Abstract
Background
Infection around the ankle joint after fracture fixation, or septic arthritis with active discharging sinuses is often challenging to manage with conventional procedures of arthrodesis. The Ilizarov method of arthrodesis gives a better alternative for salvage in such cases.
Methods
This was a retrospective study including 20 patients who were subjected to tibiotalar arthrodesis with Ilizarov method. The major pathologies included internal fixation of ankle fractures complicated by infection, posttraumatic infected ankle arthritis, and osteomyelitis. The patients were evaluated on the basis of Association for the Study and Application of the Method of Ilizarov (ASAMI) criteria. The aim of the surgery was to achieve plantigrade, stable, and painless foot with no signs of infection.
Results
A total of 20 patients were operated and reviewed at our institute. The study comprised of 15 male and 5 female patients with a mean age of 43.9 years (range 33–55 years). Out of 20 patients, 4 patients had complications of pin-tract infection and one had wire breakage of the forefoot ring. According to the ASAMI criteria, 17 patients had excellent bone scores and 18 patients had good functional scores. Union was achieved in all patients with resolution of infection and the mean limb length discrepancy was 1.92 cm (range 1–2.5 cm).
Conclusions
The Ilizarov fixator for ankle arthrodesis provides an excellent way for strong bone fusion, infection eradication, early weight-bearing, and the added benefits of compression at the arthrodesis site post-operatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle fractures with infection following fracture fixation are difficult to manage due to the superficial nature of the joint, poor soft-tissue cover around the ankle joint, and skin defects following debridement. Additionally, subluxation of the joint after implant removal further complicates the treatment in patients with previous fixation of ankle fractures. Patients with advanced age and associated comorbidities also have wound healing complications.
Ankle arthrodesis has been recognized as one of the standard procedures for salvaging ankle joints in advanced cases of degeneration with associated comorbidities [1,2,3,4,5]. Conventional methods of internal fixation for ankle arthrodesis are often difficult to use in the presence of infection and the Ilizarov method serves as a good modality of treatment [6].
Tibiotalar arthrodesis serves as one of the most commonly performed arthrodesis around the ankle joint [7,8,9,10]. Though we have made significant advances in the form of arthroscopy, arthroplasty, and arthrodiastasis, ankle arthrodesis still acts as the gold standard for end-stage disease [11]. There are various indications for arthrodesis, including post-traumatic degeneration, infection, rheumatoid arthritis, tumors, and neuromuscular conditions [11, 12].
Ankle joint presents with numerous difficulties as the amount of cases with joint destruction after complicated fractures are on the rise [10, 13, 14]. Incidence of chronic infections, bone defects, limb length discrepancy, soft-tissue loss, and joint abnormalities are quite challenging and difficult to treat [13, 14]. Amputation may present as the last resort for patients with failed arthrodesis, and therefore, fusion procedures should be thoroughly evaluated to prevent inadequate results.
The Ilizarov device is a flexible external fixator that permits dynamic and multidirectional stresses to be applied. The ability to alter the alignment of the hindfoot and forefoot after the surgery by repositioning the frame as required is a distinct benefit of the Ilizarov technique, allowing for the rectification of intraoperative errors or early postoperative loss of position. These advantages significantly improve the outcome of the surgery and are quite helpful in the correction of malalignment, providing an improved level of activity, and pain management.
The aim of this study was to evaluate the outcomes of arthrodesis of the tibiotalar joint using a relatively simple Ilizarov ring fixator frame.
Materials and Methods
Twenty ankle (tibiotalar) arthrodesis performed at our institute between May 2017 and May 2019, and followed up on until October 2021 utilizing the Ilizarov external fixator were evaluated retrospectively. The study comprised 15 men and 5 women ranging in age from 33 to 55 years at the time of arthrodesis. Fourteen individuals had their right ankle arthrodesed, whereas 6 had their left ankle arthrodesed (Table 1).
All patients had a history of trauma. The causal pathology in most of the patients was post-traumatic infection with active discharging sinus. Eighteen patients had a history of open reduction and internal fixation for bimalleolar ankle fractures and osteoarthritis, and the remaining two patients took conservative treatment for bimalleolar fractures. Most of the patients were previously operated on an average of 1.3 (range 0–4) times. The previous surgical procedures were in the form of external fixation, open reduction and internal fixation with implant in situ, bone grafting, revision surgery for wound management, implant removal, and soft-tissue defect. The primary aim of Ilizarov frame arthrodesis was to obtain a painless and solid plantigrade foot and to eradicate existing infection.
Operative Procedure
The medial and lateral approaches were used to open the ankle joint. In instances where prior incision scars and discharging sinuses were evident, the incision was modified. To minimize wound problems, full-thickness subperiosteal skin flaps were raised. If implants were present, they were removed. Debridement was performed and joint synovium was excised.
The distal 5 cm of the fibula was removed, exposing the articular surface of the ankle joint. The medial malleolus was removed at the tibial plafond level. The articular surface of the tibia was cut perpendicular to the long axis of the tibia with an oscillating saw. Talar dome articular cartilage was sliced parallel to the tibial cut. In neutral flexion and 10°–15° of external rotation, the cancellous surfaces of the tibia and talus were opposed to each other with no varus or valgus angulation. The opposing ends were secured in position and two 3 mm K-wires were passed across the ankle joint.
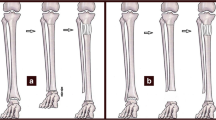
A simple preconstructed Ilizarov frame design with two full and one 5/8th ring connected with 4 rods between each other was slid over the leg (Fig. 1). The desired position of the frame over leg was maintained by keeping folded towels between leg and ring. 2 full rings were fixed to the tibia perpendicular to its axis using Schanz screws and wires. The level of the 5/8th ring was adjusted at the level of the calcaneum. Two crossing olive wires were passed in the calcaneum opposing each other and were tensioned up to 60 kg. A Schanz screw was passed using a one-hole Rancho cube from the posterior aspect of the heel into the calcaneum pointing towards the cuboid under IITV (Image intensifying TV system) guidance. One drop wire was passed through the talus and connected to the calcaneal ring using male posts.
One 5/8th ring was put in the forefoot at the level of the metatarsal neck using two olive wires. One wire from the inferomedial aspect of the 1st metatarsal neck and the another olive wire from the posterolateral aspect of the 5th metatarsal neck incorporating the 3rd and 4th metatarsal.
The forefoot ring was connected to the calcaneal ring using simple hinges and coupled washers with two rods over medial and lateral aspect. The forefoot ring was also connected to the distal tibial ring using hinges and coupled washers with one connecting rod (Figs. 2, 3, 4).
After all the connections were put in, the K-wires which were used to hold the arthrodesis in position were removed.
Corticotomy for lengthening was not done in any patient undergoing surgery as all of them were counseled preoperatively about shortening up to 1 inch. The goals of the surgery were to get a plantigrade, stable, and painless foot without any infection.
Postoperative Protocol
All patients are permitted to walk with a walker and modified footwear with weight-bearing as tolerated. The patient and a relative were both educated on pin-tract care and compression techniques. The fixator was used to compress the arthrodesis site for 10 days at a pace of 1 mm/day divided into four times. The arcing of wires in the talus and calcaneum was used to ensure that the arthrodesis site was adequately compressed. CRP levels were measured every 2 weeks until the wound healed and normal values were reached. Patients were seen as outpatients once a month. After radiological healing was confirmed, fixators were dynamized and patients were permitted to walk for another 3–4 weeks. After the fixator was removed, a plaster slab was applied for 2 weeks. After the pin tracts and skin wounds healed, a below-knee cast was applied for 6 weeks. Following that, a shoe raise with a rocker bottom sole was given.
Results
In our study, 20 patients were operated for ankle arthrodesis with the Ilizarov fixator frame. Patient age ranged from 33 to 68 years with an average of 44.75 years. 14 patients out of 20 had active osteomyelitis and the average number of previous surgeries done were 1.3 ranging from 0 to 4. The external fixation time averaged 22.9 (range 18–34) weeks. The average postoperative limb length discrepancy (LLD) was 1.9 cm (range 1–2.5 cm) and all the patients were given an appropriately sized shoe raise as none of the patients opted for bone lengthening. The average period of follow-up for all patients was 39.4 (26–50) months. Bony union was achieved in all patients (100%) at the end of the study (Fig. 5). After fusion, patients reported either no pain or mild discomfort, all could walk independently without assistance, and all were satisfied with the procedure.
On the basis of ASAMI (Association for the Study and Application of the Methods of Ilizarov) criteria, 17 patients had excellent bone scores, 2 as good and 1 as fair. (Table 2). 18 patients had good ASAMI functional scores with the remaining two as fair (Table 3). Because the ASAMI functional score included ankle range of motion, the maximum attainable function score for the fusion group was “good”.
Complications occurred in six patients, with four developing pin-tract infections which healed after oral antibiotics, repeated dressing, and wound care, and one patient had wire breakage of the forefoot ring.
Discussion
Ankle arthrodesis can be performed utilizing a variety of techniques, including external fixator compression [15, 16], internal fixation with plates or screws [17,18,19], intramedullary fixation [20], and arthroscopic ankle fusion [21]. Charnley was the first to describe the use of external fixation for ankle fusion [22]. The fixators employed were monopolar, and there were numerous difficulties such as motion at the fusion site, malunion, and delayed union. This led to the development of triangular frames to improve fixation and provide multiplanar compression [15, 23].
The Ilizarov ring fixator has distinct benefits over conventional fusion methods, making it an excellent fixing tool in patients with severe ankle pathologies [10, 16, 24]. These include dynamic axial fixation, which keeps bone contact without the need for additional bone grafting, excellent bending, shear, and torsional stability, which allows for early weight-bearing and reduces pin-tract infection, and great modularity with circumferential mechanical control, which allows for postoperative adjustments that are impossible with nails, screws, or plates. Ilizarov wires applied percutaneously can offer stable fixation in osteoporotic bones. Furthermore, arthrodesis can be performed as a one-stage procedure in the presence of active infection. Bony fusion can also be improved by gradually compressing the fusion site.
Hammerschlag achieved substantial fusion in all ten of his patients, including two who had previously failed arthrodesis, utilizing a basic two-ring circular frame [16]. Yanuka et al. conducted Ilizarov arthrodesis on six patients suffering from posttraumatic arthrosis both with and without infection. All patients had a painless fusion between 7 and 15 weeks [25].
In our study, we have fixed the arthrodesis provisionally with thick K-wires and used a simple preconstructed frame that was slid over the leg. The fixator rings were used as a reference guide to put the fixation elements. The elements were fixed to the rings without any stress on the components. The removal of malleoli allowed us to close the skin flaps without much tension as we got redundant skin post-removal of malleoli. We were able to achieve gradual compression over the fixator postoperatively till we saw arcing of talar or calcaneal wire.
Complications are a part of every procedure and ankle arthrodesis with an Ilizarov fixator also presents some. Pin-tract infections and non-union are the most frequent complications which can be reduced with proper care of pin-tract, weight-bearing, and sufficient compression at the fusion site. Joint infection and necrosis of the talus have been cited as the main causes of non-union [15]. Other risk factors include smoking, medical comorbidities, and insufficient compression [15, 26].
Ilizarov ring fixation provides the advantage of permitting early weight-bearing and has been indicated in situations with severe ankle joint disease and when bone quality is impaired to the point where adequate screw thread purchase is doubtful. Furthermore, external ring fixation allows for post-operative correction of bone alignment and joint compression.
Conclusion
Ilizarov fixator should be considered as an important tool for arthrodesis in failed ankle fractures, Charcot joint, and arthritis of ankle joint especially in presence of infection when the other methods of internal fixation are difficult to consider. Ilizarov ring fixator has an advantage over the other external fixators for better control of axial and torsional forces, better hold in osteoporotic bones, and hence providing stable fixation which would aid in early healing of fusion site.
References
Fragomen, A. T., Borst, E., Schachter, L., Lyman, S., & Rozbruch, S. R. (2012). Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion. Clinical Orthopaedics and Related Research, 470, 2864–2873.
Rabinovich, R. V., Haleem, A. M., & Rozbruch, S. R. (2015). Complex ankle arthrodesis: review of the literature. World J Orthop, 6, 602–613.
Siebachmeyer, M., Boddu, K., Bilal, A., Hester, T. W., Hardwick, T., Fox, T. P., et al. (2015). Outcome of one-stage correction of deformities of the ankle and hindfoot and fusion in Charcot neuroarthropathy using a retrograde intramedullary hindfoot arthrodesis nail. Bone Jt J, 97-B, 76–82.
Perlman, M. H., & Thordarson, D. B. (1999). Ankle fusion in a high risk population: an assessment of nonunion risk factors. Foot and Ankle International, 20, 491–496.
Christian, C. A., & Donley, B. G. (1998). Arthrodesis of ankle, knee, and hip. In S. T. Canale (Ed.), Campbell’s operative orthopaedics (9th ed., pp. 145–187). St. Louis: Mosby-Year Book.
Ogut, T., Glisson, R. R., Chuckpaiwong, B., Le, I. L., & Easley, M. E. (2009). External ring fixation versus screw fixation for ankle arthrodesis: a biomechanical comparison. Foot and Ankle International, 30, 353–360.
Hagen, R. J. (1986). Ankle arthrodesis: problems and pitfalls. Clinical Orthopaedics, 170, 184.
Iwata, I., & Norimassa, Y. (1980). Arthrpdesis of the ankle joint with rheumatoid arthritis: experience with the transfibular approach. Clinical Orthopaedics, 153, 189.
Lance, E. M., Paval, A., & Fries, I. (1979). Arthrodesis of the ankle joint: a follow-up study. Clinical Orthopaedics, 142, 146.
Hawkins, B. J., Langerman, R. J., Anger, D. M., & Calhoun, J. H. (1994). The Ilizarov technique in ankle fusion. Clinical Orthopaedics and Related Research, 303, 217–225.
Kalish, S., Fleming, J., & Weinstein, R. (2003). External fixators for elective rearfoot and ankle arthrodesis. Techniques and indications. Clinics in Podiatric Medicine and Surgery, 20, 65–96.
Mann, R. A., Van Manen, J. W., Wapner, K., & Martin, J. (1991). Ankle fusion. Clinical Orthopaedics, 268, 49–55.
Sakurakichi, K., Tsuchiya, H., Uehara, K., et al. (2003). Ankle arthrodesis combined with tibial lengthening using the Ilizarov apparatus. Journal of Orthopaedic Science, 8, 20–25.
Yanuka, M., Krasin, E., Goldwirth, M., Cohen, Z., & Otremski, I. (2000). Ankle arthrodesis using the Ilizarov apparatus: good results in 6 patients. Acta Orthopaedica Scandinavica, 71, 297–300.
Berman, A. T., Bosacco, S. J., Yanicko Jr, D. R., & Raisis, L. W. (1989). Compression arthrodesis of the ankle by triangular external fixation: an improved technique. Orthopedics, 12, 1327–1330.
Hammerschlag, W. A. (1996). Ankle arthrodesis using a ring external fixator. Techniques in Orthopaedics, 11, 263–268.
Braly, W. G., Baker, J. K., & Tullos, H. S. (1994). Arthrodesis of the ankle with lateral plating. Foot & Ankle, 15, 649–653.
Gruen, G. S., & Mears, D. C. (1991). Arthrodesis of the ankle and subtalar joints. Clinical Orthopaedics, 268, 15–20.
Mears, D. C., Gordon, R. G., Kann, S. E., & Kann, J. N. (1991). Ankle arthrodesis with an anterior tension plate. Clinical Orthopaedics, 268, 70–77.
Kile, T. A., Donnelly, R. E., Gehrke, J. C., Werner, M. E., & Johnson, K. A. (1994). Tibiotalocalcaneal arthrodesis with an intramedullary device. Foot and Ankle International, 15, 669–673.
Cameron, S. E., & Ullrich, P. (2000). Arthroscopic arthrodesis of the ankle joint. Arthroscopy, 16, 21–26.
Charnley, J. (1951). Compression arthrodesis of the ankle and shoulder. J. Bone Jt Surg, 33-B, 180–191.
Williams Jr, J. E., Marcinko, D. E., Lazerson, A., & Elleby, D. H. (1983). The calandruccio triangular compression device. A schematic introduction. J Am Podiatry Assoc, 73, 536–539.
Johnson, E. E., Weltmer, J., Lian, G. J., & Cracchiolo, A., III. (1992). Ilizarov ankle arthrodesis. Clinical Orthopaedics, 280, 160–169.
Fink, B., Niggemeyer, O., Schneider, T., Strauss, J. M., & Ruther, W. (1996). Reasons for non-unions after arthrodeses of the ankle. Foot and Ankle Surgery, 2, 145–154.
Donley, B. G., & Ward, D. M. (2002). Implantable electrical stimulation in high-risk hindfoot fusions. Foot and Ankle International, 23, 13–18.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ajit Chalak, Sushmit Singh, Ashok Ghodke, Sachin Kale, Javed Hussain, and Ronak Mishra declare that they have no conflict of interest.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chalak, A., Singh, S., Ghodke, A. et al. Ilizarov Ankle Arthrodesis: A Simple Salvage Solution for Failed and Neglected Ankle Fractures. JOIO 56, 1587–1593 (2022). https://doi.org/10.1007/s43465-022-00669-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00669-6