, J. E. (2016). Does tourniquet use in TKA affect recovery of lower extremity strength and function? A randomized trial. Clinical Orthopaedics and Related Research, 474(1), 69–77.
Worland, R. L., Arredondo, J., Angles, F., Lopez-Jimenez, F., & Jessup, D. E. (1997). Thigh pain following tourniquet application in simultaneous bilateral total knee replacement arthroplasty. Journal of Arthroplasty, 12(8), 848–852.
Tai, T. W., Lin, C. J., Jou, I. M., Chang, C. W., Lai, K. A., & Yang, C. Y. (2011). Tourniquet use in total knee arthroplasty: A meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 19(7), 1121–1130.
Girard, N., Zhang, W., Li, N., Chen, S., Tan, Y., Al-Aidaros, M., & Chen, L. (2014). The effects of a tourniquet used in total knee arthroplasty: A meta-analysis. Journal of Orthopaedic Surgery and Research, 9(1), 13.
Goel, R., Rondon, A. J., Sydnor, K., Blevins, K., O’Malley, M., Purtill, J. J., & Austin, M. S. (2019). Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty: A prospective, double-blinded, randomized controlled trial. Journal of Bone and Joint Surgery. American Volume, 101(20), 1821–1828.
Kirkley, A., Rampersaud, R., Griffin, S., Amendola, A., Litchfield, R., & Fowler, P. (2000). Tourniquet versus no tourniquet use in routine knee arthroscopy: A prospective, double-blind, randomized clinical trial. Arthroscopy, 16(2), 121–126.
Arciero, R. A., Scoville, C. R., Hayda, R. A., & Snyder, R. J. (1996). The effect of tourniquet use in anterior cruciate ligament reconstruction. A prospective, randomized study. American Journal of Sports Medicine, 24, 758–764.
Graf, B., Jensen, K., Orwin, J., Duck, H., Hagen, P., & Keene, J. (1996). The effect of tourniquet use on postoperative strength recovery after arthroscopic meniscectomy. Orthopedics, 19(6), 497–500.
Patterson, S., & Klenerman, L. (1979). The effect of pneumatic tourniquets on the ultrastructure of skeletal muscle. Journal of Bone and Joint Surgery. British Volume, 61(2), 178–183.
Netaji, J., Banerjee, S., Garg, P. K., & Elhence, A. (2021). Reappraisal of limited duration tourniquet in total knee arthroplasty: A double-blinded RCT. Indian Journal of Orthopaedics., 55(5), 1186–1194. https://doi.org/10.1007/s43465-021-00506-2
Heppenstall, R. B., Scott, R., Sapega, A., et al. (1986). A comparative study of the tolerance of skeletal muscle to ischemia. The Journal of Bone and Joint Surgery, 68(6), 820–828.
Gersoff, W. K., Ruwe, P., Jokl, P., & Panjabi, M. (1989). The effect of tourniquet pressure on muscle function. American Journal of Sports Medicine, 17(1), 123–127.
Tuncali, B., Boya, H., Kayhan, Z., & Arac, S. (2018). Tourniquet pressure settings based on limb occlusion pressure determination or arterial occlusion pressure estimation in total knee arthroplasty? A prospective, randomized, double blind trial. Acta Orthopaedica et Traumatologica Turcica, 52(4), 256–260.
Tejwani, N. C., Immerman, I., Achan, P., Egol, K. A., & McLaurin, T. (2006). Tourniquet cuff pressure: The gulf between science and practice. Journal of Trauma, 61(6), 1415–1418.
Shaw, J. A., & Murray, D. G. (1982). The relationship between tourniquet pressure and underlying soft-tissue pressure in the thigh. Journal of Bone and Joint Surgery. American Volume, 64(8), 1148–1152.
Olivecrona, C., Ponzer, S., Hamberg, P., & Blomfeldt, R. (2012). Lower tourniquet cuff pressure reduces postoperative wound complications after total knee arthroplasty: A randomized controlled study of 164 patients. J Bone Joint SurgAm., 94(24), 2216–2221.
Saunders, K. C., Louis, D. L., Weingarden, S. I., & Waylonis, G. W. (1979). Effect of tourniquet time on postoperative quadriceps function. Clinical Orthopaedics, 143, 194–199.
Pedowitz, R. A., Gershuni, D. H., Schmidt, A. H., Fridén, J., Rydevik, B. L., & Hargens, A. R. (1991). Muscle injury induced beneath and distal to a pneumatic tourniquet: A quantitative animal study of effects of tourniquet pressure and duration. J Hand Surg Am., 16(4), 610–621.
Bruner, J. M. (1951). Safety factors in the use of the pneumatic tourniquet for hemostasis in surgery of the hand. J Bone Joint Surg Am., 33(A(1)), 221–4.
Sherman, O. H., Fox, J. M., Snyder, S. J., et al. (1986). Arthroscopy: “no-problem surgery.” The Journal of Bone and Joint Surgery, 68(2), 256–265.
Alexandersson, M., Wang, E. Y., & Eriksson, S. (2019). A small difference in recovery between total knee arthroplasty with and without tourniquet use the first 3 months after surgery: a randomized controlled study. Knee Surgery, Sports Traumatology, Arthroscopy, 27(4), 1035–1042.
Clarke, M. T., Longstaff, L., Edwards, D., & Rushton, N. (2001). Tourniquet-induced wound hypoxia after total knee replacement. Journal of Bone and Joint Surgery. British Volume, 83(1), 40–44.
Merkow, D. B., Tang, A., Iorio, R., Slover, J. D., Bosco, J. A., & Schwarzkopf, R. (2021). Low dose aspirin is effective in preventing venous thromboembolism in patients undergoing primary total knee arthroplasty. Journal of Orthopaedics, 12(24), 26–28.
Funding
The research for this paper was not supported by any grants or funds from outside sources for the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and /or national research committee and with the 1964 HeIsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Natesan, R., Istiyak, M., Dhanasekara Raja, P. et al. Optimizing Tourniquet Pressure in Primary Total Knee Arthroplasty: Limb Occlusion Pressure vs Systolic Blood Pressure Method: A Randomised Controlled Study. JOIO 58, 971–978 (2024). https://doi.org/10.1007/s43465-024-01177-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01177-5