Abstract
Purpose
Total knee arthroplasty (TKA) designs continuously evolve with the aim of improving patient outcomes. The purpose of the current study was to compare clinical and patient-reported outcome (PRO) results of a new TKA implant to its predecessor. The hypothesis of this study was that joint awareness and range of motion (ROM) of the newer design would be better than the classic design.
Methods
One hundred patients undergoing TKA using the newer design (Attune®) were matched by age and gender to 200 patients with the classic design (LCS®). All patients underwent computer-navigated (Vector Vision, Brain-Lab, Germany) primary TKA by the same surgeon using the same technique. Data (FJS-12, WOMAC and ROM) were collected preoperatively and at 12 months follow-up at our implant registry.
Results
Compared to preoperative scores, FJS-12, WOMAC and ROM improved significantly at 12 months follow-up. In the Attune group, mean FJS-12 and WOMAC at follow-up were 67.6 (SD 27.8) and 14.8 (SD 14.9) respectively, compared to 70.8 (SD 33.8) and 15 (SD 17.9) in the LCS group. Mean postoperative ROM was similar in both groups (Attune 120°, range 90°–140°, SD 10.4 and LCS 120°, range 85°–140°, SD 10.3).
Conclusion
The newer TKA and the predecessor design achieved comparable joint awareness, WOMAC scores and ROM at 1-year follow-up. The benefits expected of the newer design could not be observed in early clinical and PROs. The clinical relevance of this study is that it questions the importance of implant design as the single most important factor for patient outcomes.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In an attempt to address and improve patient outcomes after TKA, manufacturers continuously develop new implants and modify the designs of their previous products. In 2013, DePuy Synthes introduced a new prosthesis design “Attune”. The most notable difference in the cruciate retaining (CR) version compared to the LCS features a gradually reducing femoral radius. Thereby, it is supposed to create a better transition during knee bending and to provide greater mid-flexion stability by increasing the conformity between the femoral component and insert while reducing unnatural sliding of the femur on the tibia. Furthermore, the femoral component profile was reduced and the trochlear groove adjusted to better resemble the native knee with the intention of improving patellar tracking and reducing anterior knee pain [1]. The Attune is available in ten femoral and tibial component sizes, plus four narrow femoral sizes, to better reproduce the variable native anatomy and reduce component overhang. So far, little data has been published comparing clinical and PROs of the Attune to a predecessor. No study has until now compared the Attune CR to the LCS Complete CR. To determine effective improvement and real value of new implant designs, it is essential to compare clinical and PROs with established standard implants. The promised benefits of newer implants have to be proven and only a better patient outcome can be considered real improvement. Therefore, the aim of this study was to compare clinical and PROs of the Attune CR to the LCS CR implant, as well as to evaluate whether differences exist in favor of the newer design and whether this would lead to increased ability to forget the operated knee than the older design. It was hypothesized that joint awareness and range of motion (ROM) of the newer design would be better than the older one.
Materials and methods
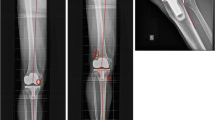
All patients meeting our inclusion criteria who had undergone computer navigated primary TKA from 2012 to 2017 were considered for the study. From 2001 on, the LCS complete knee system was the standard CR implant used at our institute. In 2013 the Attune CR was introduced and replaced the LCS as standard CR implant. Inclusion criteria were: computer navigated (VectorVision, Brain-Lab, Munich, Germany, CT-free, optoelectronic, passive marker navigation system) primary TKA using a cemented prosthesis with CR-design (Attune® or LCS® complete knee system, both DePuy Synthes, Warsaw, Indiana, USA), implanted by the same surgeon, using the same surgical ligament balancing technique and approach; comprehensive clinical records as well as completed patient-reported outcome measures (PROs) at 1-year follow-up. Revision was an exclusion criterion (two Attune knees had to be manipulated under anaesthesia due to arthrofibrosis). A patient flowchart on study inclusion is given in Fig. 1. One hundred Attune implants were matched with 200 LCS complete implants by age and gender. A standard medial parapatellar approach was used in all patients. Using navigation to position the cutting blocks no extra- or intramedullary resection guides were necessary. As these differ for the Attune and the LCS in standard instrumentation they might have been a confounder. All implants were fully cemented using third generation cementing technique. No patella resurfacing was done in either group. Uniform pain relief protocol was used in all patients postoperatively. Rehabilitation for all patients consisted of continuous passive motion in the hospital, ROM exercises instructed by physiotherapists and the use of two crutches for 6 weeks with full weight bearing as tolerated. Patient data were collected preoperatively and 12 months postoperatively in a prospective fashion. PRO was evaluated using the FJS-12 [4] and the WOMAC scores [5]. Knee joint ROM was measured with a goniometer by a trained study nurse. In the interest of greater clarity and clinical relevance, ROM data were presented according to international consensus on the definition and classification of fibrosis of the knee joint [11].
The study design was a retrospective analysis of data available from our TKA registry. Approval was obtained from the local ethics committee (Ethikkommission Ostschweiz, Project ID 2018-00927). Informed consent was obtained from all individual participants included in the study.
Statistical analysis
Descriptive statistics included means, standard deviations, ranges and proportions. Comparative statistics included unpaired t tests and Chi square tests (Fisher exact test was alternatively applied where appropriate). The confidence level for rejecting null hypotheses was set at 95% (p value < 0.05). All statistical analyses were performed using R (R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/). Matching was performed using MatchIt package. Power analysis revealed that 84 patients per group would be necessary to reach 80% power for MCID of 13 points for FJS-12, given an SD of 30 points. Therefore, the number of 100 study patients vs. 200 matched controls was considered sufficient.
Results
Mean values and standard deviations of gender, age and BMI as well as pre- and postoperative FJS-12 and WOMAC are listed in Tables 1 and 2. As far as demographic data is concerned there were no significant differences with respect to age, sex and side. Preoperatively, there was no significant difference between the Attune and LCS with respect to the FJS-12 (mean ± SD; 13.7 ± 11 vs. 16.7 ± 14; n.s.) and WOMAC (mean ± SD; 51.4 ± 15.3 vs. 50.2 ± 19.3; n.s.) scores. In both groups, FJS-12 and WOMAC improved significantly at 1-year follow-up compared to preoperatively. The FJS-12 postoperatively was slightly better in the LCS group but the difference was not statistically significant. Postoperatively, the WOMAC score improved as well, but there was no statistical difference between the groups. Pre- and postoperative average flexion was similar in both groups (Table 3). There was no significant improvement for either group at follow-up. Preoperative extension deficit improved significantly postoperatively in both groups, but was comparable between implants.
Discussion
The most important finding of the present study was that the newer TKA design achieved comparable, but not significantly better clinical and PROs compared to its predecessor. Overall, no significant differences between the two implants were found at 1 year follow-up. This is an important finding because of the human tendency to assume that “newer is better”, also when choosing the “right” implant for the patient. The expectation for new technology is that it should provide a better outcome than what is already available. However, there are reports about new prosthetic designs being equal to predecessor designs [13] or even leading to worse outcomes [2, 17]. Historically, implant survival is the preferred method for evaluating and comparing the success of implant designs. In recent joint registry reports, survival rates with the Attune have been reported as excellent and better than average. In the 2017 Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) and the National Joint Registry (NJR) for England, Wales, Northern Ireland and the Isle of Man, revision rates of 0.6% and 0.3% at 1 year for the Attune were lower compared to the LCS CR; the estimated cumulative revision rate of the overall class of cemented TKR was 1.0% at 1 year in the AOANJRR and 0.4% in the NJR. The 2016 New Zealand Joint Registry (NZOAJR) showed slightly higher yearly revision rates for the Attune compared to the LCS (0.5 vs. 0.6%).
However, such survival studies can be misleading, as patients with unsatisfactory results after TKA can be unable or unwilling to undergo revision surgery. Therefore, parameters such as any-cause revision rate alone are insufficient to provide complete and accurate assessments of outcome after joint surgery. Recently, a gradual shift to include the patients’ perspectives in outcome measurements has taken place, and PRO measures are becoming a cornerstone of outcome assessment after TKA [9]. Validated PRO measures which include factors such as pain, function in activities of daily life, stiffness, or joint awareness have become available. Joint awareness, or the ability of patients to forget about their joint arthroplasty in everyday life or even during recreational activities, is a rather new dimension of PRO and can be measured with the FJS-12. Based on the premise that in general, one is not aware of a healthy joint during usual activities of daily life, this lack of awareness of the normal healthy joint, the forgotten joint, is considered the benchmark in evaluating postoperative results. This state of the forgotten joint rules out any substantial subjective impairments such as pain, instability, or stiffness and also integrates variables such as patient`s expectations, activity levels, and psychosocial factors [4]. Compared to other PRO measures, the FJS-12 showed considerably less ceiling effect, indicating its superiority in terms of discriminatory power [3, 7, 8, 16, 19,20,21, 23]. Another advantage of the FJS-12 in clinical routine is that it is much faster to complete compared to others. This is the first study to assess joint awareness with the FJS-12 after implanting the Attune. A slight but not statistically relevant difference in the FJS-12 at 12 months postoperatively with a lower (worse) score for the Attune compared to the LCS (66 vs. 71) was shown. Compared to the mean FJS-12 score of 50 for the overall class of LCS in patients at our registry, higher FJS-12 scores were observed in the current study where results from a single surgeon were analysed [4]. However, the FJS-12 values were lower than in healthy subjects of the same age in the validation study (82.5) [4].
So far, little data have been published comparing clinical and PRO results of the Attune vs. a predecessor design. The available studies show results comparable to ours with no difference in PROs and patient satisfaction between implants, but slightly better postoperative flexion in the Attune groups in two studies. In a matched-pair analysis of 200 patients comparing the Attune PS to the PFC Sigma PS, both cemented fixed bearing, over a 2-year period, comparable Knee Society Scores (KSS) (Attune PS 169 ± 32; PFC Sigma PS 165 ± 35) and Oxford Knee Scores (Attune PS 38; PFC Sigma PS 36) were reported [10]. Another study compared a cohort of 728 patients who received the Attune PS (both rotating platform, n = 358 and fixed bearing, n = 370) to a cohort of 1165 patients who received the PFC Sigma PS at 1-year follow-up. The Sigma cohort showed significantly better KSS (93.0 vs. 90.4; p < 0.0001) compared to the Attune [15]. A third paper reported on results of a matched pair analysis of 200 patients comparing the Attune PS to the PFC Sigma PS, both cemented, but fixed or mobile bearing, over a 2-year period [18]. They, as well, reported comparable pre- and postoperative KSS for pain and function between groups with a significant improvement at 2-year follow-up (Attune PS function/pain (mean ± SD) vs. Sigma PFC PS function/pain (mean ± SD); 92 ± 9/89 ± 15 vs. 93 ± 8/89 ± 11).
In this study, similar ROM within groups as well as within pre- and postoperative follow-ups, with 118° and 116° flexion at 12 months for the Attune and LCS implants were shown. In the study published by Indelli et al. [10], the average ROM at final follow-up differed significantly with 123° (range 98°–135°) for the Attune PS cohort and 115° (range 97°–132°) for the PFC Sigma PS cohort. However, the authors question the clinical relevance of 8° of flexion between implants. The patients’ ability to perceive this relatively small difference in flexion has been discussed controversially [12, 22]. Martin et al. [15] also published significantly better flexion at 1 year follow-up in the Attune PS group compared to the PFC Sigma PS group (126.52 ± 8.19 vs. 124.93 ± 929, p < 0.001). Ranawat et al. [18] showed comparable ROM between groups without significant improvement at follow-up (mean ± SD; Attune PS 119 ± 9 vs. PFC Sigma PS 117 ± 9).
Even if newer designs like the Attune have specific theoretical advantages, an improvement in PRO has not been shown to date, in the published literature or in this study. The results of this study question the importance of implant design as being the single most important factor proposed by the industry when placing new models on the market. If the principles of TKA are constant and factors like the surgeon, implantation technique, surgical approach, post-op pain management, rehabilitation and patient characteristics like BMI, age and sex are balanced, the implant design might be of less importance in determining the PROs after TKA. The search for factors which need to be improved to reach the target of universal patient satisfaction and the completely forgotten joint after TKA has to go on. Is it conceivable that ready-made implants offer no space for further improvement and instead custom-made implants are the solution? It could be that only custom-made implants will be able to reproduce the anatomy sufficiently to cover the complexity of the anthropometric variants and to reflect them without surgical compromise [14]. Or are other factors like knee alignment, joint line orientation as well as patient factors like expectations more important than implant design?
Surgeons make important decisions when choosing the implants to be used and these decisions carry consequences for their patients’ health. The clinical relevance of this study lies in providing first results concerning joint awareness for a new implant design. These results can help in decision-making when choosing the best implant for the patient.
The authors note several limitations of the current analysis. First, the study is a retrospective review of patients, and therefore suffers the inherent limitations of retrospective analysis.
However, to provide comparability, patients were recruited from a single center, operated by the same surgeon and treated under standardised protocols. Further limitations include short-term follow-up. However, it has been shown [6], most literature on PRO consider 1 year postoperative results as the end point for measuring patients’ improvement after TKA. Furthermore, there was a selection bias. Especially in the initial phase, patients with better ROM and less varus or valgus deformity received the newer implant, whereas more complex cases were addressed with the older prosthesis. In addition, even for an experienced knee surgeon, a certain learning curve should be expected when introducing a new implant.
Conclusion
Both the newer TKA and the predecessor design achieved comparable joint awareness, WOMAC scores and range of motion at 1 year follow-up. The expected benefits of the newer design could not be observed in early clinical and PROs. The clinical relevance of this study is that it questions the importance of implant design as the single most important factor in improving patient outcome.
References
Amis AA, Senavongse W, Bull AMJ (2006) Patellofemoral kinematics during knee flexion-extension: an in vitro study. J Orthop Res 24(12):2201–2211
Anand R, Graves SE, de Steiger RN, Davidson DC, Ryan P et al (2011) What is the benefit of introducing new hip and knee prostheses? J Bone Jt Surg 3:51–54
Baumann F, Ernstberger T, Loibl M, Zeman F, Nerlich M et al (2016) Validation of the German Forgotten Joint Score (G-FJS) according to the COSMIN checklist: does a reduction in joint awareness indicate clinical improvement after arthroplasty of the knee? Arch Orthop Trauma Surg 136(2):257–264
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27(3):430–436
Bellamy N, Buchanan WW (1986) A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol 5(2):231–241
Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R et al (2004) Patient quality of life during the 12 months following joint replacement surgery. Arthritis Care Res 51:100–109
Hamilton DF, Giesinger JM, MacDonald DJ, Simpson AHRW, Howie CR et al (2016) Responsiveness and ceiling effects of the Forgotten Joint Score-12 following total hip arthroplasty. Bone Jt Res 5(3):87–91
Hamilton DF, Loth FL, Giesinger JM, Giesinger K, MacDonald DJ et al (2017) Validation of the English language Forgotten Joint Score-12 as an outcome measure for total hip and knee arthroplasty in a British population. Bone Jt J 99(2):218–224
Hossain FS, Konan S, Patel S, Rodriguez-Merchan EC, Haddad FS (2015) The assessment of outcome after total knee arthroplasty: are we there yet? Bone Jt J 97(1):3–9
Indelli PF, Pipino G, Johnson P, Graceffa A, Marcucci M (2016) Posterior-stabilized total knee arthroplasty: a matched pair analysis of a classic and its evolutional design. Arthroplasty Today 2:193–198
Kalson NS, Borthwick LA, Mann DA, Deehan DJ, Lewis P et al (2016) International consensus on the definition and classification of fibrosis of the knee joint. Bone Jt J 98(11):1479–1488
Kim YH, Park JW, Kim JS (2012) High-flexion total knee arthroplasty: survivorship and prevalence of osteolysis: results after a minimum of ten years of follow-up. J Bone Jt Surg 94(15):1378–1384
Ko YB, Jang EC, Park SM, Kim SH, Kwak YH et al (2015) No difference in clinical and radiologic outcomes after total knee arthroplasty with a new ultra-congruent mobile bearing system and rotating platform mobile bearing systems after minimum 5-year follow-up. J Arthroplasty 30:379–383
Lampart M, Behrend H, Moser LB, Hirschmann MT (2018) Due to great variability fixed HKS angle for alignment of the distal cut leads to a significant error in coronal TKA orientation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5041-0
Martin JR, Jennings JM, Watters TS, Levy DL, McNabb DC et al (2017) Femoral implant design modification decreases the incidence of patellar crepitus in Total knee arthroplasty. J Arthroplasty 32:1310–1313
Matsumoto M, Baba T, Homma Y, Kobayashi H, Ochi H et al (2015) Validation study of the Forgotten Joint Score-12 as a universal patient-reported outcome measure. Eur J Orthop Surg Traumatol 25(7):1141–1145
Peltola M, Malmivaara A, Paavola M (2012) Introducing a knee endoprosthesis model increases risk of early revision surgery. Clin Orthop Relat Res 470(6):1711–1717
Ranawat CS, White PB, West S, Ranawat AS (2017) Clinical and radiographic results of attune and PFC sigma knee designs at 2-year follow-up: a prospective matched-pair analysis. J Arthroplasty 32(2):431–436
Shadid MB, Vinken NS, Marting LN, Wolterbeek N (2016) The Dutch version of the Forgotten Joint Score: test-retesting reliability and validation. Acta Orthop Belg 82(1):112–118
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2013) Joint awareness in different types of knee arthroplasty evaluated with the Forgotten Joint Score. J Arthroplasty 29(1):48–51
Thompson SM, Salmon LJ, Webb JM, Pinczewski LA, Roe JP (2015) Construct validity and test re-test reliability of the Forgotten Joint Score. J Arthroplasty 30(11):1902–1905
Thomsen MG, Husted H, Otte KS, Holm G, Troelsen A (2013) Do patients care about higher flexion in total knee arthroplasty? A randomized, controlled, double-blinded trial. BMC Musculoskelet Disord 14:127
Vanden ETA, Schwab BPE, Cornu JPFO (2016) Joint awareness in osteoarthritis of the hip and knee evaluated with the ‘Forgotten Joint’ Score before and after joint replacement. Knee Surg Sports Traumatol Arthrosc 24(10):3346–3351
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was obtained from the local ethics committee (Ethikkommission Ostschweiz, Project ID 2018-00927).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Behrend, H., Zdravkovic, V., Bösch, M. et al. No difference in joint awareness after TKA: a matched-pair analysis of a classic implant and its evolutional design. Knee Surg Sports Traumatol Arthrosc 27, 2124–2129 (2019). https://doi.org/10.1007/s00167-019-05407-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05407-4