Abstract
Background
Patients who sustain osteoporotic fractures have excessive mortality compared to age-matched controls, which is most pronounced within the first 6 months postfracture. However, the timing and cause of death in the first 3 months after sustaining a fracture are unclear.
Questions/purposes
We therefore evaluated and compared the timing and cause of death in patients who sustained a pelvic, proximal femoral, spinal, or proximal humeral fracture 30 and 90 days after fracture.
Methods
From medical records, we recorded age at time of fracture, sex, fracture site, comorbidities, date of death, and cause of death of 1630 patients with 1630 fractures admitted to our department between 2001 and 2007. The median age at the time of fracture was 83 years and 89% of the patients were women.
Results
Fifty-eight patients died within 30 days after fracture (3.6%), and 122 patients (7.5%) died within 90 days after fracture. Cardiovascular causes of death were most frequent in all fracture groups. Patients who suffered from spinal fractures died earlier within 30 days after fracture than patients who suffered from other types of fractures.
Conclusions
This shows the severity and impact of a spinal injury compared to other typical fragility fractures.
Level of Evidence
Level II, prognostic study. See Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients suffering from osteoporotic fractures after low-impact trauma are at high risk for early death compared to age-matched controls. Men and women have an increased standardized mortality ratio (SMR) for proximal femur fractures (SMR 3.51 and 2.43), vertebral fractures (SMR 2.21 and 1.82), other major fractures such as pelvic, distal femur, and proximal tibia (SMR 1.70 and 1.65), and minor fractures such as distal arm and leg fractures (SMR 1.33 and 1.42) [1]. This increased mortality risk lasts until 5 to 10 years after fracture [2, 14, 16] but is most pronounced in the first 3 to 6 months after sustaining an osteoporotic fracture [1, 14]. The reason for this increased mortality risk is poorly understood [2, 5, 6, 14, 16]. The most used outcome parameters describing short-term mortality are in-hospital and 30-day mortality [10, 11]. Due to differences in length of stay among countries and regions, it is difficult to compare in-hospital mortality [8, 13].
Causes of death after fractures in the elderly have been investigated, specifically for proximal femur fractures, but only in patients who died more than 1 year after fracture [3, 9] or for patients with hip arthroplasty who died 30 days after sustaining a fracture [17]. No distinction has been made in cause of death between early (within 3 months after fracture) and late deaths (> 1 year after fracture).
We therefore (1) evaluated the short-term (30- and 90-day) mortality after proximal femoral, spinal, pelvic, and proximal humeral fracture; (2) evaluated the timing of death for different fracture sites in the first 3 months after fracture; and (3) compared the causes of death among the different fracture sites in the first 3 months after fracture.
Patients and Methods
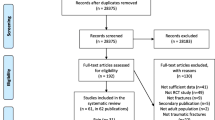
We retrospectively reviewed the charts of all 2384 patients aged 65 years and older who were admitted to our department between 2001 and 2007 with 2477 fractures of the proximal humerus, spine, proximal femur, or pelvis. We excluded 34 fractures in 34 patients with a malignant tumor who were at risk for having a fracture due to malignancy, 187 fractures due to high-energy trauma in 185 patients, 89 fractures in 89 nonresident patients, 279 fractures in 276 patients transferred from other hospitals, and 84 fractures in 83 patients with missing documentation. We also excluded 174 fractures in 87 patients who sustained a subsequent fracture. Patients with a subsequent fracture are known to have a higher mortality rate than patients who suffer one fracture (SMR 2.21 versus 1.41 in women and SMR 3.53 versus 1.82 in men) [2]. These exclusions left 1630 fractures in 1630 patients to be analyzed. The median age at the time of fracture was 83 years (interquartile range, 11.0 years), and 1448 (89%) patients were female. Fourteen percent of fractures were at the pelvis, 68% at the proximal femur, 8% at the spine, and 10% at the proximal humerus. The 30-day mortality rate was 3.6% (58 patients) and the 90-day mortality rate was 7.5% (122 patients) (Table 1). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Ethical approval for this study was obtained from the local ethics committee.
All hip fractures were treated operatively with a nail for intertrochanteric fractures or hemiarthroplasty for femoral neck fractures. The pelvic ring fractures were treated nonoperatively with pain treatment and immediate mobilization. Spinal fractures were only treated operatively in case of instability. Humeral fractures were treated nonoperatively or operatively depending on the nature of the fracture.
All patients were mobilized immediately with full weightbearing as tolerated. The antithrombotic prevention was performed with subcutaneous low-molecular-weight heparin and compression stockings.
Two of us (ISL, CR) extracted the following information from the electronic medical record (KIS PowerChart®; Cerner, Idstein, Germany): age at time of fracture, patient’s demographics, fracture site, comorbidities, date of death, and cause of death. Comorbidities were assessed according to the Charlson Comorbidity Index (CCI) [7], an index that predicts the 1-year mortality of patients with ranges of comorbid conditions. Date of death and cause of death were obtained from the National Institute for Clinical Epidemiology using the ICD-10 [19]. This institute is the official death certificate registry from the legal authorities in Austria.
All 122 patients who died within the first 90 days after fracture were included for statistical analysis. Causes of death were classified into five groups: cardiovascular, infection, respiratory, malignancy, and other (Table 2). The cardiovascular group included patients who died from myocardial infarction (ICD I25), heart failure (ICD I11), cerebrovascular disease (ICD I60–I69), and intestinal infarction (ICD K55). Patients who died from sepsis (ICD A41) or pneumonia (ICD J12–J18) were placed in the infection group. The respiratory group included patients who died from pulmonary embolism (ICD I26) or respiratory failure (ICD I27 and J43–J44), and the malignancy group included patients who died from any malignancy (ICD C00–C97). Patients were classified in the “other” group if they died from renal failure, multiple-organ failure, or reduced health state. Ultrasound or CT scans were used to diagnose a thromboembolic disease.
The distributions of age, cause of death, and fracture site were tested with the Kolmogorov-Smirnov test and these variables were determined to be nonnormally distributed. Descriptive statistics were presented as frequency, percentage, and median and interquartile range/CI. Mortality rates are presented as percentages. The median survival time was calculated for patients who died within 30 days and 90 days after fracture. The Kaplan-Meier curve and log-rank test were used to compare survival among fracture sites. The Kruskal-Wallis test was used to compare fracture groups to other fracture groups and causes of death to other causes. The chi-square test was used to determine whether the frequencies of causes of death within fracture groups were different. We used the Cox regression for multivariable analysis to determine independent predictors of death and included those factors from the Kruskal-Wallis test with a p value of less than 0.05. SPSS® Version 20.0 (IBM Corp, Armonk, NY, USA) was used for statistical analysis.
Results
Mortality rates at 30 days after fracture were 3.0%, 3.5%, 3.1%, and 3.6% for pelvic, proximal femoral, spinal, and proximal humeral fractures, respectively (Table 1). Ninety days after fracture, the mortality rates were 7.7%, 7.9%, 6.2%, and 4.2%, respectively. With multivariable analysis, we found men were more likely (p = 0.019) to die within 30 days after fracture than women, but age (p = 0.63) and CCI (p = 0.43) had no influence on 30-day mortality among the fracture site groups. The same analysis for death within 90 days after fracture showed an influence of age (p = 0.01) but not sex (p = 0.14) or comorbidities (p = 0.56).
Patients suffering from spinal fractures died earlier within 30 days after fracture than patients who sustained fractures at the other sites (p = 0.005) (Fig. 1). Within 90 days after fracture, there was still a trend (p = 0.48) toward patients with spinal fractures dying earlier (Fig. 2). There were no differences in survival times among the other fracture site groups (Table 2).
A graph shows 30-day Kaplan-Meier curves of the cumulative survival after pelvic, proximal femoral, spinal, and proximal humeral fracture. Patients suffering from spinal fractures died earlier within 30 days after fracture than patients who sustained fractures at the other sites. There were no differences in survival times among the other fracture site groups.
A graph shows 90-day Kaplan-Meier curves of the cumulative survival after pelvic, proximal femoral, spinal, and proximal humeral fracture. Within 90 days after fracture, there was still a trend toward patients with spinal fractures dying earlier. There were no differences in survival times among the other fracture site groups.
We found no differences in the frequencies of causes of death among the fracture site groups at 30 days after fracture (p = 0.62) and 90 days after fracture (p = 0.54). In the proximal femoral fracture group, more cardiovascular deaths were noted at 30 days (p < 0.01) and 90 days (p < 0.01) compared to other causes of death. In the other fracture groups, no major differences regarding cause of death could be found (Table 3). We found six patients died due to a pulmonary embolism whereas one had a pelvic fracture and five sustained a hip fracture. We did not find associations with either fracture type (p = 0.833) or survival time (p = 0.221).
Discussion
Low-impact fractures in the elderly are known to cause an excessive mortality risk compared to age-matched controls [1]. This excessive mortality risk is the most pronounced in the first 3 to 6 months after sustaining a fracture [1, 14], but not much is known about the timing and cause of death in the first 3 months. We therefore evaluated the short-term (30- and 90-day) mortality after proximal femoral, spinal, pelvic, and proximal humeral fracture. We also evaluated the timing of death for different fracture sites and compared the causes of death among the different fracture sites in the first 3 months after fracture.
Our study has some limitations. First, we had small groups of patients who died after pelvic, spinal, and humeral fractures and small numbers of patients with specific causes of death. We classified the causes of death into five fairly broad categories; otherwise, a statistical analysis would have been unreasonable. Second, most of our patients did not have a bone mineral density measurement after sustaining a fracture. Since fractures sustained after high-velocity trauma and those due to malignancy were excluded, only low-impact fractures were evaluated. Given the high percentage of women in our population and the high median age at the time of fracture, it is very likely osteoporosis played an important role in causing the fractures. Third, and probably related to the retrospective setting, we might lack some patient information that would help us to control for potential confounding variables aside from comorbidities. Furthermore, we classified our causes of death into fairly broad categories, which might reflect the clinical daily practice but potentially involves some inaccuracy.
In our population, we found a 30-day mortality rate of 3.0%, 3.6%, 3.1%, and 3.6% for pelvic, proximal femoral, spinal, and proximal humeral fractures, respectively. For proximal femoral fractures, Parvizi et al. [17] reported a similar mortality rate of 2.4% 30 days after fracture. Castronuovo et al. [4] found a 30-day mortality rate of 6.3%, but they did not compare their mortality rate to the literature and did not give an explanation for their high mortality rate.
Ninety-day mortality rates in our population for pelvic, proximal femoral, spinal, and proximal humeral fractures were 7.7%, 8.1%, 6.2%, and 4.1%, respectively. Lee et al. [15] found a mortality rate of 5.6% in men and 2.4% in women 90 days after a spinal fracture. A possible explanation for the lower mortality rate, especially in women, could be due to the fact that those authors included patients 50 years and older. We can assume their study population was healthier and younger than our population. Gronskag et al. [12] reported a 90-day mortality rate of 10% after proximal femoral fractures in women. Faramand et al. [9] reported a 90-day mortality rate of 4.3% after a proximal femoral fracture, which is lower than our mortality rate of 8.1%. The population in the study of Faramand et al. [9] was younger (mean age, 73 years) compared to our study population (mean age, 83 years), which could explain the difference in mortality rate. We could not find 30- and 90-day mortality rates for pelvic and proximal humeral fractures in the literature. Morin et al. [16] and Shortt et al. [18] compared morality between different fracture sites, but only for long-term mortality (1 year). Patients who had spinal fractures died earlier (within 30 days after fracture) than patients who had other types of fractures. Several studies [2, 6, 16] investigated the differences in mortality rates between fracture groups but did not evaluate the difference in timing of death.
We found cardiovascular disease was the most frequent cause of death in every fracture group at 30 and 90 days after fracture, which was also described previously by Cameron et al. [3] and Parvizi et al. [17]. Cameron et al. [3] investigated the cause of death after hip fracture in institutionalized elderly patients and found 44.1% of the patients died from cardiovascular (cardiac and cerebrovascular) causes after 90 days, which is higher than our finding (34%). They also found a higher rate of patients dying from infectious causes (32.2%) than in our proximal femoral fracture population (11%). An explanation for this difference could be that Cameron et al. [3] only investigated the cause of death in institutionalized patients; institutionalized patients are known to have more (cardiovascular) comorbidities than noninstitutionalized patients, which is associated with a higher risk for cardiovascular complications. They also have a higher risk of developing pneumonia than noninstitutionalized patients due to immobilization. We did not assess places of residence, but it is reasonable to assume our population also contained patients who were still living at home, and our population was therefore more mobile than an institutionalized population.
Parvizi et al. [17] studied the relationship between cause and time of death after hip arthroplasties for acute fractures and found almost all patients who died of sudden cardiorespiratory events died within 48 hours postoperatively. They suggested these deaths were attributable to the intraoperative embolization of marrow and fat elements from the bone after cementation. We found patients who died of cardiovascular or respiratory diseases in the proximal femoral fracture site group succumbed after 48 hours but earlier than patients who died of infectious causes. Compared to the results of Parvizi et al. [17], this finding could be due to the difference in operations needing cement.
Cardiovascular causes of death were the most frequently reported in all fracture groups. Furthermore, we found patients who sustained spinal fractures died earlier in comparison to patients who sustained fractures of the pelvis, proximal femur, or proximal humerus within 30 days after fracture. Since we observed no other differences among the fracture groups, we assume a spinal fracture itself is a predictor for early death after fracture. This finding shows the severity of a spinal injury compared to other typical fragility fractures.
References
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633–1650.
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–521.
Cameron ID, Chen JS, March LM, Simpson JM, Cumming RG, Seibel MJ, Sambrook PN. Hip fracture causes excess mortality owing to cardiovascular and infectious disease in institutionalized older people: a prospective 5-year study. J Bone Miner Res. 2010;25:866–872.
Castronuovo E, Pezzotti P, Franzo A, Di Lallo D, Guasticchi G. Early and late mortality in elderly patients after hip fracture: a cohort study using administrative health databases in the Lazio region, Italy. BMC Geriatr. 2011;11:37.
Cauley J, Thompson D, Ensrud K, Scott J, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Clarke A, Rosen R. Length of stay: how short should hospital care be? Eur J Public Health. 2001;11:166–170.
Farahmand BY, Michaelsson K, Ahlbom A, Ljunghall S, Baron JA. Survival after hip fracture. Osteoporos Int. 2005;16:1583–1590.
Fleischman RJ, Adams AL, Hedges JR, Ma OJ, Mullins RJ, Newgard CD. The optimum follow-up period for assessing mortality outcomes in injured older adults. J Am Geriatr Soc. 2010;58:1843–1849.
Gorra AS, Clark DE, Mullins RJ, DeLorenzo MA. Regional variation in hospital mortality and 30-day mortality for injured Medicare patients. World J Surg. 2008;32:954–959.
Gronskag AB, Romundstad P, Forsmo S, Langhammer A, Schei B. Excess mortality after hip fracture among elderly women in Norway: The HUNT study. Osteoporos Int. 2012;23:1807–1811.
Jencks SF, Williams DK, Kay TL. Assessing hospital-associated deaths from discharge data. JAMA. 1988;260:2240–2246.
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B. Mortality after osteoporotic fractures. Osteoporosis Int. 2004;15:38–42.
Lee YK, Jang S, Lee HJ, Park C, Ha YC, Kim DY. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012;23:1859–1865.
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int. 2011;22:2439–2448.
Parvizi J, Ereth MH, Lewallen DG. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg Am. 2004;86:1983–1988.
Shortt N, Robinson C. Mortality after low-energy fractures in patients aged at least 45 years old. J Orthop Trauma. 2005;19:396–400.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available at: http://apps.who.int/classifications/icd10/browse/2010/en. Accessed December 8, 2011.
Acknowledgments
The authors thank Dr. Tobias Roth and Dr. Thomas J. Luger for their intellectual help.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Medical University of Innsbruck, Innsbruck, Austria.
About this article
Cite this article
Liem, I.S., Kammerlander, C., Raas, C. et al. Is There a Difference in Timing and Cause of Death After Fractures in the Elderly?. Clin Orthop Relat Res 471, 2846–2851 (2013). https://doi.org/10.1007/s11999-013-2881-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-2881-2