Abstract
Purpose
To investigate comparative study for potential associations of adverse outcomes as well as survival rates after high tibial osteotomy (HTO) and unicompartmental knee arthroplasty (UKA).
Methods
We reviewed the Korean National Health Insurance claims database from January 1, 2007 to May 31, 2019. A total of 90,705 patients aged 30–90 years who were newly treated for HTO or UKA were identified considering their eligibility. We performed four rounds of propensity score matching to reduce imbalance of baseline characteristics, especially disparities among different age groups. Multivariable logistic regression models were used to compare the risk of revision and various unwanted medical problems between HTO and UKA treatment groups after propensity score matching.
Results
23,563 matched patients were assigned to each group on the basis of propensity score. HTO showed higher risk of revision than UKA at 5 years, 10 years and the whole observed period (hazard ratio: 1.21, 95% CI 1.10–1.34). Deep vein thromboembolism (0.27, 0.21–0.35), and surgical site infection (0.37, 0.30–0.44) were less likely for HTOs than UKAs. Postoperative admission to intensive care unit was significantly lower with HTO (odds ratio: 0.40, 0.29–0.54) while rehospitalization within 30 days (1.27, 1.16–1.38) and 90 days (1.24, 1.18–1.30) were higher than UKA.
Conclusion
When choosing the surgical method for unicompartmental knee OA, not only the survival rate, but also the risk of other adverse outcomes should be considered. In particular, attention should be paid to the risk of developing deep vein thromboembolism and surgical site infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) of the knee joint, a global health problem regardless of race, region, or gender, is one of the major diseases that degrade quality of life [1]. The spectrum of treatment ranges from conservative to surgical treatments [2]. It is reported that about half of the OA cases of the knee joint predominantly occur in the medial compartment, relatively preserving the lateral compartment and patellofemoral joint [3,4,5]. Although total knee arthroplasty (TKA) is widely recognized as the ultimate and a popular treatment for symptomatic late-stage OA, it is not preferred as a primary surgical method for OA limited to the medial compartment [6]. Instead of TKA, high tibial osteotomy (HTO) and unicompartmental knee arthroplasty (UKA) are being implemented and considered as well-documented, representational treatments for medial knee OA [7,8,9]. However, in the orthopedic field, the appropriate choice of UKA or HTO for performing a surgical treatment in patients who failed conservative treatment is a debatable issue even after decades of research [10,11,12]. The number of UKAs and HTOs performed continues to increase, and the range of surgical indication is expanding with the improvement of surgical methods and advances in implant design [13,14,15,16,17]. Various factors on the patient's side affect the selection of the two surgical methods, and the operator's training background and personal experience are also deeply involved. Moreover, both UKA and HTO provide effective and reliable results [18]. Thus, the surgical indications for both procedures have expanded, sharing a large proportion of the patient selection criteria [19]. Numerous studies have been carried out to compare the advantages and clinical results between these surgical methods, but it has not been proven that one is superior to the other [20]. However, there only small-randomized, limited reviews of literature, short-term retrospective, and individual cohort studies comparing the two surgeries exist. This study aimed to: (1) evaluate trends in utilization and revision rates of the two surgical methods and (2) analyze perioperative complications considering age-stratified subgroup characteristics.
Materials and Methods
Data Sources
We carried out a nationwide cohort study using the National Health Insurance Service (NHIS) that covers the entire Korean population. South Korea has one of the largest NHIS systems in the world, which is mandated by law and covers up to 99% of the South Korean population [21, 22]. The Korean NHIS collects database records, diagnoses, and related procedures based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes and Electronic Data Interchange codes. The NHIS database of South Korea provides data on individual identification codes, and the data linked to each code provides information on the patient age, gender, diagnosis, hospitalization records, surgical records, medication prescriptions, and local information of the hospital. Data from 1 January 2008 to 31 May 2019 were collected. Details of patients diagnosed with knee joint OA and undergoing surgical treatment for it were collected. All patient identification codes were encrypted and anonymized to ensure confidentiality in our study.
Data Collection
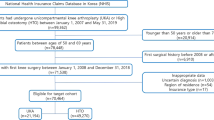
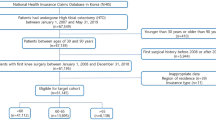
We extracted data of patients who underwent UKA or HTO for treatment of knee OA between 1 January 2008 and 31 May 2019, using the diagnostic code for knee OA (M17) and procedure codes for UKA (N2712, N2717) or HTO (N0304). Patients under 30 or over 90 years of age at the time of surgery were excluded. To identify cases that were newly diagnosed and eliminate the influence of previous procedures, a 1-year washout period without documented knee OA and its surgical treatment was established. We compared UKA and HTO by analysing the conversion to primary TKA, unwanted medical adverse outcomes, and various perioperative complications. To balance the baseline characteristics of the two groups and minimise the effect of potential confounders, we performed propensity score matching (PSM). The baseline characteristics were extracted based on the age, sex, type of insurance, type of hospital, the region of residence, and underlying diseases. The type of hospital was classified as teaching, general, independent, and private. The region of residence was classified based on the population as a city with a population of 10 million or more, 1 million or more, and city with a population of less than 1 million. The presence of underlying diseases was confirmed based on the ICD-10 diagnostic codes, with at least two claims within a year from the date of surgery. The Charlson Comorbidity Index (CCI) score was calculated from the ICD-10 codes by methods described in previous literature. We identified the difference in the baseline characteristics between the two groups and corrected it with PSM (Table 1).
Statistical Analysis
We calculated the person-years for each group of patients from the date of the primary surgery to the events of subsequent revision and perioperative complications. To estimate the difference in the survival rate between UKA and HTO, after PSM, we analysed a stratified log-rank and Kaplan–Meier curves with the consideration of potential confounders. Also, conditional logistic and stratified Cox regression analyses were conducted to calculate the perioperative complication rates. The adjusted hazard ratio (HR) and 95% confidence interval (CI) were calculated using a multivariable Cox proportional-hazard regression model adjusted for potential confounders. PSM was utilized to mitigate the imbalance of baseline characteristics between the two groups [23]. Propensity scores for being in the UKA group were estimated using a multiple logistic regression model that included baseline characteristics such as age, sex, CCI, comorbidities, type of insurance, region of residence, and type of hospital. After calculating the propensity scores, patients were matched using the nearest neighborhood (greedy matching) algorithm within a caliper width of 0.1 in propensity scores and with a ratio of 1:1. The balance of covariates between the groups was evaluated with a standardized mean difference (SMD). A SMD less than 0.1 was considered as a negligible difference between the groups.
Subgroup Analysis
Subgroup analyses, according to age (30–49 years, 50–69 years, 70 years and over) were performed; these variables are known to be associated with the indication for both the surgical methods. Outcome measures were analysed in the same context as the entire study population. As the number patients in each surgery group differed, we performed PSM at a different ratio. The applied ratios for PSM were 1:5, 1:1, and 2:1 (for the age groups 30–49 years, 50–69 years, and 70–90 years, respectively) for UKA and HTO (Table 2). All statistical analyses were performed using the R software (version 3.4.1; R Foundation for Statistical Computing) and SAS Enterprise software (version 6.1; SAS Institute Inc.).
Results
A total of 99,362 patients who underwent UKA or HTO during the 11.5-year period from 2008 to 2019 were identified, and regarding the eligibility, cases below the age of 30 or older than 90 years (n = 673), prior history of knee arthroplasties or osteotomies around the knee joint (n = 7897), and with inappropriate data (n = 87) were excluded. In the final target cohort of 90,705 patients, 29,560 patients were treated with UKA and 61,145 patients underwent HTO in the same period. HTO was implemented about twice as many times as UKA (Fig. 1). The rates of UKA and HTO in 2018 compared to 2008 increased by 5.14 times and 6.54 times, respectively, showing a significant increase in both the surgeries in Korea. The average age for UKA was 63.8 years and for HTO was 56.5 years, while the proportion of women in both groups accounted for 81.8% and 74.5%, respectively. In both groups, more than 95% of the patients were covered by medical insurance, and each identified difference in the residential areas, the size of hospitals that conducted the surgery, CCIs, and preoperative underlying diseases are listed in Tables 1 and 2. After PSM, 23,563 patients were assigned to each group, and various indicators were compared after surgery using matched patients.
There was a significant difference in the survival rate between the two groups, with a more substantial increase in the revision rate in HTO than in UKA (p < 0.001) (Fig. 2). The adjusted analysis considering base properties after PSM showed a significantly higher revision rate in HTO (HR: 1.21, 95% CI 1.10–1.34, p = 0.0002). At different time points, HRs were 1.19 (1.07–1.33) at 5 years and 1.21 (1.10–1.34) at 10 years (Table 3). After matching for different age groups, the revision rate was significantly higher for HTO in the age group of 50–69 years, (HR: 1.20, 1.12–1.28, p < 0.0001) and 70–90 years (HR: 1.62, 1.14–2.31, p = 0.007). On the other hand, there was no significant difference in the revision rate in the 30–49 years age group (p = 0.46).
Deep vein thromboembolism (DVT) was significantly less likely for HTO than UKA (HR: 0.27, 95% CI 0.21–0.35, p < 0.0001). Surgical site infection was also significantly lower in HTO than in UKA (HR: 0.37, 95% CI 0.30–0.44, p < 0.0001) in the total target population. Other adverse outcomes, including pulmonary thromboembolism, cerebrovascular disease, myocardial infarction, acute renal failure, and postoperative delirium, showed insignificant differences (Table 4). Postoperative admission to the ICU was significantly lower with HTO (OR: 0.40, 95% CI 0.29–0.54, p < 0.0001), while rehospitalization within 30 days (OR: 1.27, 1.16–1.38, p < 0.001) and 90 days (OR: 1.24, 1.18–1.30, p < 0.001) were significantly increased compared to that with UKA. However, blood transfusion during or after surgery did not differ significantly between the two methods (eTable 10 in the supplementary appendix). When stratified analysis by age was conducted for survival rates and postoperative adverse outcomes, results of the group aged 50–69 years were broadly similar to those of all the patients (eTable 4, eTable 5 in the supplementary appendix). Specifically, DVT and surgical site infection occurred significantly lesser with HTO than with UKA throughout all the age groups (eTable 2, eTable 5, eTable 8 in the supplementary appendix). In the 30–49 years age group, there was significantly lesser difference in survivorship (eTable 1 in the supplementary appendix) and in the risk of adverse outcomes following the two procedures, except for occurrence of DVT (HR: 0.27, 0.09–0.82, p = 0.02) (eTable 2 in the supplementary appendix). The risk of rehospitalization within 30 days (OR: 1.28, 1.01–1.61, p = 0.04) and 90 days (OR: 1.25, 1.09–1.43, p = 0.001) was higher with HTO than with UKA (eTable 9 in the supplementary appendix).
Discussion
Primary surgical treatments considered for knee OA limited to the unicompartment can be broadly divided into UKA and HTO [24]. According to previous studies, up to 47% of the patients suitable for knee replacements only have medial compartment OA [3,4,5]. Therefore, instead of TKA, it is necessary to choose the appropriate primary surgical method for treating medial knee OA. In the present study, during the 11.5-year follow-up period, the survival rate of UKA was significantly higher than that of HTO. Additionally, we found that the incidence of adverse outcomes after each treatment was different. Interestingly, the incidence of postoperative DVT and surgical site infection were higher in UKA than in HTO in the total study population and all age subgroups. For surgical site infections, only deep infections were included and superficial infections were excluded through review of diagnostic codes and a series of medical records.
Surgical treatment of predominantly medial knee OA using UKA or HTO is increasing steadily. In previous literature that reported the utilization status of UKA, UKA accounted for only 5% of the total number of knee arthroplasties in England and Wales, and 8% in the United States and increased by 32.5% annually [16, 17]. In the case of HTO, the number of procedures increased substantially during the last decade, comprising about 11% of TKA utilizations in South Korea [25]. Worldwide, the market for knee replacement surgery is nearing £5 billion annually [2] and the number of procedures for unicompartmental knee OA is also expected to increase [15, 24]. Despite numerous comparative investigations between these two reliable surgical methods, there still exists a lack of clarity regarding the longevity or durability and perioperative adverse outcomes [24, 26].
Long-term survival results, that is conversion to TKA following UKA and HTO varied in previous studies, some authors reported that UKA tends to need revision sooner [27], whereas another resulted in UKA showing better longevity than HTO [4, 12], the others revealed no significant differences in the survivorship [18, 24]. However, a majority of the previous comparative studies had different baseline characteristics. Few studies have performed appropriate survival analyses considering censoring and other confounding factors, which might lead to the known attrition bias. In our study, after PSM and regarding adjusted variables, UKA showed better survival rate than HTO at the 5-year, 10-year follow-up, and throughout the entire study period in all the patients. After the stratified analysis by age, similar results were reported in the patients aged 50–69 years and 70–90 years (eTable 4 and eTable 7 in the supplementary appendix).
The results for postoperative complications varied among different studies in the literature. Some researchers reported that UKA leads to significantly better functional outcomes with lower postoperative complications than HTO [10, 18, 28], while others showed no significant differences [11, 20]. However, to the best of our knowledge, major medical adverse outcomes associated with the two surgical treatments have not been investigated. In particular, the incidence of DVT and surgical site infection was significantly low in the HTO group (Table 4).
The HTO group showed significantly low infection rate, which may be related to a relatively short operation time [29, 30], and showed low risk of DVT possibly due to routine usage of mechanical compression after surgery [31], and pharmacologic prophylaxis [32]. These possible attributing factors were not identified by the Korean NHIS data. The perioperative complications, including admission to the ICU and postoperative rehospitalization within 30 days and 90 days, showed a significant difference between UKA and HTO (eTable 10 in the supplementary appendix). In several studies, the cemented arthroplasty depicted as an independent predictor of a significantly increased likelihood of admission to the ICU after the operation [33, 34]. The strength of our study is the use of one of the largest NHIS systems worldwide. Using strict PSM, we reduced confounders with a well-designed statistical technique. Regarding the different surgical indications mentioned by previous publications, we performed additional three rounds of PSM for each stratified age group (30–49, 50–69, and 70–90), which probably minimised the sampling bias. Even excluding UKA under 50 years old and HTO over 70 years old, the results of age stratified subgroup analysis of between 50 and 70 years showed similar to those of total patients. However, this study has several limitations. First, claims-based studies have inherent problems, including inaccurate diagnostic codes. The diagnostic and procedure codes cannot reflect actual medical history. Second, The Korea National Health Insurance Corporation database does not provide detailed medical records of patients. Thus, the clinical scores and various outcome-associated factors such as body mass index, osteoarthritis stage and degree of leg deformity were not provided. Third, the maximum follow-up period of this study was 11.5 years which can be extended in future studies. Fourth, in the treatment of medial compartment knee OA, it should also be considered that selection bias may occur because each surgeon has different preferences for surgery. Finally, there are still many confounding factors after considerable adjusting of variables and appropriate matching. The severity of OA cannot be identified radiologically, and other confounders such as the type of implants used or different surgical techniques were not considered. Despite these limitations, to the best of our knowledge, the current study is the first large-scale, long-term cohort study with a well-designed validation to evaluate comparative effectiveness of UKA and HTO. Nevertheless, a randomized, level one study is required to compare these two well-documented surgical methods for unicompartmental knee OA.
Conclusions
When choosing the surgical method for unicompartmental knee OA, not only the survival rate, but also the risk of other adverse outcomes should be considered. Notably, patients considering UKA should pay attention to DVT and surgical site infection that may occur after surgery.
Availability of Data and Materials
Korean National Health Insurance Claims Data are available on reasonable request. Study protocol, statistical code: available from the author JKS (e-mail, seonbell@jnu.ac.kr). Dataset: de-identified datasets generated and analysed during the present study will be made available by request from the Health Insurance & Assessment Service of Korea at https://opendata.hira.or.kr/. After user approaval by the Health Insurance Review and Assessment Service, a remote analysis system (https://ras.hira.or.kr) can be used by receiving a virtualized ID.
References
Evans, J. T., Walker, R. W., Evans, J. P., Blom, A. W., Sayers, A., & Whitehouse, M. R. (2019). How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet, 393(10172), 655–663. https://doi.org/10.1016/S0140-6736(18)32531-5
Smith, W. B., 2nd., Steinberg, J., Scholtes, S., & McNamara, I. R. (2017). Medial compartment knee osteoarthritis: Age-stratified cost-effectiveness of total knee arthroplasty, unicompartmental knee arthroplasty, and high tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy, 25(3), 924–933. https://doi.org/10.1007/s00167-015-3821-3
Mohammad, H. R., Matharu, G. S., Judge, A., & Murray, D. W. (2020). New surgical instrumentation reduces the revision rate of unicompartmental knee replacement: A propensity score matched comparison of 15,906 knees from the National Joint Registry. The Knee, 27(3), 993–1002. https://doi.org/10.1016/j.knee.2020.02.008
Cao, Z., Mai, X., Wang, J., Feng, E., & Huang, Y. (2018). Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: A systematic review and meta-analysis. Journal of Arthroplasty, 33(3), 952–959. https://doi.org/10.1016/j.arth.2017.10.025
Beard, D. J., Davies, L. J., Cook, J. A., MacLennan, G., Price, A., Kent, S., Hudson, J., Carr, A., Leal, J., Campbell, H., Fitzpatrick, R., Arden, N., Murray, D., & Campbell, M. K. (2019). The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet, 394(10200), 746–756. https://doi.org/10.1016/S0140-6736(19)31281-4
Mont, M. A., Stuchin, S. A., Paley, D., Sharkey, P. F., Parvisi, J., Tria, A. J., Jr., Bonutti, P. M., & Etienne, G. (2004). Different surgical options for monocompartmental osteoarthritis of the knee: High tibial osteotomy versus unicompartmental knee arthroplasty versus total knee arthroplasty: Indications, techniques, results, and controversies. Instructional Course Lectures, 53, 265–283.
Broughton, N. S., Newman, J. H., & Baily, R. A. (1986). Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5–10 years’ follow-up. Journal of Bone and Joint Surgery. British Volume, 68(3), 447–452. https://doi.org/10.1302/0301-620X.68B3.3733813
Ivarsson, I., & Gillquist, J. (1991). Rehabilitation after high tibial osteotomy and unicompartmental arthroplasty. A comparative study. Clinical Orthopaedics and Related Research, 266, 139–144.
Weale, A. E., & Newman, J. H. (1994). Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clinical Orthopaedics and Related Research, 302, 134–137.
Stukenborg-Colsman, C., Wirth, C. J., Lazovic, D., & Wefer, A. (2001). High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7–10-year follow-up prospective randomised study. The Knee, 8(3), 187–194. https://doi.org/10.1016/s0968-0160(01)00097-7
Takeuchi, R., Umemoto, Y., Aratake, M., Bito, H., Saito, I., Kumagai, K., Sasaki, Y., Akamatsu, Y., Ishikawa, H., Koshino, T., & Saito, T. (2010). A mid term comparison of open wedge high tibial osteotomy vs unicompartmental knee arthroplasty for medial compartment osteoarthritis of the knee. Journal of Orthopaedic Surgery and Research, 5(1), 65. https://doi.org/10.1186/1749-799X-5-65
Rodriguez-Merchan, E. C. (2014). Medial unicompartmental osteoarthritis (MUO) of the knee: Unicompartmental knee replacement (UKR) or total knee replacement (TKR). Archives of Bone and Joint Surgery, 2(3), 137–140.
Zuiderbaan, H. A., van der List, J. P., Kleeblad, L. J., Appelboom, P., Kort, N. P., Pearle, A. D., & Rademakers, M. V. (2016). Modern indications, results, and global trends in the use of unicompartmental knee arthroplasty and high tibial osteotomy in the treatment of isolated medial compartment osteoarthritis. American Journal of Orthopedics (Belle Mead, N.J.), 45(6), E355–E361.
Petersen, W., & Metzlaff, S. (2016). Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: Five years results. Archives of Orthopaedic and Trauma Surgery, 136(7), 983–989. https://doi.org/10.1007/s00402-016-2465-1
Nwachukwu, B. U., McCormick, F. M., Schairer, W. W., Frank, R. M., Provencher, M. T., & Roche, M. W. (2014). Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. Journal of Arthroplasty, 29(8), 1586–1589. https://doi.org/10.1016/j.arth.2014.04.002
Liddle, A. D., Pandit, H., Judge, A., & Murray, D. W. (2015). Optimal usage of unicompartmental knee arthroplasty: A study of 41,986 cases from the National Joint Registry for England and Wales. Bone and Joint Journal, 97-b(11), 1506–1511. https://doi.org/10.1302/0301-620X.97B11.35551
Riddle, D. L., Jiranek, W. A., & McGlynn, F. J. (2008). Yearly incidence of unicompartmental knee arthroplasty in the United States. Journal of Arthroplasty, 23(3), 408–412. https://doi.org/10.1016/j.arth.2007.04.012
Fu, D., Li, G., Chen, K., Zhao, Y., Hua, Y., & Cai, Z. (2013). Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: A meta-analysis. Journal of Arthroplasty, 28(5), 759–765. https://doi.org/10.1016/j.arth.2013.02.010
Oh, K. J., Kim, Y. C., Lee, J. S., Chang, Y. S., Shetty, G. M., & Nha, K. W. (2017). Open-wedge high tibial osteotomy versus unicompartmental knee arthroplasty: No difference in progression of patellofemoral joint arthritis. Knee Surgery, Sports Traumatology, Arthroscopy, 25(3), 767–772. https://doi.org/10.1007/s00167-017-4450-9
Yim, J. H., Song, E. K., Seo, H. Y., Kim, M. S., & Seon, J. K. (2013). Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow-up of 3 years. Journal of Arthroplasty, 28(2), 243–247. https://doi.org/10.1016/j.arth.2012.06.011
Kim, J. A., Yoon, S., Kim, L. Y., & Kim, D. S. (2017). Towards actualizing the value potential of Korea health insurance review and assessment (HIRA) data as a resource for health research: Strengths, limitations, applications, and strategies for optimal use of HIRA data. Journal of Korean Medical Science, 32(5), 718–728. https://doi.org/10.3346/jkms.2017.32.5.718
Kwon, S. (2009). Thirty years of national health insurance in South Korea: Lessons for achieving universal health care coverage. Health Policy and Planning., 24(1), 63–71. https://doi.org/10.1093/heapol/czn037
Austin, P. C. (2011). An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research, 46(3), 399–424. https://doi.org/10.1080/00273171.2011.568786
Song, S. J., Bae, D. K., Kim, K. I., & Park, C. H. (2019). Long-term survival is similar between closed-wedge high tibial osteotomy and unicompartmental knee arthroplasty in patients with similar demographics. Knee Surgery, Sports Traumatology, Arthroscopy, 27(4), 1310–1319. https://doi.org/10.1007/s00167-019-05390-w
Koh, I. J., Kim, M. W., Kim, J. H., Han, S. Y., & In, Y. (2015). Trends in high tibial osteotomy and knee arthroplasty utilizations and demographics in Korea From 2009 to 2013. Journal of Arthroplasty, 30(6), 939–944. https://doi.org/10.1016/j.arth.2015.01.002
Koh, I. J., Kim, M. S., Sohn, S., Song, K. Y., Choi, N. Y., Jung, H., & In, Y. (2019). Predictive factors for satisfaction after contemporary unicompartmental knee arthroplasty and high tibial osteotomy in isolated medial femorotibial osteoarthritis. Orthopaedics and Traumatology: Surgery and Research: OTSR, 105(1), 77–83. https://doi.org/10.1016/j.otsr.2018.11.001
Krych, A. J., Reardon, P., Sousa, P., Pareek, A., Stuart, M., & Pagnano, M. (2017). Unicompartmental knee arthroplasty provides higher activity and durability than valgus-producing proximal tibial osteotomy at 5 to 7 years. Journal of Bone and Joint Surgery. American Volume, 99(2), 113–122. https://doi.org/10.2106/JBJS.15.01031
Santoso, M. B., & Wu, L. (2017). Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. Journal of Orthopaedic Surgery and Research, 12(1), 50. https://doi.org/10.1186/s13018-017-0552-9
Hernandez, A. J., Almeida, A. M., Fávaro, E., & Sguizzato, G. T. (2012). The influence of tourniquet use and operative time on the incidence of deep vein thrombosis in total knee arthroplasty. Clinics (São Paulo, Brazil), 67(9), 1053–1057. https://doi.org/10.6061/clinics/2012(09)12
Wang, Q., Goswami, K., Shohat, N., Aalirezaie, A., Manrique, J., & Parvizi, J. (2019). Longer operative time results in a higher rate of subsequent periprosthetic joint infection in patients undergoing primary joint arthroplasty. Journal of Arthroplasty, 34(5), 947–953. https://doi.org/10.1016/j.arth.2019.01.027
Kim, Y. H., Kulkarni, S. S., Park, J. W., & Kim, J. S. (2015). Prevalence of deep vein thrombosis and pulmonary embolism treated with mechanical compression device after total knee arthroplasty in Asian patients. Journal of Arthroplasty, 30(9), 1633–1637. https://doi.org/10.1016/j.arth.2015.04.001
Snyder, M. A., Sympson, A. N., Scheuerman, C. M., Gregg, J. L., & Hussain, L. R. (2017). Efficacy in deep vein thrombosis prevention with extended mechanical compression device therapy and prophylactic aspirin following total knee arthroplasty: a randomized control trial. Journal of Arthroplasty, 32(5), 1478–1482. https://doi.org/10.1016/j.arth.2016.12.027
Sukhonthamarn, K., Grosso, M. J., Sherman, M. B., Restrepo, C., & Parvizi, J. (2020). Risk factors for unplanned admission to the intensive care unit after elective total joint arthroplasty. Journal of Arthroplasty, 35(7), 1937–1940. https://doi.org/10.1016/j.arth.2020.03.003
Song, S. J., Park, C. H., & Bae, D. K. (2019). What to know for selecting cruciate-retaining or posterior-stabilized total knee arthroplasty. Clinics in Orthopedic Surgery, 11(2), 142–150. https://doi.org/10.4055/cios.2019.11.2.142
Acknowledgements
We appreciate the Ministry of Health and Welfare and the Health Insurance Review & Assessment Service of Korea for sharing invaluable national health insurance claims data. The interpretation and conclusions contained in this study are those of the authors alone. Support was received from Chonnam National University Hwasun hospital.
Author information
Authors and Affiliations
Contributions
SHL, EKS, and JKS were responsible for study design. SHL and HRK take responsibility for the integrity of the data and the accuracy of the data analysis. SHL, HRK, EKS, and JKS were responsible for data interpretation. SHL and JKS prepared and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
IRB approval was obtained prior to the start of this study.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, SH., Kim, HR., Song, EK. et al. Risk of Revision and Adverse Outcomes Following Partial Knee Replacement and High Tibial Osteotomy for Unicompartmental Knee Osteoarthritis: A Nationwide Cohort Study. JOIO 55, 1101–1110 (2021). https://doi.org/10.1007/s43465-021-00517-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00517-z