Abstract
Introduction
A significant portion of knee osteoarthritis is diagnosed in patients under the age of 55, where greater activity demands make total knee arthroplasty less desirable. High tibial osteotomy (HTO) and unicompartmental knee arthroplasty (UKA) are useful alternatives, but there is little understanding of which procedure is advantageous. Hence, this study examines the utilization, complication, and reoperation rates among the HTO vs. UKA in young patients with primary osteoarthritis.
Methods
A retrospective review of the National Surgical Quality Improvement Program was performed to identify 2318 patients < 55 years of age who received either a HTO or UKA for primary osteoarthritis between 2011 and 2021. Bivariate analyses compared preoperative and intraoperative characteristics among each procedure. Then, multivariate analyses examined if either procedure was associated with worse 30-day postoperative complications or need for reoperation, independent of the statistically significant pre- and intraoperative disparities.
Results
UKAs were performed 14.2 times more commonly than HTOs, and the patients selected for HTO were more likely to be younger, have a lower BMI, have the healthiest ASA Class score, and less likely to have hypertension requiring medication (p < 0.001). HTOs took 17.5% longer to perform and had a longer average length of stay (p < 0.001), while UKAs were more likely to be performed out-patient (p < 0.001). HTOs also had higher rates of serious complications (p = 0.02), overall complications (p = 0.004), and need for reoperation (p = 0.004). Multivariate modelling demonstrated that procedure type was not a predictor of serious complications, but the use of HTO was significantly associated with any complications (odds ratio = 3.63, p = 0.001) and need for reoperation (3.21, p = 0.029).
Conclusion
Although healthier patients were selected for HTOs, UKAs were found to have a lower risk of complications and immediate reoperation. Additionally, UKAs had the advantage of lower operative burden, shorter length of stay, and a higher efficacy in outpatient settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis affects more than 30 million people in the United States and has been recognized as a leading cause of disability [1,2,3]. Although osteoarthritis may be treated initially with nonoperative management, progressive articular degeneration of weight bearing joints often requires surgical intervention [3]. As the knee is commonly involved and incidence is increasing, total knee arthroplasty (TKA) has become one of the most popular procedures and is considered the definitive treatment in geriatric patients [4]. However, a significant portion of osteoarthritis is diagnosed in patients under the age of 55, where greater activity and mobility demands make them less optimal candidates for total arthroplasty and other surgical management must be considered [5, 6].
Unicompartmental knee arthroplasty (UKA) and high tibial osteotomy (HTO) are other common alternatives to surgical management for osteoarthritis of the knee [4]. In comparison to TKA, UKA has been associated with a decreased intraoperative time, hospital stay, blood loss, and increased return-to-sport and physical activity [4, 7]. HTO similarly offers high levels of activity and preserves natural joint mechanics for up to 73% at 10 years [8]. The ability to return to sport and tolerate increased physical activity make both procedures appealing to younger patients, but there is considerable controversy on which procedure is preferred [9]. Patient selection based on age and BMI are often proposed in review studies, but previous evidence is suspected to be poor and it is not clearly understood if these recommendations have guided practice in the past decade [9, 10]. Some studies have also examined postoperative outcomes, but inconsistent patient allocation and a lack of multivariate analyses that control for pre- and intraoperative differences have yielded limited findings [10, 11]. This is in addition to the fact that little work has been conducted on patients under the age of 55, who are likely to have different risk factors and comorbidities than the geriatric population [5, 6].
This study leveraged the data of more than 9 million patients in the American College of Surgeons’ National Surgical Quality Improvement Program registry from 2011 to 2021 to explore primary osteoarthritis in young people [12]. We sought to examine the relative rates of usage between HTO and UKA and if one procedure had favorable 30-day postoperative complication and reoperation rates when pre- and intraoperative differences were accounted for. It was hypothesized that UKA would be utilized more frequently and have better postoperative complication and reoperation rates in comparison to HTO.
Methods
This study utilized a retrospective review of the ACS NSQIP database to identify differences in preoperative and intraoperative characteristics in young patients with primary osteoarthritis undergoing a UKA or HTO. Then, a multivariate analysis was performed to examine if either procedure was associated with worse postoperative complication and reoperation rates, independent of the pre- and intraoperative disparities.
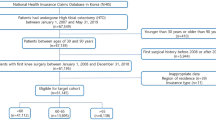
All patients with primary osteoarthritis of the knee were identified using ICD-9 (715.16) and ICD-10 (M17.0, M17.1, M17.11, and M17.12) codes. Age was restricted to ≤ 55 years, and only UKA (CPT = 27446) (n = 2165) and high tibial osteotomy (CPT = 27457, 27455, 27709, and 27705) (n = 153) procedures were included in the final analysis as shown in Fig. 1.
For each procedure, preoperative demographics of sex and age were directly reported, and BMI was calculated from the database. As this patient population is reported to be relatively active, only the lowest American Society of Anesthesiologists (ASA) status classification of “Nondisturbed” was considered. Additionally, prevalence of diabetes mellitus, functional independence, clean wound site classification, hypertension requiring medication, chronic obstructive pulmonary disease, dyspnea, smoking status, and dialysis status were included in the study.
To explore intraoperative differences between procedures, the percent performed with general anesthesia, operative duration (minutes), average length of hospital stay (days), and the percent of procedures performed out-patient was collected.
This study examined serious complications, any complications, and need for reoperation following complication. Serious complications included the need for a ventilator for greater than 48 h, unplanned intubation, stroke, pulmonary embolism, cardiac arrest requiring CPR, myocardial infarction, acute renal failure, sepsis, septic shock, and unplanned return to operating room. Any complication includes serious complications and wound disruption, surgical site infections at superficial incisions, deep incisions, or in organ spaces, pneumonia, urinary tract infection, need for transfusion, progressive renal insufficiency, and deep vein thrombosis requiring therapy.
Differences in preoperative characteristics, intraoperative characteristics, complication rates, and reoperation rates for HTO and UKA were compared using Mann–Whitney U-Tests and chi-square tests as appropriate. Statistical significance was defined as p < 0.05. Then, to determine if differences in complication and reoperation rates can be explained by the patient characteristics and intraoperative differences, variables with bivariate p-values less than 0.05 were then entered into multivariate models. Additionally, procedure type (HTO vs. UKA) was entered into the model to identify if the surgery was a predictor of postoperative characteristics, independent of the patient selection. Only data with values for each variable were analyzed. All statistical work was conducted in R 4.1.0.
Results
The patients selected for HTO were more likely to be male (73.20% vs. 46.8%, p < 0.001), younger (44.96 vs. 50.09, p < 0.001), and have a lower BMI (32.04 vs. 33.50, p < 0.001) (Table 1). Additionally, HTO patients were also generally healthier, with a higher percentage with a “Nondisturbed” ASA Class (24.18% vs. 5.54%, p < 0.001) and less hypertension requiring medication (22.88% vs. 39.77%, p < 0.001) (Table 2). It was also found that UKA has been utilized far more commonly than HTO from 2011 to 2021 (Fig. 2).
Intraoperative analysis revealed that HTO was performed with general anesthesia nearly twice as much as UKA (90.20% vs. 48.68%, p < 0.001), took 17.5% longer to perform (106 min vs. 91.41 min, p < 0.001), and had a longer average length of stay (1.23 days vs. 1.03 days, p < 0.001). Meanwhile, UKA was more likely to be performed out-patient (53.16% vs. 33.99%, p < 0.001) (Table 3).
Comparison of postoperative characteristics found that HTO had a higher rate of serious complications (3.92% vs. 1.20%, p = 0.02), any complications (7.19% vs. 2.60%, p = 0.004), and need for reoperation (4.20% vs. 1.03%, p = 0.004) (Table 4).
Multivariate modeling demonstrated that serious complications were only predicted by a slight increase in operative duration (odds ratio = 1.01, p = 0.027) with the procedure type having no significant role (Table 5). However, use of the HTO procedure was significantly associated with any complications (odds ratio = 3.63, p = 0.001) (Table 6) and need for reoperation (3.21, p = 0.029) (Table 7), independent of preoperative patient characteristics.
Discussion
As the optimal treatment for osteoarthritis in younger populations remains a point of study (5–6), comparing usage, complication, and revision rates among interventions provides a perspective on short-term disparities between treatments. While previous studies have examined the utilization of HTOs and UKAs in osteoarthritis, few limit the demographics to younger patients, as defined as those with diagnosis and/or intervention before the age of 55 [5, 6]. To our knowledge, this study is the first to leverage 10 years of patient data to examine the utilization, 30-day complication, and 30-day reoperation rates comparing UKA to HTO for the purpose of treating primary osteoarthritis in young patients.
Despite frequent utilization of osteotomies in Asian countries, the usage of HTOs in the United States remains significantly lower than arthroplasty [13,14,15,16,17]. Analysis of US insurance database claims from 2007 to 2011 reported UKA utilization rate to be 14.6 times higher than HTO [13]. Our study finds this trend to be consistent from 2011 to 2021 with UKAs being performed 14.2 times more than HTOs (Fig. 2). Patient characteristics may hold a significant role in this usage disparity. Preferences for HTO over UKA in patients of younger age, lower BMI, and male sex have been previously expressed, which our analysis supports (Table 1) [10]. However, we also found that HTOs were deployed in patients with a mean BMI greater than previously published recommendations of a BMI < 27–30 [18, 19]. Similarly, despite limiting the study cohort to young patients, mean age during HTO was found to 5 years higher than in previous reports [13, 20]. Overall, this analysis of updated data suggests that despite low utilization of HTO, it is being deployed in increasingly diverse settings, possibly due to increased incidence and prevalence of osteoarthritis [21].
Although overall healthier patients were being selected for an HTO rather than a UKA, the HTO was associated with worse complication rates as seen in Table 4. Preoperative characteristics such as ASA class and hypertension are well-studied in retrospective orthopaedic cohorts [20]. This study described a preoperative cohort that is largely similar to previous studies, although 21% fewer HTO members had a “Non-disturbed” ASA designation and 22.4% more HTO patients had hypertension needing medication than a previous patient database examination [20]. It is possible that filtering by procedure and diagnosis of osteoarthritis in this study accounts for these differences, as physical debilitation and hypertension are commonly co-morbid with osteoarthritis [22]. Regardless, bivariate comparison of complications among groups revealed higher rates among HTO patients (Table 4). A systematic review of HTO outcomes found an intraoperative complication rate of 5.5% and a postoperative complication rate of 6.9%, consistent with the 7.19% complication rate found here (Table 4) [23]. In cohorts under the age of 65, 1.54% of UKA procedures reported myocardial infarction, deep joint infection, and pulmonary embolism, comparable to the 1.20% serious complication rate in this study [24].
Multivariate analysis confirmed that HTOs were associated with increased complications. There is a current lack of studies multivariate analysis that examines complications between HTO and UKA, but a systematic review of 559 patients showed that although HTO patients were younger, they experienced less favorable post-operative outcomes [10]. However, this analysis considered patients of all ages, and did not elucidate the effects of age, sex, and significantly different pre- and post-operative factors. Other authors analyzed 362 patients to find that UKA patients had an odds ratio of 2.03 for a good postoperative outcome [25]. Our analysis expands this evidence to 2,318 patients and controlled for the younger age, lower BMI, healthier ASA designation, and lower hypertension rates in the HTO group. This analysis showed a higher chance of any complication following HTO than previously described (odds ratio = 3.63, 95% CI 1.58–7.74) and a higher chance of reoperation within 30 days (odds ratio = 3.21, 95% CI 1.04–8.68). Interestingly, although age is used as an indication for these procedures, it was not independently associated with short-term complications. This supports emerging evidence from smaller studies that increased age is not a significant factor in HTO outcomes [26, 27]. Other studies conflict with this result and find age to predict early conversion to TKA [28], and hence, future study is needed to confirm this finding.
The complexity of each procedure and surgical expertise may play a significant role in the differences in postoperative characteristics. Procedure volume is a well-studied predictor of surgical outcomes across multiple surgical specialties, including arthroplasty [29,30,31]. It has also been studied as an important factor for revisions of TKA, which is a long term outcome following HTO and UKA [32]. The nearly 15 times lower overall utilization of HTOs in the US, a + 4.7% annual growth rate of UKA utilization but -3.9% annual rate of HTO utilization, and increased UKA training during residency and fellowship may lead to disparities in expertise and complication rates between the procedures [13, 33, 34]. Moreover, new technologies have been credited in aiding the adoption of the UKA and lowering complication rates, further skewing UKA procedure complication rates and longevity over HTO [35, 36].
Health system cost and utility for the patient between UKA and HTO are also often discussed in decisions to offer one procedure over the other [37]. UKA has been noted to be more cost-effective for care systems due to decreased preoperative burden [38]. The lower operation time, shorter length of stay, and lower use of general anesthesia with UKA support this calculation (Table 3). A statistically significantly larger percentage of UKAs were also performed outpatient from 2011 to 2021. Outpatient procedures have been shown to have similar safety [39], greater satisfaction [40], and have been generally proposed as a more economically efficient procedure [41]. Moreover, while patient cost varies greatly by location, outpatient arthroplasty surgery does have some evidence of lower costs for patients [42]. Overall, determining cost efficiency needs future work, including considerations for the cost of medical education, regional estimates, and stratification insurance type. However, our finding that UKAs procedures are more agile and popular in outpatient settings may have implications on care as outpatient procedures continue to increase [41].
Although the NSQIP database allowed for large-scale analysis, there are several limitations to this study. While the demographic distribution is similar to the surgical population of the US, the data is voluntarily submitted from each participating hospital and may not be a nationally representative sample of procedures and complication rates [43]. Additionally, only a set of 30-day postoperative complication and revision rates were able to be tracked, which excluded patient reported outcomes, and functional outcomes such as range-of-motion where HTO has been proposed to provide advantages [10]. As prior surgical experience and volume can play a significant role in favorable outcomes, future analysis on surgeon experience may shed light on variations in postoperative characteristics. Longer term follow-up would have also provided analysis on revision rate to TKA, which is a frequent surgery in this patient population. As converting to TKA from HTO verses UKA has been linked with different outcomes, this may be an important metric to study in future work [44]. Additionally, despite our strict inclusion/exclusion criteria using both diagnostic codes and procedural codes to specify the patient population, there are several approaches to both HTO and UKA that were not able to be differentiated in this study [45,46,47,48].
Conclusion
Comparing usage, complication, and revision rates among interventions like the high tibial osteotomy and the unicompartmental knee arthroplasty for osteoarthritis in younger populations provides a perspective on short-term disparities between the treatments. This study found that although younger and healthier patients were generally selected for high tibial osteotomies, unicompartmental knee arthroplasties were found to have a lower risk of complications and need for reoperation, possibly due to the higher surgical volume and experience with arthroplasty. In addition, we note that arthroplasty had the advantage of lower operative burden, shorter length of stay, and a higher efficacy in outpatient settings.
Data availability
NSQIP data was accessed through Albany Medical Center institutional account.
References
Vos T, Flaxman AD, Naghavi M et al (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 380:2163–2196. https://doi.org/10.1016/S0140-6736(12)61729-2
Guccione AA, Felson DT, Anderson JJ et al (1994) The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health 84:351–358. https://doi.org/10.2105/ajph.84.3.351
London NJ, Miller LE, Block JE (2011) Clinical and economic consequences of the treatment gap in knee osteoarthritis management. Med Hypotheses 76:887–892. https://doi.org/10.1016/j.mehy.2011.02.044
Khan M, Adili A, Winemaker M, Bhandari M (2018) Management of osteoarthritis of the knee in younger patients. CMAJ 190:E72–E79. https://doi.org/10.1503/cmaj.170696
Bourne RB, Chesworth BM, Davis AM et al (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63. https://doi.org/10.1007/s11999-009-1119-9
Parvizi J, Nunley RM, Berend KR et al (2014) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472:133–137. https://doi.org/10.1007/s11999-013-3229-7
Witjes S, Gouttebarge V, Kuijer PPFM et al (2016) Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med 46:269–292. https://doi.org/10.1007/s40279-015-0421-9
Niinimäki TT, Eskelinen A, Mann BS et al (2012) Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee. J Bone Joint Surg Br 94-B:1517–1521. https://doi.org/10.1302/0301-620X.94B11.29601
Dettoni F, Bonasia DE, Castoldi F et al (2010) High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J 30:131–140
Santoso MB, Wu L (2017) Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J Orthop Surg Res 12:50. https://doi.org/10.1186/s13018-017-0552-9
He M, Zhong X, Li Z et al (2021) Progress in the treatment of knee osteoarthritis with high tibial osteotomy: a systematic review. Syst Rev 10:56. https://doi.org/10.1186/s13643-021-01601-z
Raval MV, Pawlik TM (2018) Practical guide to surgical data sets: national surgical quality improvement program (NSQIP) and Pediatric NSQIP. JAMA Surg 153:764. https://doi.org/10.1001/jamasurg.2018.0486
Nwachukwu BU, McCormick FM, Schairer WW et al (2014) Unicompartmental knee arthroplasty versus high tibial osteotomy: united states practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplasty 29:1586–1589. https://doi.org/10.1016/j.arth.2014.04.002
Niinimäki TT, Eskelinen A, Ohtonen P et al (2012) Incidence of osteotomies around the knee for the treatment of knee osteoarthritis: a 22-year population-based study. Int Orthop 36:1399–1402. https://doi.org/10.1007/s00264-012-1508-7
Domnick C, Garcia P, Raschke MJ et al (2017) Trends and incidences of ligament-surgeries and osteotomies of the knee: an analysis of German inpatient records 2005–2013. Arch Orthop Trauma Surg 137:989–995. https://doi.org/10.1007/s00402-017-2704-0
Kawata M, Sasabuchi Y, Inui H et al (2017) Annual trends in knee arthroplasty and tibial osteotomy: analysis of a national database in Japan. Knee 24:1198–1205. https://doi.org/10.1016/j.knee.2017.06.005
Koh IJ, Kim MW, Kim JH et al (2015) Trends in high tibial osteotomy and knee arthroplasty utilizations and demographics in Korea from 2009 to 2013. J Arthroplasty 30:939–944. https://doi.org/10.1016/j.arth.2015.01.002
Akizuki S, Shibakawa A, Takizawa T et al (2008) The long-term outcome of high tibial osteotomy. J Bone Joint Surg Br 90-B:592–596
Brinkman J-M, Lobenhoffer P, Agneskirchner JD et al (2008) Osteotomies around the knee. J Bone Joint Surg Br 90-B:1548–1557. https://doi.org/10.1302/0301-620X.90B12.21198
Delva ML, Samuel LT, Roth A et al (2021) Contemporary knee osteotomy in the united states: high tibial osteotomy and distal femoral osteotomy have comparable complication rates despite differing demographic profiles. J Knee Surg 34:816–821. https://doi.org/10.1055/s-0039-3400742
Hamood R, Tirosh M, Fallach N et al (2021) Prevalence and incidence of osteoarthritis: a population-based retrospective Cohort Study. J Clin Med. https://doi.org/10.3390/jcm10184282
Lo K, Au M, Ni J, Wen C (2022) Association between hypertension and osteoarthritis: a systematic review and meta-analysis of observational studies. J Orthop Translat 32:12–20. https://doi.org/10.1016/j.jot.2021.05.003
Miltenberg B, Puzzitiello RN, Ruelos VCB et al (2023) Incidence of complications and revision surgery after high tibial osteotomy: a systematic review. Am J Sports Med. https://doi.org/10.1177/03635465221142868
Hansen EN, Ong KL, Lau E et al (2019) Unicondylar knee arthroplasty has fewer complications but higher revision rates than total knee arthroplasty in a study of large united states databases. J Arthroplasty 34:1617–1625. https://doi.org/10.1016/j.arth.2019.04.004
Gandhi R, Ayeni O, Davey JR, Mahomed NN (2009) High tibial osteotomy compared with unicompartmental arthroplasty for the treatment of medial compartment osteoarthritis: a meta-analysis. Curr Orthop Pract 20:164–169. https://doi.org/10.1097/BCO.0b013e3181938d36
Goshima K, Sawaguchi T, Sakagoshi D et al (2017) Age does not affect the clinical and radiological outcomes after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 25:918–923. https://doi.org/10.1007/s00167-015-3847-6
Kuwashima U, Okazaki K, Iwasaki K et al (2019) Patient reported outcomes after high tibial osteotomy show comparable results at different ages in the mid-term to long-term follow-up. J Orthop Sci 24:855–860. https://doi.org/10.1016/j.jos.2018.12.022
Keenan OJF, Clement ND, Nutton R, Keating JF (2019) Older age and female gender are independent predictors of early conversion to total knee arthroplasty after high tibial osteotomy. Knee 26:207–212. https://doi.org/10.1016/j.knee.2018.11.008
Lau RL, Perruccio AV, Gandhi R, Mahomed NN (2012) The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Disord 13:250. https://doi.org/10.1186/1471-2474-13-250
Peterson ED (2004) Procedural volume as a marker of quality for CABG surgery. JAMA 291:195. https://doi.org/10.1001/jama.291.2.195
Schrag D (2000) Influence of hospital procedure volume on outcomes following surgery for colon cancer. JAMA 284:3028. https://doi.org/10.1001/jama.284.23.3028
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg 83:45–49. https://doi.org/10.1302/0301-620X.83B1.10871
Carender CN, Duchman KR, Shamrock AG et al (2023) Unicompartmental knee arthroplasty utilization among early career surgeons: an evaluation of the american board of orthopaedic surgery part-ii database. J Knee Surg 36:759–766. https://doi.org/10.1055/s-0042-1742648
Jeon YS, Ahn CH, Kim M-K (2017) Comparison of HTO with articular cartilage surgery and UKA in unicompartmental OA. J Orthop Surg 25:230949901668409. https://doi.org/10.1177/2309499016684092
Argenson J-NA, Komistek RD, Aubaniac J-M et al (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty 17:1049–1054. https://doi.org/10.1054/arth.2002.34527
Sun Y, Liu W, Hou J et al (2021) Does robotic-assisted unicompartmental knee arthroplasty have lower complication and revision rates than the conventional procedure? A systematic review and meta-analysis. BMJ Open 11:e044778. https://doi.org/10.1136/bmjopen-2020-044778
Konopka JF, Gomoll AH, Thornhill TS et al (2015) The cost-effectiveness of surgical treatment of medial unicompartmental knee osteoarthritis in younger patients. J Bone Joint Surg 97:807–817. https://doi.org/10.2106/JBJS.N.00925
Nwachukwu BU, Hamid KS, Bozic KJ (2013) Measuring value in orthopaedic surgery. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.M.00067
Bovonratwet P, Ondeck NT, Tyagi V et al (2017) Outpatient and inpatient unicompartmental knee arthroplasty procedures have similar short-term complication profiles. J Arthroplasty 32:2935–2940. https://doi.org/10.1016/j.arth.2017.05.018
Crawford ZT, Southam B, Matar R et al (2020) A nomogram for predicting 30-day mortality in elderly patients undergoing hemiarthroplasty for femoral neck fractures. Geriatr Orthop Surg Rehabil 11:2151459320960087. https://doi.org/10.1177/2151459320960087
Munnich EL, Parente ST (2014) Procedures take less time at ambulatory surgery centers, keeping costs down and ability to meet demand up. Health Aff 33:764–769. https://doi.org/10.1377/hlthaff.2013.1281
Scully RD, Kappa JE, Melvin JS (2020) “Outpatient”—same-calendar-day discharge hip and knee arthroplasty. J Am Acad Orthop Surg 28:e900–e909. https://doi.org/10.5435/JAAOS-D-19-00778
Participant Use File: ACS NSQIP User Guide. In: American College of Surgeons National Surgical Quality Improvement Program. https://www.facs.org/media/yaol5yoj/nsqip_puf_userguide_2020.pdf
Shen G, Shen D, Fang Y et al (2022) Clinical outcomes of revision total knee arthroplasty after high tibial osteotomy and unicompartmental knee arthroplasty: a systematic review and meta-analysis. Orthop Surg 14:1549–1557. https://doi.org/10.1111/os.13311
Koyonos L, Slenker N, Cohen S (2012) Complications in brief: osteotomy for lower extremity malalignment. Clin Orthop Relat Res 470:3630–3636. https://doi.org/10.1007/s11999-012-2392-6
Kim TK, Mittal A, Meshram P et al (2021) Evidence-based surgical technique for medial unicompartmental knee arthroplasty. Knee Surg Relat Res 33:2. https://doi.org/10.1186/s43019-020-00084-x
Fuller RM, Wicker DI, Getman GW et al (2021) A medial subvastus approach for lateral unicompartmental knee arthroplasty: technique description and early outcome results. Arthroplast Today 9:129–133. https://doi.org/10.1016/j.artd.2021.04.013
Lee DC, Byun SJ (2012) high tibial osteotomy. Knee Surg Relat Res 24:61–69. https://doi.org/10.5792/ksrr.2012.24.2.61
Funding
The authors did not receive support from any organization for the submitted work. DO declares shareholder status in ROM Tech, is a committee member in AAOS, and is a board member in NYSSOS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors did not receive support from any organization for the submitted work. DO declares shareholder status in ROM Tech, is a committee member in AAOS, and is a board member in NYSSOS.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Debopadhaya, S., Acosta, E. & Ortiz, D. Trends and outcomes in the surgical management of young adults with knee osteoarthritis using high tibial osteotomy and unicompartmental knee arthroplasty. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05362-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05362-x