Abstract
Purpose
Complex ankle fractures accompanied with infection and segmental bone loss are a worrying issue. This prospective study was conducted to explore the effectiveness of using Ilizarov concepts in achieving salvage arthrodesis and reconstructing post-debridement defects in such complicated scenarios.
Methods
A total of 44 consecutive patients (mean age 35.61 ± 8.57 years, 30 males, 44 feet) of post-traumatic infected ankle fractures, who met our selection criteria, were enrolled and subjected to radical debridement and salvage arthrodesis using the bifocal bone transport concepts of Ilizarov. All patients were treated between 2012 and 2017 either by acute shortening compression of the arthrodesis site with re-lengthening (ASRL) through the created proximal metaphyseal osteotomy (group I, n = 20) or by gradual bone transport (BT) through the proximal osteotomy with gradual closure of the distal ankle defect (group II, n = 24). Plain-radiographs were used for radiological assessment. Clinically, the outcomes were objectively graded according to the Hawkins criteria, while subjectively the patients reported their satisfaction on a 1–5 points acceptance scale.
Results
The mean follow-up was 37.16 ± 5.31 (30–48 months). Successful fusion was achieved in 43/44 patients, with a significantly (P < 0.05) lesser needs for bone-grafting in favour of group II. The results were good in 32 cases, fair in 11, and poor in a single case with no significant difference between the two groups. The acceptance scores were significantly (P < 0.05) superior in group II (3.08 ± 1.1 points) than that group I (2.25 ± 1.4 points).
Conclusions
Bifocal bone transport is effective in salvaging troublesome infected ankle fractures with bone loss. BT is more comprehensive and acceptable than ASRL with lesser needs for bone grafting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle injuries involving the distal tibia and/or talus associated with infection and bone loss are a matter of concern and have limited treatment options. The main technical difficulties are the existence of infection, soft-tissue loss, bone defects, and leg shortening. The shortening is due either to the initial violent event or to the subsequent debridement procedures [1,2,3]. The goals of treatment are essentially directed for controlling infection, having a plantigrade and painless foot, and promoting rapid recovery to previous activities. It is difficult to obtain the above-mentioned goals by methods other than arthrodesis. In this concern, the internal fixation modalities, which could provide better patients’ compliance after ankle arthrodesis, is not appropriate in the settings of complicated scenarios, which makes external fixation a more applicable alternative [4,5,6]. One of the traditional techniques in ankle arthrodesis is the use of simple external fixator around the ankle to stabilize and to compress the arthrodesis site. The drawback of such technique is the residual limb shortening with high failure rates [7, 8]. The rational of the present study was to evaluate the results of bifocal bone transport concepts using the Ilizarov external fixator to achieve reasonable union rates and to compensate the resultant shortening after through radical debridement of the infected tissues.
Patients and methods
This prospective study included 44 consecutive patients of infected post-traumatic ankle defects, who met our selection criteria and were treated in the authors’ institution between 2012 and 2017 (Table 1). Inclusion criteria involved isolated ankle fractures complicated by deep infection, while exclusion criteria included any debilitating comorbidity, smoking, associated neurovascular injuries, and ipsilateral lower limb fractures. There were 30 males and 14 females with a mean age 35.61 ± 8.57 years. Patients were subjected to two to three debridement settings before they presented to our institute. Informed consents were obtained from all the patients before surgery.
Operative technique
All procedures were performed under general or epidural anaesthesia in supine position. A tourniquet was applied routinely until completion of debridement and deflated thereafter. All cases were subjected to removal of the existing implants and radical debridement of all infected bone and soft-tissues through either anterior or transmalleolar approaches. The articular surface of the distal tibia and talus (or calcaneus in cases of talectomy) was thoroughly debrided. The procedure was then completed by applying a bridging Ilizarov frame and creating proximal tibial metaphyseal osteotomy. Two different techniques were used to achieve arthrodesis and to compensate the resulting post-debridement shortening. The first technique (group I, n = 20 cases) consisted of acute shortening of the arthrodesis site and re-lengthening (ASRL) through the proximal metaphyseal osteotomy. The second technique (group II, n = 24 cases) was gradual bone transport (BT) through the proximal osteotomy with gradual closure of the resultant distal ankle defect (Fig.1). The wound over the defect in group II was primarily sutured over a wide-bore suction drain which was left for ten days. The use of either methods depended on the size of the intra-operative post-debridement defect. ASRL was used for defects not more than 3 cm, while BT was reserved for larger defects (i.e., > 3 cm). The mean bone defects in group I was 2.45 ± 0.51, while those in group II was 5.17 ± 0.76.
Post-operative regimen and patient’s evaluation
Patients were discharged from the hospital after 48 hours and they were educated how to clean the frame and how to deal with wound dressing. They were instructed to attend the first follow-up visit at the tenth post-operative day. At this visit, gradual distraction at the proximal osteotomy site was started at a rate of divided 1 mm per day among both groups, with an additional step of compression at the distal post-debridement defect in group II. Patients were then followed up radiologically every two weeks to evaluate the course of lengthening in group I and to monitor the progress of the transport among group II. Also, the quality of the newly formed bone at the proximal distraction site was evaluated, frame stability was checked, and pin tract infection, if any, was managed. Partial weight-bearing was allowed as tolerated using walking aids. Follow-up was conducted every two weeks until the expected length was gained in group I and till the transported fragment reached the docking site in group II. At this step, the arthrodesis site in group I was examined clinically and radiologically for signs of fusion and for the need of iliac-rest bone grafting. Also, the docking site among group II patients was routinely refreshed in a second planned surgery with removal of all interposed tissues to provide good contacting surfaces between the two opposing fragments. The quality of bone ends was also evaluated for the need of bone grafting.
Patients were then followed every month to monitor the consolidation of both the proximal regenerate site and the arthrodesis site, and to manage any malalignment, if any. Consolidation was confirmed clinically by the ability of the patient to perform single-leg stance test on the operated side and radiologically by complete ossification of at least three cortices. Frame was then removed under sedation in an out-patient basis and an above-knee weight-bearing cast was applied for additional four weeks.
The outcomes were graded as good, fair, or poor based on the criteria described by Hawkins et al. [9]. A good outcome indicted achieving solid ankle fusion with a plantigrade painless foot with an acceptable function. A fair outcome was considered in cases where the fusion site had achieved union but in a deformed and/or painful state. A poor result was resorted to cases with failure to attain ankle fusion or by persistence of infection. In addition, patients were asked to fulfill a subjective satisfaction scale between 1 and 5 points to provide their acceptance and tolerance to the whole procedure, with higher scores indicated more acceptance.
Statistical analysis
The results were expressed as means and standard deviations. The t test was used to compare two mean numerical values; while the chi-square test was used for comparing categorical variables. P value < 0.05 was considered significant.
Results
The mean follow-up was 36.95 ± 6.09 months in group I and 37.33 ± 4.74 in group II. All results are summarized in Table 2. Successful fusion was achieved in 43 of the 44 patients (e.g. Figs. 2, 3). None of the cases ended up with mal-union or had limb length discrepancy. Bone grafting was essential in only 20.8% (5/24) of group II patients, which was significantly lesser (P < 0.05) than those needed in group I (55% (11/20) of cases). The mean external fixation index which is the time needed to complete consolidation of the regenerate divided by the length of the defect was 35.58 ± 2.95 and 36.7 ± 2.82 days/cm in groups I and II, respectively. According to the Hawkins criteria, the results were good in 32 cases, fair in 11, and poor in a single case with no significant difference (P > 0.05) between the two groups. The mean acceptance score was 2.25 ± 1.4 in group I and 3.08 ± 1.1 in group II, and the difference between the two groups was significant (P < 0.05). Regarding the effect of different variables on the results, there was no significant effect (P > 0.05) of either the age, gender, size of the post-debridement defect, or the primary cause of injury on the final functional or radiological end results.
a Clinical and radiographic photos of 34-year-old male presented with an infected open fracture-dislocation of the right ankle after 2 unsuccessful debridement settings. b Radical debridement and talectomy was done resulting in 4-cm bone defect. c Gradual BT was done and finally the docking site was explored and debrided with no need for bone grafting. d Final clinical and radiological photos with fixator index 34 days/cm, good Hawkins result, and a satisfaction score of 4 points
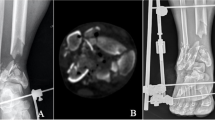
a Clinical and radiographic photos of 50-year-old female presented with bimalleolar fracture and infected hardware after 2 unsuccessful debridement settings. b Radical debridement was done with a resulting 3-cm bone defect. c ASRL was performed with no need for bone grafting. d Final clinical and radiological photos with fixator index 36 days/cm, good Hawkins result, and a satisfaction score of 2 points
A 50-year-old patient in group I showed aseptic nonunion of the arthrodesis site during follow-up. Revision arthrodesis, by internal fixation and iliac crest bone graft, was performed, with a successful solid fusion. Refracture of the regenerate site was recorded in one patient in group II at three months after frame removal because of falling on the stairs, and an above-knee casting for two months was enough to manage this issue. During the process of transport, 15 patients needed further unplanned procedures in the form of wires/pins exchanging because of infection in six cases and further debridement of the infection site in the other nine cases.
Discussion
Complex ankle fractures complicated by infection and bone destruction are a worrying issue leaving sizeable defect either from the original accident or after radical debridement of devitalized bone and soft-tissue envelope [1, 2]. Ankle arthrodesis is considered the method of choice in these complicated scenarios. Many methods were introduced to achieve sound successful arthrodesis across the ankle including internal fixation by screws, monolateral external fixators, and the more applicable circular Ilizarov external fixator [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Principles of successful fusion across infected ankles are radical debridement of all infected and devitalized tissues, adequate bone apposition, good blood supply to opposing bone ends, and stable fixation [2, 3]. To achieve the above-mentioned principles, residual limb shortening is inevitable and should be compensated. The choices available to overcome this dilemma and to reconstruct such defects are limited and include the bone transport Ilizarov principles. In this prospective study, radical debridement of all the infected bone and soft-tissues was essentially performed in all included cases. The resulting post-debridement defect was measured, which was the basis for our choice of one of the two main Ilizarov principles (i.e., ASRL or BT) to compensate such defects. There is a general agreement that acute bone compression in the leg is allowed in no more than 3 cm to avoid compressing neurovascular structures [20, 21]. Accordingly, either ACRL (for ≤ 3 cm defects) or BT (more than 3 cm) was selected in the present study depending on the post-debridement defect.
In the literature, few studies focused on the bifocal method of Ilizarov procedure with proximal osteotomy to achieve ankle fusions. Hawkins et al. [9] reported solid fusion with satisfactory results in 16 of their 20 patients with complex ankle pathology treated with Ilizarov fixator. Salem et al. [14] used proximal tibial lengthening in six of their 22 cases and stated that lengthening allows debridement of all necrotic bone while overcoming the resulting shortening. In a series of six cases, Sakurakichi et al. [18] documented satisfactory results of ankle arthrodesis using Ilizarov fixator (ASRL in three cases and BT in the other three). Kotnis et al. [22] reported a single case of infected total ankle arthroplasty successfully managed using the bone transport concept. Katsenis et al. [23] described two cases of infected nonunion that were efficiently managed by removal of all dead bone, acute compression, and deformity correction followed by proximal lengthening. Moreover, Kienast et al. [24] in his large series including 133 cases of infected ankle fractures used a two-stage technique; first radical debridement and antibiotic beads with applying a simple fixator. This was followed by second grafting setting after four weeks. They reported uncontrollable infection in 4.5% of their cases which necessitated below knee amputations. Also, there was leg length discrepancy of 13 mm in average. Our results are comparable to the work of Mochocki et al. [25] who reported satisfactory outcomes in all of their 18 patients with ankle arthrosis managed by the bifocal concept. They stated that patients appreciated the early undependable weight-bearing of the operated limb through the course of treatment.
The cornerstone of our procedures was radical resection of all devitalized infected bone/soft-tissues which is crucial for eradicating the infection and achieving successful fusion. Moreover, the proximal metaphyseal osteotomy provides gradual distraction of the transporting bone with the benefit of compensating the resultant post-debridement defect/shortening. This is beside the added theoretical benefits of increasing blood flow of the affected limb as proposed previously by Salem [14] and Sakurakichi [18]. All cases except one (group I) have caught complete consolidation of the lengthening site and fusion of the arthrodesis site. The only non-united case among this group was a 50-year-old male with a 3-cm post-debridement bone defect on top of infected pilon fracture. He developed aseptic failure of the fusion after three months following frame removal and was successfully managed by revision arthrodesis using internal fixation and iliac crest bone grafting. In the present study, the final mean Hawkins clinical scores were comparable (P > 0.05) between the two groups, with 32 patients assigned good results, 11 cases of fair, and a single case of poor results. Additionally, all patients were subjected to a questioner to report their subjective satisfaction and acceptance of the whole procedure which was significantly superior (P < 0.05) in favor of the BT technique (group I).
Grafting of the arthrodesis site is reported as a chief step to guarantee reasonable union. During the follow-up visits in the current study, the fusion site in group I (ASRL) was evaluated radiologically and clinically with 11 (55%) of the 20 cases subjected to bone grafting. Regarding group II (i.e., BT cases), the arthrodesis site was explored and refreshed as a routine planned second stage at the end of the transport method. Interestingly, the ends of the transported fragment and the docking site were healthy with good blood supply and only five (20.8%) of the included 24 cases in this group needed bone grafting. The need for bone grafting of the arthrodesis site, with its known donor site morbidity, was significantly less in the BT group (P < 0.05).
Another attractive alternative for radical resection and reconstruction of such bone defects is the induced membrane (Masquelet) technique [26]. This comprises filling the post-debridement defect by cement spacer for about six weeks followed by removal of the spacer, cancellous bone grafting, and fixation. However, the benefits of this procedure are partially outweighed by the need for a series of operative intervention, started by the initial debridement setting, passing through osteosynthesis procedure as a second planned stage, and then removing the hardware later. This is in addition to the reported issues that morbid reinfection, refracture, and graft donor site commonly complicate this procedure [27].
The present study highlights the effectiveness of applying Ilizarov principles in managing infected ankle fractures with bone defects. Also, our results indicate the preference for BT technique over the ASRL in these settings because of the following:
-
The ability of BT to overcome any defect, whatever its size, which is considered a shortage in the ASRL technique that is only applicable for ≤ 3 cm defects.
-
More patients’ acceptance and satisfaction immediately after surgery in group II as a result of not feeling crippled by any limb discrepancy which is usually accompanying the cases in group I until they complete the re-lengthening period.
-
During bone transport, the gradual proximal distraction with progressive closure of the post-debridement defect propels any residual hidden infected tissues with subsequent lesser incidence of recurrence of infection at the arthrodesis site.
-
Gradual BT gives better chance to the operator to re-evaluate the need for bone grafting at the docking site, if any, after the completion of the transport. Hence, the need to perform bone grafting is significantly less required.
This study has some shortcomings. First, the limited number of cases is the main shortcoming which is expected due to our strict selection criteria because cases with debilitating comorbidity, smoking, associated neurovascular injuries, or ipsilateral lower limb fractures were intently excluded to minimize the known adverse impacts of these variables on the outcomes. Second, we are likely to be criticized for our approach in comparing the efficiency of two different Ilizarov techniques in the presence of a noticeable difference in the size of the reconstructed bone defects between the two groups. Nevertheless, it is worth noting that the fixator index used in this study, which does not depend at all on the size of bone defect, was comparable (P > 0.05) between the two studied groups. This is in addition to that the results among group II, which included more complicated injuries, were better than the results in group I, which highlights the noticeable superiority of the former. Therefore, it is self-evident that its use in less-affected cases is more easy and effective.
Conclusions
Applying Ilizarov principles in managing infected ankle fractures with bone loss is effective in overcoming all aspects of the problem. BT is more comprehensive and acceptable than ASRL with lesser rates of bone grafting.
References
SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS (2009) Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am 91(5):1042–1049
Chalayon O, Wang B, Blankenhorn B (2015) Factors affecting the outcomes of uncomplicated primary open ankle arthrodesis. Foot Ankle Int 36(10):1170–1179
Bozic V, Thordarson DB, Hertz J (2008) Ankle fusion for definitive management of non-reconstructable pilon fractures. Foot Ankle Int 29:914–918
Hoover JR, Santrock RD, James WC (2011) Ankle fusion stability: a biomechanical comparison of external versus internal fixation. Orthopedics 34
Ogut T, Glisson RR, Chuckpaiwong B, Le IL, Easley ME (2009) External ring fixation versus screw fixation for ankle arthrodesis: a biomechanical comparison. Foot Ankle Int 30:353–360
Thevendran G, Younger A, Pinney S (2012) Current concepts review: risk factors for nonunion in foot and ankle arthrodesis. Foot Ankle Int 33:1031–1040
Kiene J, Schulz AP, Hillbricht S, Jürgens CH, Paech A (2009) Clinical results of resection arthrodesis by triangular external fixation for posttraumatic arthrosis of the ankle joint in 89 cases. Eur J Med Res 14(1):25–29
Kollig E, Esenwein S, Muhr G, Kutscha-Lissberg F (2002) Fusion of the septic ankle: experience with 15 cases using hybrid external fixation. J Trauma 55:685–691
Hawkins BJ, Langerman DO, Anger DM, Calhoun JH (1994) The Ilizarov technique in ankle fusion. Clin Orthop 303:217–225
Rochman R, Jackson Hutson J, Alade O (2008) Tibiocalcaneal arthrodesis using the Ilizarov technique in the presence of bone loss and infection of the talus. Foot Ankle Int 29:1001–1008
El-Rosasy M, Mahmoud A, El-Gebaly O, Rodriguez E, Thione A (2019) Definition of bone transport from an orthoplastic perspective. Int J Orthoplastic Surg 2(2):62–71
Zarutsky E, Rush SA, Schubereth JM (2005) The use of circular wire external fixation in the treatment of salvage ankle arthrodesis. J Foot Ankle Surg 44:22–31
Fragomen AT, Borst E, Schachter L, Lyman S, Rozbruch SR (2012) Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion. Clin Orthop Relat Res 470:2864–2873
Salem KH, Kinzl L, Schmelz A (2006) Ankle arthrodesis using Ilizarov ring fixators: a review of 22 cases. Foot Ankle Int 27:764–770
Saltzman CL (2005) Salvage of diffuse ankle osteomyelitis by single stage resection and circumferential compression frame arthrodesis. Iowa Orthop 25:47–52
Kitaoka HB, Anderson PJ, Morrey BF (1992) Revision of ankle arthrodesis with external fixation for non-union. J Bone Joint Surg Am 74-A:1191–1200
Onodera T, Majima T, Kasahara Y, Takahashi D, Yamazaki S, Ando R, Minami A (2012) Outcome of transfibular ankle arthrodesis with Ilizarov apparatus. Foot Ankle Int 33:964–968
Sakurakichi K, Tsuchiya H, Uehara K (2002) Ankle arthrodesis combined with tibial lengthening using the Ilizarov apparatus. J Orthop Sci 8:20–25
Kovoor CC, Padmanabhan V, Bhaskar D, George VV, Viswanath S (2009) Ankle fusion for bone loss around the ankle joint using the Ilizarov technique. J Bone Joint Surg (Br) 91(8):1120
El-Rosasy MA (2007) Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Joint Surg (Br) 89(1):80–88
Atef A, El-Tantawy A (2014) Management of open infected comminuted tibial fractures using Ilizarov concept. Eur J Orthop Surg Traumatol 24(3):403–408
Kotnis R, Pasapula C, Anwar F, Cooke PH, Sharp RJ (2006) The management of failed ankle replacement. J Bone Joint Surg (Br) 88-B:1039–1047
Katsenis D, Bhave A, Paley D, Herzenberg JE (2005) Treatment of malunion and non-union at the site of an ankle fusion with the Ilizarov apparatus. J Bone Joint Surg Am 87-A:302–309
Kienast B, Kiene J, Gille J, Thietje R, Gerlach U, Schulz P (2010) Posttraumatic severe Infection of the ankle Joint long term Results of the treatment with Resection Arthrodesis In 133 cases. J Med Res 15:54–58 I
Mochocki K, Górski R, Żarek S, Szelerski L, Małdyk P (2018) Ankle arthrodesis with simultaneous lengthening of the lower limb using the Ilizarov fixator. Orrttopediia Traumatologia Rehabilitacja 6(6); Vol. 20, 465–474
Masquelet AC, Begue T (2010) The concept of induced membrane for reconstruction of long bone defects. Orthop Clin N Am 41:27–37
Morris R, Hossain M, Evans A, Pallister I (2017) Induced membrane technique for treating tibial defects gives mixed results. Bone Joint J 99-B(5):680–685
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
All procedures performed were in accordance with the ethical standards of our institutional ethical committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consents were obtained from all patients before their participation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Atef, A., El-Rosasy, M. & El-Tantawy, A. Salvage arthrodesis for infected ankle fractures with segmental bone-loss using Ilizarov concepts: a prospective study. International Orthopaedics (SICOT) 45, 233–240 (2021). https://doi.org/10.1007/s00264-020-04874-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04874-6