Abstract
Background
Mesenteric ischemia has remained without effective pharmacological management for many years. Sumatriptan, an abortive medication for migraine and cluster headaches, has potent anti-inflammatory properties and ameliorated organ ischemia in previous animal studies. Similarly, inhibition of the kynurenine pathway ameliorated renal and myocardial ischemia/reperfusion (I/R) in many preclinical studies. Herein, we assessed the effect of sumatriptan on experimental mesenteric I/R and investigated whether kynurenine pathway inhibition is a mechanism underlying its action.
Methods
Ischemia was induced by ligating the origin of the superior mesenteric artery (SMA) and its anastomosis with the inferior mesenteric artery (IMA) with bulldog clamps for 30 min. Ischemia was followed by 1 h of reperfusion. Sumatriptan (0.1, 0.3, and 1 mg/kg ip) was injected 5 min before the reperfusion phase, 1-methyltryptophan (1-MT) (100 mg/kg iv) was used to inhibit kynurenine production. At the end of the reperfusion phase, samples were collected from the jejunum of rats for H&E staining and molecular assessments.
Results
Sumatriptan improved the integrity of intestinal mucosa after I/R, and 0.1 mg/kg was the most effective dose of sumatriptan in this study. Sumatriptan decreased the increased levels of TNF-α, kynurenine, and p-ERK but did not change the decreased levels of NO. Furthermore, sumatriptan significantly increased the decreased ratio of Bcl2/Bax. Similarly, 1-MT significantly decreased TNF-α and kynurenine and protected against mucosal damage.
Conclusions
This study demonstrated that sumatriptan has protective effects against mesenteric ischemia and the kynurenine inhibition is potentially involved in this process. Therefore, it can be assumed that sumatriptan has the potential to be repurposed as a treatment for acute mesenteric ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute mesenteric ischemia refers to sudden disruption of the intestinal blood supply, which can lead to extensive intestinal necrosis if untreated. The only effective management for this condition is early surgical intervention. The occlusive type of acute mesenteric ischemia is usually seen among patients with atrial fibrillation or a hypercoagulable state. The non-occlusive type is more common in patients with myocardial infarction or other causes of cardiac insufficiency. Strangulation of a herniated bowel or venous thrombosis can also mimic mesenteric ischemia [1, 2]. Despite its rare incidence, acute mesenteric ischemia is an emergency and a serious cause of acute abdomen with a high mortality rate. Even after survival the consequences of short bowel, such as altered bowel habitus and malabsorption, impair patients’ quality of life [3].
Occlusion of the superior mesenteric artery (SMA) can reproduce mesenteric ischemia in animal models and has the most similarity to what happens in humans [4, 5]. In this study, mesenteric ischemia was induced by clamping the SMA and its anastomosis to the inferior mesenteric artery (IMA). Furthermore, to simulate the clinical settings, sumatriptan was administered after ischemia and the reperfusion phase was reduced to one hour since the surgeon must determine the extent of excision before abdominal wall closure.
Uncontrolled release of reactive oxygen species (ROS) and inflammatory cytokines, local activation of immune cells, particularly neutrophils, and overactivation of apoptotic signaling pathways are involved in the pathogenesis of acute mesenteric ischemia [6, 7]. In addition, gut microbiota infiltration can further deteriorate the inflammatory response and accelerate intestinal necrosis [6].
Kynurenine is an accessory metabolite of tryptophan. Indolamine 2,3-dioxygenase (IDO) is the main rate-limiting enzyme of the kynurenine pathway in the intestines [8, 9]. After being produced by IDO, kynurenine can be converted to various metabolites such as anthranilic acid, 3-hydroxykynurenine, 3-hydroxyanthrnilic acid, picolinic acid, and quinolinic acid [10]. Previously, it has been indicated that inhibition of different metabolites and enzymes of the kynurenine pathway can differently affect inflammatory bowel disease and colorectal cancer [10]. For instance, IDO activation has been protective against inflammatory bowel disease but enhanced tumorigenesis in the gastrointestinal tract. Additionally, it has been shown that IDO inhibition can protect against myocardial and renal ischemia in experimental studies [11, 12]. An elevated level of kynurenine was observed in intestinal inflammation [13]. Similarly, inflammatory factors such as interleukin. 1 (IL-1), interferon-gamma (IFN-γ), and tumor necrosis factor-alpha (TNF-α) can upregulate IDO. 1-Methyltryptophan (1-MT) is widely used as an IDO inhibitor in preclinical and clinical studies [10].
Sumatriptan, a serotonin receptor agonist, is the conventional drug for acute migraine attacks and cluster headaches [14]. Recent studies demonstrated that low-dose sumatriptan has significant anti-inflammatory properties [15, 16]. Sumatriptan can inhibit nuclear factor κB (NF-κB), suppress inflammatory cytokine release, prevent apoptosis, and enhance endogenous anti-oxidant defense [17, 18]. The routine doses of sumatriptan are contraindicated in vasospasm, peripheral arterial disease, angina pectoris, and bowel ischemia; however, there is insufficient information about low-dose sumatriptan or its application during acute mesenteric ischemia [14]. Moreover, low-dose sumatriptan exhibited promising effects in other animal models of organ ischemia such as myocardial ischemia, skin flap, and testicular torsion [15, 18, 19]. Recently, it has been found that signaling pathways activated by serotonin and kynurenine, two metabolites of tryptophan, have mutual interactions in the gastrointestinal tract [20]. Furthermore, the balance between serotonergic and kynurenine pathways has been implicated in the regulation of microbial composition, immune response, and inflammation in the intestines [20]. Hence, we investigated the effect of low-dose sumatriptan on mesenteric ischemia and measured the possible involvement of kynurenine.
Materials and methods
Animals
Thirty male Wistar rats, weighing 200–250 g, were purchased from the Pharmacology Research Center, Faculty of Medicine, Tehran University of Medical Sciences (TUMS). The animals were kept in a temperature-controlled room (23 ± 2 °C), with 55 ± 2% humidity and 12-h light/dark cycles with free access to food and water. The protocol of this project was approved by the ethics committee of the Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1399.664). All experiments were performed by the Guide for the Care and Use of Laboratory Animals (8th edition, 1996, National Academies Press published by National Academy Press, USA) and institutional guidelines for animal care and use (Department of Pharmacology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran). The total number of animals used in the experiment was 30. The animals were randomly divided into 5 groups (6 per group), including sham, control, and sumatriptan (0.1, 0.3, and 1 mg/kg, ip) [21]. 3–4 Specimens were then taken out randomly within the group for each of the molecular tests. The study began after the acclimatization lasting for 24 h. All efforts were made to minimize suffering. At the end of the study the animals were euthanized in a CO2 chamber.
Intestinal I/R induction and treatment schedule
In the sham group, after anesthesia with ketamine (85 mg/kg, Trittau Co., Germany, batch: 70,689) and xylazine 2% (15 mg/kg, alfasan, Woerden-Holland, batch: 1801005–02) and shaving, the abdominal wall was incised in the midline. Specimens were then collected from the jejunum. In other groups, after anesthesia and 5 min before laparotomy, the animals received a high dose of heparin due to the lack of concurrent angiographic interventions in this study (Caspian Tamin Rasht-Iran, Batch No; 031, 250 U per animal, intraperitoneal). After midline laparotomy and exposure of the intestinal loops, SMA was found and clamped near its origin. Similarly, the anastomosis between the SMA and the IMA was clamped. Several hallmarks, such as intestinal pallor, cyanosis, and dark bluish discoloration of supplying blood vessels and their tortuosity, were checked for confirming the accuracy of ischemia. After 30 min of ischemia, the clamps were reopened for reperfusion [21, 22]. The aforementioned changes were reversed in the reperfusion phase and the SMA and its branches quickly turned red as shown in Supplementary Fig. 1. Intestinal pallor was replaced by hyperemia, congestion, and redness. Reperfusion lasted for one hour and then specimens were collected from the jejunum. In both the ischemic and reperfusion phases, the intestinal loops were covered with wet sterile gas. Two samples were taken from each animal for histological staining and molecular assessments.
Sumatriptan (0.1, 0.3, and 1 mg/kg ip) was delivered 5 min before reopening the clamps, and 1-MT (100 mg/kg iv) was administered 15 min before sumatriptan. As our aim was treating mesenteric ischemia rather than its pretreatment, the drugs were used after ischemia.
Pathological assessment
Specimens were cut longitudinally to expose the luminal surface before fixation. One of the specimens of each rat’s jejunum was kept in formaldehyde at 4% and stained with H&E (hematoxylin and eosin) after tissue processing. An expert pathologist blinded to the groups interpreted the samples. Mucosal damage was assessed by Chiu’s histological scoring system (Table 1).
TNF-α levels measurement by ELISA
The specimens were snap-frozen after collection. Specimens were kept at – 80 °C until the assay. After homogenization, TNF-α was measured by sandwich ELISA. A DuoSet® Ancillary Reagent Kit was purchased to perform the measurement. High-quality bovine serum albumin (BSA) was used as a reagent diluent. The sandwich ELISA method was performed with rat TNF-α capture antibody and rat TNF-α detection antibody. First, 100 µL of sample or standard in reagent diluent was added to each well. Also, 100 µL of diluted detection antibody was added to each well. Likewise, other steps were performed according to the manufacturer’s instructions, and finally, the wavelength was set to 540 nm for reading the wells. TNF-α level measurement was done in triplicate for each group, and data are shown as mean ± SEM.
Kynurenine level measurement by colorimetric method and ELISA
A rat kynurenine (KYNU) ELISA kit (MBS745507) was purchased to measure kynurenine in intestinal tissue homogenate. The competitive enzyme immunoassay technique utilizing a polyclonal anti-KYNU antibody and a KYNU-HRP conjugate was applied. The intensity of color was read at 450 nm. Kynurenine level measurement was done in triplicate for each group and data are shown as mean ± SEM.
Griess test
The Griess test was utilized to measure nitrite (NO2−) levels in aqueous solutions of intestinal tissue based on the colorimetric method. Intestinal tissue was homogenized as described above and the supernatant was obtained and used to measure nitrite levels. Nitrite is the metabolite of nitric oxide (NO), and the Greiss test indirectly measures NO production. Distilled water treated with a mixed bed ion exchange resin or ultrapure (17 MW × cm or equivalent) water, was used as nitrite-free water. Griess reagent (catalog number G4410) was used for nitrite assay. Equal volumes of 1 × Griess Reagent and samples were mixed, and the absorbance was read at 540 nm after 20 min. The Griess test was done in triplicate for each group and data are shown as mean ± SEM.
Western blotting
After 1 h of reperfusion, intestinal specimens were collected for western blotting to evaluate anti-apoptotic factors such as Bcl2, pro-apoptotic proteins such as Bax, intra-cellular kinases such as phosphorylated extracellular signal-regulated kinase (p-ERK), and housekeeping protein glyceraldehyde-3-phosphate dehydrogenase (GAPDH). Each group in western blotting included two rats. The tissue specimens were homogenized in lysis buffer (including tris hydrochloric acid, ethylenedieamine tetraacetate (EDTA), NaCl, sodium dodecyl sulfate (SDS), sodium deoxycholate, NP40, protease inhibitor cocktail). The homogenate was centrifuged (Eppendorf 5415 R) at 12,000 g for 10 min at 4 °C. Then, the Bradford assay was done for calculating protein concentration in each sample. The running buffer included 1.5 g Tris, 1.5 g SDS, 7.2 g glycine, water up to 500 mL, and pH = 8.3. The samples were loaded on the SDS-PAGE and transferred (2.42 g Tris, 11.25 g glycin, 200 ml methanol, up to 1000 mL water) onto polyvinylidene difluoride (PVDF) membranes. Membranes were blocked with 2% non-fat skim milk for 75 min and incubated with the following primary antibodies overnight: p-ERK (Santa Cruz, sc-16981-R, 1:200), ERK (sc-292838), Bax (sc-7480), Bcl2 (Santa Cruz, sc-492, CA, USA 1: 200), and GAPDH (sc-32233, 1:1000). Membranes were then washed with TBST (TBS + tween 80) and incubated with secondary antibodies (mouse anti-rabbit IgG-HRP: sc-2357, 1:1000) for 75 min. BM chemiluminescence western blotting kit was used for detecting bands by gel doc [23]. Image J was used to determine the optical density of each band. The relative activity of p-ERK, Bcl-2, and Bax was calculated by Prism 7 (GraphPad Inc.) and compared with the control group.
Statistical analysis
Statistical analysis was performed using GraphPad Prism software (version 6.07). The homogeneity of variances and normal distribution of data were checked using a Brown-Forsythe test and a Shapiro–Wilk test, respectively. One-way analysis of variance (ANOVA) followed by Tukey’s post hoc test was used for normally distributed data. Kruskal–Wallis test followed by Dunn’s post hoc for multiple comparisons was performed for non-normal data. A p value < 0.05 was considered statistically significant.
Results
The effect of sumatriptan on intestinal histopathological alterations after I/R
Sumatriptan at a dose of 0.1 mg/kg ip) preserved the intestinal mucosa and prevented its destruction compared with the ischemic control. In particular, Kruskal–Wallis test and Dunn’s post hoc test revealed that sumatriptan significantly decreased Chiu score after I/R (H(3) = 9.18, p = 0.046) (Fig. 1).
Histological assessment of jejunum mucosa using H&E staining and Chiu score (scale 0–5). Ischemia/reperfusion deranged mucosal structure and reduced villous height in the ischemic control group (A). Images B–D illustrate the jejunum mucosa after treatment with sumatriptan (1 mg/kg, 0.3 mg/kg, and 0.1 mg/kg ip, respectively). Kruskal–Wallis test followed by Dunn’s post hoc test; n = 4. *p < 0.05 compared with the ischemic control group. H&E hematoxylin and eosin
Sumatriptan downregulated kynurenine
Kynurenine levels were measured to determine any possible interactions between sumatriptan and kynurenine pathways. I/R markedly increased kynurenine levels in the intestinal tissue compared with the sham group. Kruskal–Wallis and Dunn’s post hoc tests showed that kynurenine levels were significantly decreased after sumatriptan 0.3 mg/kg, ip, (H(4) = 15.21, p = 0.01), compared with the ischemic control group (Fig. 2a).
A Kynurenine levels in intestinal tissue measured by ELISA. Compared with the sham group, ischemia/reperfusion increased kynurenine levels. Sumatriptan (0.3 mg/kg ip) significantly decreased kynurenine levels, compared with the ischemic control group. Data are presented as medians and interquartile ranges; n = 4. Kruskal–Wallis test followed by Dunn’s post hoc. B TNF α levels in intestinal tissue measured by ELISA. Ischemia/reperfusion notably increased TNF-α levels, while sumatriptan decreased it. Data are presented as means ± SEM; n = 3. One-way ANOVA followed by post hoc Tukey’s tests. C Ischemia/reperfusion significantly decreased NO metabolites measured via the Griess test, but sumatriptan did not cause a significant change in NO levels.. Data are shown as mean ± SEM; n = 3. One-way analysis of variance (ANOVAs) followed by post hoc Tukey’s tests were used for comparisons. @p < 0.05, @@p < 0.01, @@@p < 0.001, and @@@@p < 0.0001 compared with the sham group. *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001 compared with the ischemic control group. NO Nitric oxide, TNF-α tumor necrosis factor-alpha
TNF-α levels were decreased after treatment with sumatriptan
TNF-α was assessed to determine the potential anti-inflammatory effect of sumatriptan on intestinal I/R. One-way ANOVA and post hoc Tukey’s tests indicated that compared with the sham group, I/R significantly increased the tissue levels of TNF-α (p = 0.0000). Compared with the ischemic control group, administration of sumatriptan 0.1 mg/kg (p = 0.0000), 0.3 mg/kg (p = 0.0004), and 1 mg/kg (p = 0.0002), ip, significantly decreased TNF-α levels (F4,10 = 31.97, df = 10) (Fig. 2b).
Nitric oxide was downregulated after I/R and remained unchanged after treatment with sumatriptan
ANOVA and post hoc Tukey’s tests showed that compared with the sham group, I/R injury significantly decreased the concentration of nitrite metabolites in the tissue homogenates (p = 0.001, F4,10 = 17.01, df = 10). Administration of sumatriptan (0.1, 0.3 and 1 mg/kg, ip) could not change the tissue levels of nitrite metabolites (Fig. 2c).
Sumatriptan upregulated Bcl2 and downregulated p-ERK and Bax in intestinal I/R
The effects of sumatriptan on p-ERK/GAPDH and Bcl2/Bax ratios are shown in Fig. 3. Kruskal–Wallis and post hoc Dunn’s tests revealed that compared with the ischemic control group, sumatriptan (0.1 mg/kg, ip) significantly increased Bcl2/Bax ratio (H(4) = 16.32, p = 0.001). In addition, Kruskal–Wallis and post hoc Dunn’s tests revealed that sumatriptan (0.1 mg/kg, ip) significantly reduced the p-ERK/GAPDH ratio (H(4) = 12.83, p = 0.035).
The relative expression of p-ERK, Bcl2, Bax, and GAPDH in intestinal tissue measured by Western blotting. Compared with the sham group, ischemia/reperfusion reduced Bcl2/Bax ratio, and sumatriptan ( 0.1 mg/kg ip) strongly increased it. Ischemia/reperfusion increased p-ERK level, and sumatriptan (0.1 mg.kg ip) decreased it. Data are shown as median and interquartile ranges; (n = 3–4). Kruskal–Wallis followed by post hoc Dunn’s test was used for comparisons. @p < 0.05, @@p < 0.01, @@@p < 0.001, and @@@@p < 0.0001 compared with the sham group. *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001 compared with the ischemic control group. p-ERK phosphorylated extracellular signal-regulated kinase
The effects of 1-MT on intestinal I/R
The effects of sumatriptan 0.1 mg/kg, ip (B), 1-MT 100 mg/kg, iv (C), and sumatriptan 0.1 mg/kg, ip + 1-MT 100 mg/kg, iv (D) on the intestinal mucosa is shown via H&E staining in Fig. 4. Kruskal–Wallis and Dunn’s post hoc tests indicated that sumatriptan (0.1 mg/kg, ip) significantly decreased the Chiu’s score after I/R injury (H(3) = 8.56, p = 0.045) (Fig. 4).
Histological assessment of jejunum mucosa using H&E staining and Chiu score (scale 0–5). Ischemia/reperfusion severely damaged mucosal structure and reduced villous height in the control group (A). Images B, C, and D illustrate the jejunum mucosa after treatment with sumatriptan (0.1 mg/kg, ip), 1-MT (100 mg/kg, iv), and a combination of sumatriptan (0.1 mg/kg, ip) + 1-MT (100 mg/kg, iv), respectively. Sumatriptan (0.1 mg/kg, ip) maintained mucosal integrity. Significance was determined using the Kruskal–Wallis test followed by Dunn’s post hoc test, n = 4. *p < 0.05 compared with the ischemic control group. H&E hematoxylin and eosin, 1-MT 1-methyltryptophan
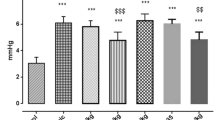
The effects of 1-MT on intestinal I/R
The effects of 1-MT (100 mg/kg, iv), sumatriptan (0.1 mg/kg, ip) and a combination of 1-MT (100 mg/kg, iv) + sumatriptan (0.1 mg/kg, ip) were assessed and depicted in Fig. 5. Kruskal–Wallis and Dunn’s post hoc tests revealed that the combination of 1-MT (100 mg/kg iv) and sumatriptan (0.1 mg/kg, ip) was significantly effective in reducing kynurenin (H(4) = 12.64, p = 0.006) and TNF-α (H(4) = 17.40, p = 0.025) levels. ANOVA and post hoc Tukey’s tests revealed that compared with the ischemic control group, sumatriptan (0.1 mg/kg, ip) (F3,8 = 99.00, p < 0.0001) and the combination of 1-MT (100 mg/kg, iv) and sumatriptan (0.1 mg/kg, ip) (F3,8 = 99.00, p < 0.0001), significantly increased Bcl2/Bax ratio (Fig. 5).
Relative levels of Bcl2/Bax, TNF-α, and kynurenine after treatment with 1-MT and sumatriptan, assessed by Western blotting. n = 3 rats per group. Compared with the ischemic control group, kynurenine, and TNF-α levels were reduced after administration of 1-MT (100 mg/kg iv), sumatriptan (0.1 mg/kg ip), and their combination. For TNF-α and kynurenine, data are shown as median with interquartile ranges, analyzed via Kruskal–Wallis test with Dunn’s post hoc. For Bcl2/Bax, data are shown as mean ± SEMand analyzed using one-way ANOVA followed by post hoc Tukey’s test; n = 3. Bcl2/Bax levels remained unchanged with 1-MT compared with the ischemic control group. *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001 compared with the ischemic control group. TNF-α tumor necrosis factor-alpha, and 1-MT 1-methyltryptophan
Discussion
The present study investigated the effects of low-dose sumatriptan on acute mesenteric ischemia. The results demonstrated that sumatriptan ameliorates mucosal damage induced by acute mesenteric ischemia. Further, sumatriptan alleviates inflammation, attenuated apoptosis, and downregulated ERK phosphorylation and kynurenine production.
Intestinal ischemia is associated with the uncontrolled release of numerous inflammatory mediators. These factors, including ROS, inflammatory cytokines, nitric oxide, and lytic enzymes, severely damage intestinal mucosa [24]. Reperfusion provides oxygen and supplements for the half-dead intestine; however, it can also intensify inflammation. Reperfusion can recruit neutrophils to the ischemic intestine. This phenomenon accelerates inflammation and apoptosis [25,26,27]. Thus, it is expected that ischemia and reperfusion cause inflammation and induce apoptosis, as indicated in our results.
Hypoxia affects many signaling pathways, and the subsequent innate immune response aggravates the inflammatory response [26, 28]. TNF-α is a critical cytokine in the progression of hypoxia and apoptosis. Enhanced expression of this cytokine is associated with the forthcoming breakdown of intestinal mucosa [29]. In addition to enhancing the inflammatory response, TNF-α is responsible for activating the external pathway of apoptosis [30]. TNF-α activates caspase 8 and subsequent executive caspases [31, 32], characterized by decreased Bcl2/Bax ratio. A higher Bcl2/Bax ratio can enhance cell survival and improve the outcome of I/R injury [33]. In the present study, sumatriptan 0.1 mg/kg could markedly decrease TNF-α and thereby increase the Bcl2/Bax ratio, preserving the epithelial cells of the intestine. In a previous study on oral mucositis in rats, sumatriptan 0.3 mg/kg could alleviate the mucosal inflammation and apoptosis [23]
As mentioned previously, higher kynurenine levels are found during inflammation [34, 35]. Several inflammatory mediators, especially INF-γ, can stimulate the expression of IDO in an inflammatory context [36]. It was observed that kynurenine level increases proportionate to intestinal endoscopic inflammation [37]. Increased IDO activity usually stimulates an anti-inflammatory response; however, it almost always prognosticates the poor condition of the disease. A recent systematic review showed that stroke and cerebral ischemia activates the kynurenine pathway. Interestingly, there was a positive correlation between kynurenine pathway activation and the severity of clinical outcomes such as cognitive impairments [38]. This could be explained by the fact that the kynurenine pathway can produce toxic end-metabolites in I/R [39]. In the current study, we have shown that kynurenine level peaked after mesenteric I/R, and downregulation of it was protective in this disease.
In a recent study on a murine model of chronic stress, an elevated concentration of 5-HT was observed in the hippocampal tissue of the mice, following a treatment which affected the kynurenine pathway [40]. This indicates the negative correlation between serotonin and kynurenine; approving the role of sumatriptan in downregulation of kynurenine, as a serotonergic agonist. Moreover, in our study, low-dose sumatriptan significantly reduced both kynurenine and TNF-α levels, showing that the drug exerts its effects via this pathway. Finally, 1-MT, as an IDO inhibitor, mimics the effects of sumatriptan in reducing kynurenine and TNF-α, further confirming the involvement of the kynurenine pathway.
In our study, Bcl2/Bax ratios were not changed via 1-MT, even though it resembled the effects of sumatriptan in the other experiments. This could be explained considering studies mentioning that the effects of 1-MT on apoptosis may be controversial [41]. A recent study on 1-MT isomers revealed that the protective effects of the molecule on renal ischemia could be through other mechanisms than the Kynurenine/IDO pathway [42]. As a result, the effects of 1-MT on the Bcl2/Bax pathway of apoptosis need further investigation.
I/R activates ERK [43]. ERK inhibition ameliorated renal, hepatic, and spinal cord I/R [44,45,46]. Similarly, intestinal I/R was shown to activate ERK [47]. Also, alleviation of intestinal injury was associated with decreased ERK phosphorylation [47]. Activated ERK can potentiate NF-κB-mediated inflammatory response and mucosal cell damage in intestinal I/R [48]. In addition, ERK promotes neutrophil infiltration into the inflamed intestine by upregulating adhesion molecules [49]. Based on our results, sumatriptan decreased phosphorylated ERK, as another mechanism of intestinal cells’ protection. This negative correlation between serotonin and ERK has been previously reported as well [50].
Intestinal I/R is associated with impaired NO production, mainly due to inducible nitric oxide synthase (iNOS) overactivity, which is harmful. In contrast, intestinal I/R suppresses the protective function of neuronal nitric oxide synthase (nNOS) and endothelial nitric oxide synthase (eNOS). This dysregulation of the NO system deteriorates the outcome of ischemia [51,52,53]. Our study could not prove that sumatriptan alters total NO production in intestinal I/R; nevertheless, the activity of the mentioned enzymes was not measured separately in the present work, In a previous study on mice, chronic administration of sumatriptan (0.1 mg/kg, ip) could alter NO levels, while the acute form did not, consistent with the results of the present study [54].
Using a rat model of mesenteric I/R, this study has shown that low-dose sumatriptan and 1-MT are effective pharmacological managements for mesenteric ischemia; however, more studies are needed to fully dissect the underlying mechanisms. More signaling pathways and inflammatory mediators could be measured. In addition, the effect of sumatriptan or 1-MT could be measured on different durations of ischemia. It is also needed to assess the effect of sumatriptan or 1-MT after a longer duration of reperfusion. Moreover, the kynurenine pathway has many metabolites and enzymes, which were not targeted in this study. Future clinical trials are recommended to investigate the effects of sumatriptan and 1-MT as pharmacological management of acute mesenteric ischemia.
Conclusions
Taken together, sumatriptan protected against mucosal damage after acute mesenteric ischemia. Sumatriptan decreased TNF-α levels and prevented apoptosis. Interestingly, sumatriptan decreased kynurenine production, indicating the possible role of the kynurenine pathway in the protective effect of sumatriptan. As kynurenine levels surged with mesenteric I/R, it has the potential to serve as a diagnostic or prognostic tool in the future. Possible relationship between the tryptophan and kynurenine pathways could be of interest for future investigations, yielding a complete picture of the whole pathway. Future studies are needed to further explore the efficacy and underlying mechanisms of sumatriptan and 1-MT in ameliorating acute mesenteric I/R.
Limitations
The sample size used in the present preclinical study was rather small which made it impossible to use the optimal statistical methods. Furthermore, kynurenine pathway has several enzymes and metabolites and we focused exclusively on the inhibition of IDO and kynurenine. Consequently, future studies should explore the role of different components of the kynurenine pathway in mesenteric I/R injury.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request. Western blot images are included in Supplementary materials.
Abbreviations
- eNOS:
-
Endothelial nitric oxide synthase
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- H&E:
-
Hematoxylin and Eosin
- IDO:
-
Indolamine 2,3-dioxygenase
- IFN-γ:
-
Interferon-gamma
- IL-1:
-
Interleukin 1
- IMA:
-
Inferior mesenteric artery
- iNOS:
-
Inducible nitric oxide synthase
- ip:
-
Intraperitoneally
- iv:
-
Intravenously
- I/R:
-
Ischemia/reperfusion
- 1-MT:
-
1-Methyltryptophan
- nNOS:
-
Neuronal nitric oxide synthase
- p-ERK:
-
Phosphorylated extracellular signal-regulated kinase
- SMA:
-
Superior mesenteric artery
- ROS:
-
Reactive oxygen species
- TNF-α:
-
Tumor necrosis factor-alpha
References
Stoney RJ, Cunningham CG. Acute mesenteric ischemia. Surgery. 1993;114:489–90.
Trompeter M, Brazda T, Remy CT, Vestring T, Reimer P. Non-occlusive mesenteric ischemia: etiology, diagnosis, and interventional therapy. Eur Radiol. 2002;12:1179–87.
Kärkkäinen JM, Acosta S. Acute mesenteric ischemia (part I)–incidence, etiologies, and how to improve early diagnosis. Best Pract Res Clin Gastroenterol. 2017;31:15–25.
Sağıroğlu T, Oğuz S, Sağıroğlu G, Çopuroğlu E, Yalta T, Sayhan MB, et al. The effects of apelin on mesenteric ischemia and reperfusion damage in an experimental rat model. Balkan Med J. 2012;29:148.
Jacob T, Ascher E, Hingorani A, Kallakuri S. Glycine prevents the induction of apoptosis attributed to mesenteric ischemia/reperfusion injury in a rat model. Surgery. 2003;134:457–66.
Bertoni S, Ballabeni V, Barocelli E, Tognolini M. Mesenteric ischemia-reperfusion: an overview of preclinical drug strategies. Drug Discov Today. 2018;23:1416–25.
Demiryas S, Orhan A. Redox status in age-related acute mesenteric ischemia. In: Redox signaling and biomarkers in ageing. Cham: Springer; 2022. p. 385–412.
Wolf AM, Wolf D, Rumpold H, Moschen AR, Kaser A, Obrist P, et al. Overexpression of indoleamine 2, 3-dioxygenase in human inflammatory bowel disease. Clin Immunol. 2004;113:47–55.
Martin-Gallausiaux C, Larraufie P, Jarry A, Béguet-Crespel F, Marinelli L, Ledue F, et al. Butyrate produced by commensal bacteria down-regulates indolamine 2, 3-dioxygenase 1 (IDO-1) expression via a dual mechanism in human intestinal epithelial cells. Front Immunol. 2018;9:2838.
Ala M. Tryptophan metabolites modulate inflammatory bowel disease and colorectal cancer by affecting immune system. Int Rev Immunol. 2022;41:326–45.
Eleftheriadis T, Pissas G, Golfinopoulos S, Liakopoulos V, Stefanidis I. Role of indoleamine 2, 3-dioxygenase in ischemia-reperfusion injury of renal tubular epithelial cells. Mol Med Report. 2021;23:1–13.
Melhem NJ, Chajadine M, Gomez I, Howangyin KY, Bouvet M, Knosp C, et al. Endothelial cell indoleamine 2, 3-Dioxygenase 1 Alters cardiac function after myocardial infarction through kynurenine. Circulation. 2021;143:566–80.
Clarke G, McKernan DP, Gaszner G, Quigley EM, Cryan JF, Dinan TG. A distinct profile of tryptophan metabolism along the kynurenine pathway downstream of toll-like receptor activation in irritable bowel syndrome. Front Pharmacol. 2012;3:90.
Brar Y, Saadabadi A. Sumatriptan. StatPearls [Internet]: StatPearls Publishing; 2019.
Dehdashtian A, Afshari K, Jazaeri SZ, Haddadi N-S, Sheikhi M, Abbaszadeh-Kasbi A, et al. Sumatriptan Increases skin flap survival through activation of 5-Hydroxytryptamine 1b/1d receptors in rats: the mediating role of the nitric oxide pathway. Plast Reconstr Surg. 2019;144:70e-e77.
Haddadi N-S, Foroutan A, Shakiba S, Afshari K, Ostadhadi S, Daneshpazhooh M, et al. Attenuation of serotonin-induced itch by sumatriptan: possible involvement of endogenous opioids. Arch Dermatol Res. 2018;310:165–72.
Khalilzadeh M, Panahi G, Rashidian A, Hadian MR, Abdollahi A, Afshari K, et al. The protective effects of sumatriptan on vincristine-induced peripheral neuropathy in a rat model. Neurotoxicology. 2018;67:279–86.
Dejban P, Rahimi N, Takzare N, Jahansouz M, Dehpour AR. Protective effects of sumatriptan on ischaemia/reperfusion injury following torsion/detorsion in ipsilateral and contralateral testes of rat. Andrologia. 2019;51: e13358.
Sheibani M, Faghir-Ghanesefat H, Dehpour S, Keshavarz-Bahaghighat H, Sepand MR, Ghahremani MH, et al. Sumatriptan protects against myocardial ischaemia–reperfusion injury by inhibition of inflammation in rat model. Inflammopharmacology. 2019;27:1071–80.
Haq S, Grondin JA, Khan WI. Tryptophan-derived serotonin-kynurenine balance in immune activation and intestinal inflammation. FASEB J. 2021;35: e21888.
Gharishvandi F, Abdollahi A, Shafaroodi H, Jafari RM, Pasalar P, Dehpour AR. Involvement of 5-HT1B/1D receptors in the inflammatory response and oxidative stress in intestinal ischemia/reperfusion in rats. Eur J Pharmacol. 2020;882: 173265.
Parlar A, Arslan SO. Resveratrol normalizes the deterioration of smooth muscle contractility after intestinal ischemia and reperfusion in rats associated with an antioxidative effect and modulating tumor necrosis factor alpha activity. Ann Vasc Surg. 2019;61:416–26.
Ala M, Jafari RM, Ala M, Agbele AT, Hejazi SM, Tavangar SM, et al. Sumatriptan alleviates radiation-induced oral mucositis in rats by inhibition of NF-kB and ERK activation, prevention of TNF-α and ROS release. Arch Oral Biol. 2020;119: 104919.
Chen H, Min X-H, Wang Q-Y, Leung FW, Shi L, Zhou Y, et al. Pre-activation of mesenchymal stem cells with TNF-α, IL-1β and nitric oxide enhances its paracrine effects on radiation-induced intestinal injury. Sci Rep. 2015;5:1–14.
Cuzzocrea S, Chatterjee PK, Mazzon E, Dugo L, De Sarro A, Van de Loo FAJ, et al. Role of induced nitric oxide in the initiation of the inflammatory response after postischemic injury. Shock. 2002;18:169–76.
Cerqueira NF, Hussni CA, Yoshida WB. Pathophysiology of mesenteric ischemia/reperfusion: a review. Acta Cir Bras. 2005;20:336–43.
Welbourn CRB, Goldman G, Paterson IS, Valeri CR, Shepro D, Hechtman HB. Pathophysiology of ischaemia reperfusion injury: central role of the neutrophil. Br J Surg. 1991;78:651–5.
Ito H, Sadatomo A, Inoue Y, Yamada N, Aizawa E, Hishida E, et al. Role of TLR5 in inflammation and tissue damage after intestinal ischemia-reperfusion injury. Biochem Biophys Res Commun. 2019;519:15–22.
la Garza FJG-d, Ibarra-Hernandez JM, Cordero-Perez P, Villegas-Quintero P, Villarreal-Ovalle CI, Torres-Gonzalez L, et al. Temporal relationship of serum markers and tissue damage during acute intestinal ischemia/reperfusion. Clinics. 2013;68:1034–8.
Kim JJ, Lee SB, Park JK, Yoo YD. TNF-α-induced ROS production triggering apoptosis is directly linked to Romo1 and Bcl-X L. Cell Death Differ. 2010;17:1420–34.
Günther C, Martini E, Wittkopf N, Amann K, Weigmann B, Neumann H, et al. Caspase-8 regulates TNF-α-induced epithelial necroptosis and terminal ileitis. Nature. 2011;477:335–9.
Wang L, Du F, Wang X. TNF-α induces two distinct caspase-8 activation pathways. Cell. 2008;133:693–703.
Liu Y-Q, Liu Y-F, Ma X-M, Xiao Y-D, Wang Y-B, Zhang M-Z, et al. Hydrogen-rich saline attenuates skin ischemia/reperfusion induced apoptosis via regulating Bax/Bcl-2 ratio and ASK-1/JNK pathway. J Plast Reconstr Aesthet Surg. 2015;68:e147–56.
Van der Leek AP, Yanishevsky Y, Kozyrskyj AL. The kynurenine pathway as a novel link between allergy and the gut microbiome. Front Immunol. 2017;8:1374.
Wang Q, Liu D, Song P, Zou M-H. Tryptophan-kynurenine pathway is dysregulated in inflammation, and immune activation. Front Biosci (Landmark Ed). 2015;20:1116–43.
Grant RS, Naif H, Espinosa M, Kapoor V. IDO induction in IFN-γ activated astroglia: a role in improving cell viability during oxidative stress. Redox Rep. 2000;5:101–4.
Sofia MA, Ciorba MA, Meckel K, Lim CK, Guillemin GJ, Weber CR, et al. Tryptophan metabolism through the kynurenine pathway is associated with endoscopic inflammation in ulcerative colitis. Inflamm Bowel Dis. 2018;24:1471–80.
Delevati Colpo G, Venna VR, McCullough LD, Teixeira AL. Systematic review on the involvement of the kynurenine pathway in stroke: pre-clinical and clinical evidence. Front Neurol. 2019;10:778.
Zheng X, Zhang A, Binnie M, McGuire K, Webster SP, Hughes J, et al. Kynurenine 3-monooxygenase is a critical regulator of renal ischemia–reperfusion injury. Exp Mol Med. 2019;51:1–14.
Deng Y, Zhou M, Wang J, Yao J, Yu J, Liu W, et al. Involvement of the microbiota-gut-brain axis in chronic restraint stress: disturbances of the kynurenine metabolic pathway in both the gut and brain. Gut Microbes. 2021;13:1–16.
Lee J-W, Oh JE, Rhee K-J, Yoo B-S, Eom YW, Park SW, et al. Co-treatment with interferon-γ and 1-methyl tryptophan ameliorates cardiac fibrosis through cardiac myofibroblasts apoptosis. Mol Cell Biochem. 2019;458:197–205.
Čepcová D, Kema IP, Sandovici M, Deelman LE, Šišková K, Klimas J, et al. The protective effect of 1-methyltryptophan isomers in renal ischemia-reperfusion injury is not exclusively dependent on indolamine 2, 3-dioxygenase inhibition. Biomed Pharmacother. 2021;135: 111180.
Zhang J, Xia J, Zhang Y, Xiao F, Wang J, Gao H, et al. HMGB1-TLR4 signaling participates in renal ischemia reperfusion injury and could be attenuated by dexamethasone-mediated inhibition of the ERK/NF-κB pathway. Am J Transl Res. 2016;8:4054.
Pan G-Z, Yang Y, Zhang J, Liu W, Wang G-Y, Zhang Y-C, et al. Bone marrow mesenchymal stem cells ameliorate hepatic ischemia/reperfusion injuries via inactivation of the MEK/ERK signaling pathway in rats. J Surg Res. 2012;178:935–48.
Ye Q, Zhu YI, Ye S, Liu H, She X, Niu Y, et al. Gypenoside attenuates renal ischemia/reperfusion injury in mice by inhibition of ERK signaling. Exp Ther Med. 2016;11:1499–505.
Lu K, Cho C-L, Liang C-L, Chen S-D, Liliang P-C, Wang S-Y, et al. Inhibition of the MEK/ERK pathway reduces microglial activation and interleukin-1-beta expression in spinal cord ischemia/reperfusion injury in rats. J Thorac Cardiovasc Surg. 2007;133:934–41.
Crisafulli C, Mazzon E, Galuppo M, Paterniti I, Caminiti R, Cuzzocrea S. Olprinone attenuates the development of ischemia/reperfusion injury of the gut. Intensive Care Med. 2010;36:1235–47.
Chen K, Xie W, Luo B, Xiao W, Teitelbaum DH, Yang H, et al. Intestinal mucosal barrier is injured by bmp2/4 via activation of nf-b signals after ischemic reperfusion. Mediat Inflamm. 2014;2014:1–11.
Mizuno R, Kamioka Y, Kabashima K, Imajo M, Sumiyama K, Nakasho E, et al. In vivo imaging reveals PKA regulation of ERK activity during neutrophil recruitment to inflamed intestines. J Exp Med. 2014;211:1123–36.
Takeda K, Tsuji M, Miyagawa K, Takeda H. 5-HT(7) receptor-mediated fear conditioning and possible involvement of extracellular signal-regulated kinase. Neurosci Lett. 2017;638:69–75.
Rivera LR, Pontell L, Cho H-J, Castelucci P, Thacker M, Poole DP, et al. Knock out of neuronal nitric oxide synthase exacerbates intestinal ischemia/reperfusion injury in mice. Cell Tissue Res. 2012;349:565–76.
Turan I, Ozacmak HS, Ozacmak VH, Barut F, Araslı M. Agmatine attenuates intestinal ischemia and reperfusion injury by reducing oxidative stress and inflammatory reaction in rats. Life Sci. 2017;189:23–8.
Drucker NA, Jensen AR, te Winkel JP, Markel TA. Hydrogen sulfide donor GYY4137 acts through endothelial nitric oxide to protect intestine in murine models of necrotizing Enterocolitis and intestinal ischemia. J Surg Res. 2019;234:294–302.
Hassanipour M, Rajai N, Rahimi N, Fatemi I, Jalali M, Akbarian R, et al. Sumatriptan effects on morphine-induced antinociceptive tolerance and physical dependence: the role of nitric oxide. Eur J Pharmacol. 2018;835:52–60.
Funding
This study was financially supported by the Experimental Medicine Research Center, Tehran University of Medical Sciences, Tehran, Iran [Grant No 99-2-209-48776] and Iran National Science Foundation (INSF) (Grant No. 96002757).
Author information
Authors and Affiliations
Contributions
MA performed surgery and procedures, wrote the manuscript, and analyzed data; MRFK performed surgery; RMJ performed Western blotting, edited the manuscript, and conceptualized the project; MS performed molecular assay; SG analyzed the data and wrote the manuscript, MAS determined the surgery procedure; ARD conceived study as the principal investigator and supervised. All authors studied and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
43440_2023_470_MOESM1_ESM.tif
Supplementary Fig 1. The typical macroscopic changes of the intestines during mesenteric I/R, including intestinal pallor, cyanosis, and dark bluish discoloration of supplying blood vessels and their tortuosity. Supplementary file1 (TIF 1057 KB)







Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ala, M., Fallahpour Khoshdel, M.R., Mohammad Jafari, R. et al. Low-dose sumatriptan improves the outcome of acute mesenteric ischemia in rats via downregulating kynurenine. Pharmacol. Rep 75, 623–633 (2023). https://doi.org/10.1007/s43440-023-00470-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-023-00470-8