Abstract
Background
The literature is scanty on reports directly comparing the outcomes of anterior open reduction (AOR) and medial open reduction (MOR) in the management of developmental dysplasia of the hip (DDH).
Purpose of the Study
To compare clinical and radiographic outcomes of surgical treatment using either AOR or MOR in children with DDH aged < 24 months and to evaluate the procedure-inherent risks of avascular necrosis of the femoral head (AVN) and need for further corrective surgery (FCS).
Methods
61 children who underwent surgical treatment for DDH were categorized into two groups: AOR (31 hips of 28 patients) and MOR (39 hips of 33 patients). The mean age was 17 ± 5.85 (range 7–24) months in group AOR and 13 ± 5.31 (range 6–24) months in group MOR. The mean follow-up was 118 ± 41.2 (range 24–192) months and 132 ± 36.7 (range 24–209) months in group AOR and MOR. At the final follow-up, mid- to long-term clinical and radiographic outcomes were assessed. FCS was recorded.
Results
Regarding McKay’s clinical criteria, both groups exhibited similar results (p = 0.761). No significant differences were observed between the groups in both the center–edge–angle (p = 0.112) and the Severin score (p = 0.275). The AVN rate was 32% in the AOR group and 20% in the MOR group (p = 0.264). The FCS rate was 22% in the AOR group and 12% in the MOR group (p = 0.464).
Conclusions
This study showed similar clinical and radiological outcomes with AOR and MOR with no significant relation to AVN and FCS.
Level of Evidence
Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The main goal of primary treatment for developmental dysplasia of the hip (DDH) is to achieve a concentric stable reduction to facilitate proper femoral head and acetabulum development and to prevent avascular necrosis of the femoral head (AVN) and need for further corrective surgery (FCS), including acetabular and/or femoral osteotomy as well as re-surgery for subluxation or dislocation [1, 2]. To accomplish this goal, Pavlik harness is regarded as the initial treatment method during the first 6 months of infancy [3, 4]. Open reduction is typically reserved for children aged 6–18 months in whom non-surgical methods fail to obtain stable reduction [3]. Several surgeons consider open reduction as the first-line treatment for children aged older than 18 months [3, 5].
The most common surgical approaches for open reduction are medial approach open reduction and anterior approach open reduction. Both approaches can directly address hindrances in concentric reduction, including the iliopsoas, transverse acetabular ligament, ligamentum teres, neolimbus, pulvinar, and acetabulum [6]. However, as compared with the anterior open reduction (AOR), despite its advantage of less blood loss, medial open reduction (MOR) provides no access for capsular plication and pelvic osteotomy (if required) [5]. Furthermore, AVN and FCS rates relevant to the two approaches range extensively in the literature [3, 4, 7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35], and the medial approach has been more commonly associated with AVN and FCS [6, 10, 25, 36,37,38].
Current literature illustrates the pros and cons of each approach individually; however, there is still a lack of evidence comparing the two approaches to determine the more advantageous one [1, 6, 39,40,41]. Therefore, this study aimed to compare the mid-term clinical and radiographic outcomes of surgical treatment using either AOR or MOR in children with DDH aged < 24 months and specifically to assess the procedure-inherent risks of AVN and FCS.
Materials and Methods
After obtaining approval from the institutional review board, a total of 91 consecutive patients who underwent surgical treatment with either AOR or MOR for the treatment of DDH from 2003 to 2011 were retrospectively reviewed. Based on the eligibility criteria (Table 1), 30 children were excluded; the remaining 61 children were enrolled in the study. Parents were informed that medical records could be used for scientific purposes only; thus, written informed consent was obtained at the final visit.
Patients included in the study were categorized into two groups based on the surgical approach used during the initial operation: AOR and MOR. The AOR group included 31 hips of 28 patients (27 females and 4 males), whereas the MOR group consisted of 39 hips of 33 patients (29 females and 3 males).
During the initial operation, the mean age of the patients was 17 ± 5.85 (range 7–24) months in group AOR and 13 ± 5.31 (range 6–24) months in group MOR. The mean follow-up was 118 ± 41.2 (range 24–192) months and 132 ± 36.7 (range 24–209) months in group AOR and MOR, respectively. Patients in either group were comparable in terms of demographic data as shown in Table 2 (p > 0.05 for gender, side, number of hips, and duration of follow-up).
Six hips of 5 children in group AOR and 7 hips of 6 children in group MOR experienced previous treatment failure with closed reduction under general anesthesia and a hip spica cast. The remaining children in both groups had been primarily operated.
With regard to additional procedures performed during the initial open reduction (Table 3), 11 children (12 hips) in group AOR underwent a percutaneous adductor tenotomy for mild adduction contracture. However, in three children (four hips) with severe adduction contracture, an open adductor tenotomy was preferred. Otherwise, the adductor tenotomy was a certain component of medial approach open reduction. If hip abduction was more than 30°, adduction contracture was defined as mild. If hip abduction was less than 30°, adduction contracture was defined as severe. Four children (four hips) in group AOR and seven children (eight hips) in group MOR in whom closed reduction had been practicable underwent a hip arthrogram in order to determine the quality of the initial reduction. Among these patients, open reduction was required due to an increased medial dye pool in three children (three hips) from group AOR and two children (three hips) from group MOR. In addition, none of the hips in group MOR underwent any additional surgical procedures during the initial operation; however, femoral varization derotational osteotomy in two hips with unilateral DDH was performed in group AOR.
Management and Follow-Up Protocol
None of the patients from both groups underwent preoperative hip traction. Open reduction is indicated in both groups based on the following reasons:
-
Failure of closed reduction
-
Unstable hip following closed reduction
-
Non-concentric reduction after closed reduction
-
Stability achieved by closed reduction that can be only maintained by placing the hip in an extreme degree of internal rotation or abduction.
Open reduction of hips was performed using anterolateral [42] or medial approaches [43, 44] by three pediatric orthopedic surgeons as previously described in the literature. The surgical approach used decided based on the surgeon’s preference and experience. Nine children with bilateral involvement were operated at the same session; three and six of them underwent bilateral anterior approach and bilateral medial approach, respectively.
After achieving a concentric hip reduction, all patients were placed in a hip spica cast postoperatively, with hip abduction of < 60° and flexion of not > 100° for 3 months based on the surgeon’s preference. Based on the surgeon’s preference, in group AOR, the reduction was postoperatively confirmed by computed tomography (CT) in three children (three hips) and magnetic resonance imaging (MRI) in seven children (seven hips). In group MOR, the postoperative reduction was checked by CT in four children (four hips) and MRI in eight children (nine hips). In both groups, postoperative imaging showed concentric reduction and congruity of the femoral head into the true acetabulum. The cast was routinely changed at least once under general anesthesia at the midpoint of this period. Then, patients were put in an abduction orthosis with both hips flexed at 90° and abducted at 30° for nearly 12 weeks (full time for the first 6 weeks and only during sleep for the next 6 weeks).
Clinical and Radiological Assessment
The clinical and radiological assessments were performed by two experienced pediatric orthopaedic surgeons.
During the clinical assessment, the modified McKay’s clinical criteria [45] were used for each patient at the final follow-up in addition to measuring the hip range of motion (ROM) and hip muscle strength.
ROM was measured using a universal standard goniometer. The isometric muscle strength was measured using a portable, hand-held dynamometer (The wireless microFET®2 Digital Handheld Dynamometer muscle tester, Hoggan Scientific LLC, Salt Lake City, USA) based on a described previously validated method [46] in the hip flexor and abductor muscles. The measurement protocol in terms of dynamometer and positioning was standardized depending on procedures previously often used in clinical settings [47]. The dynamometer was calibrated before and after each round of measurement in accordance with the manufacturer’s instructions. Each measurement was performed according to “the make test” protocol [46], where the examiner holds the dynamometer in a stationary position while the child pushes the dynamometer with a maximal strength.
In the radiological assessment, each hip with DDH was classified based on the Tönnis staging (grade 1–4) [48], and the acetabular index (AI) was measured on preoperative anteroposterior (AP) pelvic radiographs. [49] At the final follow-up, the center–edge–angle (CEA) was measured to examine the residual acetabular dysplasia, [49] and the Severin score [50] was calculated based on AP pelvic radiographs to assess the radiographic results (presence of femoral head and femoral neck deformity or subluxation).
The primary outcomes in this study were AVN and FCS rates for each approach. AVN was assessed based on Kalamchi and MacEwen criteria [51] in a minimum of 2-year follow-up radiographs.
FCS including an additional reconstructive procedure (acetabular and/or femoral osteotomy) and/or reconstructive open reduction of the hip was also recorded from the review of institutional medical records.
Statistical Analyses
IBM SPSS Statistics software, version 20.0 (IBM Corp., Armonk, New York, NY, USA), was used for statistical analysis. A p < 0.05 was considered statistically significant. Normality tests were conducted using the Shapiro–Wilk test and histogram graphics. Data are presented as “minimum”, “maximum”, “range”, “arithmetic mean”, “standard deviation”, and ‘’percentage’’. Between-group comparisons were performed using the Student t test for continuous variables, and Pearson’s Chi-square test, Fisher’s exact test, or Fisher–Freeman–Halton’s exact test for categorical variables.
Results
Clinical Evaluation
The patients’ clinical outcomes in each group are demonstrated in Table 4. Regarding ROM measurements, no differences were observed between the two groups (p > 0.05 for each variable). Although no difference was observed in the measurement of abductor muscle strength (p = 0.133), the flexor muscle strength was significantly higher in the AOR group than that in the MOR (p = 0.037; p < 0.05). Regarding McKay’s clinical criteria, both groups exhibited similar results (p = 0.761).
Radiographic Evaluation
The radiographic outcomes of patients in for each group are demonstrated in Table 5. In the preoperative Tönnis grading of DDH, no significant difference was recognized between the two groups (p = 0.518). Furthermore, both groups demonstrated similar preoperative AI values (Figs. 1 and 2, examples of preoperative and postoperative radiographs for AOR and MOR).
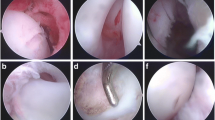
At the final follow-up, no significant differences were observed between the two groups in terms of CEA measurement (p = 0.112), as well as the AVN rate and grade (Fig. 3) (p = 0.264 and 0.084, respectively) (Figs. 4 and 5, examples of AVN types following AOR and MOR). Although statistically insignificant, the rate of AVN was higher in the AOR group (32%) than in the MOR group (22%), but the severity of AVN was higher in the MOR group according to Kalamchi and MacEwen criteria (Table 5).
Revision Surgery
In both groups, there was no case that developed AVN or required FCS among children who had failure of previous treatment with closed reduction and casting. One child with unilateral DDH from each group had developed a re-dislocation recognized by the MRI. Then, patients underwent a revision surgery by an anterolateral approach. No signs of AVN were observed at the follow-up. Two patients in the AOR group and three in the MOR group underwent Salter’s innominate osteotomy for residual acetabular dysplasia. Furthermore, femoral varization derotational osteotomy was performed in two patients in the AOR group and one in the MOR group for coxa valga and increased femoral anteversion. The FCS rate was 22% in the AOR group and 12% in the MOR group (p = 0.464) (Fig. 3; Table 6). Lastly, final follow-up examination revealed that one child experienced coxa breva and overgrowth of the greater trochanter secondary to type 4 AVN (right hip) following MOR (Fig. 4). This patient had undergone Salter’s innominate osteotomy for residual dysplasia after open reduction at 5 years old. At the final follow-up, we planned a femoral neck-lengthening osteotomy and transfer of the greater trochanter to prevent early osteoarthritis. Lastly, one child developed caput valgum deformity secondary to type 2 AVN (left hip) and residual acetabular dysplasia (Fig. 5) in the AOR group. For this patient, we planned a revision surgery including pelvic osteotomy and if necessary, proximal femoral osteotomy.
Discussion
In the management of DDH, although several authors reported favorable results for open reduction with either AOR or MOR [3, 4, 7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35], only few studies directly compared the outcomes of both approaches in the literature [1, 6, 39,40,41]. Therefore, this study provides additional evidence that MOR and AOR approaches could confer similar clinical and radiographic outcomes at mid- to long-term follow-up. Besides, AVN and NFS constitute the most vital problems that may jeopardize the outcome of a successfully performed open reduction in the postoperative period of DDH [52]. Hence, comparing the AVN and NFS rates was chosen as primary outcomes in this study.
Based on our comprehensive review of the current literature, AVN rates associated with MOR varied from 0 to 43%, with majority of investigations reporting 10–30% [3, 4, 7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Even though the reported AVN rates following AOR have ranged from 0 to 35% [23,24,25,26,27,28,29,30,31,32,33,34,35], these ratios are under the top rates in MOR studies. Similar to AVN, FCS rates following the open reduction of DDH seemed inconsistent. MOR rates varied from 0 to 53%, with most authors reporting < 30% [7, 9, 11,12,13,14,15,16,17, 20, 36]. Likewise, FCS following AOR showed a range from 0 to 57%, with majority of researchers reporting < 30% [23,24,25, 29, 33, 34]. For both MOR and AOR, the AVN (20% and 32%, respectively) and FCS (12% and 22%, respectively) rates obtained in this study are consistent with those in the literature.
Based on the aforementioned information, previous reports have focused on the risk assessment of AVN and FCS for open reductions of DDH. Nonetheless, few clinical studies have directly compared the AVN and FCS rates for both approaches to date (Table 7) [1, 6, 39, 41]. In one study, Bulut et al. [41] found that the AVN rate was lower in the medial approach (6%, 3/47 hips) than that in the anterior approach (30%, 4/13 hips) in children aged < 24 months. In contrast, the authors observed no significant difference in FCS between medial (21%, 10/47 hips) and anterior approaches (6%, 4/14 hips). In another comparative study, Tarassoli et al. [1] prospectively assessed AVN and FCS risks for both approaches, with a mean follow-up of 70 (range 26–228) months. The authors concluded that children treated via an early MOR were not highly at risk of AVN at the early to mid-term follow-up as compared to those treated via a delayed AOR. Similar to Tarassoli et al. but with longer follow-up, early MOR was found to carry similar risks in terms of AVN and FCS as compared to delayed AOR. Although statistically insignificant, it is also worth noting that in our series, AVN is more frequent in AOR but more severe in MOR according to Kalamchi and MacEwen criteria.
With a new perspective on the issue, Gardner et al. [53] conducted a systematic review of 14 studies to identify the rate of clinically significant AVN following MOR. Therefore, the authors did not include type I AVN because it has an insignificant impact on the outcome and found that the rate of clinically significant AVN (types 2–4) was 20% (149/734 hips). Based on Gardner et al.’s study design, the rate of clinically significant AVN in our study was higher in the MOR group (25%) than those in the AOR group (12%) despite no statistical significance.
The primary limitation of this and previous comparative studies [1, 39,40,41] is the higher age profile in the AOR group than that in the MOR, which may have influenced the results. Hoellwarth et al. [6] attempted to eliminate this potential confounder by comparing two techniques in an age-matched manner (mean age: 6 [range 1.4–14.9] months) and found no relationship between the surgical approach and risk of AVN (22%, 4/18 hips in MOR and 28%, 5/18 hips in AOR) and FCS (21%, 4/19 hips in MOR and 37%, 7/19 in AOR). Nevertheless, drawing a definitive conclusion is difficult due to the small sample size. Therefore, prospective, matched-pair, and observational designed further studies including larger sample sizes are needed to better clarify these relationships.
The final radiographic outcomes in this study were assessed based on the Severin classification due to its reliability [54]. In the literature, the mean rate of excellent and good radiographic results according to Severin classification is 73.8% (range 33–96%) in the AOR series [8, 10, 25, 27, 40, 55], and 62.9% (range 45.7–79%) in the MOR series [12, 56, 57]. Therefore, our radiographic results for both AOR and MOR groups seemed favorable without significant difference and are comparable to other series. Therefore, if the follow-up period is short, physicians must be more careful in making judgments regarding the final outcome since the Severin criteria become more reliable with increasing patient age. Considering our follow-up period that is longer than most studies cited above, we believe that this study can particularly confer strong evidence on the radiographic results of open reduction treatment in patients with DDH. In contrast, although some children had been regularly followed by clinical and radiographic evaluation for many years in both groups, most of them had solely a few years of follow-up because of the absence of complaints about their hips. Thus, we could not evaluate the changes in AI on subsequent radiographs, which can be considered as a limitation.
Furthermore, the clinical outcomes should also be discussed. To evaluate the patients’ final clinical status, the modified McKay criteria that is mostly preferred in the literature have been used. Excellent and good clinical outcomes have been reported with a rate of 84.6–98% for the AOR series [33, 35, 41] and 83–98% for the MOR series [11, 25, 35, 58,59,60]. For both surgical approaches, the rate of excellent and good clinical outcomes in our study is favorably comparable with those in previous studies. Nonetheless, the modified McKay criteria are a subjective scoring system to evaluate the functional status of the hip joint. Therefore, unlike most studies, the hip ROM was measured with a universal goniometer in addition to hip flexor and abductor muscle strength using a portable, hand-held dynamometer, a reliable and validated method, in order to provide more objective functional results. Our measurements indicated that although no differences in ROM and abductor muscle strength existed, the flexor muscle strength was significantly higher in the AOR group than that in the MOR.
When interpreting the findings in this study, some limitations and strengths should be considered. The first limitation was its retrospective nature. Second, despite the use of an upper age limit, children in the AOR group had a higher mean age, which may have affected our results. Otherwise, the two groups were comparable in terms of Tönnis classification, which may be a determinant for the risk of AVN or FCS. Third, since type II AVN frequently does not become evident for several years after surgery [52], the mid-term follow-up of the current study is insufficient to make an accurate judgment concerning the rate of type II AVN. Last, the current study is a non-randomized, surgeon dependent study where three different surgeons performed all the operations. This may have biased the results because of surgeon’s preference and experience. Despite these limitations, our study is one of few studies [1, 39,40,41] that compare clinical and radiological outcomes of AOR and MOR as the surgical treatment for DDH.
Conclusion
Evidence from this study has demonstrated that in the management of DDH, AOR and MOR can provide similar favorable clinical and radiological outcomes with no significant relation to AVN and FCS at the mid-term follow-up.
References
Tarassoli, P., Gargan, M. F., Atherton, W. G., & Thomas, S. R. Y. W. (2014). The medial approach for the treatment of children with developmental dysplasia of the hip. Bone and Joint Journal, 96, 406–413.
Novais, E. N., Hill, M. K., Carry, P. M., & Heyn, P. C. (2016). Is age or surgical approach associated with osteonecrosis in patients with developmental dysplasia of the hip? A meta-analysis. Clinical Orthopaedics and Related Research, 474, 1166–1177.
Biçimoglu, A., Ag, H., Ömeroglu, H., & Tümer, Y. (2003). Six years of experience with a new surgical algorithm in developmental dysplasia of the hip in children under 18 months of age. Journal of Pediatric Orthopedics, 23, 693–698.
Gardner, R. O., Bradley, C. S., Sharma, O. P., Feng, L., Shin, M. E., Kelley, S. P., et al. (2016). Long-term outcome following medial open reduction in developmental dysplasia of the hip: A retrospective cohort study. Journal of Children’s Orthopaedics, 10, 179–184.
Murphy, R. F., & Kim, Y.-J. (2016). Surgical management of pediatric developmental dysplasia of the hip. Journal of American Academy of Orthopaedic Surgeons, 24, 615–624.
Hoellwarth, J. S., Kim, Y. J., Millis, M. B., Kasser, J. R., Zurakowski, D., & Matheney, T. H. (2015). Medial versus anterior open reduction for developmental hip dislocation in age-matched patients. Journal of Pediatric Orthopedics, 35, 50–56.
Mankey, M. G., Arntz, G., & Staheli, L. T. (1993). Open reduction through a medial approach for congenital dislocation of the hip. A critical review of the Ludloff approach in sixty-six hips. Journal of Bone Joint Surgery America, 75, 1334–1345.
Koizumi, W., Moriya, H., Tsuchiya, K., Takeuchi, T., Kamegaya, M., & Akita, T. (1996). Ludloff’s medial approach for open reduction of congenital dislocation of the hip: A 20-year follow-up. Journal of Bone and Joint Surgery. British Volume, 78, 924–929.
Konigsberg, D. E., Karol, L. A., Colby, S., & O’Brien, S. (2003). Results of medial open reduction of the hip in infants with developmental dislocation of the hip. Journal of Pediatric Orthopedics, 23, 1–9.
Morcuende, J. A., Meyer, M. D., Dolan, L. A., & Weinstein, S. L. (1997). Long-term outcome after open reduction through an anteromedial approach for congenital dislocation of the hip. Journal of Bone and Joint Surgery. American Volume, 79, 810–817.
Tumer, Y., Ward, W. T., & Grudziak, J. (1997). Medial open reduction in the treatment of developmental dislocation of the hip. Journal of Pediatric Orthopedics, 17, 176–180.
Ucar, D. H., Isiklar, Z. U., Stanitski, C. L., Kandemir, U., & Tumer, Y. (2004). Open reduction through a medial approach in developmental dislocation of the hip: A follow-up study to skeletal maturity. Journal of Pediatric Orthopedics, 24, 493–500.
Kiely, N., Younis, U., Day, J., & Meadows, T. (2004). The Ferguson medial approach for open reduction of developmental dysplasia of the hip: A clinical and radiological review of 49 hips. Journal of Bone and Joint Surgery. British Volume, 86, 430–433.
Okano, K., Yamada, K., Takahashi, K., Enomoto, H., Osaki, M., & Shindo, H. (2009). Long-term outcome of Ludloff’s medial approach for open reduction of developmental dislocation of the hip in relation to the age at operation. International Orthopaedics, 33, 1391–1396.
Duman, S., Camurcu, Y., Sofu, H., Ucpunar, H., Akbulut, D., & Yildirim, T. (2019). Arthroscopic versus open, medial approach, surgical reduction for developmental dysplasia of the hip in patients under 18 months of age. Acta Orthopaedics, 90, 1–7.
Pollet, V., Van Dijk, L., Reijman, M., Castelein, R. M. C., & Sakkers, R. J. B. (2018). Long-term outcomes following the medial approach for open reduction of the hip in children with developmental dysplasia. Journal of Bone and Joint Surgery. British Volume, 100, 822–827.
Ozkut, A. T., Iyetin, Y., Unal, O. K., Soylemez, M. S., Uygur, E., & Esenkaya, I. (2018). Radiological and clinical outcomes of medial approach open reduction by using two intervals in developmental dysplasia of the hip. Acta Orthopaedica et Traumatologica Turcica, 52, 81–86.
Youssef, A. O. (2018). Medial approach open reduction with ligamentum teres partial excision and plication for the management of congenital hip dislocation. Journal of Pediatric Orthopedics. Part B, 27, 244–249.
Çıtlak, A., Saruhan, S., & Baki, C. (2013). Long-term outcome of medial open reduction in developmental dysplasia of hip. Archives of Orthopaedic and Trauma Surgery, 133, 1203–1209.
Iyetin, Y., Turkmen, I., Saglam, Y., Akcal, M. A., Unay, K., & Unsac, B. (2015). A modified surgical approach of the hip in children: Is it safe and reliable in patients with developmental hip dysplasia? Journal of Children’s Orthopaedics, 9, 199–207.
Farsetti, P., Caterini, R., Potenza, V., & Ippolito, E. (2015). Developmental dislocation of the hip successfully treated by preoperative traction and medial open reduction: A 22-year mean followup. Clinical Orthopaedics and Related Research, 473, 2658–2669.
Yamada, K., Mihara, H., Fujii, H., & Hachiya, M. (2014). A long-term follow-up study of open reduction using Ludloff’s approach for congenital or developmental dislocation of the hip. Bone and Joint Research., 3, 1–6.
Berkeley, M. E., Dickson, J. H., Cain, T. E., & Donovan, M. M. (1984). Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. Journal of Bone and Joint Surgery. American Volume, 66, 412–420.
Galpin, R. D., Roach, J. W., Wenger, D. R., Herring, J. A., & Birch, J. G. (1989). One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. Journal of Bone and Joint Surgery. American Volume, 71, 734–741.
Ordier, W., Tönnis, D., Kalchschmidt, K., Storch, K. J., & Katthagen, B. D. (2005). Long-term results after open reduction of developmental hip dislocation by an anterior approach lateral and medial of the iliopsoas muscle. Journal of Pediatric Orthopaedics, 14, 79–87.
Barrett, W. P., Staheli, L., & Chew, D. E. (1986). The effectiveness of the Salter innominate osteotomy in the treatment of congenital dislocation of the hip. Journal of Bone and Joint Surgery. American Volume, 68, 79–87.
Gulman, B., Tuncay, I. C., Dabak, N., & Karaismailoglu, N. (1994). Salter’s innominate osteotomy in the treatment of congenital hip dislocation: A long-term review. Journal of Pediatric Orthopedics, 14, 662–666.
Wenger, D. R., Lee, C.-S., & Kolman, B. (1995). Derotational femoral shortening for developmental dislocation of the hip: Special indications and results in the child younger than 2 years. Journal of Pediatric Orthopedics, 15, 768–779.
Alassaf, N. (2018). Predictors of femoral shortening for pediatric developmental hip dysplasia surgery: An observational study in 435 patients. Patient Safety Surgery, 12, 29.
Emara, K., Kersh, M. A. A., & Hayyawi, F. A. (2019). Duration of immobilization after developmental dysplasia of the hip and open reduction surgery. International Orthopaedics, 43, 405–409.
Kothari, A., Grammatopoulos, G., Hopewell, S., & Theologis, T. (2016). How does bony surgery affect results of anterior open reduction in walking-age children with developmental hip dysplasia? Clinical Orthopaedics and Related Research, 474, 1199–1208.
Arsian, H., Sucu, E., Ozkul, E., Gem, M., & Kisin, B. (2014). Should routine pelvic osteotomy be added to the treatment of DDH after 18 months. Acta Orthopaedica Belgica, 80, 205–210.
Mehmet, G., Arslan, H., Özkul, E., Alemda, C., Azboy, İ., & Demirtaş, A. (2014). One-stage bilateral open reduction using the anterior iliofemoral approach in developmental dysplasia of the hip. Acta Orthopaedica Belgica, 80, 211–215.
Szepesi, K., Szücs, G., Szeverényi, C., & Csernátony, Z. (2013). Long-term follow-up of DDH patients who underwent open reduction without a postoperative cast. Journal of Pediatric Orthopedics. Part B, 22, 85–90.
Szepesi, K., Biró, B., Fazekas, K., & Szücs, G. (1995). Preliminary results of early open reduction by an anterior approach for congenital dislocation of the hip. Journal of Pediatric Orthopedics. Part B, 4, 171–178.
Agus, H., Ömeroglu, H., Uçar, H., Biçimoglu, A., & Tümer, Y. (2002). Evaluation of the risk factors of avascular necrosis of the femoral head in developmental dysplasia of the hip in infants younger than 18 months of age1. Journal of Pediatric Orthopedics. Part B, 1, 41–46.
Thomas, I., Dunin, A., Cole, W., & Menelaus, M. B. (1989). Avascular necrosis after open reduction for congenital dislocation of the hip: Analysis of causative factors and natural history. Journal of Pediatric Orthopedics, 9, 525–531.
Clarke, N. M., Jowett, A. J., & Parker, L. (2005). The surgical treatment of established congenital dislocation of the hip: Results of surgery after planned delayed intervention following the appearance of the capital femoral ossific nucleus. Journal of Pediatric Orthopedics, 25, 434–439.
Yorgancıgil, H., & Aslan, A. (2016). Comparison of the clinical and radiological outcomes of open reduction via medial and anterior approach in devleopmental dysplasia of the hip. Eklem hastaliklari cerrahisi., 27, 74–80.
Holman, J., Carroll, K. L., Murray, K. A., MacLeod, L. M., & Roach, J. W. (2012). Long-term follow-up of open reduction surgery for developmental dislocation of the hip. Journal of Pediatric Orthopedics, 32, 121–124.
Bulut, M., Gürger, M., Belhan, O., Batur, O. C., Celik, S., & Karakurt, L. (2013). Management of developmental dysplasia of the hip in less than 24 months old children. Indian Journal of Orthopaedics., 47, 578.
Wedge, J. H., Thomas, S. R., & Salter, R. B. (2008). Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. Journal of Bone and Joint Surgery. American Volume, 90, 238–253.
Ludloff, K. (1913). The open reduction of the congenital hip dislocation by an anterior incision. Journal of Bone and Joint Surgery. American Volume, 2, 438–454.
Ferguson, J. R. (1973). Primary open reduction of congenital dislocation of the hip using a median adductor approach. Journal of Bone and Joint Surgery. American Volume, 55, 671–689.
Mckay, D. W. (1974). A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clinical Orthopaedics and Related Research, 98, 124–132.
Eek, M. N., Kroksmark, A.-K., & Beckung, E. (2006). Isometric muscle torque in children 5 to 15 years of age: Normative data. Archives of Physical Medicine and Rehabilitation, 87, 1091–1099.
Thorborg, K., Petersen, J., Magnusson, S. P., & Hölmich, P. (2010). Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scandinavian Journal of Medicine and Science in Sports, 20, 493–501.
Tönnis, D. (1987). General radiography of the hip joint. Congenital dysplasia and dislocation of the hip in children and adults (pp. 100–142). Berlin: Springer.
Omeroglu, H., Kaya, A., & Guclu, B. (2007). Evidence-based current concepts in the radiological diagnosis and follow-up of developmental dysplasia of the hip. Acta Orthopaedica et Traumatologica Turcica, 41(Suppl 1), 14–18.
Severin, E. (1941). Contribution to the knowledge of congenital dislocation of the hip joint. Acta Chir Scand, 84, 163.
Kalamchi, A., & MacEwen, G. D. (1980). Avascular necrosis following treatment of congenital dislocation of the hip. Journal of Bone and Joint Surgery. American Volume, 62, 876–888.
Bache, C. E., Graham, H. K., Dickens, D. R. V., Donnan, L., Johnson, M. B., Nattrass, G., et al. (2008). Ligamentum teres tenodesis in medial approach open reduction for developmental dislocation of the hip. Journal of Pediatric Orthopaedics, 28, 607–613.
Gardner, R. O. E., Bradley, C. S., Howard, A., Narayanan, U. G., Wedge, J. H., & Kelley, S. P. (2014). The incidence of avascular necrosis and the radiographic outcome following medial open reduction in children with developmental dysplasia of the hip: A systematic review. The Bone and Joint Journal., 96, 279–286.
Carroll, K. L., Murray, K. A., MacLeod, L. M., Hennessey, T. A., Woiczik, M. R., & Roach, J. W. (2011). Measurement of the center edge angle and determination of the Severin classification using digital radiography, computer-assisted measurement tools, and a Severin algorithm: Intraobserver and interobserver reliability revisited. Journal of Pediatric Orthopaedics., 31, e30–e35.
Angliss, R., Fujii, G., Pickvance, E., Wainwright, A. M., & Benson, M. K. D. (2005). Surgical treatment of late developmental displacement of the hip: Results after 33 years. The Journal of Bone and Joint Surgery British Volume., 87, 384–394.
Varner, K. E., Incavo, S. J., Haynes, R. J., & Dickson, J. A. (2010). Surgical treatment of developmental hip dislocation in children aged 1 to 3 years: A mean 18-year, 9-month follow-up study. Orthopedics, 33, 3.
Wang, T. M., Wu, K. W., Shih, S. F., Huang, S. C., & Kuo, K. N. (2013). Outcomes of open reduction for developmental dysplasia of the hip: Does bilateral dysplasia have a poorer outcome? Journal of Bone and Joint Surgery. American Volume, 95, 1081–1086.
Baki, C., Sener, M., Aydin, H., Yildiz, M., & Saruhan, S. (2005). Single-stage open reduction through a medial approach and innominate osteotomy in developmental dysplasia of the hip. Journal of Bone and Joint Surgery. British Volume, 87, 380–383.
Erturk, C., Altay, M. A., Yarimpapuc, R., & Isikan, U. E. (2011). Medial open reduction of developmental dysplasia of the hip using the Weinstein-Ponseti approach. Saudi Medical Journal, 32, 901–906.
Biçimoğlu, A., Ağuş, H., Ömeroğlu, H., & Tümer, Y. (2008). Posteromedial limited surgery in developmental dysplasia of the hip. Clinical Orthopaedics and Related Research, 466, 847–855.
Author information
Authors and Affiliations
Contributions
ÖNE: Substantial contributions to the conception, design of the work, the acquisition, analysis and interpretation of data for the work. MD: Substantial contributions to the conception, design of the work, the acquisition, analysis and interpretation of data for the work. EM: The acquisition, analysis and interpretation of data for the work. VŞ: Analysis and interpretation of data for the work. FB: Substantial contributions to the conception, design of the work, and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Ergin, O.N., Demirel, M., Meric, E. et al. A Comparative Study of Clinical and Radiological Outcomes of Open Reduction Using the Anterior and Medial Approaches for the Management of Developmental Dysplasia of the Hip. JOIO 55, 130–141 (2021). https://doi.org/10.1007/s43465-020-00171-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00171-x