Abstract
Inflammation is a well-recognized factor associated with preeclampsia (PE). Stress granules (SGs) have been shown to play an important role in regulating inflammation and immune responses. However, whether SGs are involved in the pathogenesis of PE has not been studied. Here, we evaluated the expression of SG components in placenta of pregnancies with PE. Placental samples or serum were collected from PE patients (n = 31) or healthy age-matched pregnancy (n = 17). mRNA expressions of SG-associated genes in placenta from PE or normal pregnancies were detected by real-time quantitative PCR, and protein expressions of HuR and G3BP were detected using western blot. Immunofluorescence staining was performed to evaluate SG components expression in placentas or 10% serum treated HTR-8/Svneo cells using antibodies against HuR and G3BP. Our study showed higher levels of elavl1, lsm2, lsm4, and ago1 mRNA expression and SG marker proteins expression in placental homogenates of PE patients. HuR/G3BP-positive SG structure was further observed in placental villi of PE by immunofluorescence assay. Besides, serum from PE patients could induce SG aggregation in human trophoblast cell line HTR-8/Svneo cells, suggesting the involvement of SGs in the development of PE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preeclampsia (PE) is a hypertensive disorder of pregnancy caused by multiple factors including gene, heredity, epigenetics, and immunity. It is a primary cause of high maternal and perinatal morbidity and mortality and affects 3–5% of pregnancies around the world [1, 2]. The current understanding of the underlying etiology and pathogenesis of the disease is based on a two-stage model of PE theory. Ischemia and hypoxia lead to shallow invasion of the trophoblast and remodeling dysfunction of the spiral arteries. The excessive placental oxidative stress will induce the release of inflammatory cytokines (TNF-α, IL-2), anti-angiogenic factors (soluble Fms-like tyrosine kinase-1, sEng), or alarmins (uric acid, cell-free fetal DNA) into the maternal circulation (the first stage) [3,4,5,6,7,8]. These factors or alarmins further elicit an overreaction of inflammatory response, including vascular endothelial injury, thrombosis, and activation of renin angiotensin aldosterone system. All of these eventually lead to organ hypoperfusion and dysfunction as part of composite PE manifestation (the second stage) [4, 6, 7]. Although more and more studies have been done on the pathogenesis of PE, the incidence of PE has not declined. It is urgent to develop new intervention targets and therapeutic strategies for PE patients.
Stress granules (SGs) are dense particles (non-membranous cytoplasmic foci) formed in the cytoplasm of eukaryotic cells. RNA SGs primarily consist of poly(A)+ mRNAs containing 48S preinitiation complexes, small ribosomal subunits, mRNA decay factor tristetraprolin, translation initiation factors such as eukaryotic translation initiation factor-4E (eIF4E), eIF4G, eIF4A, and eIF4B, and many RNA-binding proteins that regulate mRNA structure and function, including HuR, Staufen, Smaug, TTP, Fragile X mental retardation protein, G3BP, CPEB, and SMN. SGs also contain putative scaffold proteins such as Fas-activated serine/threonine phosphoprotein [9]. The assembly of SGs is considered to be a protection mechanism of cells in response to a variety of stress stimuli such as ischemia, hypoxia, oxidative stress, heat shock, or viral infection. When stressed, the process of protein translation is suspended temporarily. mRNAs are released from ribosomes and enter SGs with the envelope of specific RNA-binding proteins. Once the pressure is released, mRNAs leave the SG structure and then be transported to cytoplasm for protein translation or to processing bodies (PBs) for RNA degradation [10,11,12]. SGs are highly conserved cytoplasmic RNP granules, which play an important role in cell activities, such as translation regulation, cell apoptosis, virus infection, inflammatory response, and cellular lesions caused by protein misfolding [12].
However, it has not been reported whether SGs are involved in the pathogenesis of PE. This study was designed to evaluate the expression of SG components in placenta of pregnancies with PE. Placental samples or serum were collected from PE patients or healthy age-matched pregnancy. Placental histology was analyzed by H&E staining. mRNA expressions of SG-associated genes and protein expressions of HuR and G3BP in placenta from PE or normal pregnancies were detected. Immunofluorescence staining was also performed to evaluate SG components expression in placentas or serum treated HTR-8/Svneo cells.
Materials and Methods
Human Subjects
Placental samples were collected from PE patients (n = 31) with severe features or healthy age-matched pregnancy (n = 17) who had visited the Department of Obstetrics in the Affiliated Hospital of Qingdao University from June 2018 to June 2020. The diagnosis of PE with severe features followed the guidelines of the task force on hypertension during pregnancy [13]. PE patients has also mechanistically been classified into early onset PE (eo-PE, n = 13) (< 34 gestational weeks) and late onset PE (lo-PE, n = 18) (≥ 34 gestational weeks), based on gestational age at diagnosis and/or delivery [14]. Pregnancy controls were selected from gestational age-matched pregnancy deliveries, including pre-term delivery due to cervical incompetence or acute fetal distress caused by umbilical cord entanglement. Gestational or pre-existing diabetes, chronic hypertension, daily smoking, fetal death, fetal malformations, and multiple pregnancies were excluded. Demographic information is shown in Table 1 (see also supplementary material, Table S1). After washed with chilled PBS solution, a portion of the placental specimen was embedded in Tissue-Tek optimal cutting temperature (OCT) compound ( Sakura Finetek, CA, USA) for immunofluorescence analysis; a portion was fixed in 10% formalin for hematoxylin and eosin staining; and the remaining was stored at − 80 °C. Serum samples were collected and stored at – 80 °C.
The study guidelines were approved by the Affiliated Hospital of Qingdao University Review Board, and informed consent was obtained from all subjects.
Cell Culture
Human trophoblast cell line HTR-8/SVneo was purchased from Cell Bank (Chinese Academy of Sciences, Shanghai) and cultured in DMEM/F12 (GIBCO) supplemented with penicillin-streptomycin and 10% FBS at 37 °C in a 5% CO2 atmosphere. For immunofluorescent staining, cells were seeded at 200,000 cells/well onto 12-well culture plates. After washed with serum-free medium, cells were treated with 10% sera from normal pregnancy or PE patients for 24 h, and then fixed with 4% paraformaldehyde for 15 min.
qRT-PCR
Total RNA was extracted from placental samples with RNAiso Plus (TAKARA) and were then reverse-transcribed to cDNA using Evo M-MLV RT Premix (Accurate Biotechnology). Real-time quantitative PCR analysis was performed using SYBR GREEN mix (TAKARA) on an ABI 7500 (Applied Biosystems). Primers are shown in Table 2.
Western Blot
Placental samples were lysed in 2% SDS lysis buffer. Western blot was detected as described previously [13]. The following primary antibodies were used for PVDF membranes incubation: anti-GAPDH (AB0037, Abways), anti-α-tubulin (11224-1, Proteintech), anti-HuR/ELAVL1 (ab200342, Abcam), anti-G3BP (ab56574, Abcam), and then the PVDF membranes were reacted with HRP-conjugated secondary antibodies, respectively (Pierce, 1:5,000). The proteins were detected by luminescent substrate (WBKLS0050, Millipore) and quantified by ImageJ.
Immunofluorescence Assays
Immunofluorescence assays were conducted as previously described [15]. In brief, Tissue-Tek OCT (Sakura Finetek, CA, USA) embedded placental samples was sectioned for 5 μm with a Freezing Microtome (Leica). The sections or HTR8/SV-neo cells were fixed in 4% paraformaldehyde for 15 min, penetrated with 0.1% Triton-X 100 for 30 min, blocked with 5% BSA for 1 h and treated with anti-HuR/ELAVL1 antibody (ab200342, Abcam) and anti-G3BP antibody (ab56574, Abcam) at 4 °C overnight, and then reacted with fluorescent secondary antibody (Abcam), respectively.
Histopathology
Placental samples were fixed in 10% formalin and embedded in paraffin, after which 4-μm-thick sections were cut and stained with hematoxylin and eosin (H&E).
Statistical Analysis
The differences between study groups are compared via Wilcoxon rank-sum test or chi-squared test, respectively. A two-sided p value of < 0.05 is considered as statistically significant.
Results
Characteristics of the PE Patients
The demographic characteristics of the PE patients with severe features are presented in Table 1. No differences in age, height, gestational week, and hemoglobin at delivery were noted between both groups. However, weight and body mass index before delivery, systolic/diastolic blood pressure, ALT/AST, uric acid, lactate dehydrogenase, platelet, neonatal Apgar score, and birth weight of infants were significantly different between both groups.
H&E Staining of Placental Samples from PE
Inflammation is involved in the pathological process of PE. We therefore first analyzed the pathological characteristics of placental samples by H&E staining (n = 6). Healthy pregnant women had the morphological characteristics of normal placenta (Fig. 1a). The trophoblasts around the placental villi were normal, and the structure of villous interstitium was complete and well-defined without deposits and swelling. In addition, the size of vascular lumen of villi was normal, and clear red blood cells could be seen in the blood vessels (Fig. 1a).While in the placenta of PE patients, villous ischemic infarction was observed with infiltration of small to slightly large-sized round-shaped cells (Fig. 1b), and the blood vessels in villi interstitium were dilated and congested, and fibrin was deposited around the villi (Fig. 1c, d).
RNA SG-Associated Gene Expression in Placenta from PE
SGs play an important role in regulating inflammation and immune responses [12]. With the use of quantitative real-time PCR, we analyzed the expression of several RNA SG-associated genes, and found many of them, such as elavl1, lsm2, lsm4, and ago1 (Fig. 2) were increased in human placental samples of PE (p < 0.05, n = 6) compared with healthy controls. We further analyzed the expression of RNA SG-associated genes in eo-PE vs. gestational age-matched pregnancy deliveries (eo-control) (< 34 gestational weeks) and lo-PE with severe features vs. gestational age-matched pregnancy deliveries (lo-control) (≥ 34 gestational weeks) (Table S1). RNA SG-associated genes, such as elavl1, lsm2, lsm4, and ago1 were significantly increased in human placental samples of eo-PE compared with eo-control (p < 0.05, n = 6). In addition, increased abundance of RNA SG-associated genes was also observed in the placenta from lo-PE relative to lo-control (p < 0.05, n = 6). However, no difference in RNA SG-associated genes expression was observed in the placentas from eo-PE with severe features vs. lo-PE with severe features (Fig. S1A).
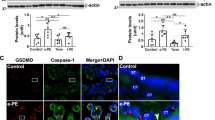
SG Aggregation in Placenta from PE
We further detected two classic SG marker proteins (HuR and G3BP) by western blot. The result showed HuR and G3BP protein expression was markedly increased in placenta from PE compared with control (p < 0.05, n = 8) (Fig. 3). Similar to quantitative real-time PCR result, no difference in HuR expression was observed in the placenta from eo-PE with severe features vs. lo-PE with severe features (Fig. S1B). To confirm the aggregation of SGs in PE, we performed immunofluorescence assay. As shown in Fig. 4, HuR or G3BP containing SGs were observed in placenta from PE, but barely in control group (n = 6).
Serum from PE Induces SG Aggregation in HTR-8/Svneo Cells
PE is an excessive inflammatory reaction of women to pregnancy. To determine whether PE serum can induce the formation of SGs, HTR-8/Svneo cells were treated with 10% serum from PE or healthy pregnancy for 24 h and analyzed HuR or G3BP containing SGs by immunofluorescence (n = 6). Confocal imaging revealed that PE serum markedly induced the formation of SGs but not control serum (Fig. 5).
Immunofluorescent staining of HuR or G3BP containing SGs in HTR-8/Svneo cells. HTR-8/Svneo cells were exposed to 10% PE serum or healthy pregnancy serum for 24 h and the expression of HuR and G3BP was detected by fluorescent microscope in situ (n = 6). Data are representative of three independent experiments. Scale bar 25 μm
Taking together, we conclude that SGs were aggregated in placenta from PE patients.
Discussion
The present study showed obvious SG aggregation in placenta from PE patients. We found higher levels of mRNA for SG-associated genes and SG marker proteins expression in placental homogenates of PE patients. HuR/G3BP-positive SG structure was further observed in placental villi of PE by IF assay. SGs studies in the PE are scarce. To our knowledge, this study is the first to investigate SGs formation in placenta from PE patients.
During normal pregnancy, trophoblasts in the placenta have growth characteristics similar to tumor cells, such as proliferation and invasion, and they are precisely regulated [16]. It was found that when the placenta was delivered, the symptoms of patients with preeclampsia were improved. Therefore, the placenta was considered as the initial focus of PE [17, 18]. Due to insufficient trophoblast infiltration and spiral artery remodeling defects, placental blood perfusion was insufficient and lead to placental shallow implantation, and then cause PE diseases [7]. In our study, we found abnormal pathological characteristics in the placenta of PE patients with villous ischemic infarction, dilated and congested blood vessels in villi interstitium, and deposited fibrin around the villi.
Stressed cells form SGs through interactions network that involve HuR and G3BP [9]. Here, we found HuR and G3BP protein expression was markedly increased in placenta from PE, and further detected HuR/G3BP-positive SG structure in placental villi of women with PE. Notably, no difference in RNA SG-associated genes or HuR protein expression was observed in the placentas from eo-PE with severe features vs. lo-PE with severe features. The expression of SGs in placenta of pregnancies with mild PE needs to be evaluated in the future. The change of HuR can lead to the occurrence and development of many inflammation related diseases. Many pro-inflammatory factors, such as TNF-α, IL-4, or IL-3 mRNA, contain AU-rich elements (AREs) in the 3′-untranslated region. HuR can improve their stability by targeting the AREs and further upregulate their expression in cells, so HuR protein is considered to promote inflammation in cells [19], while in mouse myeloid cells, the overexpression of HuR gene can inhibit lipopolysaccharide induced inflammation with decreased levels of TNF-α, IL-1 β, and TGF-β 1 in the blood [20]. The result confirmed that the main function of HuR in the body is to inhibit inflammatory reaction. Further research on the role of HuR whether to promote or inhibit inflammation in PE is needed.
Severe systemic inflammatory response has been reported in PE. The levels of TNF-α, IFN-γ, CRP, and IL-8 in serum of PE patients were obviously higher than those of healthy pregnant women [21,22,23,24]. In mucositis, proinflammatory cytokines IFN-γ and TNF-α can induce the formation of SG through the phosphorylation of eIF2 α [25]. In accordance with that, we also found serum from PE, not healthy pregnancy, can induce SG aggregation in HTR-8/Svneo cells, which can be explained by the higher levels of proinflammatory cytokines in PE serum. The impaired invasion of the trophoblast is an important factor in the development of PE. Placental hypoperfusion in PE leads to placental ischemia and hypoxia, and cells are in a state of continuous oxidative stress, resulting in the damage of trophoblast function. At the same time, the increase of endotoxic substances and inflammatory mediators reduces the corresponding vasodilation function, resulting in the release of vascular endothelial cell active factors, leading to endothelial cell injury or dysfunction [3, 4, 8]. The injured placenta-released extracellular vesicles also disrupted the endothelial integrity and induced vasoconstriction [26]. The formation of SGs makes mRNA and many proteins form high aggregates in the cells which promotes their mutual regulation, and plays an important role in post transcriptional regulation, apoptosis, immunity, and inflammation response [12]. The components of SGs are different under different stimulation conditions. It will be very interesting to explore the components of SGs in trophoblast cell and the effect on trophoblast function.
In summary, we found HuR/G3BP-positive SG aggregated in placental tissue of PE patients and serum from PE patients can induce SG aggregation in human villous trophoblasts cell line HTR-8/Svneo. The findings suggest the involvement of SGs in the development of PE. SGs can be triggered by a variety of exogenous and endogenous stimuli. Understanding the formation of SGs involved in PE pathogenesis may promote the development of targeted therapy. Further study should focus on the regulation of SG assembly in PE and whether inhibition of SG components can be a feasible target for PE therapy.
References
Mol B, Roberts C, Thangaratinam S, Magee L, de Groot C, Hofmeyr G. Pre-eclampsia. Lancet. 2016;387(10022):999–1011. https://doi.org/10.1016/s0140-6736(15)00070-7.
Young B, Levine R, Karumanchi S. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010;5:173–92. https://doi.org/10.1146/annurev-pathol-121808-102149.
Sharma S. Autophagy-based diagnosis of pregnancy hypertension and pre-eclampsia. Am J Pathol. 2018;188(11):2457–60. https://doi.org/10.1016/j.ajpath.2018.09.001.
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim Y, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006;12(6):642–9. https://doi.org/10.1038/nm1429.
Tong M, Cheng S, Chen Q, DeSousa J, Stone P, James J, et al. Aggregated transthyretin is specifically packaged into placental nano-vesicles in preeclampsia. Sci Rep. 2017;7(1):6694. https://doi.org/10.1038/s41598-017-07017-x.
Cheng S, Davis S, Sharma S. Maternal-fetal cross talk through cell-free fetal DNA, telomere shortening, microchimerism, and inflammation. Am J Reprod Immunol. 2018;79(5):e12851. https://doi.org/10.1111/aji.12851.
Poon L, Shennan A, Hyett J, Kapur A, Hadar E, Divakar H, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(suppl 1):1–33. https://doi.org/10.1002/ijgo.12802.
Schmella M, Assibey-Mensah V, Parks W, Roberts J, Jeyabalan A, Hubel C, et al. Plasma concentrations of soluble endoglin in the maternal circulation are associated with maternal vascular malperfusion lesions in the placenta of women with preeclampsia. Placenta. 2019;78:29–35. https://doi.org/10.1016/j.placenta.2019.02.014.
Anderson P, Kedersha N. Stress granules: the Tao of RNA triage. Trends Biochem Sci. 2008;33(3):141–50. https://doi.org/10.1016/j.tibs.2007.12.003.
Mokas S, Mills J, Garreau C, Fournier M, Robert F, Arya P, et al. Uncoupling stress granule assembly and translation initiation inhibition. Mol Biol Cell. 2009;20(11):2673–83. https://doi.org/10.1091/mbc.e08-10-1061.
Kedersha N, Stoecklin G, Ayodele M, Yacono P, Lykke-Andersen J, Fritzler M, et al. Stress granules and processing bodies are dynamically linked sites of mRNP remodeling. J Cell Biol. 2005;169(6):871–84. https://doi.org/10.1083/jcb.200502088.
Decker C, Parker R. P-bodies and stress granules: possible roles in the control of translation and mRNA degradation. Cold Spring Harb Perspect Biol. 2012;4(9):a012286. https://doi.org/10.1101/cshperspect.a012286.
Roberts J, August P, Bakris G, Barton J, Bernstein I, Druzin M, et al. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet. Gynecol. 2013;122(5):1122–31. https://doi.org/10.1097/01.aog.0000437382.03963.88.
Yung H, Atkinson D, Campion-Smith T, Olovsson M, Charnock-Jones D. Bur ton G. Differential activation of placental unfolded protein response pathways implies heterogeneity in causation of early- and late-onset preeclampsia. J. Pathol. 2014;234(2):262–76. https://doi.org/10.1002/path.4394.
Li Z, Chen Z, Zhang T, Wei C, Shi W. TGF-β and NF-κB signaling pathway crosstalk potentiates corneal epithelial senescence through an RNA stress response. Aging. 2016;8(10):2337–54. https://doi.org/10.18632/aging.101050.
Fisher S. The placental problem: linking abnormal cytotrophoblast differentiation to the maternal symptoms of preeclampsia. Reprod Biol Endocrinol. 2004;2:53. https://doi.org/10.1186/1477-7827-2-53.
George E, Granger J. Mechanisms and potential therapies for preeclampsia. Curr Hypertens Rep. 2011;13(4):269–75. https://doi.org/10.1007/s11906-011-0204-0.
Warrington J, George E, Palei A, Spradley F, Granger J. Recent advances in the understanding of the pathophysiology of preeclampsia. Hypertension. 2013;62(4):666–73. https://doi.org/10.1161/hypertensionaha.113.00588.
Fan J, Ishmael F, Fang X, Myers A, Cheadle C, Huang S, et al. Chemokine transcripts as targets of the RNA-binding protein HuR in human airway epithelium. J Immunol. 2011;186(4):2482–94. https://doi.org/10.4049/jimmunol.0903634.
Katsanou V, Papadaki O, Milatos S, Blackshear P, Anderson P, Kollias G, et al. HuR as a negative posttranscriptional modulator in inflammation. Mol Cell. 2005;19(6):777–89. https://doi.org/10.1016/j.molcel.2005.08.007.
Luppi P, Deloia J. Monocytes of preeclamptic women spontaneously synthesize pro-inflammatory cytokines. Clin Immunol. 2006;118(2-3):268–75. https://doi.org/10.1016/j.clim.2005.11.001.
Raghupathy R. Cytokines as key players in the pathophysiology of preeclampsia. Med Princ Pract. 2013;22(suppl 1):8–19. https://doi.org/10.1159/000354200.
Peraçoli J, Rudge M, Peraçoli M. Tumor necrosis factor-alpha in gestation and puerperium of women with gestational hypertension and pre-eclampsia. Am J Reprod Immunol. 2007;57(3):177–85. https://doi.org/10.1111/j.1600-0897.2006.00455.x.
Tangerås L, Silva G, Stødle G, Gierman L, Skei B, Collett K, et al. Placental inflammation by HMGB1 activation of TLR4 at the syncytium. Placenta. 2018;72:53–61. https://doi.org/10.1016/j.placenta.2018.10.011.
Hu S, Claud E, Musch M, Chang E. Stress granule formation mediates the inhibition of colonic Hsp70 translation by interferon-gamma and tumor necrosis factor-alpha. Am J Physiol Gastrointest Liver Physiol. 2010;298(4):G481–92. https://doi.org/10.1152/ajpgi.00234.2009.
Han C, Wang C, Chen Y, Wang J, Xu X, Hilton T, et al. Placenta-derived extracellular vesicles induce preeclampsia in mouse models. Haematologica. 2020;105(6):1686–94. https://doi.org/10.3324/haematol.2019.226209.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 127 kb)
Rights and permissions
About this article
Cite this article
Ma, C., Li, C., Shao, S. et al. Assembly of Cytoplasmic Stress Granules in Placentas in Women with Preeclampsia. Reprod. Sci. 28, 2869–2877 (2021). https://doi.org/10.1007/s43032-021-00592-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00592-5