Abstract
Background
We hypothesized that an entire pedicle screw tract cement augmentation has greater strength than traditional techniques.
Method
Twenty-four fresh frozen calf lumbar spines were randomized into three study groups, each having eight vertebrae: (1) screw cemented after vertebroplasty; (2) fenestrated cemented screw; and (3) cementation of the entire pedicle screw tract. For the right side screws, two pedicle screws were inserted in each vertebra with the standard position in the sagittal plane, whereas the left side screws were placed at a 30° angle craniocaudal plane. From the recorded force–displacement curves, the maximum peak load (failure load) of each screw was determined. The mode of failure was screw stripping at all levels tested.
Results
The pull-out strength for standard screw replacement at the sagittal plane was 1843.3 N, 1707.45 N, and 5365.1 N consecutively. The failure load value in the standard position in the sagittal plane in the cementation of the entire pedicle screw tract group was significantly higher than that in the fenestrated cemented screw group and screw cemented after vertebroplasty (p < 0.001 and p < 0.001, respectively). The standard pedicle screw position in the sagittal plane showed a significant pull-out strength than the others (p < 0.001).
Conclusion
The pull-out strength of the cementation of the entire pedicle screw tract was 2.5 times higher than the others. The pull-out strength of the pedicle screws in malposition obtained the same strength to the standard positions after the augmentation procedure in our study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the increase in life expectancy, the frequency of performing spine surgery also increases in elderly patients [1]. The most important factor for successful spine surgery is the durability of the implant until bone fusion is achieved [2]. However, the strength of the implant alone is not sufficient, and the maximal strength of the bone implant is a requirement [3].
Pedicle screws, which provide successful results in spine surgery, have been reported to have fusion problems on bone screw surface due to osteoporosis in recent years [4, 5]. Weiser et al. recommend that augmentation procedures can be used in patients with low bone mineral density [5].
With regard to augmentation techniques, only two main practices were reported in the literature: cementation via cannulated pedicle screw (fenestrate) and screwed after vertebroplasty [6,7,8,9,10,11,12,13]. Many biomechanical studies have shown that the pull-out strength of pedicle screws significantly increased with cement augmentation [10,11,12,13]. Besides, clinical studies have shown successful results using the cementation technique [14,15,16,17]. Polymethyl methacrylate (PMMA) coating of the femoral stem provides long-term survival due to interdigitation on larger surfaces on hip arthroplasty [17, 18]. The cementation around the pedicle screws can positively affect the stability and pull-out strength due to the large bone cement surface. However, data on the biomechanical effects of cementing around the pedicle screw circumference are not available.
Another factor that defines the stability of the pedicle screws is the axial and sagittal positions of the screws. Costa et al. found that the pull-out resistance was significantly reduced when the screws were placed craniocaudally in the sagittal plane [19]. However, increasing the pull-out strength of the screws in malposition using the augmentation procedure is yet to be investigated.
In this study, we researched two major subjects. One of them; the difference of pull-out strength between standard augmentation technique and cementing around the pedicle screw circumference. The other subject is the effects of pull-out strength in pedicle screws with different directions on the sagittal plane.
Materials and Methods
Specimens
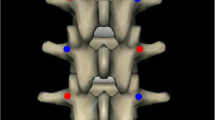
The study was approved by the ethical committee of the Istanbul University Faculty of Medicine. Twenty-four fresh frozen calf lumbar spines were obtained and stripped of unnecessary muscle tissue, ligaments, and joint capsules. Computed tomography scans were performed to evaluate the quality of the vertebrae and exclude vertebrae with any fracture, osteolysis, or deformation. After harvesting, the specimens were sealed in plastic bags and stored at − 20 °C. All vertebrae were randomized into three study groups, each having eight vertebrae: [1] screw cemented after vertebroplasty; [2] fenestrated cemented screw; and [3] cementation of the entire pedicle screw tract (Fig. 1). Each study group had the same number of left and right pedicles instrumented, with the two screw techniques compared in the same vertebra. For the right side (A), the screw with the standard position was inserted in the sagittal plane, whereas the left side screws were placed at a 30° craniocaudal plane (B).
Instrumentation
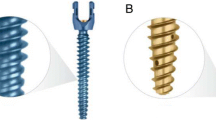
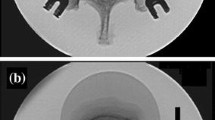
All instrumentations were performed by the same experienced spine surgeon (T.A). Using standard operative techniques, a targeting needle was directed into appropriate pedicles via fluoroscopy (Arcadis® Orbic Mobile X-Ray System, Siemens Medical Solutions USA). A K-wire was placed, and the targeting needle was removed. To simulate the soft spongious structure of the calf spine, a 5-mm drill was used over the K-wire. The 6.5-mm bone tap was placed over the K-wire and threaded into the anterior third of the vertebral body. At the end of the screw tunnel, a cavity was created using the surgical curette (Fig. 1). Standard pedicle screws with an outer diameter of either 6.5 mm, length of 45 mm, fenestrated, polyaxial, and titanium screws were used. The thread design and pitch were the same for all groups. All screws were placed in the sagittal and mediolateral planes with fluoroscopic guidance to ensure correct positioning for each group. In addition, the injected PMMA cement volume was 3 ml for groups 1 and 2, and 4.5 ml for group 3 (Figs. 2, 3). Screw positions were checked to ensure no cortical breakout. The surrounding anatomy was inspected for cement extravasation. Cement leakage into the spinal canal was not observed.
Mechanical Testing
Before mechanical testing, the cement was allowed to harden at room temperature for at least 12 h. The vertebral body was parallel to the testing machine. The fixture was constructed in such a way that the specimens were fixed to the posterior border of the vertebral body, but the pedicle remained completely free (Fig. 4). During the mounting of the specimens, proper alignment of the longitudinal screw axis was ensured with the vertical pulling direction of the testing machine. Pull-out testing was performed in displacement controlled mode with a velocity of 5 mm/min while data were recorded with a sample rate of 10 Hz (Shimadzu Corp., Kyoto, Japan; Autograph AGS-J model universal testing machine). The maximum peak load (failure load) of each screw was determined from the recorded force–displacement curves. The mode of failure was screw stripping at all levels tested.
Statistical Analysis
Statistical analysis was performed using the software SPSS (IBM SPSS Statistics, Version 24.0 for Windows, IBM Corporation, Armonk, New York, USA). The data were tested for normal distribution using the Shapiro–Wilk test Comparisons were performed using one-way analysis of variance, and significance was accepted at p < 0.05 at 95% confidence interval. For comparison among the three groups, Tukey range test was used among post hoc tests. An independent t test was used to compare the result of different angle screw fixations for all groups.
Results
In the biomechanical analysis of pull-out strength, the mean failure load of groups 1A and 1B was 1843.3 N and 1707.45 N, respectively. No significant differences were found between the groups (p = 0.248).
The mean failure load of groups 2A and 2B was 1869.3 N and 1766.97 N, respectively. No significant differences were found between the groups (p = 0.318).
The mean failure load of groups 3A and 3B was 5365.1 N an 4517.96 N, respectively. No significant differences were found between the groups (p = 0.07) (Table 1).
The failure load value in the standard position in the sagittal plane in the cementation of the entire pedicle screw tract group was significantly higher than that in the fenestrated cemented screw group and screw cemented after vertebroplasty (p < 0.001 and p < 0.001, respectively).
However, no statistical difference was found between the fenestrated cemented screw group and screw cemented after the vertebroplasty group (p = 0.981). Group 3 has a significant pull-out strength than the other groups in screws in the 30° craniocaudal plane.
Discussion
Osteoporosis occurs due to the negative effects of bone turnover in advanced ages. Although osteoporosis causes thinning of the cortical bone, the most important bone loss occurs in the spongious bone in the vertebral body. Many screw techniques or augmentations are used to improve the strength of pedicle screws used in spine surgery at an advanced age. The main factor is insufficient pedicle screw integration to the spongious bone. The following is recommended: screws should pass through the anterior cortex, a wide range of screws should be used, screw structure should be changed, and augmentations should be performed to improve screw strength in osteoporotic vertebrae [5,6,7,8,9,10]. Many studies have shown that all these techniques are superior to the standard screw placement. Lorenz et al. found that standard pedicle screws using the augmentation procedure were stiffer than the new-generation pedicle screw [11].
PMMA is the most effective substance for bone-implant integration in orthopedic surgery. Implant integration of bone cement is performed using the compression method, and bone integration is performed using the interdigitation method [15, 16]. The use of pedicle screws with cementation provides successful clinical results [16, 17]. Cementation via cannulated pedicle screw and screwed after vertebroplasty are the most commonly used methods for cementation techniques. Lorenz et al. reported no statistically significant difference between these main methods; however, they emphasized the importance of the amount of cement [11]. A cement volume of 1–3 ml has been suggested as optimal, with > 3 ml providing no improvement in fixation strength and greater potential for cement leakage [6, 16]. In our study, 3 ml cement was used in all specimens, whereas 4.5 ml was used for group 3 to avoid any problems caused by cement leakage. In this study, we found similar results with those of comparing the study by Leichtle et al. that found that solid pedicle screws augmented with high-viscosity cement provided comparable screw stability in pull-out testing to that of sophisticated and more expensive fenestrated screws [14]. No differences were found in pull-out strength between the two groups. However, the main problem is that the screws have high integration on a limited surface and do not have ideal integration on other surfaces.
The difference in our study was we evaluated the pull-out strength of the cementation of the entire pedicle screw tract. Since 1960, PMMA coating the femoral stem has positive effects on the survival rate due to the cementation of the entire stem on hip arthroplasty [17]. The main hypothesis of this study is that the cementation of the entire screw tract can provide a wider surface of cement interdigitation and a large surface of adhesion. The screw was only integrated into the body of the corpus but not enough to the pedicle tract in other techniques. We obtained a pull-out strength 2.5 times higher in the cementation of the entire pedicle screw tract technique than the other techniques in this study. Verrier et al. investigated the cancellous bone reaction against PMMA and reported that PMMA showed good osteointegration without any negative effect on bone quality in vivo and tissue cell cultures [18].
The screw malpositioned in the sagittal plane can be tolerated with cement augmentation. Costa et al. found the ideal positions for biomechanically maximal stability of the pedicle screw in the sagittal plane [19]. Craniocaudal orientations have been reported to have an adverse effect on stability. However, our study showed that the major problem of sagittal misorientations can be corrected using the augmentation technique. The pull-out strength of the pedicle screws in malposition obtained the same strength to the standard positions after using augmentation techniques.
Our study has some limitations. First, we used calf vertebra specimens, which could have changed the mechanical properties of the bone, and therefore, the absolute pull-out strength. However, this should not have affected the relative comparison of the pull-out forces for different screw types and implantation techniques during paired comparison in the individual vertebrae. Furthermore, our new cementation technique with high biomechanical force can be seen as a deficiency due to the lack of clinical studies. Second, the difficulties for the clinical use of the technique is another limitation.
Conclusion
The most important evidence of this study is that cannulated-fenestrated screws, which are more expensive, do not have a significant advantage over standard cementing techniques. We obtained a pull-out strength in the cementation of the entire pedicle screw tract technique that is 2.5 times higher than the other techniques in this study. The pull-out strength of the pedicle screws placed in malposition obtained the same strength to the standard positions after using augmentation techniques in our study.
References
Szpalski, M., Gunzburg, R., Mélot, C., & Aebi, M. (2003). The aging of the population: A growing concern for spine care in the twenty-first century. European Spine Journal, 12(Suppl 2), S81–S83.
Gruskay, J. A., Webb, M. L., & Grauer, J. N. (2014). Methods of evaluating lumbar and cervical fusion. Spine J, 14, 531–539.
Mueller, T. L., van Lenthe, G. H., Stauber, M., Gratzke, C., Eckstein, F., & Müller, R. (2009). Regional, age and gender differences in architectural measures of bone quality and their correlation to bone mechanical competence in the human radius of an elderly population. Bone, 45, 882–891.
Liu, M. Y., Tsai, T. T., Lai, P. L., Hsieh, M. K., Chen, L. H., & Tai, C. L. (2020). Biomechanical comparison of pedicle screw fixation strength in synthetic bones: Effects of screw shape, core/thread profile and cement augmentation. PLoS ONE, 15(2), e0229328.
Weiser, L., Huber, G., Sellenschloh, K., Viezens, L., Püschel, K., Morlock, M. M., et al. (2017). Insufficient stability of pedicle screws in osteoporotic vertebrae:biomechanical correlation of bone mineral density and pedicle screw fixation strength. European Spine Journal, 26, 2891–2897.
Frankel, B. M., D’Agostino, S., & Wang, C. (2007). A biomechanical cadaveric analysis of polymethylmethacrylate-augmented pedicle screw fixation. Journal of Neurosurgery Spine, 7, 47–53.
Chang, M. C., Liu, C. L., & Chen, T. H. (2008). Polymethylmethacry-late augmentation of pedicle screw for osteoporotic spinal surgery: A novel technique. Spine (Phila Pa 1976), 33, E317–E324.
Burval, D. J., McLain, R. F., Milks, R., & Inceoglu, S. (2007). Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: Biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976), 32, 1077–1083.
Hoppe, S., & Keel, M. J. (2017). Pedicle screw augmentation in osteoporotic spine: İndications, limitations and technical aspects. European Journal of Trauma and Emergency Surgery, 43(1), 3–8.
Elder, B. D., Lo, S. F., Holmes, C., Goodwin, C. R., Kosztowski, T. A., Lina, I. A., et al. (2015). The biomechanics of pedicle screw augmentation with cement. The Spine Journal, 15(6), 1432–1445.
Lorenz, A., Leichtle, C. I., Frantz, S., Bumann, M., Tsiflikas, I., Shiozawa, T., et al. (2017). Pull out strength of dual outer diameter pedicle screws compared to uncemented and cemented standard pedicle screws: A biomechanical in vitro study. Orthop Surg, 9(2), 229–236.
Allen, R. F., Baldini, N. C., Donofrio, P. E., et al. (1998). Standard test method for determining axial pull-out strength of medical bone screws (F1691-96). In American So-ciety for Testing and Materials (Ed.), Annual book of ASTM standards: medical devices and services. West Conshohocken (PA): American Society for Testing and Materials.
Kiyak, G., Balikci, T., Heydar, A. M., & Bezer, M. (2018). Comparison of the pullout strength of different pedicle screw designs and augmentation techniques in an osteoporotic bone model. Asian Spine Journal, 12(1), 3–11.
Leichtle, C. I., Lorenz, A., Rothstock, S., Happel, J., Walter, F., Shiozawa, T., et al. (2016). Pull-out strength of cemented solid versus fenestrated pedicle screws in osteoporotic vertebrae. Bone & Joint Research, 5(9), 419–426.
Aydogan, M., Ozturk, C., Karatoprak, O., Tezer, M., Aksu, N., & Hamzaoglu, A. (2009). The pedicle screw fixation with vertebroplasty augmentation in the surgical treatment of the severe osteoporotic spines. Journal of Spinal Disorders & Techniques, 22(6), 444–447.
Bullmann, V., Liljenqvist, U. R., Rodl, R., et al. (2010). Pedicle screw augmentation from a biomechanical perspective. Orthopäde, 39, 673–678.
Charnley, J. (1960). Anchorage of the femoral head prosthesis to the shaft of the femur. The Journal of Bone and Joint Surgery. British volume, 42-B, 28–30.
Verrier, S., Hughes, L., Alves, A., Peroglio, M., Alini, M., & Boger, A. (2012). Evaluation of the in vitro cell-material interactions and in vivo osteo-integration of a spinal acrylic bone cement. European Spine Journal, 21(Suppl 6), S800–S809.
Costa, F., Villa, T., Anasetti, F., Tomei, M., Ortolina, A., Cardia, A., et al. (2013). Primary stability of pedicle screws depends on the screw positioning and alignment. The Spine Journal, 13(12), 1934–1939.
Acknowledgements
The authors would like to thank Enago (www.enago.com) for the English language review.
Funding
The study was funded by Istanbul University BAP numbered as TSA-2018-27709.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical standard statement
All procedures performed in the study were in accordance with the ethical standards of the institutional and or/ national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This article does not contain any studies with human or animal subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akgül, T., Korkmaz, M., Pehlivanoglu, T. et al. Biomechanical Comparison of Pull-out Strength of Different Cementation and Pedicle Screw Placement Techniques in a Calf Spine Model. JOIO 54 (Suppl 1), 134–140 (2020). https://doi.org/10.1007/s43465-020-00199-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00199-z