Abstract
Objective
Mobilizing out of bed and ambulation are key components of recovery following posterior spinal fusion (PSF) for adolescent idiopathic scoliosis (AIS). However, there remains a paucity of studies identifying risk factors associated with delayed ambulation and its impact on postoperative outcomes. The aim of this study was to investigate patient- and surgical-level risk factors associated with delayed ambulation and the ramifications of delayed ambulation on healthcare utilization for patients undergoing PSF for AIS.
Methods
The medical records of 129 adolescent (10–18 years) patients diagnosed with AIS undergoing posterior spinal fusion at a major academic institution between 2013 and 2020 were reviewed. Patients were categorized based on days from surgery to ambulation: early (≤ 1 day), intermediate (2 days), or late (≥ 3 days). Patient demographics, comorbidities, spinal deformity characteristics, intraoperative variables, postoperative complications, LOS, and unplanned readmissions were assessed. The odds ratios for risk-adjusted delayed ambulation and extended LOS were determined via multivariate stepwise logistic regressions.
Results
One Hundred and Twenty Nine patients were included in this study, of which 10.8% (n = 14) were classified as Early ambulators, 41.9% (n = 54) Intermediate ambulators, and 47.3% (n = 61) were Late ambulators. Late ambulators were significantly younger than early and intermediate ambulators (Early: 15.7 ± 1.9 years vs. Intermediate: 14.8 ± 1.7 years vs. Late: 14.1 ± 1.9 years, p = 0.010). The primary and secondary spinal curves were significantly worse among Late ambulators (p < 0.001 and p = 0.002 respectively). Fusion levels (p < 0.01), EBL (p = 0.014), and the rate of RBC transfusions (p < 0.001) increased as time to ambulation increased. Transition time from IV to oral pain medications (Early: 1.6 ± 0.8 days vs. Intermediate: 2.2 ± 0.6 days vs. Late: 2.4 ± 0.6 days, p < 0.001) and total hospital length of stay (Early: 3.9 ± 1.4 days vs. Intermediate: 4.7 ± 0.9 days vs. Late: 5.1 ± 1.2 days, p < 0.001) were longer in Late ambulators. On multivariate analysis, significant predictors of delayed ambulation included primary curve degree ≥ 70° [aOR: 5.67 (1.29‒31.97), p = 0.030] and procedure time [aOR: 1.66 (1.1‒2.59), p = 0.019].
Conclusions
Our study suggests that there may be patient- and surgical-level factors that are independently associated with late ambulation following PSF for AIS, including extent of major curve and length of operative time. Additionally, delayed ambulation has implications to length of hospital stay and postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With a prevalence of roughly 5% in the United States, adolescent idiopathic scoliosis (AIS) is a relatively common spinal pathology that costs the healthcare system upwards of $500 million annually [1]. Although bracing may be utilized in minor cases of AIS, surgical management is typically required for more severe curvatures [2]. Posterior spinal fusion (PSF) is the mainstay approach for corrective surgery, which has significant implications such as blood loss, postoperative complications, extended hospital stays, and unplanned readmissions [2,3,4,5]. Previously identified risk factors for poorer outcomes after PSF for AIS include obesity, pulmonary diseases, anemia, and affective disorders [3, 4, 6,7,8]. Investigation of additional risk factors is important to improve patient outcomes and decrease unnecessary healthcare expenditures.
One aspect of postoperative recovery for patients undergoing PSF is early mobilization and ambulation. Previous studies have suggested that ambulation later in the postoperative course may be associated with inferior surgical outcomes [9]. For example, in an institutional retrospective cohort study of 136 patients undergoing elective PSF for AIS from 2012 to 2018, Knight et al. demonstrated on binominal logistic regression analysis that decreased ambulation distance was significantly predictive of postoperative complications such as urinary retention [9]. However, there remains an overall paucity of studies that identify risk factors associated for delayed ambulation and its impact on postoperative outcomes.
The aim of this study was to investigate patient- and surgical-level risk factors associated with delayed ambulation and the ramifications of delayed ambulation on healthcare utilization for patients undergoing PSF for AIS.
Methods
The electronic medical records of 194 adolescent (10–18 years) with spinal deformity undergoing elective posterior spinal fusion at a major academic institution between 2013 and 2020 were retrospectively reviewed. Patients with a diagnosis of AIS were included, while those diagnosed with congenital, syndromic, and neuromuscular scoliosis were excluded. Timing of post-operative ambulation was defined by documented ambulation by the inpatient Physical Therapy team. Patients were categorized based on postoperative day (POD) of ambulation: early ambulators (POD 0 or 1), intermediate ambulators (POD 2), and late ambulators (POD ≥ 3) which was defined as the 75th percentile of the entire cohort. The primary outcome investigated in this study was the risk factors associated with delayed ambulation following surgery. Approval from the Institutional Review Board was obtained prior to study initiation.
Baseline characteristics and demographic variables assessed included gender, age, ethnicity, race, and body mass index (BMI) as defined by patient height and weight at the time of surgery. Co-morbidities included affective disorder, defined by diagnosis of depression and/or anxiety, attention deficit disorder (ADD), attention deficit hyperactivity disorder (ADHD), autism spectrum disorder, congenital heart defect, anemia, obesity, hypothyroidism, seizure disorder, gastroesophageal reflux disease (GERD), eczema, number of allergies. Obesity was defined by a BMI at or above the 95th percentile of age-, gender-, and race-specific growth charts defined by the Centers for Disease Control and Prevention [10]. Anemia was defined using age-, gender-, and race-defined hemoglobin values [11, 12]. Pre-operative lab values collected at most one month before surgery included hematocrit (%), hemoglobin (g/dL), platelets (x1000µL), creatine (g/dL), and albumin (g/dL). Deformity characteristics included degree and orientation of the major and secondary curve of scoliosis, defined by the preoperative standing scoliosis x-ray. The secondary curve was defined by the second largest curve measured on x-ray.
Intraoperative variables included the number of fused vertebral levels, osteotomies performed, estimated blood loss (EBL), estimated blood volume (EBV) loss, and blood products given, including packed red blood cells (RBC), platelets and fresh frozen plasma (FFP), cell saver, and albumin. Other intraoperative variables included administration of tranexamic acid (TXA) and aminocaproic acid (AMICAR), and procedure time. Intraoperative complications considered were spinal cord injury, durotomy, changes in neuromonitoring. The assistance of a plastic surgeon on closure, drain insertion, and administration of intrathecal opioids was also recorded.
Postoperative physical therapy (PT) variables included pain reported on the first day of physical therapy following surgery, number of steps taken on the first day of ambulation following surgery and on the final day of physical therapy before discharge were recorded. Pain scores were assessed by PT at time of mobilization and categorized as none/mild, moderate/severe, or not specified if no pain information was recorded. Additionally, transition time from intravenous to oral analgesics were also recorded. Post-operative adverse events included fever (> 37° C), persistent tachycardia, hypertension, hypotension, anemia, blood transfusions, atelectasis, ileus, and urinary retention. Post-operative hematocrit (%) and hemoglobin (g/dL) collected within 24 h of surgery were included. Other post-operative variables included length of stay in the pediatric intensive care unit (PICU), total hospital length of stay (LOS), discharge disposition (home vs. home with home services), and unplanned readmission within 30 days of discharge.
Statistical analysis
Nominal variables were compared with Chi-square or, test if at least 20% of the cells had counts < 5, with Fisher’s exact test. The Shapiro–Wilk normality test was used to determine the normality of continuous variables. Parametric data were expressed as means ± standard deviation (SD) and compared via Student’s t-test while nonparametric data was expressed as median [interquartile range] and compared with the Mann–Whitney U test. Delayed ambulation and extended LOS were defined as greater than the 75th percentile of the entire cohort (3 and 5 days, respectively). Univariate and multivariate regressions were fitted with delayed ambulation and extended LOS as the outcome variables to calculate odds ratio (OR) or adjusted odds ratio (aOR), respectively. Inclusion criteria for univariate regression analysis was a p-value < 0.20 between cohorts in previous statistical analysis. For model optimization of the multivariable regression, a reverse feature elimination stepwise regression was used. Inclusion and stay criteria for multivariate analysis was a p-value < 0.20. To address plausible confounding, patient age and sex were forced into the multivariate regression. Delayed ambulation was forced into the multivariate regression for extended LOS. A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using R Studio, Version 1.4.1717, RStudio, PBC, Boston, MA.
Results
Patient demographics and comorbidities
A total of 129 patients were included in this study, of which 10.9% were categorized as early ambulators (n = 14), 41.9% were found to be intermediate ambulators (n = 54), and 47.3% were identified as late ambulators (n = 61), Table 1. Late ambulators were significantly younger than the other cohorts (Early: 15.7 ± 1.9 years vs. Intermediate: 14.8 ± 1.7 years vs. Late: 14.1 ± 1.9 years, p = 0.010), Table 1. The three cohorts were similarly matched in gender (Early: 78.6% female vs. Intermediate: 70.4% female vs. Late: 83.6% female, p = 0.236), race (p = 0.763), and BMI (Early: 22.1 ± 3.0 kg/m2 s vs. Intermediate: 22.6 ± 4.6 kg/m2 vs. Late: 21.7 ± 3.8 kg/m2, p = 0.544), Table 1. Prevalence of comorbidities including ADD/ADHD, asthma, anemia, hypothyroidism, eczema, and number of allergies did not differ between the three cohorts, Table 1.
Deformity characteristics
Primary curve (Early: 56.8 ± 8.6° vs. Intermediate: 57.8 ± 9.0° vs. Late: 64.0 ± 12.1°, p < 0.001) and secondary curve magnitude (Early: 40.1 ± 12.4° vs. Intermediate: 42.7 ± 12.5° vs. Late: 49.1 ± 12.1°, p = 0.002) was significantly greater in the late ambulation cohort, Table 2. Additionally, primary curve flexibility was similar between the cohorts (Early: 50.7 ± 17.3% vs. Intermediate: 55.8 ± 16.3% vs. Late: 51.1 ± 16.2%, p = 0.828) there was no significant difference between the primary (p = 0.616) or secondary curve orientation (p = 0.789), or Risser stage (p = 0.057) between the three cohorts, Table 2.
Intraoperative variables
The median [IQR] number of spinal levels fused during surgery (Early: 12.0 [9.5–12.8] vs. Intermediate: 12.0 [11.0–13.0] vs. Late: 13.0 [12.0–13.0], p < 0.001), procedure time (Early: 5.8 ± 1.3 h vs. Intermediate: 6.6 ± 1.1 h vs. Late: 7.2 ± 1.3 h, p < 0.001), EBL.
(Early: 775.0 ± 565.0 mL vs. Intermediate: 1011.0 ± 428.0 mL vs. Late: 1159.0 ± 517.0 mL, p = 0.014), EBV loss (Early: 19.8 ± 12.0% vs. Intermediate: 25.8 ± 12.9% vs. Late: 33.3 ± 18.2%, p = 0.001), transfusions of RBC (Early: 14.3% vs. Intermediate: 48.1% vs. Late: 73.8%, p < 0.001), administration of albumin (Early: 28.6% vs. Intermediate: 59.3% vs. Late: 73.8%, p < 0.01), and administration of intrathecal opioids (Early: 57.1% vs. Intermediate: 86.8% vs. Late: 93.3%, p < 0.01) were increased with Late ambulation, Table 3. There was a significant difference in drain use among the three cohorts (p < 0.001), Table 3. There were no significant differences in performance of thoracoplasty (p = 0.570), mean implant density (p = 0.735), osteotomies performed (p = 0.075), platelet/FFP transfusions (p = 0.527), cell saver transfusions (p > 0.99), administration of TXA (p = 0.102), or administration of AMICAR (p = 0.229), Table 3.
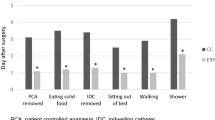
Post-operative pain and physical therapy
Transition time from IV analgesics to oral pain medications significantly increased with Late ambulators (Early: 1.6 ± 0.8 days vs. Intermediate: 2.2 ± 0.6 days vs. Late: 2.4 ± 0.6 days, p < 0.001), Table 4. The pain reported before the first session of PT after surgery was not significantly different between the three cohorts (p = 0.603), Table 4. The number of steps on the first day of ambulation after surgery significantly increased with Late ambulators (Early: 40.0 ± 44.0 steps vs. Intermediate: 82.0 ± 104.0 steps vs. Late: 117.0 ± 96.4 steps, p < 0.01), Table 4. There was no difference between the cohorts in the maximum number of steps taken before discharge (p = 0.181), Table 4.
Truncal and shoulder balance
Both preoperative and postoperative truncal and shoulder balance were similar between cohorts. Preoperatively, a greater proportion of Intermediate and Late ambulators had right sided truncal elevation compared to Early ambulators, though this difference was not statistically significant (Early: 30.8% vs. Intermediate: 44.4% vs. Late: 44.3%, p = 0.911), Table 5. Similarly, mean truncal balance was similar between cohorts (Early: 6.0 ± 5.3 mm vs. Intermediate: 6.1 ± 5.1 mm vs. Late: 6.9 ± 7.3 mm, p = 0.996), Table 5. Additionally, mean shoulder height balance was similar between cohorts (Early: 9.4 ± 8.0 mm vs. Intermediate: 7.9 ± 6.4 mm vs. Late: 10.5 ± 9.4 mm, p = 0.509), Table 5. Postoperatively, mean truncal balance was similar between cohorts (Early: 6.7 ± 5.4 mm vs. Intermediate: 6.3 ± 6.9 mm vs. Late: 4.9 ± 5.3 mm, p = 0.481), as was mean shoulder height balance (Early: 12.0 ± 13.4 mm vs. Intermediate: 12.3 ± 12.8 mm vs. Late: 13.0 ± 9.7 mm, p = 0.525), Table 5. Additionally, while primary curve percent correction was similar between cohorts (Early: 73.2 ± 11.7 vs. Intermediate: 72.2 ± 10.4 vs. Late: 73.2 ± 9.1, p = 0.860), secondary curve percent correction increased with time to ambulation (Early: − 59.4 ± 22.0 vs. Intermediate: -65.7 ± 17.3 vs. Late: -70.6 ± 11.0, p = 0.034), Table 5. There was no significant difference in unplanned 30-day hospital readmission rates between the cohorts (p > 0.99), Table 5. The driver for readmission for Intermediate cohort patient was diarrhea from Clostridioides difficile; and for the Late cohort were pneumonia and wound dehiscence.
Post-operative complications and healthcare resource utilization
Rates of postoperative persistent tachycardia significantly increased with Late ambulators (Early: 14.3% vs Intermediate: 46.3% vs Late: 52.5%, p = 0.035), while rates of other postoperative complications including fever (p = 0.091), anemia (p = 0.412), blood transfusion (p = 0.578) atelectasis (p = 0.67), hypotension (p = 0.843), hypertension (p = 0.644), ileus (p = 0.233), and urinary retention (p > 0.99) were not significantly different between the cohorts, Table 6. Total hospital length of stay increased as time to ambulation increased (Early: 3.9 ± 1.4 days vs. Intermediate: 4.7 ± 0.9 days vs. Late: 5.1 ± 1.2 days, p < 0.001), Table 6.
Univariate and multivariate regression for delayed ambulation
On univariate analysis, independent predictors of delayed ambulation included lower age, primary curve degree ≥ 70 degrees, secondary curve degree ≥ 50 degrees, ≥ 13 spinal levels fused, EBL, RBC transfusion, albumin transfusion, procedure time, and intrathecal opioid use, Table 7. Increasing Risser stage was inversely associated with delayed ambulation on univariate analysis, Table 7. However, on multivariate analysis, the only independent predictors of delayed ambulation were primary curve degree ≥ 70 degrees [aOR: 5.67 (1.29‒31.97), p = 0.030] and procedure time [aOR: 1.66 (1.1‒2.59), p = 0.019], Table 7.
Discussion
In this retrospective, single institutional study of 129 pediatric patients undergoing elective PSF for AIS, we demonstrate that increased major curve degree and procedure time were significantly associated with delayed ambulation following PSF for AIS.
While there is a paucity of studies within the AIS patient population, there has been prior literature that have attempted to identify patient- and surgical-level risk factors associated with delayed ambulation following adult spine surgery. In a retrospective matched cohort study of 23,295 patients undergoing elective lumbar spine surgery between 2015 and 2018, Zakaria et al. showed that age, gender, race, comorbidities, insurance status, previous spine surgery, levels fused, and surgery duration were all significantly associated with early versus late ambulation [13]. In studies that have analyzed ambulation differences in AIS patient population, the factors identified varied. For instance, in an institutional retrospective cohort study of 56 patients undergoing PSF for AIS between 1999 and 2007, Sugarman et al. demonstrated that patients in the all-pedicle screw group mobilized out of bed significantly earlier than patients in the hybrid instrumentation group [14]. In our study, we demonstrated that the extent of the major curve and procedure time were significantly associated with delayed postoperative ambulation. However, given the relative paucity of studies, further investigation is needed to verify these results and better characterize their impact on delayed ambulation to better optimize preoperative expectations and patient care.
While the impact of delayed ambulation on patient outcomes has been limited in the AIS population, this has been investigated in other areas of adult spinal surgery. In the Zakaria et al. study of 23,295 patients undergoing lumbar spine surgery, the authors demonstrated that late ambulation was significantly associated with increased LOS and higher rates of non-routine discharge, 30- and 90-day readmission, postoperative urinary retention, UTI, and ileus [13]. In an another institutional retrospective cohort study of 285 patients undergoing elective surgical correction of adult spinal deformity between 2010 and 2017, Oe et al. demonstrated on multiple logistic regression analysis that a greater number of days to ambulation was a significant independent predictor of medical complications [15]. Our study similarly found that delayed ambulation may have implications on length of hospital stay and postoperative complications. Therefore, it is important to fully elucidate the impact of delayed ambulation following surgery on patient outcomes so as to develop risk-stratification protocols to improve patient care.
The negative impact of delayed ambulation on clinical outcomes and healthcare utilization has led many researchers to investigate ERAS protocols to expedite ambulation and mobilization postoperatively. In a systematic review and meta-analysis of 2456 patients from 14 studies undergoing surgical correction of AIS, Koucheki et al. showed that patients in the ERAS protocol cohort reached first ambulation roughly 30 h earlier than those in the traditional discharge cohort [16]. Further, in an institutional retrospective cohort study of 72 patients undergoing PSF for idiopathic scoliosis from 2013 and 2015, Kim et al. demonstrated that patients in the new protocol consisting of a Perioperative Surgical Home ambulated significantly earlier than those in the old, traditional care protocol [17]. The effect on surgical outcomes of ERAS protocols that expedite ambulation following PSF for AIS has also been studied. In an institutional quality improvement project including 322 patients undergoing PSF for AIS from 2011 to 2015, Muhly et al. demonstrated that the implementation of a rapid recovery protocol emphasizing early postoperative mobilization led to a decrease in mean hospital LOS from 5.7 days to 4.0 days. [18] Similarly, in a retrospective monocentric observational study performed on 163 patients who underwent surgical correction of AIS between 2015 and 2018, Julien-Marsollier et al. found that the implementation of an ERAS protocol with early mobilization shortened median hospital LOS by 3 days and significantly decreased post-operative constipation rates [19]. ERAS protocols therefore have the potential to markedly improve surgical outcomes for patients undergoing PSF for AIS, and their use should be considered in this every candidate within this patient population.
This study has several limitations with potential implications for study interpretation. First, although all variables were recorded preoperatively, perioperatively, and postoperatively, they were reviewed retrospectively, and, as such, are limited by the weaknesses inherent to retrospective analyses. Second, we were limited to what was available in the medical charts, and therefore the recorded data may be inaccurately recorded, such as patient diagnoses, complications, and reasons for clinical decision making. Thirdly, during this time period there were variations in intraoperative and postoperative protocols practices such as intrathecal morphine, pain regiment, threshold for blood transfusion may have implications on our findings. Fourthly, preoperative and postoperative patient reported outcomes and quality surveys were not employed which may have provided insight for our findings. Finally, a relatively small patient sample size from only a single academic center was used, making broad conclusions difficult, potentially biasing our results for particular patient populations or treatment paradigms. Furthermore, there was heterogeneity in the number of cases per surgeon at the institution, therefore practices intraoperatively and postoperatively may vary and have implications on our findings. Despite these limitations, this study sheds light onto the impact that delayed ambulation has on adolescent patients undergoing posterior spinal fusion for adolescent idiopathic scoliosis.
Conclusion
Our study suggests that there may be patient- and surgical-level factors that are independently associated with late ambulation following PSF for AIS, including extent of major curve and length of operative time. Additionally, delayed ambulation has implications to length of hospital stay and postoperative complications. Further studies are necessary to identify protocols to increase postoperative ambulation after PSF for AIS.
Data availability
Not applicable.
Code availability
Not applicable.
References
Jada A, Mackel CE, Hwang SW et al (2017) Evaluation and management of adolescent idiopathic scoliosis: a review. Neurosurg Focus 43(4):E2. https://doi.org/10.3171/2017.7.Focus17297
Lonner BS, Ren Y, Yaszay B et al (2018) Evolution of surgery for adolescent idiopathic scoliosis over 20 years: have outcomes improved? Spine (Phila Pa 1976) 43(6):402–410. https://doi.org/10.1097/brs.0000000000002332
Elsamadicy AA, Koo AB, Kundishora AJ et al (2019) Impact of patient and hospital-level risk factors on extended length of stay following spinal fusion for adolescent idiopathic scoliosis. J Neurosurg Pediatr 24:1–7. https://doi.org/10.3171/2019.5.Peds19161
Elsamadicy AA, Freedman IG, Koo AB et al (2021) The effects of pulmonary risk factors on hospital resource use after posterior spinal fusion for adolescent idiopathic scoliosis correction. World Neurosurg 149:e737–e747. https://doi.org/10.1016/j.wneu.2021.01.109
Al-Mohrej OA, Aldakhil SS, Al-Rabiah MA, Al-Rabiah AM (2020) Surgical treatment of adolescent idiopathic scoliosis: complications. Ann Med Surg (Lond) 52:19–23. https://doi.org/10.1016/j.amsu.2020.02.004
Koo AB, Elsamadicy AA, Kundishora AJ et al (2020) Geographic variation in outcomes and costs after spinal fusion for adolescent idiopathic scoliosis. World Neurosurg 136:e347–e354. https://doi.org/10.1016/j.wneu.2019.12.175
Elsamadicy AA, Freedman IG, Koo AB et al (2021) Impact of preoperative anemia on outcomes after posterior spinal fusion for adolescent idiopathic scoliosis. World Neurosurg 146:e214–e224. https://doi.org/10.1016/j.wneu.2020.10.074
Elsamadicy AA, Koo AB, Lee M et al (2019) Reduced influence of affective disorders on perioperative complication rates, length of hospital stay, and healthcare costs following spinal fusion for adolescent idiopathic scoliosis. J Neurosurg Pediatr 24(6):722–727
Knight BA, Bayne AP, Zusman N, Barney N, Yang S (2020) Postoperative management factors affect urinary retention following posterior spinal fusion for adolescent idiopathic scoliosis. Spine Deform 8(4):703–709. https://doi.org/10.1007/s43390-020-00090-9
(CDC) CfDCaP. 2000 CDC growth charts. https://www.cdc.gov/growthcharts/cdc_charts.htm. Accessed 15 Feb 2022
Powers JM, Sandoval C (2021). In: Donald H, Mahoney J, Lorin MI, Armsb C (eds) Approach to the child with anemia. UpToDate, Waltham
Baker RD, Greer FR, Nutrition Co (2010) Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics 126(5):1040–1050
Zakaria HM, Bazydlo M, Schultz L et al (2020) Ambulation on postoperative day #0 is associated with decreased morbidity and adverse events after elective lumbar spine surgery: analysis from the Michigan spine surgery improvement collaborative (MSSIC). Neurosurgery 87(2):320–328. https://doi.org/10.1093/neuros/nyz501
Sugarman E, Sarwahi V, Amaral T, Wollowick A, Gambassi M, Seimon L (2013) Comparative analysis of perioperative differences between hybrid versus pedicle screw instrumentation in adolescent idiopathic scoliosis. J Spinal Disord Tech 26(3):161–166. https://doi.org/10.1097/BSD.0b013e31823b9e1b
Oe S, Yamato Y, Hasegawa T et al (2020) Association between a prognostic nutritional index less than 50 and the risk of medical complications after adult spinal deformity surgery. J Neurosurg Spine 33:1–6. https://doi.org/10.3171/2020.1.Spine191410
Koucheki R, Koyle M, Ibrahim GM, Nallet J, Lebel DE (2021) Comparison of interventions and outcomes of enhanced recovery after surgery: a systematic review and meta-analysis of 2456 adolescent idiopathic scoliosis cases. Eur Spine J 30(12):3457–3472. https://doi.org/10.1007/s00586-021-06984-0
Kim E, Lee B, Cucchiaro G (2017) Perioperative surgical home: evaluation of a new protocol focused on a multidisciplinary approach to manage children undergoing posterior spinal fusion operation. Anesth Analg 125(3):812–819. https://doi.org/10.1213/ane.0000000000002030
Muhly WT, Sankar WN, Ryan K et al (2016) Rapid recovery pathway after spinal fusion for idiopathic scoliosis. Pediatrics. https://doi.org/10.1542/peds.2015-1568
Julien-Marsollier F, Michelet D, Assaker R et al (2020) Enhanced recovery after surgical correction of adolescent idiopathic scoliosis. Paediatr Anaesth 30(10):1068–1076. https://doi.org/10.1111/pan.13988
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ACH, WBD, BCR, SC, SB, MC, JH, TF, ABK, DAT, MD, AAE: Made substantial contributions to the conception and design of the work, acquisition, analysis, or interpretation of data; drafted the work and revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tuason: Depuy, A Johnson & Johnson Company: Paid Consultant, Paid presenter or speaker. Globus Medical: Paid presenter or speaker. OrthoPediatrics: Paid Consultant, Paid presenter or speaker. Pediatric Orthopaedic Society of North America: Board or Committee member. Scoliosis Research Society: Board committee member. All other authors have no other disclosures.
Ethical approval
IRB Protocol Approval # 2000028261.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hengartner, A.C., David, W.B., Reeves, B.C. et al. Effects of delayed ambulation following posterior spinal fusion for adolescent idiopathic scoliosis: a single institutional study. Spine Deform 11, 1127–1136 (2023). https://doi.org/10.1007/s43390-023-00693-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00693-y