Abstract
Purpose
This study aimed to determine the radiographic outcomes of patients with cerebral palsy (CP) who underwent posterior spinal fusion from T2/3 to L5 at two quaternary hospitals.
Methods
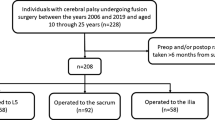
From January 2010 to January 2020, 167 non-ambulatory patients with CP scoliosis underwent posterior spinal fusion using pedicle screws from T2/3 to L5 in both centers, with a minimum of 2 years follow-up (FU). Radiological measurements and chart reviews were performed.
Results
A total of 106 patients aged 15.6 ± 0.4 years were included. None of the patients was lost to FU. All patients had significant correction of the Cobb angle (MC) and pelvic obliquity (PO), thoracic kyphosis (TK), and lumbar lordosis (LL), without loss of correction at the last FU (LFU). The mean values for preoperative, immediate postoperative, and LFU were MC 93.4°, 37.5°, and 42.8°; PO 25.8°, 9.9°, and 12.7°; TK 52.2°, 44.3°, and 45°; and LL − 40.9°, − 52.4°, and − 52.9°, respectively. Higher residual PO at LFU was associated with more severe MC and PO baselines, lower implant density, and an apex located at L3.
Conclusions
CP scoliosis and PO can be corrected, and this correction is maintained over time with posterior spinal fusion using pedicle screws, with L5 as the lowest instrumented vertebra. Larger preoperative MC and PO values associated with the apex at L3 appear to be related to residual PO. Comparative large-scale studies of patient-related clinical outcomes are required to determine whether this intervention is associated with improved surgical outcomes and reduced complication rates.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgery for scoliosis in non-ambulatory patients with cerebral palsy (CP) can be challenging. Even if the benefits are clear for them and their caregivers [1, 2], frailty [3] and complications [4,5,6,7,8,9] must be considered.
The benefits of fusing the pelvis versus selecting L5 as the lowest instrumented vertebra (LIV) in these patients remain unclear [10,11,12]. There is a wide spectrum of advantages and disadvantages on both sides.
Pelvic fixation (PF) could provide better long-term pelvic obliquity (PO) correction and better sitting position [13,14,15]. The main postulated risks are increased surgical time, blood loss, and infections [16, 17].
Setting L5 as the LIV should have a shorter surgical time and less bleeding, thereby decreasing the risk of complications. In addition, leaving a mobile disc may potentially allow for easier transfers or sitting and compensation if the pelvic obliquity remains [10,11,12, 18].
However, satisfaction and improvement in quality of life seem to be unrelated to the degree of deformity correction [19] in these patients, making the decision to fix the pelvis even more complex.
This study aimed to evaluate the radiological outcomes of a homogenous cohort of non-ambulatory patients with CP treated with posterior instrumented fusion using pedicle screws from T2-3 to L5 between 2010 and 2020 at two quaternary hospitals.
We analyzed correction in Cobb angle and PO and how these values are maintained over time to determine whether ending instrumentation at L5 can be an option for these patients.
Materials and methods
After IRB GOSH3034 institutional approval, all patients with confirmed CP diagnosis and Gross Motor Functional Classification Scale (GMFCS) grades IV and V, treated by posterior instrumented fusion (PSF) between the 1st of January 2010 and the 31st of December 2020, were retrospectively assessed in the electronic patient record systems for inclusion in both quaternary level treating hospitals.
The inclusion criteria were age between 10 and 18 years, scoliosis > 50°, PSF as the primary surgery with fusion from T2–3 to L5, at least 2 years of follow-up (FU), complete FU, and medical and radiological records.
We excluded patients with incomplete records, when X-ray measurements could not be performed, FU shorter than 2 years, and surgeries other than primary PSF.
As per the institutions’ traditions, all patients are treated by PSF using L5 as the LIV. All surgeries were performed by five senior spinal surgeons working in both hospitals.
Radiographic measurements using anteroposterior and lateral sitting radiographs were performed at three time points: preoperative, immediate postoperative (once the patient could sit in the wheelchair), and LFU by a senior spine surgeon (RAMC) not involved in the surgeries and a senior spinal fellow. In case of a discrepancy, a randomized surgeon from the five involved in the surgeries was asked to assess the X-rays. The final average of the three measurements was used.
The evaluated parameters were main curve Cobb (MC), PO using Maloney’s method [20], L1 to S1 lumbar lordosis (LL), and T1–T12 thoracic kyphosis (TK). Curve type was classified using Lonstein classification [21] and the apex was evaluated for the main curve. Other sagittal alignment parameters were not evaluated due the non-ambulatory condition of these patients, the poor visibility of pelvic landmarks due to pelvic obliquity and poor bone quality, and the lack of consensus in the literature about this analysis in CP patients [22].
L5 tilt was defined as the angle between the superior end plate of L5 and the crestal line.
Radiographs were obtained in Digital Imaging and Communication in Medicine (DICOM) format using a Picture Archiving and Communication System (PACS) and measured using the TraumaCad System (Brainlab®).
The primary outcomes were MC and PO correction and whether they were maintained at the LFU. Loss of correction was defined as a > 10° difference between the immediate postoperative and LFU radiographs.
Patient variables were obtained from electronic patient records. The reported variables included age, sex, weight, muscular tone, leg traction, number of fused levels, upper instrumented vertebra (UIV), implant density (screws per level), rod diameter (5.5 mm vs 6 mm), and rod material (titanium vs. cobalt chromium).
Length of stay (LOS) was defined as the duration of hospitalization related to primary surgery. Readmissions due to late complications that required further treatment after discharge were not included. The duration of admission to the pediatric intensive care unit (PICU) was counted for all days spent in the PICU during LOS, including readmissions during the primary hospitalization.
A standardized manual defining complications was used in both hospitals. Complications were classified as gastrointestinal, instrumentation related, medical, neurological, respiratory, surgical site infection, and death. Major complications were defined as reoperation, LOS prolongation, or life-threatening. If more than one complication occurred in the same patient, the major or most severe complication was considered as the overall rate.
Statistical analysis
Continuous variables are presented as mean and standard deviation (SD), and categorical variables are presented as absolute and relative frequencies based on the central limit theorem. Significant differences in categorical variables were determined using the Chi-square test.
Descriptive statistics were performed on demographic and clinical data. Normality of data distribution was determined using the D’Agostino and Pearson test and quantile–quantile plots. Significant differences in the correction parameters at the three specified time points were determined using one-way ANOVA tests corrected for multiple comparisons using Tukey’s test. Statistical significance was set at p < 0.05.
A dichotomized analysis was performed based on the PO value at LFU to evaluate whether there were differences in the baseline characteristics between the groups.
All statistical tests were performed using Prism 9.3.1c (GraphPad Software Inc., CA, USA). The study was performed according to the Preferred Reporting of CasE Series in Surgery (PROCESS) guidelines for case series studies [23].
Surgical technique
All patients underwent surgery on the Jackson table under total intravenous anesthesia and intraoperative multimodal neuromonitoring. Tranexamic acid was routinely administered at loading doses of 15 mgrs and 3 mg/kg/h during surgery. However, this was not maintained during the postoperative period. A cell saver was routinely used. Head traction was applied using Gardner tongs in all patients. Leg’s bilateral soft traction was used in patients without fixed hip contractures.
A midline incision and subperiosteal exposure were made until the pars interarticularis and inferior facets were visualized in the lumbar and thoracic spines, respectively. Screw placement was performed using freehand technique. Hooks were used when the anatomy was unfavorable for pedicle screws. Inferior and medial facetectomies (Schwab grade 1) [24] were performed at the latest stage to minimize bleeding, preserving the ligamentum flavum, and not exposing the dural sleeve. Various titanium screw systems have been used, changing over the last years from 5.5 to 6 mm titanium rods. Intraoperative fluoroscopy was used to confirm implant position and L5 coronal and sagittal orientation, aiming for a parallel L5–S1 disc space. Correction was achieved using rod bending, coronal and sagittal translation, and compression or distraction at the lowest levels. Final decortication and 80–120 cc of bone substitute (Pro Osteon, Zimmer Biomet®) were applied with 1 g vancomycin. The layers were closed without drains. A battery-operated negative pressure dressing (PICO, Smith-Nephew®) was used in all patients and kept in place until wound review on day three.
Patients were electively admitted to the pediatric intensive care unit (PICU) depending on the anesthetic assessment.
Results
A total of 167 patients with CP were treated with PSF from T2/T3–L5 at both hospitals within the specified timeframe. In total, 106 patients met the inclusion criteria. Most of the exclusions were related to a lack of complete data available from patient records or inadequate X-rays for measurements. None of the patients was lost to follow-up.
Population baseline is summarized in Table 1.
Mean surgical time (MST) was 221 ± 54.9 min, with an average of 15.6 ± 0.4 levels fused and implant density (ID) of 1.4 ± 0.17. Estimated blood loss (EBL) was 470 ± 373 cc (12.2 ± 9.7% of the estimated blood volume), and the length of stay (LOS) was 18 ± 53 days. Most patients (86, 81.1%) were electively admitted to the pediatric intensive care unit (PICU) with an average stay of 2.4 ± 7.6 days. One patient experienced severe complications, with an LOS of 558 days and a PICU stay of 78 days, including readmission.
Regarding surgery, 75 (70.7%) patients had T2 UIV, and in 52 (49.0%) leg traction was used, 5.5 mm in diameter (85 patients, 80.1%), and titanium rods (101 patients, 95.2%) were the most frequently used.
55 patients (51%) experienced at least one complication. Major complications occurred in 37 (34.9%) patients. Respiratory infections were the most frequent (24 cases, 22.6%), and surgical site infections occurred in seven patients (6.6%). None of the patients in this series required revision surgery because of mechanical complications, residual deformities, or progressive loss of correction.
Deformity correction
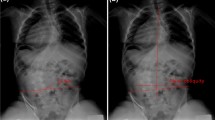
Table 2 summarizes the radiographic deformity baseline and Fig. 1a–d shows changes from preoperative, immediately postoperative, and at last follow-up for MC, PO, TK, and LL, respectively.
Cobb correction
Analysis of the mean correction and standard deviation (SD) showed that the mean Cobb angle improved significantly immediately after surgery from 93.4° (SD 1.7) to 37.5° (SD 1.6). The mean Cobb angle at LFU was 42.8° (SD 1.7). A Paired T Test indicated a significant postoperative improvement in MC of 55.8° (95% CI 50.1–61.4) (t = 23.2, df 210), p < 0.001. The difference between immediate postoperative measurements and LFU was 4.5° 95% CI [− 0.08 to − 9.23] (t = 1.9, df 210), and this difference was not significant (p = 0.054), demonstrating a stable correction over time.
Pelvic obliquity correction
When considering the mean correction and standard deviation (SD), the PO improved immediately after surgery, from 25.8° (SD 1.1) to 9.9° (SD 0.6). The PO at the LFU was 12.7° (SD 0.8). The mean difference before and after surgery was 15.8° 95% CI [12.9–18.0] (t = 11.9, df 210), p < 0.001, and between immediately after surgery and LFU was 2.7°, 95% CI [− 5 to 0.1] (t 2.7, df 210); p = 0.07), demonstrating that PO did not change significantly over the FU time.
Figure 2a–c shows a radiographic example of MC and PO correction from the preoperative to immediate postoperative and last follow-up.
Sagittal correction
Both thoracic kyphosis and lumbar lordosis showed significant improvement from baseline to the immediate postoperative period. This correction was maintained at < 10° for all variables in the FU.
TK improved from 52.2° (SD 2.4) to 44.3° (SD 1.6), (t = 2.9, df 210, p = 0041), at LFU 45° (SD 1.5) (t = 0.35, df 210, p = 0.7).
When evaluating LL, the improvement ranged from − 40.9° (SD 3.2) to − 52.4° (SD 1.3) (t = 3.3, df 210, p = 0.001). Correction at LFU was − 52.9° (SD 1.4) (t = 0.21, df 210, p = 0.828).
Group analysis
Table 3 summarizes the comparison between the groups using the cutoff PO value at LFU.
Demographics and intraoperative variables were similar between the two groups. When analyzing deformity, patients with higher residual PO at LFU had more severe MC and PO baselines, ID was lower with the apex at L3.
Discussion
The main goals of surgery in non-ambulatory patients with neuromuscular scoliosis are to avoid deformity progression and maintain an acceptable sitting position in the wheelchair while minimizing operative time, bleeding, and intra- and postoperative complications [25,26,27].
To improve the sitting position, it is important to correct scoliosis and PO [28, 29]. To the present, there is a lack of consensus in the literature regarding pelvic fixation (PF) for CP scoliosis surgery [10, 12, 16, 18]. The PO cutoff values for PF vary from publication, with a wide range oscillating from 10° [30], 15° [16, 30] to 20° [17, 30].
The expected benefits of avoiding PF include reduced operative time, bleeding, and complications, whereas the main potential risks are residual pelvic obliquity, progressive loss of correction, and revision surgery.
Our series presented a large and homogeneous population of patients with non-ambulatory GMFCS IV/V CP-only scoliosis treated exclusively with PSF from T2/3 to L5, with a mean FU of 5.2 years.
From our results, it appears that significant corrections in MC, TK, LL, and PO can be achieved, and that correction is maintained over time. Regarding PO, the mean value at LFU was 12.7°, which falls below the thresholds for PF of 15° and 20° published in literature.
Tøndevold et al. [18] compared 91 non-ambulatory patients with neuromuscular scoliosis treated using PSF in two different hospitals choosing the distal level at L5 or the pelvis by tradition. The mean preoperative PO were 25° and 14° in the L5 and PF groups, respectively. PO was significantly improved in the second group without an increased risk of complications, suggesting that PF should be performed in patients with preoperative coronal or sagittal imbalance. In their study, approximately 50% of the patients had diagnoses other than CP, which can play a role in deformity correction and maintenance, and it can be argued that PF with preoperative PO < 15° cannot always be required. In addition, it can sometimes be challenging to establish coronal or sagittal balance using sitting X-rays in non-ambulatory patients without trunk control. An interesting finding of this study was that the risk of complications related to PF was not significantly different between the groups.
Recently, Farshad et al. [12] evaluated 49 patients with neuromuscular scoliosis treated with PSF and selected an LIV at L5 or the pelvis. PF was indicated in non-ambulatory patients with a PO > 35°. In the subgroup analysis of 20 non-ambulatory patients with GMFCS IV/V, the PO at LFU in both groups was not significantly different, with mean values of 19° and 18°, respectively. Sitting balance and imbalance were also similar between the groups. The revision rate due to symptomatic residual or progressive PO did not increase in L5. They concluded that PF might not always be necessary in non-ambulatory patients, even with a preoperative PO of up to 35°.
Stiel et al. [17] published a series of 37 patients with neuromuscular scoliosis treated with PSF ending at L5 or the pelvis. In this study, the indication for PF was a PO > 20°. The main limitation of this study is the mixed etiology, including patients with low muscular tone (only 13 patients had CP) and some had combined approaches. Both these factors can influence the results. In this series, 21 patients underwent PSF with an LIV at L5. They reported significant PO correction, remaining within < 10° of the loss of correction at the LFU.
Interestingly, all the above-mentioned publications showed that MC significantly improves with the use of all pedicle screw fixations, without it being the same for PF and PO.
Regarding complications, our 34.9% of major complications is like the published rates for neuromuscular scoliosis correction with PF [5, 6, 9, 31], suggesting that avoiding PF might not be related to decreased overall complications rate.
If we analyze MST and EBL, our results show shorter operative time (mean 221 min) and less bleeding (mean 470 mL) compared to the series published by Tøndevold [18] (MST: 273 min, EBL 1300) and Stiel [17] (MST: 344 min, EBL 1530 ml). Even if these parameters seem to not increase the complication rate, this population certainly benefits from shorter surgeries with the minimum bleeding possible.
We do not have patient-reported outcome measurements (PROMs) during the FU period and this is a limitation of this study. No patient required revision surgery due to progressive sitting imbalance, pain, or skin problems like pressure sores. Accepting the limitations of these data, it seems that from the clinical perspective that the clinical improvement achieved with surgery was maintained over time.
Based on these findings, the main benefits of using L5 as LIV could be decreased surgical time, bleeding, and costs. However, further large comparative studies are required to identify the clinical relevance of these findings.
However, patients with an apex at L3 and more severe preoperative MC and PO are at risk of ending up within the higher end of the spectrum for PO at the LFU. These points should be carefully considered during surgical planning.
Strengths and limitations
We report the largest homogeneous series of patients with GMFCS grade IV/V CP treated only with PSF and L5 as the LIV, with the longest mean follow-up to date (at least 5.2 years).
The lack of functional or patient outcomes is a major limitation of this study, especially considering patients with residual PO from under-correction, in which stopping at L5 may not be the best option.
Recent publications suggest that improvement in quality of life after scoliosis surgery is not related to the degree of correction of MC or PO [2], and more clinical data in the future should help in understanding how residual pelvic obliquity can affect patients’ quality of life and impact global surgical outcomes.
Patients with severe preoperative MC, PO, and apex at L3 should be carefully evaluated owing to the risk of residual pelvic obliquity.
Conclusions
Our results showed that CP scoliosis and PO can be corrected, and this correction may be maintained over time with posterior spinal fusion using all pedicle screws, setting L5 as the lowest instrumented vertebra, independent of preoperative pelvic obliquity values. However, larger preoperative MC and PO values associated with the apex at L3 may be related to residual PO, thus emphasizing the relevance of preoperative planning in this group of patients.
It appears that avoiding PF is not related to a decreased risk of complications. The main advantages of avoiding PF could be shorter operative time, less bleeding, and lower costs.
Comparative large-scale studies of patient-related clinical outcomes are required to determine whether this intervention is associated with improved surgical outcomes and reduced complication rates.
References
Jain A et al (2018) Caregiver perceptions and health-related quality-of-life changes in cerebral palsy patients after spinal arthrodesis. Spine (Phila Pa 1976) 43(15):1052–1056
Miller DJ et al (2020) Improving Health-related quality of life for patients with nonambulatory cerebral palsy: who stands to gain from scoliosis surgery? J Pediatr Orthop 40(3):e186–e192
Miyanji F et al (2018) Assessing the risk-benefit ratio of scoliosis surgery in cerebral palsy: surgery is worth it. J Bone Joint Surg Am 100(7):556–563
Toll BJ et al (2021) Risk factors for proximal junctional kyphosis following surgical deformity correction in pediatric neuromuscular scoliosis. Spine (Phila Pa 1976) 46(3):169–174
Vandendriessche E et al (2021) Complication rate after scoliosis surgery in children with cerebral palsy. Acta Orthop Belg 87(2):255–261
Yaszay B et al (2020) Major complications following surgical correction of spine deformity in 257 patients with cerebral palsy. Spine Deform 8(6):1305–1312
Furdock R, Luhmann SJ (2020) The value of preoperative labs in identifying “at-risk” patients for developing surgical site infections after pediatric neuromuscular spine deformity surgery. Spine Deform 8(3):517–522
Luhmann SJ, Furdock R (2019) Preoperative variables associated with respiratory complications after pediatric neuromuscular spine deformity surgery. Spine Deform 7(1):107–111
Matsumoto M et al (2018) Perioperative complications in posterior spinal fusion surgery for neuromuscular scoliosis. Spine Surg Relat Res 2(4):278–282
Strom SF et al (2022) Is it necessary to fuse to the pelvis when correcting scoliosis in cerebral palsy? World J Orthop 13(4):365–372
Li Y et al (2022) Pelvic fixation is not always necessary in children with cerebral palsy scoliosis treated with growth-friendly instrumentation. Spine Deform 10(4):925–932
Farshad M et al (2022) Pelvic fixation in surgical correction of neuromuscular scoliosis. N Am Spine Soc J 10:100123
Tsirikos AI, Mains E (2012) Surgical correction of spinal deformity in patients with cerebral palsy using pedicle screw instrumentation. J Spinal Disord Tech 25(7):401–408
Wu Z et al (2021) Iliac screw instrumentation to the pelvis in children with neuromuscular and syndromic scoliosis. No lateral connectors and respect sagittal balance. Spine Deform 9(4):1115–1123
Nielsen E et al (2019) Don’t you wish you had fused to the pelvis the first time: a comparison of reoperation rate and correction of pelvic obliquity. Spine (Phila Pa 1976) 44(8):E465–E469
Suresh KV et al (2021) Spinal fusion with sacral alar iliac pelvic fixation in severe neuromuscular scoliosis. JBJS Essent Surg Tech 11(3):4
Stiel N et al (2020) Pedicle screw instrumentation with or without pelvic fixation in neuromuscular scoliosis: outcome and complications in a series of 37 patients with a minimum 2-year follow-up. Surgeon 18(5):e7–e12
Tondevold N et al (2020) Should instrumented spinal fusion in nonambulatory children with neuromuscular scoliosis be extended to L5 or the pelvis? Bone Joint J 102-B(2):261–267
Nordon DG et al (2017) Correlation between the degree of correction of neuromuscular scoliosis and patient quality of life. Clinics (Sao Paulo) 72(2):71–80
Shrader MW et al (2018) Inter- and intraobserver reliability of pelvic obliquity measurement methods in patients with cerebral palsy. Spine Deform 6(3):257–262
Lonstein JE, Akbarnia A (1983) Operative treatment of spinal deformities in patients with cerebral palsy or mental retardation. An analysis of one hundred and seven cases. J Bone Joint Surg Am 65(1):43–55
Ilharreborde B et al (2020) Spinal sagittal alignment and head control in patients with cerebral palsy. J Child Orthop 14(1):17–23
Agha RA et al (2018) The PROCESS 2018 statement: updating consensus preferred reporting of CasE series in surgery (PROCESS) guidelines. Int J Surg 60:279–282
Schwab F et al (2015) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 76(Suppl 1):S33-41
Willoughby KL et al (2022) Epidemiology of scoliosis in cerebral palsy: A population-based study at skeletal maturity. J Paediatr Child Health 58(2):295–301
Yoshida K et al (2018) Natural history of scoliosis in cerebral palsy and risk factors for progression of scoliosis. J Orthop Sci 23(4):649–652
Murphy RF, Mooney JF 3rd (2019) Current concepts in neuromuscular scoliosis. Curr Rev Musculoskelet Med 12(2):220–227
Loughenbury PR, Tsirikos AI (2022) Current concepts in the treatment of neuromuscular scoliosis: clinical assessment, treatment options, and surgical outcomes. Bone Jt Open 3(1):85–92
Cloake T, Gardner A (2016) The management of scoliosis in children with cerebral palsy: a review. J Spine Surg 2(4):299–309
Hasler C et al (2020) Spine deformities in patients with cerebral palsy; the role of the pelvis. J Child Orthop 14(1):9–16
Funk S et al (2016) Rigid instrumentation for neuromuscular scoliosis improves deformity correction without increasing complications. Spine (Phila Pa 1976) 41(1):46–52
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
RAMC: made substantial contributions to the conception, design, analysis, major revisions and interpretation of data; drafted and critically revised the work, approved the version to be published, and agrees to be accountable for all aspects of the work. JL, ST, MH: made substantial contributions to the analysis, and revision and interpretation of data; drafted and revised the work, approved the version to be published, and agree to be accountable for all aspects of the work. ST, TE, MH, EB: revised the work, approved the version to be published, and agree to be accountable for all aspects of the work. TE: made substantial contributions to the analysis and interpretation of data and revised the manuscript. EB: made substantial contributions to the design, analysis, revision, and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no competing interests to declare relevant to the content of this article.
Ethics approval
Ethical approval was waived by the local Ethics Committee of Great Ormond Street Hospital under the number GOSH3034 in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morales Ciancio, R.A., Lucas, J., Tucker, S. et al. Distal level in scoliosis surgery for non-ambulatory patients with cerebral palsy: is L5 an option? A case series study. Spine Deform 11, 1467–1475 (2023). https://doi.org/10.1007/s43390-023-00722-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00722-w