Abstract
Purpose
This study sought to analyze factors that predict postoperative shoulder balance based on clinical photography.
Methods
Based on inclusion criteria, 132 AIS patients were selected. Age, sex, and BMI of each patient were recorded. The following parameters were recorded from radiographs: clavicle angle, T1 tilt, the upper instrumented vertebra (UIV), lowest instrumented vertebra (LIV) thoracic kyphosis, lumbar modifier, preoperative and postoperative proximal thoracic Cobb angle, preoperative and postoperative main thoracic Cobb angle, and preoperative and postoperative thoracolumbar Cobb angle, if applicable. Two spine surgeons independently assigned the photographs shoulder balance grades based on the WRVAS (1–2 = Acceptable, 3–5 = Unacceptable). Surgeons were blinded as to whether the photographs were taken preoperatively or postoperatively. The shoulders were also graded as right high, left high, or balanced.
Results
Of all variables analyzed, only main thoracic Cobb angle correction (MTCAC) showed a statistically significant relationship with postoperative shoulder balance (p = 0.01). Odds of having unacceptable shoulder balance increase by 21% for every 5° increase in MTCAC (Adjusted OR = 1.21, 95% CI 1.015–1.452). The odds of unbalanced shoulders are 4.7 times higher for patients whose MTCAC is 40° or more (p = 0.001). Inter-rater reliability was excellent (k =0 .7). Intra rater reliability was perfect for Surgeon 1 (kappa = 1.0) and showed substantial agreement for Surgeon 2 (kappa = 0.8)
Conclusions
Greater correction of main thoracic Cobb angle predicts unacceptable postoperative shoulder balance with 40° of correction signifying a major dichotomy between acceptable and unacceptable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional deformity of the spine affecting up to 3% of the population. While often benign, the natural progression of AIS may result in disturbances of the body that affect morphology and physiology [1]. One of the greatest concerns of the patient is the overall body appearance, both before and after surgery. Shoulder balance, as measured by the Walter Reed Visual Assessment Scale (WRVAS), is one of the most commonly rated specific appearance concerns described by children with AIS and has shown validity as a means for assessment of scoliotic deformity [2]. In one review of 112 surgically treated patients with AIS, preoperative shoulder imbalance was a concern in 75% and postoperative imbalance was still a concern in 24% [1]. Even more disappointing is the patient with acceptable shoulder balance before surgery who unexpectedly has unacceptable shoulder balance postoperatively.
Shoulder balance can be measured clinically, radiographically, and/or by clinical photography [3]. Ono et al. showed that shoulder height asymmetry based on clinical photography can be subclassified into two distinct regions, lateral and medial [4]. Medial shoulder balance was reflected in trapezial prominence and lateral shoulder balance was reflected in lateral shoulder asymmetry. Studies using preoperative and postoperative radiographs suggest that several parameters affect final shoulder balance after AIS surgery, particularly the amount of correction of the coronal curvatures and the preoperative shoulder level [5]. More recently, Yang et al. showed that the ratio of preoperative proximal thoracic to main thoracic curvature is predictive of postoperative shoulder imbalance [6]. However, this literature was radiographic based, without consideration of shoulder balance based on clinical appearance. One study used the soft-tissue shadows present on radiographs to assess shoulder balance [7]. More recently, Sielatycki et al. assessed shoulder balance with clinical photographs, but their study involved anterior photographs [8].
Since patients worry about their visible appearance, understanding the variables that affect shoulder balance may be useful when discussing surgical treatment with patients and their families. This study sought to analyze factors that predict postoperative shoulder balance based on clinical photography, so that informed patient consent can be discussed. Proper consent requires addressing the percent likelihood of shoulder imbalance given their preoperative clinical appearance and the desired amount of coronal plane correction.
Materials and methods
This was a level 3 case–control, IRB approved study.
Patient Selection—A search of RedCAP data base of the operative spine patients of two surgeons at our institution from 2007–2016 revealed 277 patients with adolescent idiopathic scoliosis based on SRS M&M classification. One hundred and forty of these patients met the study population criteria.
Inclusion criteria
-
(1)
Children with adolescent idiopathic scoliosis who underwent posterior spinal fusion and instrumentation between the ages of 10–18 years.
-
(2)
Quality preoperative and postoperative photographs that showed the shoulders within 3–6 months of surgery.
-
(3)
Adequate preoperative and postoperative standing PA and lateral scoliosis radiographs.
-
4)
All Lenke AIS classification types.
Exclusion criteria
-
(1)
Inadequate radiographs or clinical photography.
-
(2)
Unable to hide postoperative incision from image.
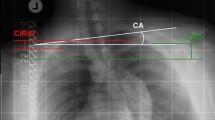
A review of patient medical records was conducted to identify patient age, sex, and body mass index (BMI). Radiographs were reviewed using InteleViewer™ radiology system to assess clavicle angle (angle subtended by two highest points on the clavicle and a horizontal), T1 tilt (angle subtended by the superior endplate of T1 and a horizontal), thoracic kyphosis (T5–12), lumbar modifier (A, B or C), preoperative proximal thoracic Cobb angle, preoperative main thoracic Cobb angle, preoperative thoracolumbar Cobb angle, upper instrumented vertebra (UIV), lowest instrumented vertebra (LIV), postoperative proximal thoracic Cobb angle, postoperative main thoracic Cobb angle, and postoperative thoracolumbar Cobb angle if applicable. Clavicle angle was defined as positive if the left shoulder was higher than the right, consistent with the previous studies. The amount of Cobb angle correction (defined as preoperative Cobb angle minus postoperative Cobb angle), Lenke classification, and thoracic sagittal profile (N, −, +) were then determined.
A total of 132 patients had adequate preoperative and postoperative clinical photographs. All of the photographs were obtained between the 3 and 6 months postoperative period. Patients faced a wall in neutral standing position on level ground. The midline was covered to blind the reviewers as to whether the photographs were taken preoperatively or postoperatively (Fig. 1).
Shoulder Balance Grading Reference—the clinical photographs of eight idiopathic scoliosis patients who were not in the study were randomly selected. The photographs were examined by two experienced pediatric spine surgeons. Using the Delphi process and iterative rounds, the two surgeons were: (1) surveyed for current practice of analyzing shoulder balance; (2) presented with a detailed systematic review of relevant literature about shoulder balance; (3) given the opportunity to voice opinion collectively; and (4) asked to vote for acceptable or unacceptable shoulder balance privately. Shoulder balance was assessed using the WRVAS with a score of 1 or 2 deemed as acceptable shoulder balance while a 3–5 was graded as unacceptable (Fig. 2). Round 1 was conducted using a paper survey. Initial results were compiled and discussed face-to face. Round 2 was conducted allowing participants to vote for acceptable or unacceptable shoulder balance. Agreement of > 80% was considered consensus. Grading without consensus was discussed and revised, if feasible. These eight patients then served as a grading reference for all the photographs included in the study.
A ten-patient trial was then conducted using photographs of patients with AIS who did not meet all inclusion criteria. The trial had a kappa = 0.7 showing excellent inter-rater reliability. The tester was then repeated 11 days later. Surgeon 1’s responses on the retrial matched with his original responses on all 10 photographs (kappa = 1.0) showing excellent agreement. Surgeon 2’s responses matched on 9 of 10 photographs (kappa = 0.8) showing substantial agreement. With confidence in the level of surgeon reliability established, the surgeons analyzed the 280 clinical photographs for the study using the WRVAS. The surgeons also graded each patient’s shoulder balance as balanced shoulders, right shoulder high, or left shoulder high. All WRVAS scores equal to 1 or 2 were graded as balanced. The high/low analysis was used to determine if certain preoperative shoulder elevations predispose to postoperative balance status. The photographs that were scored as 3–5 on the WRVAS were graded as right high or left high based on surgeon perception.
Results
Of the 132 patients, 112 were female and 20 were male. There were 76 type 1 Lenke curves (57%), 20 Lenke 2 (15%), 16 Lenke 3, (12%), 14 Lenke 5 (11%), and 5 Lenke 6 (4%), with only one Lenke 4 curve. Descriptive statistics for the study are shown in Table 1.
Prior to surgery, 71 patients (54%) had acceptable shoulder balance. Postoperatively, 91 patients (69%) had acceptable shoulder balance. Although many patients improved with surgery, some did not achieve acceptable shoulder balance and others went from acceptable to unacceptable (Table 2). Patients with acceptable postoperative shoulder balance showed a mean preoperative thoracic Cobb angle of 61°, while unacceptable postoperative shoulder balance patients had a preoperative thoracic Cobb angle of 65°. Of the 91 patients who had acceptable postoperative shoulder balance, the average main thoracic Cobb angle correction (MTCAC) was 39°. For the 41 patients with unacceptable shoulder balance postoperatively, the MTCAC was 45° (p = 0.01). The median preoperative thoracic Cobb angle for patients who had acceptable shoulder balance postoperatively was 58° versus 63° in those considered unbalanced postoperatively (p = 0.02).
Chi -quare tests and t tests were performed on each input variable to determine if it affected postoperative shoulder balance (Table 1). MTCAC was the only variable that correlated with postoperative shoulder balance (p = 0.01).
Table 2 illustrates the postoperative shoulder balance status based on preoperative shoulder level (right high, left high or balanced). No correlation was found between preoperative shoulder level and postoperative balance (p = 0.3).
A multivariate logistic regression model was used to evaluate possible factors predictive of postoperative shoulder balance. The variables chosen were preoperative shoulder balance status, clavicle angle, BMI, and MTCAC (Table 3). These variables were chosen based on the experimental hypothesis with the exception of MTCAC, which was chosen because of demonstrated significance in the univariate analysis. MTCAC was the only variable that had statistical significance (p = 0.03). The model also revealed that for every 5° correction of the main thoracic curve Cobb angle, the odds of having unbalanced shoulders postoperatively increased by 21% (95% CI 1.0–1.5). In other words, a patient with a 50° MTCAC would have a 21% greater chance of having unbalanced shoulders than an identical patient with a 45° MTCAC (adjusted odds ratio of 1.2, p = 0.01). Additionally, logistic regression analysis demonstrated that patients with MTCAC greater than or equal to 40° had 4.7 times the odds of having unbalanced shoulders (95% CI 1.9–11.8). Of those with greater than or equal to a 40° MTCAC, 46.7% had unbalanced shoulders, while only 14.6% of those with less than a 40° MTCAC had unbalanced shoulders (p = 0.0001).
Figures 3 and 4 illustrate patients with excessive and desirable MTCAC, respectively.
Image A is a preoperative radiograph of a patient with main thoracic Cobb angle of 68° Image B is same patient’s clinical photograph preoperatively. Image C shows the patient’s main thoracic Cobb angle which has been corrected to 17°. Image D is the patient’s clinical photograph with unbalanced shoulders due to overcorrection of main thoracic Cobb angle
Image A is a preoperative radiograph of a patient with a main thoracic Cobb angle of 58°. Image B is same patient’s clinical photograph preoperatively. Image C shows the patient’s main thoracic Cobb angle has been corrected to 21°. Image D shows the patient’s clinical photograph with balanced shoulders due to adequate correction of main thoracic Cobb angle
Discussion
This study sought predictors of postoperative shoulder balance based on clinical appearance. A major concern for 24–34% of patients is the persistence of unbalanced shoulders following surgery, demonstrating a need for a more thorough understanding of factors that predict shoulder balance [1, 9]. Our study showed that the amount of correction of the main thoracic Cobb angle was the only significant variable predictive of shoulder balance. We also demonstrated that a higher preoperative main thoracic Cobb angle corresponded with an increased likelihood for unbalanced shoulders postoperatively. These findings build off each other as a larger preoperative Cobb angle naturally lends itself to increased correction. Gotfryd et al. proposed that overcorrection of the main thoracic curve can drive the contralateral shoulder toward imbalance if the shoulders are symmetrical preoperatively [10]. This could explain the 26 patients that were initially balanced preoperatively, but were unbalanced postoperatively in this study.
Many studies have examined radiographic variables that predict postoperative shoulder balance with varying results. Kuklo et al. showed that clavicle angle correlated with both radiographic and patient perception of shoulder balance [7]. T1 tilt has also been implicated as a predictive factor of shoulder balance, but conflicting evidence exists regarding this variable [7, 10, 11]. Ono et al., however, found that T1 tilt correlated with medial trapezial prominence [4]. We did not find that T1 tilt or clavicle angle was predictive of shoulder balance. However, the WRVAS is probably a better assessment of lateral shoulder balance, so the contribution of T1 tilt to shoulder balance, as reflected by trapezial prominence, may be underappreciated in our study. Similar to the findings of our study, some recent studies have shown that the most important variable may be the degree of correction of the main thoracic curve [8, 10, 12,13,14]. Brooks et al. reviewed three groups of patients based on the UIV: T2, T3, or T4. They found that patients fused to T4 had more balanced shoulders postoperatively compared to those with a UIV of T2 or T3 regardless of which shoulder was elevated preoperatively [15]. Likewise, we also did not find that preoperative shoulder position was predictive of postoperative balance. Unlike their study, however, we found that UIV was not predictive of shoulder balance. Perhaps, their use of radiographs to assess shoulder balance rather than clinical photographs accounts for the difference in findings. Our study also found that the LIV was not predictive of postoperative shoulder balance. Yaszay et al. analyzed shoulder balance in Lenke 5 curves and found that although half had an elevated contralateral shoulder preoperatively, most were balanced postoperatively regardless of whether or not the compensatory thoracic curve was included in the construct [16].
To our knowledge, only a few studies have used clinical photography as a means for assessing the outcome of postoperative shoulder balance [3, 8, 17,18,19]. Sielatycki et al. demonstrated that undercorrection of the proximal thoracic curve and overcorrection of the main thoracic curve increased the likelihood of unbalanced shoulders postoperatively [8]. The study used anterior photographs of patients with Lenke 1 and 2 curves. Our study differed as we used posterior photographs and included all Lenke curve types, although 72% of our cohort had either Lenke 1 or 2 curve types. However, our study yielded similar findings regarding main thoracic curve correction, but we found a numerical relationship based on the absolute degree of correction, rather than percentage correction. This absolute degree of correction may provide surgeons and patients with a simpler interpretation of the numerical relationship between MTCAC and shoulder balance. Theologis et al. and Raso et al., also used clinical photographs to study trunk deformity, but neither study evaluated shoulder balance, specifically [17, 18]. Dzulkarnain et al. examined anterior photographs of 84 patients with Lenke 1 and 2 curves and found that leveling the upper thoracic spine does not guarantee clinically balanced shoulders, particularly lateral shoulder balance [19]. Our findings were similar in that neither upper thoracic curve Cobb angle correction nor the UIV was found to be predictive of postoperative shoulder balance.
The use of clinical photography is useful, because patients and their families can observe their appearance and use it as a benchmark to gauge the success of their surgery. Our study demonstrated that for every 5° of additional correction of the MTCAC, the likelihood of unbalanced shoulders increases by 21%. Forty degrees of MTCAC appears to provide a threshold at which increasing correction yields diminishing outcomes. Knowledge of this relationship is valuable for surgeons as it allows for more educated decision-making regarding the desired amount of correction. Additionally, it has value for patients as information from this study will allow surgeons to give a more realistic expectation of postoperative appearance based on individual profile. This is an important discussion to have with the family, as it should be a realistic constraint on their expectation to have their child “as straight as possible”.
This study had several major limitations. Adequate preoperative and postoperative clinical photographs were only available for 132 of the 277 patients who had surgery for AIS during the period of the study. Therefore, patients were selected based on photograph availability and were not consecutive patients in a series, which potentially introduces selection bias. Photographs were taken 6 months postoperatively for a majority of patients, but 3-month postoperative photos were used when necessary. This short duration of follow up does not allow for observation of long-term changes that may develop in subsequent years. There were also few patients in the study with Lenke curve types 2–6, so we were underpowered to make conclusions about patients with these curve types. Future studies based on clinical appearance of shoulder balance with more patients with these curve types would be helpful. Furthermore, we did not analyze specific surgical details, such as correction techniques, as two surgeons were involved in the care of the subjects, and surgical techniques have evolved to some extent over the time frame of the study. In general, however, it has been standard for T2 to be the UIV in patients with structural proximal thoracic curves and/or preoperative left shoulder elevation. Additionally, it has been our practice to instrument and fuse all structural curves. Finally, we only examined correction of the coronal plane. There may be different relationships when both the sagittal and axial planes are considered.
Key Points
-
1)
Increased surgical coronal plane correction leads to an increased likelihood of unacceptable postoperative shoulder balance.
-
2)
A higher preoperative Cobb angle of the primary curve correlates with less likelihood of acceptable postoperative shoulder balance.
-
3)
For every 5° of additional correction of the MTCAC, the likelihood of unbalanced shoulders increases by 21%.
References
Kotwicki T, Chowsanka J, Kinel E et al (2013) Optimal management of idiopathic scoliosis in adolescence. Adolesc Health Med Ther 4:59–73
Pineda S, Bago J, Gilperez C et al (2006) Validity of the walter reed visual assessment scale to measure subjective perception of spine deformity in patients with idiopathic scoliosis. Scoliosis 11:18
Menon KV, Pillay HM, Tahasildar N et al (2015) Post-operative shoulder imbalance in adolescent idiopathic scoliosis: a study of clinical photographs. Scoliosis 10:31
Ono T, Bastrom TP, Newton PO (2012) Defining 2 components of shoulder imbalance: clavicle tilt and trapezial prominence. Spine 37:1511–1516
Hong JY, Suh SW, Modi HN et al (2013) Analysis of factors that affect shoulder balance after correction surgery in scoliosis: a global analysis of all the curvature types. Eur Spine J 22:1273–1285
Yang Y, Yang M, Zhao J et al (2019) Postoperative shoulder imbalance in adolescent idiopathic scoliosis: risk factors and predictive index. Eur Spine J 28:1331–1341
Kuklo TR, Lenke LG, Graham EJ et al (2002) Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus non-fusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine 27:2013–2020
Sielatycki JA, Cerpa M, Beauchamp EC et al (2019) The amount of curve correction is more important than upper instrumented vertebra selection for ensuring postoperative shoulder balance in lenke type 1 and type 2 adolescent idiopathic scoliosis. Spine 44:E1031–E1037
Han X, Liu Z, Qiu Y et al (2016) Clavicle chest cage angle difference: is it a radiographic and clinical predictor of postoperative shoulder imbalance in lenke I adolescent idiopathic scoliosis? Spine 4:1346–1354
Gotfryd AO, Silber Caffaro MF, Meves R et al (2017) Predictors for postoperative shoulder balance in Lenke 1 adolescent idiopathic scoliosis: a prospective cohort study. Spine Deform 5:66–71
Luhmann SJ, Sucato DJ, Johnston CE et al (2016) Radiographic assessment of shoulder position in 619 idiopathic scoliosis patients: can T1 tilt be used as an intraoperative proxy to determine postoperative shoulder balance? J Pediatr Orthop 36:691–694
Jian YM, Yang SH, Hu MH (2018) Assessment of change of shoulder balance in patients with adolescent idiopathic scoliosis after correctional surgery. Orthop Surg 10:198–204
Namikawa T, Matsumura A, Kato M et al (2015) Radiological assessment of shoulder balance following posterior spinal fusion for thoracic adolescent idiopathic scoliosis. Scoliosis 10:S18
Chang DG, Kim JH, Kim SS et al (2014) How to improve shoulder balance in the surgical correction of double thoracic adolescent idiopathic scoliosis. Spine 39:E1359–E1367
Brooks JT, Bastrom TP, Barley M et al (2018) In search of the ever-elusive postoperative shoulder balance: Is the T2 UIV the key? Spine Deformity 6:707–711
Yaszay B, Bastrom TP, Newton PO (2013) Should shoulder balance determine proximal fusion levels in patients with lenke 5 curves. Spine Deformity 1:447–451
Theologis TN, Jefferson RJ, Simpson AHRW et al (1993) Quantifying the cosmetic defect of adolescent idiopathic scoliosis. Spine 18:909–912
Raso JV, Lou EM, Hill DL et al (1998) Trunk distortion in adolescent idiopathic scoliosis. J Pediatr Orthop 18:222–226
Dzulkarnain A, Yaszay B, Bartley CE et al (2016) Does Leveling the Upper Thoracic Spine Have Any Impact on Postoperative Clinical Shoulder Balance in Lenke 1 and 2 patients? Spine 41:1122–1127
Acknowledgements
We grant permission to reproduce copyrighted materials. Reviewed and approved by the Pediatric IRB at The Children’s Mercy-Kansas City. The authors would like to thank Julia Leamon, MS, RN, CPN for her assistance with the study.
Funding
No funding was received for the purpose of this study.
Author information
Authors and Affiliations
Contributions
AH: substantial contributions to the conception or design of the work and acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published. RT: substantial contributions to the conception or design of the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published. EE: substantial contributions to the conception or design of the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published. AS: acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published. JA: substantial contributions to the conception or design of the work and acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published. RS: substantial contributions to the conception or design of the work and acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
Corresponding author
Ethics declarations
IRB Approval
IRB # 16050398
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hiett, A., Tung, R., Emanuelli, E. et al. The amount of surgical correction of the main thoracic curve is the best predictor of postoperative clinical shoulder balance in patients with Adolescent Idiopathic Scoliosis. Spine Deform 8, 1279–1286 (2020). https://doi.org/10.1007/s43390-020-00147-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00147-9