Abstract
Introduction
The current published evidence for the treatment of developmental dysplasia of the hip (DDH) with failed closed reduction (CR) following failed Pavlik harness (PH) treatment is still limited. This study aimed to determine whether an one-stage open reduction (OR) would lead to a similar outcome to a two-stage OR in these patients. Meanwhile, the occurrence of femoral head avascular necrosis (AVN) and further surgery (pelvic osteotomy, PO) within the follow-up period was investigated.
Materials and methods
A consecutive series of DDH patients who failed CR following failed PH treatment and received OR finally between January 2008 and December 2020 were studied. The patients were divided into two groups. One group of which received OR immediately after failed CR (one-stage OR group, Group A), and the other received a delayed OR (two-stage OR group, Group B). The McKay’s criteria, acetabular index (AI) and the degree of dislocation of the hips were evaluated for the final outcomes.
Results
At the last follow-up, 54 (84.4%) of the 64 hips in Group A and 26 (83.9%) of 31 hips in Group B were in excellent or good condition. Comparison between the two groups revealed that there were no differences in terms of McKay grading (P = 0.950), AI (P = 0.783), incidence of AVN (P = 0.745), and also incidence of PO (P = 1.000). However, a significant lower mean AI was found in Group A, when the OR was performed in Group B (31.06 ± 4.45° vs. 33.87 ± 4.12°, P = 0.004).
Conclusion
Both of the one- and two-stage OR may acheive favorable outcomes. Moreover, one-stage OR is of without the general anesthesia risk associated with two-stage OR. We therefore advocate that an OR should be performed in appropriate DDH patients during the same session once a failed CR is detected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) is a common developmental deformity of the lower extremity and one of the leading causes of total hip arthroplasty in young people [1, 2]. It is currently accepted that, early detection and Pavlik harness (PH) treatment in infants less than 6 months of age can yield favorable outcomes [1, 3]. While failure of PH treatment are unavoidable. In these patients, a closed reduction (CR) of the dislocated hip is usually firstly considered for further treatment [2, 4]. Unfortunately, failure of CR is still encountered. Thus open reduction (OR) is indicated [1, 5, 6]. However, the timing of OR after failed CR is still not well established.
To our knowledge, previous reports regarding management after failed CR have focused on issues such as the occurrence of femoral head avascular necrosis (AVN), patient’s age at intervention, the incidence of further surgery and so on, while few studies specially reported the timing of OR. Accordingly, the corresponding data is still limited. Therefore, in this study, we compared the clinical and radiographic outcomes of OR between two groups of DDH patients with failed CR following failed PH treatment, aiming to determine whether an one-stage OR would lead to a similar outcome to a two-stage OR in these patients. Meanwhile, the occurrence of AVN and further surgery (pelvic osteotomy, PO) within the follow-up period was investigated.
Materials and methods
In our hospital, a CR is usually attempted in DDH patients with failed PH treatment. When the CR fails, an OR is usually performed during the same session (one-stage OR). Before CR, all legal guardians gave their formal consent for the treatment protocol they would accept after being explained the pros and cons and the potential complications of each method. For those who do not accept one-stage OR, a delayed (two-stage) OR is performed.
Patients
After the Institutional Review Board approved this study, we retrospectively reviewed the medical records of all DDH patients who were treated with OR between January 2008 and December 2020. The study included a total of 95 consecutive DDH patients who failed CR following failed PH treatment and received OR finally. According to the time when OR was performed, the patients were divided into two groups. Of these patients, 64 cases underwent OR immediately after failed CR during the same operative session, and were designated as the one-stage OR group (Group A). Thirty-one cases underwent delayed OR after several months of consideration of the legal guardians following the failed CR, and were designated as the two-stage OR group (Group B). Inclusion criteria included: (1) diagnosis of DDH, (2) failure of previous CR and PH treatment, younger than 6 months (mean 4 months) when PH treatment started and the duration of treatment was not more than 1.5 months, (3) treated by OR in our hospital within 18 months of age. Exclusion criteria included bilateral DDH, presence of AVN before OR, genetic or neuromuscular disorders, and older than 18 months of age when OR is performed.
The operative techniques were similar as reported in previous studies [7]. Under general anesthesia, a CR combined with percutaneous adductor tenotomy was attempted in all cases, with the aid of arthrography and under fuoroscopic guidance. In Group A, when a concentric and stable reduction of the hip was not achieved, the CR was confirmed failed, and the procedure was immediately converted to OR during the same operative session through an anterior approach using the bikini incision. During the procedure, an iliopsoas tenotomy was routinely performed followed by a capsulorrhaphy including removal of the ligamentum teres and transection of the transverse acetabular ligament to create space for the reduction. Moreover, all of the soft tissue blockage in the acetabular fossa was removed so as to make the reduced hip more stable. In Group B, a delayed OR was performed after failed CR, and the operative techniques were the same as that used in Group A. All reductions were performed by one senior surgeon (J. S.).
After OR, the patients were immobilized in a 1.5 hip cast for six weeks, with the hips 30° fexion and 45° abduction. On postoperative day two, MRI examination was carried out to reconfirm the stable concentric reduction of the hips. After removal of the cast, the patients were required to wear a full-time (24 h/day) abduction orthosis for 12 weeks, and then to wear only at night time for 12 weeks. Patients were followed up regularly every 3-month interval within the first year, 6-month interval within the second year, and then yearly after the surgery up till skeletal maturity of the hips.
Outcome measures
At the last follow-up, the clinical outcomes were evaluated according to McKay’s criteria [8]. In all patiens, the antero-posterior X-ray films taken pre- and postoperatively till the final follow-up were evaluated for the acetabular index (AI), meanwhile, the degree of dislocation of the hips was categorized according to Tönnis grade [9] prior to OR. AVN of the femoral head was assessed using the Kalamchi and McEwen classification system [10], among which only grades II-IV were considered significant and included in the analysis. The incidence of PO were also observed within the follow-up period.
Statistical analysis
Means and standard deviations were used for normally distributed continuous variables, and the medians were used for non-normally distributed continuous variables. Frequencies were used for categorical variables. Within groups, a paired t test was applied to compare continuous variables, while an independent Student’s t test was applied between groups. The chi-square test or the Fisher’s exact test was applied to compare categorical variables. A P value less than 0.05 was considered statistically significant. All data were analyzed utilizing IBM SPSS 26.0 (IBM Corp., Armonk, New York).
Results
All of the 95 unilateral DDH patients were followed. The median follow-up time was 51 months (range 25–93). There were 64 patients in Group A and 31 patients in Group B. No statistically significant differences between the two groups were found in terms of the mean age at failed CR, sex ratio, afected side, Tönnis grade prior to OR and follow-up duration (P > 0.05). Detailed clinical information of the study population is shown in Table 1.
The clinical outcomes were evaluated according to McKay’s criteria. At the last follow-up, 54 (84.4%) of the 64 hips in Group A and 26 (83.9%) of 31 hips in Group B were in excellent or good condition. The difference in the McKay classification between the two groups was not significant (P = 0.950) (Table 2). At failed CR, the mean AI was 36.19 ± 4.07° and 36.23 ± 4.46° in Group A and Group B respectively, and the difference was found no significant (P = 0.967). At the last follow-up, the AIs in both groups were significantly improved (P = 0.000 in Group A and P = 0.000 in Group B), and no significant difference was found between the two groups (21.13 ± 4.95° in Group A vs. 22.42 ± 4.75° in Group B, P = 0.229). However, at the time when OR was performed in Group B, the mean AI in Group A was significantly lower than that in Group B (31.06 ± 4.45° vs. 33.87 ± 4.12°, P = 0.004) (Table 3).
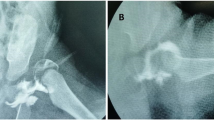
At the final follow-up, according to the Kalamchi and McEwen classification system, AVN of the femoral head was detected in 12 patients (12.6%). Among whom, nine (14.1%) cases in Group A (one case of grade II, four cases of grade III and four cases of grade IV) and in three (9.7%) cases in Group B (one case of grade II, one case of grade III and one case of grade IV). Seven patients (10.9%) in Group A and three patients (9.7%) in Group B underwent PO (Fig. 1). Although the incidence of PO and AVN in Group A were higher than those in Group B, no significant difference was found between the two groups (P > 0.05). (Table 4).
(a) A 17-month-old girl in Group B with right hip dislocation of Tönnis grade IV. (b) Image obtained 2 days after right hip open reduction. (c) Image obtained 6 months after open reduction showing AVN of grade I and acetabular dysplasia. (d) Follow-up images at 71 months of age showing right hip dysplasia
Discussion
The fundamental principle of DDH treatment is to achieve a stable and concentric reduction of the hip, so as to provide an optimal environment and facilitate the normal development of all structures of the hip, while avoiding complications such as AVN and early osteoarthrosis [1, 2, 11]. The management for DDH is largely related to the age of the child and the degree of bone deformity. It is generally accepted that the treatment of DDH should be performed as early as possible. The early the reduction, the better outcome. Because younger patients may be associated with a higher remodeling potential of the hip, and that the potential may decline with age. When degenerative joint disease present radiologically, the opportunity for preventative measures has been lost, and surgical intervention is the only option [1, 12]. Studies also demonstrated that early treatment may lead to a less difficult reduction and optimized development of the hip, with less further surgery requirement [11, 13].
OR is the preferred treatment option when CR failed [1, 5, 6, 14]. For patients who failed CR following failed PH treatment, the pathologic changes become more complex with age. Meanwhile, the treatment becomes more difficult [15]. The general trend in the literature is that younger DDH patients may have better outcomes after OR [11, 15,16,17]. However, the current published evidence for the treatment is still limited, and the optimal protocol for these patients remains unclear. To the best of our knowledge, there have been no published data comparing the efficacy of one- with two-stage OR in these patients up to now.
At the last follow-up, the majority of the patients achieved satisfactory results in both groups. Comparison between the two groups revealed that there were no differences in terms of McKay grading (P = 0.950), AI (P = 0.783), incidence of AVN (P = 0.745), and incidence of PO (P = 1.000). We therefore concluded that the outcome of one-stage OR was similar to that of two-stage OR. The results were consistent with previous reports [7, 18], also with many other studies concerning one-stage OR with or without femoral or pelvic osteotomy [15, 19,20,21].
Many authors have demonstrated the remarkable remodeling potential of the hip at early age of life [1, 16, 22, 23], and AI has proven to be the best parameter for evaluating the development of acetabulum, meanwhile associated with the remodeling potential [1, 24]. In the present study, we found a significant lower mean AI in Group A, when OR was performed in Group B. Which may be explained by the improvement of acetabular development following relatively early reduction in the one-stage OR group.
Conflicting evidence exists regarding the timing of OR in relation to the occurrence of AVN. Some authors noted that OR in younger patients is associated with a higher rate of AVN [11, 25,26,27], while others reported opposite results [13, 28, 29]. Also, there have studies reporting that age at the time of reduction had no effect on the incidence of AVN [30, 31]. Although the optimal timing of OR remains ambiguous, there is an increasing number of surgeons apply OR to treat DDH patients with decreasing age. In a study by Alves and colleagues [32], which is the largest and most comprehensive one to date, surveying DDH evaluation and management preferences among paediatric orthopaedic surgeons, the authors reported that 32% and 13% of the Pediatric Orthopaedic Society of North America (POSNA) members set the minimum age of OR at six months and 12 months, respectively. The corresponding data were 16% and 15% for European Paediatric Orthopaedic Society (EPOS) members. Our results showed that, although no significant difference was found, the incidence of PO and AVN in Group A were higher than those in Group B. However, the overall incidence of AVN in our series was 12.6%, which was relatively lower than that reported by many authors [27, 30, 33,34,35,36]. The developmental mechanism of AVN is multifactorial. Besides, for patients who failed CR, it is difficult to accurately attribute the occurrence of AVN to OR [2]. Therefore, further standardized, high-quality evidence is still required to clarify this complex problem.
As is well known, persistent acetabular dysplasia can lead to degenerative joint disease at a young age, and an appropriately selected pelvic osteotomy before any irreversible cartilage damage occurs could provide a biomechanically sound hip joint while prevent premature osteoarthritis of the hip. Several months of consideration of the legal guardians led to a delayed OR in Group B. Our results showed no significant difference regarding the incidence of PO between the two groups. Furthermore, the clinical outcomes including walking function were similar. However, because that the follow-up duration was not long enough, further research will be necessary to ascertain the true association between the time when OR was performed and the eventual outcome.
There are several limitations to this study. First, this was a retrospective study. Second, the sample sizes of Group B was relatively small. Third, this study only included unilateral DDH patients.
In summary, despite the limitations, this is the first study comparing the efficacy of one- with two-stage OR in DDH patients with failed CR following failed PH treatment up to now. Our findings suggested that both of the treatment protocols may acheive favorable outcomes. Moreover, one-stage OR is of without the general anesthesia risk associated with two-stage OR. We therefore advocate that an OR should be performed in appropriate DDH patients during the same session once a failed CR is detected.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Vaquero-Picado A, Gonzalez-Moran G, Garay EG, Moraleda L (2019) Developmental dysplasia of the hip: update of management. EFORT Open Rev 4:548–556. https://doi.org/10.1302/2058-5241.4.180019
Cooper AP, Doddabasappa SN, Mulpuri K (2014) Evidence-based management of developmental dysplasia of the hip. Orthop Clin North Am 45:341–354. https://doi.org/10.1016/j.ocl.2014.03.005
Kelley SP, Feeney MM, Maddock CL, Murnaghan ML, Bradley CS (2019) Expert-based Consensus on the principles of Pavlik Harness Management of Developmental Dysplasia of the hip. JB JS Open Access 4:e0054. https://doi.org/10.2106/JBJS.OA.18.00054
Arneill M, Cosgrove A, Robinson E (2021) Should closed reduction of the dislocated hip be attempted after failed Pavlik harness treatment in developmental dysplasia of the hip? Bone Jt Open 2:584–588. https://doi.org/10.1302/2633-1462.28.BJO-2021-0088.R1
Yang S, Zusman N, Lieberman E, Goldstein RY (2019) Developmental Dysplasia of the hip. Pediatrics 143. https://doi.org/10.1542/peds.2018-1147
Garcia S, Demetri L, Starcevich A, Gatto A, Swarup I (2022) Developmental Dysplasia of the hip: controversies in management. Curr Rev Musculoskelet Med 15:272–282. https://doi.org/10.1007/s12178-022-09761-8
Liu Y, Kan L, Sun J, Zhang Y (2022) Impact of failed Pavlik Harness Treatment on the outcomes following closed or open reduction in Developmental Dysplasia of the hip. Indian J Orthop 56:1634–1639. https://doi.org/10.1007/s43465-022-00680-x
McKay DW (1974) A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res 124–132. https://doi.org/10.1097/00003086-197401000-00013
Tönnis D (1990) Surgical treatment of congenital dislocation of the hip. Clin Orthop Relat Res 33–40
Kalamchi A, MacEwen GD (1980) Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am 62:876–888
Holman J, Carroll KL, Murray KA, Macleod LM, Roach JW (2012) Long-term follow-up of open reduction surgery for developmental dislocation of the hip. J Pediatr Orthop 32:121–124. https://doi.org/10.1097/BPO.0b013e3182471aad
Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL (2004) Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br 86:876–886. https://doi.org/10.1302/0301-620x.86b6.14441
Luhmann SJ, Bassett GS, Gordon JE, Schootman M, Schoenecker PL (2003) Reduction of a dislocation of the hip due to developmental dysplasia. Implications for the need for future surgery. J Bone Joint Surg Am 85:239–243. https://doi.org/10.2106/00004623-200302000-00009
Castañeda PG, Moses MJ (2019) Closed compared with Open Reduction in developmentally dislocated hips: a critical analysis review. JBJS Rev 7:e3. https://doi.org/10.2106/JBJS.RVW.18.00179
Forlin E, Munhoz da Cunha LA, Figueiredo DC (2006) Treatment of developmental dysplasia of the hip after walking age with open reduction, femoral shortening, and acetabular osteotomy. Orthop Clin North Am 37:149–160. https://doi.org/10.1016/j.ocl.2005.11.005. vi
Ganger R, Radler C, Petje G, Manner HM, Kriegs-Au G, Grill F (2005) Treatment options for developmental dislocation of the hip after walking age. J Pediatr Orthop B 14:139–150. https://doi.org/10.1097/01202412-200505000-00001
Castañeda P, Masrouha KZ, Ruiz CV, Moscona-Mishy L (2018) Outcomes following open reduction for late-presenting developmental dysplasia of the hip. J Child Orthop 12:323–330. https://doi.org/10.1302/1863-2548.12.180078
Ning B, Yuan Y, Yao J, Zhang S, Sun J (2014) Analyses of outcomes of one-stage operation for treatment of late-diagnosed developmental dislocation of the hip: 864 hips followed for 3.2 to 8.9 years. BMC Musculoskelet Disord 15:401. https://doi.org/10.1186/1471-2474-15-401
Jamil K, Saharuddin R, Abd Rasid AF, Abd Rashid AH, Ibrahim S (2022) Outcome of Open reduction alone or with Concomitant Bony Procedures for Developmental Dysplasia of the hip (DDH). Child (Basel) 9. https://doi.org/10.3390/children9081213
Ruszkowski K, Pucher A (2005) Simultaneous open reduction and Dega transiliac osteotomy for developmental dislocation of the hip in children under 24 months of age. J Pediatr Orthop 25:695–701. https://doi.org/10.1097/01.bpo.0000164877.97949.22
El-Sayed MM (2009) Single-stage open reduction, Salter innominate osteotomy, and proximal femoral osteotomy for the management of developmental dysplasia of the hip in children between the ages of 2 and 4 years. J Pediatr Orthop B 18:188–196. https://doi.org/10.1097/BPB.0b013e32832bf618
Pavlik A (1992) The functional method of treatment using a harness with stirrups as the primary method of conservative therapy for infants with congenital dislocation of the hip. 1957. Clin Orthop Relat Res:4–10
Cashman JP, Round J, Taylor G, Clarke NM (2002) The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up. J Bone Joint Surg Br 84:418–425. https://doi.org/10.1302/0301-620x.84b3.12230
Alassaf N (2020) Treatment of developmental dysplasia of the hip (DDH) between the age of 18 and 24 months. Eur J Orthop Surg Traumatol 30:637–641. https://doi.org/10.1007/s00590-019-02601-5
Apostolides M, Gowda SR, Roslee C, Beamish B, Burby N, Richards RH (2021) The presence of the ossific nucleus and its relation to avascular necrosis rates and the number of secondary procedures in late-presenting developmental dysplasia of the hip. J Pediatr Orthop B 30:139–145. https://doi.org/10.1097/BPB.0000000000000767
Clarke NM, Jowett AJ, Parker L (2005) The surgical treatment of established congenital dislocation of the hip: results of surgery after planned delayed intervention following the appearance of the capital femoral ossific nucleus. J Pediatr Orthop 25:434–439. https://doi.org/10.1097/01.bpo.0000158003.68918.28
Gardner RO, Bradley CS, Howard A, Narayanan UG, Wedge JH, Kelley SP (2014) The incidence of avascular necrosis and the radiographic outcome following medial open reduction in children with developmental dysplasia of the hip: a systematic review. Bone Joint J 96–B:279–286. https://doi.org/10.1302/0301-620X.96B2.32361
Bolland BJ, Wahed A, Al-Hallao S, Culliford DJ, Clarke NM (2010) Late reduction in congenital dislocation of the hip and the need for secondary surgery: radiologic predictors and confounding variables. J Pediatr Orthop 30:676–682. https://doi.org/10.1097/BPO.0b013e3181efb8c7
Hoellwarth JS, Kim YJ, Millis MB, Kasser JR, Zurakowski D, Matheney TH (2015) Medial versus anterior open reduction for developmental hip dislocation in age-matched patients. J Pediatr Orthop 35:50–56. https://doi.org/10.1097/BPO.0000000000000338
Firth GB, Robertson AJ, Schepers A, Fatti L (2010) Developmental dysplasia of the hip: open reduction as a risk factor for substantial osteonecrosis. Clin Orthop Relat Res 468:2485–2494. https://doi.org/10.1007/s11999-010-1400-y
Pospischill R, Weninger J, Ganger R, Altenhuber J, Grill F (2012) Does open reduction of the developmental dislocated hip increase the risk of osteonecrosis? Clin Orthop Relat Res 470:250–260. https://doi.org/10.1007/s11999-011-1929-4
Alves C, Truong WH, Thompson MV, Suryavanshi JR, Penny CL, Do HT, Dodwell ER (2018) Diagnostic and treatment preferences for developmental dysplasia of the hip: a survey of EPOS and POSNA members. J Child Orthop 12:236–244. https://doi.org/10.1302/1863-2548.12.180034
Isiklar ZU, Kandemir U, Ucar DH, Tumer Y (2006) Is concomitant bone surgery necessary at the time of open reduction in developmental dislocation of the hip in children 12–18 months old? Comparison of open reduction in patients younger than 12 months old and those 12–18 months old. J Pediatr Orthop B 15:23–27. https://doi.org/10.1097/01202412-200601000-00005
Ağuş H, Ömeroğlu H, Uçar H, Biçimoǧlu A, Türmer Y (2002) Evaluation of the risk factors of avascular necrosis of the femoral head in developmental dysplasia of the hip in infants younger than 18 months of age. J Pediatr Orthop B 11:41–46. https://doi.org/10.1097/01202412-200201000-00007
Qiu M, Chen M, Sun H, Li D, Cai Z, Zhang W, Xu J, Ma R (2022) Avascular necrosis under different treatment in children with developmental dysplasia of the hip: a network meta-analysis. J Pediatr Orthop B 31:319–326. https://doi.org/10.1097/BPB.0000000000000932
Novais EN, Hill MK, Carry PM, Heyn PC (2016) Is Age or Surgical Approach Associated with osteonecrosis in patients with Developmental Dysplasia of the hip? A Meta-analysis. Clin Orthop Relat Res 474:1166–1177. https://doi.org/10.1007/s11999-015-4590-5
Funding
This work was supported by the Natural Science Foundation of Anhui Province (Grant number 1808085MH288).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yong Liu, Lisheng Kan, Jie Huang, Jun Sun and Yapeng Zhang. The first draft of the manuscript was written by Lisheng Kan and Yong Liu commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
The Research Ethics Committee of the Affiliated Provincial Pediatric Hospital of Anhui Medical University has confirmed that no ethical approval is required.
Consent to participate
Written informed consent was obtained from patients.
Consent to publish
The authors affirm that the parents provided informed consent for publication of the present study.
Competing interests
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Y., Kan, L., Huang, J. et al. Open reduction after failed closed reduction following failed Pavlik harness treatment in developmental dysplasia of the hip: One- or two-stage?. Arch Orthop Trauma Surg 144, 1557–1563 (2024). https://doi.org/10.1007/s00402-024-05236-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05236-2