Abstract
Purpose
Postoperative shoulder imbalance (PSI) is a common complication of adolescent idiopathic scoliosis (AIS). However, results regarding risk factors for PSI are contradictory. This study was performed to explore the risk factors associated with PSI in AIS and determine whether PSI could be predicted.
Methods
Medical records of AIS patients receiving correction surgery from January 2012 to January 2015 were reviewed. Anteroposterior films were evaluated before and after the surgery and at the 2-year follow-up. Patients were divided into two groups according to whether PSI was observed at 2-year follow-up. Risk factors for PSI were analyzed, and a PSI index was proposed and verified.
Results
A total of 114 AIS patients (PSI/non-PSI: 60/54) were included. The univariate analysis showed that PTC (proximal thoracic curve), preoperative PTC-to-MTC (main thoracic curve) ratio, preoperative bending Cobb angle of PTC, preoperative bending Cobb angle of the lumbar curve, postoperative PTC, postoperative AVT (apical vertebral translation) of PTC, AVT of PTC at follow-up, and adding-on angle were significantly different between two groups. Adjusted logistic regression analysis showed that postoperative AVT of PTC and adding-on angle were the primary contributors to PSI in patients with AIS. The PSI index was defined as 1.2 × postoperative AVT of PTC + 1.1 × adding-on angle. According to the receiver operating characteristic curve, the cutoff point for the PSI index in predicting the development of PSI was 15. The positive and negative predictive values were 80% and 87%, respectively.
Conclusions
To prevent PSI, we recommend sufficient correction of AVT of PTC and prevention of adding-on.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a complex three-dimensional deformity of the spine characterized by at least 10° of scoliotic curve in the coronal plane, deviation of the sagittal spinal profile, and vertebral rotation in the transverse plane [1, 2]. Correction surgery is still considered as an effective treatment option in treating AIS, especially for AIS with scoliotic curve > 45°, although surgery was challenged by poor correction of deformity, massive blood loss, high complication rates, need for reoperations, etc. [3].
AIS commonly affects women, with a female-to-male ratio of 1.5:1–3:1, who pay more attention to appearance than men [1]. Postoperative shoulder imbalance (PSI) is an important aspect when we evaluate the effectiveness of correction surgery, which has an influence on patients’ appearance and satisfaction [4, 5]. Thus, achieving shoulder balance is one of the goals of correction surgery.
However, risk factors for PSI and methods to prevent the development of PSI after correction surgery remain controversial. Lee et al.’s study [6] revealed that PSI was correlated with a higher Risser grade, larger postoperative proximal wedge angle, and higher postoperative proximal thoracic curve (PTC)/main thoracic curve (MTC) ratio. Yagi et al. [7] found that the clavicle chest cage angle difference (CCAD) and apical vertebral rotation (AVR) of MTC were independent risk factors for PSI in surgically treated patients with AIS. Namikawa et al. [8] suggested that sufficient correction of PTC that was matched with correction of MTC was necessary to prevent PSI.
Regarding predictors for evaluating PSI, Liu et al.’s study [9] demonstrated that CCAD could be a reliable predictor for evaluating PSI in patients with AIS undergoing selective posterior fusion for Lenke 5C curves, which was verified by Han et al. in patients with Lenke 1 AIS [10]. However, these authors [9,10,11] only focused on the role of shoulder parameters in predicting PSI, regardless of other risk factors, such as preoperative PTC, preoperative radiological shoulder height (RSH), and postoperative PTC/MTC. Therefore, we performed this retrospective study to explore the risk factors associated with PSI in patients with AIS and determine whether PSI could be predicted after correction surgery using demographics and pre- and postoperative radiological parameters.
Methods and materials
Patient population
Medical records of patients with AIS undergoing correction surgery with all-pedicle screw instrumentation in our hospital from January 2012 to January 2015 were reviewed. The inclusion criteria were as follows: (1) diagnosis of AIS; (2) age between 12 and 18 years; (3) main Cobb angle > 45°; (4) one-stage posterior pedicle screw instrumentation by the same treatment group, with at least of 2-year follow-up; and (5) sufficient full spine X-ray films before and after the surgery and at final follow-up. The exclusion criteria were as follows: (1) other scoliosis, such as neuromuscular scoliosis and degenerative scoliosis; (2) insufficient radiological parameters; and (3) infections, tumors, and other spine diseases. This study was approved by the Institutional Review Board of our university, and all patients in our study provided written informed consent.
Data collection
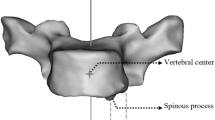
Demographic data were collected, including age, Risser sign, upper instrumented vertebra (UIV), UIV-T1 (the segments between UIV and T1), fusion levels, and Lenke types. The standing and bending posteroanterior data before surgery, at 2 weeks after surgery (initial), and 2-year follow-up were recorded. Radiological parameters were evaluated, including PTC (preoperative, postoperative, and at follow-up), MTC (preoperative, postoperative, and at follow-up), lumbar curve (LC) (preoperative, postoperative, and at follow-up), preoperative PTC/MTC ratio, preoperative MTC/LC ratio, preoperative bending Cobb angle of PTC, flexibility of PTC [(preoperative PTC-preoperative bending Cobb angle of PTC)/preoperative PTC], preoperative bending Cobb angle of MTC, flexibility of MTC [(preoperative MTC-preoperative bending Cobb angle of MTC)/preoperative MTC], preoperative bending Cobb angle of LC, flexibility of LC [(preoperative LC-preoperative bending Cobb angle of LC)/preoperative LC], AVT (apical vertebral translation) of PTC [the distance from the central sacrovertebral line (CSVL) to the center of the proximal thoracic apical vertebra] (preoperative, postoperative, and at follow-up), AVT of MTC [the distance from CSVL to the center of the main thoracic apical vertebra] (preoperative, postoperative, and at follow-up), AVT of LC [the distance from CSVL to the center of the lumbar apical vertebra] (preoperative, postoperative, and at follow-up), clavicular angle [measured by the intersection of the line connecting the highest two points of each clavicle and a horizontal line] (preoperative, postoperative, and at follow-up), RSH [Radiographic shoulder height], which is defined as the difference in soft tissue shadows directly superior to the acromioclavicular joints on both sides] (preoperative, postoperative, and at follow-up), coronal balance [the horizontal distance between the center of C7 plumb line and the CSVL line] (preoperative, postoperative, and at follow-up), correction of PTC ([preoperative PTC-postoperative PTC]/preoperative PTC), correction of MTC ([preoperative MTC-postoperative MTC]/preoperative MTC), correction of LC ([preoperative LC-postoperative LC]/preoperative LC), correction of PTC-to-correction of MTC ratio, and correction of MTC-to-correction of LC ratio.
In addition, we also evaluated whether patients with AIS had adding-on at the final follow-up, according to the definition by Wang et al. [12]. Progressive increase in the number of vertebrae included within the distal curve, with either an increase of more than 5 mm in the deviation of the first vertebra below the instrumentation from the CSVL (the vertical line bisecting the proximal sacrum), or an increase of more than 5° in the angulation of the first disk below the instrumentation. The adding-on angle was evaluated at the final follow-up, which is defined as the angle between the upper end plate of LIV and the lower end plate of LIV + 2 (Fig. 1). In addition, Scoliosis Research Society (SRS)-22 scores were also evaluated to determine the patient-centered outcome, including pain, appearance, activity, mental health, and satisfaction. All parameters were obtained by two independent surgeons with two repetitions, and the average value was calculated.
At the final follow-up, patients were divided into two groups on the basis of whether PSI developed, according to the RSH at follow-up [9]: PSI group (RSH ≥ 10 mm) and non-PSI group (RSH < 10 mm). All demographic and radiological parameters were compared between these two groups (univariate analysis). Unadjusted binary logistic regression analysis was performed to determine the risk factors for the development of PSI using the variables that were found significant in the univariate analysis. In the adjusted regression analysis, parameters at follow-up were deleted because we aimed to establish a regression equation including the radiological parameters that could change during the correction surgery and prevent the development of PSI. Furthermore, the PSI index was set according to the results of the adjusted logistic regression, as a novel predictor for PSI. The positive and negative predictive values of the predictive power of the development of PSI using the PSI index were calculated, and the receiver operating characteristic (ROC) curve was drawn.
Statistical analysis
The software SPSS 22.0 was used for all statistical analyses. Descriptive statistics were presented in the form of mean and standard deviation (SD), and categorical data were presented in numbers. Independent two-sample t test was used to compare the differences in variables between the two groups. The X2 test was used to compare the differences in count data. Binary logistic regression models, with forward elimination (conditional), were constructed using variables that were found significant in a comparison study in order to find independent risk factors associated with PSI. ROC curves were constructed to determine the optimal cutoff value of the PSI index as indicators for the development of the PSI phenomenon. A P value < 0.05 was considered statistically significant.
Results
General information
A total of 114 patients with AIS were recruited in our study, with a mean age of 16.61 ± 4.92 years. The mean Risser sign was 3.59 ± 1.53°. There were 56 Lenke 1 patients, 12 Lenke 2 patients, 6 Lenke 3 patients, 4 Lenke 4 patients, 29 Lenke 5 patients, and 7 Lenke 6 patients. In addition, adding-on developed in 18 patients with AIS at the final follow-up, with a prevalence of 15.8%. All abbreviations are shown in Table 1. The demographics and radiological parameters are summarized in Table 2.
Univariate analysis
Sixty patients had PSI at the final follow-up, and 54 patients were recruited in the non-PSI group. There was no significant difference in age, Risser sign, distribution of UIV, UIV-T1, fusion levels, and Lenke types between the two groups (Table 3). Radiological parameters showing significant differences between these two groups were as follows: preoperative PTC (P = 0.002), preoperative PTC/MTC ratio (P = 0.004), preoperative bending Cobb angle of PTC (P = 0.006), preoperative bending Cobb angle of LC (P = 0.050), postoperative PTC (P = 0.036), postoperative AVT of PTC (P = 0.006), and AVT of PTC at follow-up (P = 0.004). However, we did not observe any significant difference in other radiological parameters (all P > 0.05). Data are summarized in Table 3.
Furthermore, 15 patients in the PSI group had adding-on, while only three patients in the non-PSI group had adding-on, with a P value of 0.004 (Table 3). Significant difference in adding-on angle was observed between the two groups (9.52 ± 6.43 vs. 7.53 ± 2.77, P = 0.038, Table 3).
The scores of pain, appearance, activity, mental health, and satisfaction were 4.5, 4.0, 4.6, 4.2, and 4.2, and the total score was 4.2 in patients with PSI, and these scores were 4.5, 4.3, 4.5, 4.3, 4.4, and 4.3 in patients without PSI, respectively; there were no significant differences between both groups (all P > 0.05, Table 3).
Two typical cases are shown in Figs. 2 and 3.
Typical case is shown in the figure. A 13-year-old female AIS patient received correction surgery in our hospital in June 2012. The preoperative MTC, RSH, and coronal balance were 45o, − 15 mm and 2 mm, respectively. a LIV and UIV were chosen at L1 and T3, respectively. After surgery, shoulder returned to be balanced; however, the postoperative AVT of PTC was 20 mm. b Postoperative coronal balance increased to 20 mm. At 2-year follow-up, PSI occurred with RSH of +22 mm. Adding-on also occurred with adding-on angle of 17o, and coronal balance decreased to 5 mm. c PSI index = 1.2 × 20 + 1.1 × 17 = 42.7 > 15. PSI occurred and coronal alignment was rebalanced, indicating that ‘‘Adding-on’’ might be a compensation for PSI and coronal balance
Typical case is shown in the figure. A 14-year-old female AIS patient received correction surgery in our hospital in June 2013. Preoperative MTC was 54o, with preoperative shoulder imbalanced of − 2 mm. a Preoperative coronal balance was 11 mm. After correction surgery, postoperative RSH and postoperative AVT of PTC were − 5 mm and 9 mm, respectively. b At final follow-up, patient’s shoulder remained unchanged, and coronal alignment was decreased to 8 mm. c No adding-on was observed in this patient with Adding-on angle of 0o. PSI index = 1.2 × 9 + 1.1 × 0 = 10.8 < 15
Multivariate analysis
The unadjusted logistic regression analysis showed that AVT of PTC at follow-up (P = 0.021) and adding-on angle (P = 0.018) were the primary contributors to PSI in patients with AIS (Table 4). However, these were parameters at the final follow-up, which were difficult to use, predict, and correct before and during the surgery. In order to make our regression equation more easy to use, we replaced AVT of PTC at follow-up with postoperative AVT of PTC in our adjusted regression analysis (AVT of PTC at follow-up was significantly correlated with postoperative AVT of PTC: r = 0.883, P < 0.001). Our adjusted logistic regression analysis showed that postoperative AVT of PTC (P = 0.035) and adding-on angle (P = 0.026) were the primary contributors to PSI in patients with AIS (Table 4).
Based on results of the adjusted logistic regression analysis, we defined PSI index as 1.2 × postoperative AVT of PTC + 1.1 × adding-on angle.
ROC curve
Based on the ROC curve, the optimal cutoff value of the PSI index as an indicator for the development of PSI was estimated to be 15. The positive and negative predictive values were 80% and 87%, respectively.
Discussion
Health-related quality of life (HRQOL) in patients with AIS who underwent spinal fusion is becoming recognized as important, and surgeons now pay more attention to patients’ HRQOL and satisfaction to surgery rather than correction of scoliosis itself [13]. The SRS-22 questionnaire is specifically designed for the assessment of HRQOL in patients with AIS. It is the most widely used questionnaire for evaluating HRQOL of patients with AIS and includes five domains: “Pain,” “Appearance,” “Activity,” “Mental Health,” and “Satisfaction.” In the “Appearance” domain, shoulder balance is an important evaluation aspect. Patients with AIS seem to pay more attention to their appearance rather than actual correction of their spinal deformity. Therefore, how to restore and keep shoulder balance in patients with AIS after correction surgery is a great concern to spine surgeons. Determining risk factors that predict PSI should be valuable in reducing the PSI rate and might also help enhance our understanding of this phenomenon.
Several risk factors have been identified to be significantly associated with PSI in patients with AIS, including preoperative CCAD [9, 10], postoperative PTC/MTC ratio [6], and sufficient correction of PTC that is matched with correction of MTC [8]. However, these results were controversial. Furthermore, a recent meta-analysis performed by Zhang et al. [4] showed that Risser sign, preoperative LC, postoperative RSH, correction rate of PTC and MTC at follow-up, and LC at follow-up were risk factors for PSI in patients with scoliosis. However, whether these factors could be used as predictors for PSI remains unclear.
In our univariate analysis, preoperative PTC, preoperative bending Cobb angle of PTC, postoperative PTC, postoperative AVT of PTC, and AVT of PTC at follow-up were significantly larger in the PSI group than those in the non-PSI group, indicating the important role of PTC in the development of PSI. It is believed that PSI can result from PTC that is left unfused and was caused by the surgeon’s failure to properly correct PTC [6, 14]. Our results suggested that sufficient correction of PTC should be performed during surgery, including correction of scoliotic curves and AVT of PTC. These results were consistent with Zhang et al.’s study [4]. They reported that correction rate of PTC at follow-up was one of the risk factors for PSI in patients with scoliosis and also recommended sufficient correction of PTC in surgery.
In addition, preoperative bending Cobb angle of PTC was larger in patients with AIS with PSI, illustrating that the rigidity of PTC might play an important role in PSI, which should be taken into consideration during the preoperative decision-making. Moreover, if the rigid PTC is not included in correction and fusion, patients may develop severe PSI [15]. However, how to choose the fusion levels of PTC remains controversial. Akin et al. [16] suggested that extending fusion to T2 or T3 was not needed for nonstructural PTC. However, the commonly recommended upper fusion level is T2 for patients with AIS and double thoracic curve. We did not observe any significant difference in UIV and UIV-T1, suggesting that fusion levels might not be associated with PSI in patients with AIS. Selection of patients, measurement errors, and sample size might be the important contributors to this difference. Although we did not observe a significant difference in UIV between PSI and non-PSI patients, we also recommend that stopping the fusion at T3 would be adequate if the PTC was mild, according to our clinical experiences.
Our study also showed that patients with AIS with PSI had larger preoperative PTC/MTC ratio than non-PSI patients, indicating that both PTC and MTC should be taken into consideration when performing correction surgery. However, there was no significant difference in correction of PTC/MTC ratio and postoperative MTC between the two groups, which was inconsistent with Zhang et al.’s meta-analysis [4]. It was also found that overcorrection of MTC was also correlated with PSI, which might have an influence on the correction of PTC, indicating the importance of interrelationships between correction of PTC and MTC [4]. The larger preoperative PTC/MTC ratio and postoperative PTC in patients with PSI demonstrated the results of Zhang et al.’s [4] and Lee et al.’s studies [6], verifying the importance of relationships between PTC and MTC correction. Interestingly, we also found smaller preoperative bending Cobb angle of LC in patients with AIS with PSI, suggesting that the more flexible the LC was, the more likely patients with AIS would develop PSI. It is easily understood because overcorrection of LC is more likely to occur in patients with flexible LC, leading to the mismatch of PTC, MTC, and LC. Finally, PSI might develop to compensate for the mismatch of scoliotic curves. Therefore, the relationships between PTC, MTC, and LC should be noted, and we recommend sufficient correction of PTC and moderate correction of MTC and LC in surgery, which is consistent with Zhang et al.’s study [4]. In addition, although there was no significant difference in fusion levels between both groups, more vertebrae might be fused in patients with PSI, suggesting that extension of fusion levels might be an effective strategy to prevent PSI.
Although no significant difference in SRS-22 scores was observed between the two groups, patients with AIS with PSI tended to have worse Satisfaction and Appearance domains, which might be attributed to the sample size and selection bias of the study populations. Worse appearance and satisfaction scores verified the important role of shoulder balance in correction surgery. We believe that the absence of a significant difference in SRS-22 scores between the PSI and non-PSI groups might be attributed to the relatively short follow-up period. In addition, the absence of difference in SRS can also be explained by the fact that PSI is mainly a cosmetic issue, especially if slightly greater than 1 cm, and thus, the patients are generally well satisfied. Besides, the other reason should be the small population enrolled in the study. Therefore, whether PSI could result in the change of SRS-22 scores remains unclear and needs further studies with a long-term follow-up period.
Furthermore, AVT of PTC at follow-up and adding-on angle were the primary contributors to PSI in our unadjusted regression analysis, verifying the importance of correction of PTC during surgery. Considering the fact that it was difficult to use at follow-up in predicting PSI, we replaced AVT of PTC at follow-up with postoperative AVT of PTC in our adjusted regression analysis (AVT of PTC at follow-up was significantly correlated with postoperative AVT of PTC: r = 0.883, P < 0.001). Our adjusted logistic regression analysis showed that postoperative AVT of PTC and adding-on angle were the primary contributors to PSI in patients with AIS. Our results suggested that we should pay more attention to the correction of AVT of PTC in surgery to prevent the development of PSI.
It is widely believed that adding-on is an important compensatory mechanism of PSI [4, 15], which was verified in our study. Adding-on developed in 51 patients in the non-PSI group (94.5%), significantly greater than that in the PSI group (75%). Our adjusted and unadjusted regression analyses also showed that adding-on angle could be used to predict PSI in patients with AIS after correction surgery. The larger the adding-on angle is, the more likely patients with AIS would develop PSI. In our opinion, PSI is also a compensatory mechanism for adding-on, which was consistent with Lee et al.’s study [6]. They recommended that PSI should be prevented for not only the patients’ postoperative appearance but also the prevention of the adding-on phenomenon [6]. Based on these findings, we believe that adding-on and PSI are compensatory mechanisms for each other.
Based on the results of the adjusted logistic regression analysis, we defined PSI index as 1.2 × postoperative AVT of PTC + 1.1 × adding-on angle. According to our results, it can be predicted that PSI is due to the insufficient correction of AVT of PTC and the development of adding-on. The larger the postoperative AVT of PTC and adding-on angle is, the larger the PSI index would be, and the more likely it would be for patients with AIS to develop PSI after correction surgery. Therefore, we recommend sufficient correction of AVT of PTC in the surgery and the prevention of adding-on. Based on the ROC curve, the optimal cutoff value of PSI index as indicator for the development of PSI was estimated to be 15. In the surgery, we should rebalance the AVT of PTC to the central sacral vertical line, and selection of LIV and other risk factors should be taken into consideration to prevent adding-on, leading to a PSI index < 15.
Although we found a novel predictor for PSI and evaluated its effectiveness, there are some limitations of this study that should be addressed. First, our study was a single-center study, and the sample size was relatively small. Second, other radiological parameters that were found to be associated with PSI such as CCAD were not analyzed. Lastly, studies with long-term follow-up should be performed to determine the influence of PSI on HRQOL, as well as the effectiveness of the PSI index. In addition, although we included all subgroups of AIS in our study to investigate the risk factors for PSI because there is no significant difference in the distribution of AIS classification (P = 0.088) and segments of UIV-T1 (P = 0.288) in patients with and without PSI, there might be some other differences in selection of UIV in each subtype of AIS that might be ignored in our study due to the sample size, selection bias, or other factors. Therefore, how to select UIV and how to make a predefined surgical approach for the selection of the UIV need further investigation. Large-scale and multicenter studies should be performed to conduct a more comprehensive research into the effectiveness of the PSI index in predicting the development of PSI.
Conclusion
Postoperative AVT of PTC and adding-on angle were the primary contributors to PSI. Adding-on and PSI are compensatory mechanisms for each other. The PSI index could be used to predict PSI effectively. To prevent the development of PSI, we recommend sufficient correction of AVT of PTC and prevention of adding-on.
References
Choudhry MN, Ahmad Z, Verma R (2016) Adolescent idiopathic scoliosis. Open Orthop J 10:143–154. https://doi.org/10.2174/1874325001610010143
Yang M, Li C, Li Y, Zhao Y, Wei X, Zhang G, Fan J, Ni H, Chen Z, Bai Y, Li M (2015) Application of 3D rapid prototyping technology in posterior corrective surgery for Lenke 1 adolescent idiopathic scoliosis patients. Medicine 94:e582. https://doi.org/10.1097/md.0000000000000582
Lonner BS, Ren Y, Yaszay B, Cahill PJ, Shah SA, Betz RR, Samdani AF, Shufflebarger HL, Newton PO (2017) Evolution of surgery for adolescent idiopathic scoliosis over 20 years: have outcomes improved? Spine. https://doi.org/10.1097/brs.0000000000002332
Zhang S, Zhang L, Feng X, Yang H (2017) Incidence and risk factors for postoperative shoulder imbalance in scoliosis: a systematic review and meta-analysis. Eur Spine J. https://doi.org/10.1007/s00586-017-5289-y
Smyrnis PN, Sekouris N, Papadopoulos G (2009) Surgical assessment of the proximal thoracic curve in adolescent idiopathic scoliosis. Eur Spine J 18:522–530. https://doi.org/10.1007/s00586-009-0902-3
Lee CS, Hwang CJ, Lim EJ, Lee DH, Cho JH (2016) A retrospective study to reveal factors associated with postoperative shoulder imbalance in patients with adolescent idiopathic scoliosis with double thoracic curve. J Neurosurg Pediatr 25:744–752. https://doi.org/10.3171/2016.6.peds16162
Yagi M, Takemitsu M, Machida M (2013) Chest cage angle difference and rotation of main thoracic curve are independent risk factors of postoperative shoulder imbalance in surgically treated patients with adolescent idiopathic scoliosis. Spine 38:E1209–1215. https://doi.org/10.1097/BRS.0b013e31829e0309
Namikawa T, Matsumura A, Kato M, Hayashi K, Nakamura H (2015) Radiological assessment of shoulder balance following posterior spinal fusion for thoracic adolescent idiopathic scoliosis. Scoliosis 10:S18. https://doi.org/10.1186/1748-7161-10-s2-s18
Liu Z, Hu ZS, Qiu Y, Zhang Z, Zhao ZH, Han X, Zhu ZZ (2017) Role of clavicle chest cage angle difference in predicting postoperative shoulder balance in Lenke 5C adolescent idiopathic scoliosis patients after selective posterior fusion. Orthop Surg 9:86–90. https://doi.org/10.1111/os.12305
Han X, Liu Z, Qiu Y, Sha S, Yan H, Jin M, Zhu Z (2016) Clavicle chest cage angle difference: is it a radiographic and clinical predictor of postoperative shoulder imbalance in Lenke I adolescent idiopathic scoliosis? Spine 41:1346–1354. https://doi.org/10.1097/brs.0000000000001521
Terheyden JH, Wetterkamp M, Gosheger G, Bullmann V, Liljenqvist U, Lange T, Schulze Bovingloh A, Schulte TL (2017) Predictors of shoulder level after spinal fusion in adolescent idiopathic scoliosis. Eur Spine J. https://doi.org/10.1007/s00586-017-5210-8
Wang Y, Hansen ES, Hoy K, Wu C, Bunger CE (2011) Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine 36:1113–1122. https://doi.org/10.1097/BRS.0b013e3181f51e95
Akazawa T, Kotani T, Sakuma T, Minami S, Torii Y, Orita S, Inage K, Fujimoto K, Shiga Y, Inoue G, Miyagi M, Saito W, Ohtori S, Niki H (2017) Midlife changes of health-related quality of life in adolescent idiopathic scoliosis patients who underwent spinal fusion during adolescence. Eur J Orthop Surg Traumatol Orthop Traumatol. https://doi.org/10.1007/s00590-017-2027-4
Lenke LG, Bridwell KH, O’Brien MF, Baldus C, Blanke K (1994) Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation. Spine 19:1589–1597
Cao K, Watanabe K, Hosogane N, Toyama Y, Yonezawa I, Machida M, Yagi M, Kaneko S, Kawakami N, Tsuji T, Matsumoto M (2014) Association of postoperative shoulder balance with adding-on in Lenke Type II adolescent idiopathic scoliosis. Spine 39:E705–712. https://doi.org/10.1097/brs.0000000000000325
Cil A, Pekmezci M, Yazici M, Alanay A, Acaroglu RE, Deviren V, Surat A (2005) The validity of Lenke criteria for defining structural proximal thoracic curves in patients with adolescent idiopathic scoliosis. Spine 30:2550–2555
Acknowledgements
This study was supported by National Natural Science Fund of China (31870985) and Natural Science Fund of Shanghai (16ZR1449100).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, Y., Yang, M., Zhao, J. et al. Postoperative shoulder imbalance in adolescent idiopathic scoliosis: risk factors and predictive index. Eur Spine J 28, 1331–1341 (2019). https://doi.org/10.1007/s00586-019-05933-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05933-2