Abstract
Pre-eclampsia, one of the major disorders of pregnancy, is characterized by inadequate trophoblast invasion and defective trophoblast-mediated remodeling of placental vasculature. Hypoxia-inducible transcription factor (HIF)-2α plays a critical role in regulating cellular function of trophoblasts; however, its role in placental development and in the pathogenesis of pre-eclampsia remains elusive. CCK-8 assay was used to detect cell viability. Invasion assay was performed to determine the effect of HIF-2α on trophoblast function. Flow cytometry was used for detecting apoptosis and cell cycle. The mRNA and protein expressions of HIF-2α, VEGF, iNOS, and ET-1 were determined by quantitative real-time PCR and western blot techniques. The roles of HIF-2α in JEG-3 trophoblast cells were examined using siRNA technology. The presence of HIF-2α siRNA reduced the levels of cell viability after 48 h incubation, and the cell viability further reduced at 72 h. Besides, HIF-2α siRNA enhanced trophoblast apoptosis, as determined by flow cytometric measurement. Increased G1-phase and decreased S-phase cell population were induced by HIF-2α siRNA based on the determination of cell cycle distribution using propidium iodide staining. Furthermore, the invasive ability of JEG-3 trophoblasts was significantly reduced by HIF-2α siRNA. In addition, knockdown of the HIF-2α gene significantly decreased VEGF, iNOS, and ET-1 levels in JEG-3 human trophoblasts. Our findings provide preliminary evidence of the functions of HIF-2α in trophoblast biology and suggest that the downregulation of HIF-2α enhances cell apoptosis and limits trophoblast invasion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pre-eclampsia is one of the most frequently encountered medical complication of pregnancy and affects 3–5% of pregnant women worldwide [1]. Pre-eclampsia is typically characterized by new-onset hypertension, proteinuria, and other systemic disturbances in the second half of pregnancy, during labor, or in the early period after delivery [2], and it confers adverse pregnancy outcomes as well as maternal and fetal morbidity. Currently, the etiology of pre-eclampsia remains to be fully understood.
Although enormous efforts have been put in the recent decades in determining the mechanisms underlying the development of pre-eclampsia, the results remain inconclusive. Hence, understanding the molecular mechanisms underlying the pathogenesis of pre-eclampsia and searching for reliable targeting biomarkers are still the primary tasks for pre-eclampsia therapy.
Delivery of the placenta is the only known cure for pre-eclampsia, implying that the placenta is the principle contributor to the pathogenesis of pre-eclampsia. During early normal placental development, extravillous trophoblasts of fetal origin invade the uterine spiral arteries of the deciduas and myometrium and remodel the placental vasculature to allow sufficient placental perfusion for nourishment of the fetus. However, inadequate placental trophoblast invasion has been well documented in pre-eclampsia, and it is generally believed to be the main cause for placental underperfusion and development of pre-eclampsia [1]. The molecular regulatory networks underlying trophoblast invasion have not been well defined. A number of genes that are associated with preelcampsia, such as hypoxia-inducible transcription factors (HIF), have been demonstrated to play a role in trophoblast invasion in vitro [3, 4], yet a lot more remains to be explored.
HIF-2α, also known as endothelial PAS (Per, Arnt, Sim) domain protein 1 (EPAS-A), belongs to the PAS family of basic helix-loop-helix (bHLH) transcription factors. HIF has been regarded as potential contributor to the normal development of the human placenta [5]. Under hypoxic conditions, HIF-2α over-expression owing to excessively activated hypoxic response pathway is considered the key point in the hypoxic dysfunction of trophoblasts in preeclamptic placenta [6]. However, no studies have provided evidence regarding the role of HIF-2α in normal human trophoblasts under conditions of normoxia.
These results suggest that HIF-2α play a critical role in maintaining trophoblast biology and that their downregulation contribute to the pathogenesis of pre-eclampsia. In this study, we aimed to investigate the effects of HIF-2α on JEG-3 trophoblast biology using gene knockdown technique and analyze the involved mechanisms as well as the interrelationships of HIF-2α in human trophoblasts.
Materials and Methods
Cell Culture
The JEG-3 trophoblast cell line was obtained from the Cell Culture Center, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences (Beijing, China), and cultured in Dulbecco’s modified Eagle’s medium (DMEM, Gibco, Carlsbad, CA, USA) supplemented with 10% (v/v) fetal bovine serum (FBS, Gibco, Carlsbad, CA, USA) in a humidified culture chamber under conditions of 95% air/5% CO2 at 37 °C.
Transfection with Small Interfering RNA (siRNA)
JEG-3 cells were seeded at a density of 1 × 105 cells/ml into a 6-well plate (2 ml/well). The adherent cells were transfected with three designed HIF-2α siRNAs: siRNA1, sense: CUCCUCAGUUUGCUCUGAATT, anti-sense: UUCAGAGCAAACUGAGGAGTT; siRNA2, sense: CAGAACUGAUUGGUUACCATT, anti-sense: UGGUAACCAAUCAGUUCUGTT; and siRNA3, sense: CAUCUUUGGAUAACGACCUTT, anti-sense: AGGUCGUUAUCCAAAGAUGTT (GenePharma, Shanghai, China), using the Exfect2000 Transfection Reagent (Vazyme Biotech Co. Ltd., Nanjing, China), in accordance with the manufacturer’s instructions. A negative control (NC) siRNA was used as the transfection control. Six hours after infection, the medium was replaced with fresh complete culture medium (CCM). Cells were harvested 72 h after changing medium, and the expression level of HIF-2α was examined by qPCR to evaluate the infection efficiency. Among the three siRNAs, siRNA3 was the most powerful to silence the expression of HIF-2α (Fig. 1). Therefore, HIF-2α siRNA3 was used for further studies.
CCK-8 Assay for Cell Viability
Cell viability was determined using cell counting kit-8 (CCK-8; Multisciences (Lianke) Biotech Co., Ltd., Hangzhou, China) according to the manufacturer’s instructions. JEG-3 cells were seeded at a density of 5 × 103 cells/well into a 96-well plate and transfected with siRNAs to HIF-2α. After transfection for 6 h, the medium was changed to fresh CCM followed by incubation for up to 24, 48, and 72 h. CCK-8 solution (10 μl) was then added to each well of the plate at indicated time points, followed by 1 h incubation at 37 °C. The optical density was measured at 450 nm using a microplate reader (SpectraMax Plus384, Molecular Devices, San Francisco, CA, USA).
Annexin V-FITC/Propidium Iodide (PI) Staining for Detecting Cell Apoptosis
Cell apoptosis was measured using the Annexin V-FITC/PI apoptosis kit (Multisciences (Lianke) Biotech Co., Ltd., Hangzhou, China) according to the manufacturer’s instructions. Briefly, cells were collected at the indicated time points and washed once with cold PBS, followed by centrifugation (1, 500 rpm, 5 min). The pellet was suspended in 500 μl binding buffer containing Annexin V-FITC and PI solution and was stained in the dark for 5 min at RT. The percentage of cell apoptosis was determined using the BD Accuri C6 personal flow cytometer (Piscataway, NJ, USA).
Cell Cycle Analysis
Cell cycle was measured using the Cell Cycle Staining Kit (Multisciences (Lianke) Biotech Co., Ltd., Hangzhou, China) according to the manufacturer’s instructions. Briefly, cells were collected at the indicated time points and washed once with cold PBS, followed by centrifugation (1, 500 rpm, 5 min). The pellet was suspended in 1 ml DNA staining solution containing 10 μl permeabilization solution and was stained in the dark for 30 min at RT. Analysis of cell cycle distribution was performed using the BD Accuri C6 personal flow cytometer (Piscataway, NJ, USA).
Transwell Invasion Assay
The Transwell assay was performed to assess cell invasion in vitro at 48 and 72 h after transfection. Briefly, 5 × 104 cells re-suspended in 200 μl 2% FBS/DMEM were placed in the upper chamber of the Transwell apparatus (Corning, New York, USA) that was precoated with phenol red-free Matrigel (Corning, BD Biocoat, USA), and the Transwell chambers were placed in 24-well plates containing 500 μl 10% FBS/DMEM in each well, followed by incubation at 37 °C for 24 h. Thereafter, the non-invasive cells and Matrigel on the top surface of the Transwell chamber membrane were removed using a cotton swab. The invaded cells adherent to the bottom of the chamber membrane were fixed with 4% paraformaldehyde (PFA, Sinopharm Chemical Reagent Co., Ltd., Shanghai, China) and stained with crystal violet (Sigma-Aldrich, Saint Louis, MO, USA). Images were obtained with an inverted optical microscope (IX73, Olympus, Japan); for each chamber, five random fields (200×) were investigated, and the average numbers of invaded cells were quantified.
Real-Time PCR
Total RNA was extracted with the Total RNA Fast Extraction Kit (Spin-column) (Generay Biotech, Co., Ltd., Shanghai, China) following the manufacturer’s instructions. Reverse transcription was conducted using the HiScript II Q RT SuperMix for qPCR Kit (Vazyme Biotech Co., Ltd., Nanjing, China) following the manufacturer’s protocol. Quantitative real-time PCR was performed using the ChamQ SYBR Color qPCR Master Mix Kit (Vazyme Biotech Co., Ltd., Nanjing, China), and fluorescence amplification was detected by the CFX Connect Real-Time PCR Detection System (Bio-Rad, USA). The PCR primers used are summarized in Table 1.
Western Blotting
JEG-3 cells were transfected with the indicated vector(s) in the method described above. At 48 h and 72 h post-transfection, protein levels of VEGF, iNOS, and ET-1 in the transfected cells were determined by western blot analysis. Cells were lysed with cell lysis buffer (Beyotime, Beijing, China), and total proteins were extracted following the standard protocol. The BCA Protein Assay Kit (Beyotime, Beijing, China) was used for protein quantification following the manufacturer’s instructions. Next, a total of 30 μg proteins from each sample were separated by 8% SDS-PAGE gel followed by electro transfer to polyvinylidene difluoride (PVDF) membranes (Millipore, Bedford, MA, USA) for immunoblotting. PVDF membranes were blocked with 5% non-fat milk solution and incubated with rabbit primary antibodies against VEGF (1:2000) or iNOS (1:500) or mouse primary antibody against ET-1 (1:500) (Abcam, Cambridge, MA, USA) overnight at 4 °C followed by probing with horseradish peroxidase (HRP)-labeled goat anti-rabbit or anti-mouse IgG secondary antibody (1:5000; MultiSciences (Lianke) Biotech, Co., Ltd., Hangzhou, China) at room temperature for 2 h and signal detection using the ECL solution (Beyotime Biotechnology, Shanghai, China). To verify equal loading and transfer, the membrane was stripped with the stripping buffer (Beyotime Biotechnology, Shanghai, China) and re-probed with anti-GAPDH antibody (MultiSciences (Lianke) Biotech, Co., Ltd., Hangzhou, China) as the internal reference. Chemiluminescent images of specific protein bands were obtained using the Bio-Rad Chemidoc XRS Gel Pro Imaging System (Watertown, MA, USA).
Statistical Analysis
All data are presented as the mean ± standard deviation (SD). Unpaired Student’s t test was used to analyze differences between two groups. Statistical analyses were performed using the GraphPad Prism Software (version 5.0; San Diego, CA, USA). The difference was considered statistically significant when P < 0.05.
Results
Downregulation of HIF-2α Reduced the Viability of JEG-3 Cells
The human trophoblast cell line JEG-3 was transfected with NC siRNA or HIF-2α siRNA, and the mRNA level of HIF-2α remarkably reduced in cells transfected with the target genes compared with the NC group (Fig. 1). Among the three siRNAs, siRNA-3 was the most powerful for gene silencing. Therefore, we used siRNA-3 for subsequent analysis. No significant changes in cell viability were observed at 24 h in cells transfected with target genes compared with that in control cells (Fig. 2). However, downregulation of HIF-2α significantly reduced the viability of JEG-3 at 48 and 72 h as assessed by the CCK-8 assay (Fig. 2). Our results indicate that the downregulation of HIF-2α reduced viability of cultured trophoblasts.
Downregulation of HIF-2α Increased Apoptosis in JEG-3 Cells
To further examine the role of HIF-2α, apoptosis in cultured JEG-3 cells was analyzed. Using Annexin V-FITC/PI staining, we observed a significantly higher apoptotic rate in cells with downregulated HIF-2α levels than in control (Fig. 3). These findings indicate that the downregulation of HIF-2α enhances apoptosis in cultured trophoblasts.
HIF-2α-siRNA increased apoptosis of JEG-3 trophoblast cells. Cells were transfected with HIF-2α specific siRNA for 6 h; then, Annexin-FITC-based flow cytometry assay was performed to detect cell apoptosis at 48 h (a and b) and 72 h (c and d). N = 3, **P < 0.01, ***P < 0.001 vs. NC; NC, negative control siRNA
Downregulation of HIF-2α Blocked G1 to S Transition in JEG-3 Cells
We also examined the effect of HIF-2α downregulation on changes in the cell cycle. According to the cell cycle assay, downregulation of HIF-2α significantly increased cell population in the G1 phase compared with that in controls (±, P < 0.05; ±, P < 0.01; Fig. 4). These results suggest that the downregulation of HIF-2α blocked cell cycle transition from G1-phase to S-phase.
HIF-2α-siRNA increased G1-phase cell population and decreased S-phase apoptosis of JEG-3 trophoblast cells. Cells were transfected with HIF-2α specific siRNA for 6 h; then, cell cycle at 48 h (a–c) and 72 h (d–f) was analyzed using a DNA staining kit. N = 3, ***P < 0.001 vs. NC; NC, negative control siRNA
Downregulation of HIF-2α Inhibited the Invasion of JEG-3 Cells
To study the role of HIF-2α on human trophoblast function, the Matrigel membrane invasion assay was used. Matrigel-based invasion assay showed that the invasiveness of JEG-3 cells was prominently limited after HIF-2α siRNA transfection (Fig. 5). Cumulatively, these results indicated that the downregulation of HIF-2α significantly suppressed the invasiveness of JEG-3 cells, suggesting that HIF-2α play critical roles in trophoblast physiology.
HIF-2α-siRNA inhibited invasion function of JEG-3 trophoblast cells. Cells were transfected with HIF-2α specific siRNA for 6 h; then, Transwell invasion assay at 48 h (a and b) and 72 h (c and d) was used to evaluate the effect of HIF-2α-siRNA on JEG-3 cells. N = 5, *P < 0.05, **P < 0.01 vs. NC; NC, negative control siRNA
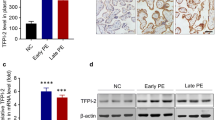
Effects of HIF-2α siRNA on the Expression of VEGF, iNOS, and ET-1 in JEG-3 Cells
We further investigated the molecular mechanism underlying the role of HIF-2α in JEG-3 cells. Downregulation of HIF-2α reduced the expression of HIF-2α, VEGF, iNOS, and ET-1 in cultured trophoblasts compared with that in the NC group (Fig. 6).
HIF-2α-siRNA decreased ET-1, iNOS, and VEGF expressions in JEG-3 trophoblast cells. Quantitative real-time PCR was used to determine mRNA changes (a–c). Western blotting analysis was performed to determine protein changes (d). Con, control. N = 3, *P < 0.05, **P < 0.01, ***P < 0.01 vs. NC; NC, negative control siRNA
Discussion
Pre-eclampsia (PE) is an adverse pregnancy syndrome characterized by the occurrence of hypertension and proteinuria in pregnant women [7]. The etiology and pathophysiology of the PE syndrome are not well understood. Dysfunctional trophoblast invasion has been considered an essential process in PE progression [8]. Trophoblast cells are a heterogeneous group of cells forming the fetal–maternal interface, exhibiting a wide spectrum of functions. JEG-3, epithelial cells of the human placenta, are widely used in studies on trophoblast biology. JEG-3 cells express HIF, including HIF-1α and HIF-2α. Notably, HIF-2α has been extensively studied in PE [6, 9,10,11]. However, the role of HIF-2α in the biology of trophoblast and their interrelationship remains unclear. In the current study, we employed small interference RNA (siRNA) to knockdown HIF-2α gene expression in vitro using JEG-3 cell lines. The properties of apoptosis and invasion were studied, and the involved molecular mechanisms were also explored using in vitro model.
The HIF-2α molecule plays an important role during pregnancy. Highet et al [12] found that HIF-2α level dramatically increased in trophoblasts during embryonic development. In the present study, we found that downregulation of HIF-2α resulted in decreased cell viability and enhanced apoptosis of JEG-3 human trophoblasts. Downregulation of HIF-2α also blocked cell cycle transition from G1-phase to S-phase in JEG-3 trophoblasts. Besides, the downregulation of HIF-2α remarkably inhibited invasion function of JEG-3 cells.
To date, inadequate trophoblast invasion is recognized as a major pathological factor for PE [13]. Extensive work has been conducted to address the molecular mechanisms underlying impaired trophoblast invasion, and a number of molecules have been identified to play roles in trophoblast invasion. Dubinsky et al. [14] noted that VEGF stimulates the invasion of trophoblast cells. Our in vitro experiment demonstrated that HIF-2α knockdown significantly suppressed the expression levels of VEGF in human trophoblastic JEG-3 cells. Inducible nitric oxide synthase (iNOS) is a signature molecule with diverse functions. Upregulation of this enzyme appears to be involved in several biological activities, including cell proliferation [15], migration [16], and apoptosis [17, 18]. Glynn et al. [19] found that increased iNOS enhanced cell motility and invasion in estrogen receptor-negative breast cancer cells. It was noted that trophoblast invasion, similar to tumor invasion, shares common biochemical mechanisms in this inherent nature [20]. Our study demonstrated that the downregulation of HIF-2α, which limited cell invasion, induced remarkable reduction of iNOS expression in JEG-3 human trophoblasts, consistent with previous observations in cancer. Endothelin-1 (ET-1), the prominent ET isoform, is a promoter of cell invasion [21]. In this study, our findings revealed that the downregulation of HIF-2α significantly reduced ET-1 levels in cultured human trophoblasts.
It was demonstrated that the modulation of HIF expression under different levels of O2 may result in different cellular responses [22]. Our findings demonstrate that under normoxic conditions, the downregulation of HIF-2α significantly impairs human JEG-3 trophoblast cells. In the present study, we only made observations under normoxic conditions. It would be interesting to compare both normoxia and hypoxia. Therefore, further studies are still needed to add value to these observations.
Conclusion
We demonstrated that the downregulation of HIF-2α could enhance apoptosis and suppress the invasion function of JEG-3 trophoblast cells. This study supports the cytoprotective properties of HIF-2α in maintaining normal human trophoblast biology. Considering the substantial contribution of apoptosis and cellular dysfunction in the pathophysiology of placental insufficiency, our findings suggest that targeting HIF-2α is a novel approach for therapeutic intervention to improve maternal and fetal health.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
References
Walker JJ. Pre-eclampsia. Lancet. 2000;356(9237):1260–5. https://doi.org/10.1016/s0140-6736(00)02800-2.
Young BC, Levine RJ, Karumanchi SA. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010;5:173–92. https://doi.org/10.1146/annurev-pathol-121808-102149.
Meade ES, Ma YY, Guller S. Role of hypoxia-inducible transcription factors 1alpha and 2alpha in the regulation of plasminogen activator inhibitor-1 expression in a human trophoblast cell line. Placenta. 2007;28(10):1012–9. https://doi.org/10.1016/j.placenta.2007.04.005.
Jadoon A, Cunningham P, McDermott LC. Regulation of fatty acid binding proteins by hypoxia inducible factors 1α and 2α in the placenta: relevance to pre-eclampsia. Prostaglandins Leukot Essent Fatty Acids. 2015;93:25–9. https://doi.org/10.1016/j.plefa.2014.09.004.
Rajakumar A, Conrad KP. Expression, ontogeny, and regulation of hypoxia-inducible transcription factors in the human placenta. Biol Reprod. 2000;63(2):559–69. https://doi.org/10.1095/biolreprod63.2.559.
Liu W, Wang SJ, Lin QD. Study on the expressions of PHD and HIF in placentas from normal pregnant women and patients with preeclampsia. Int J Biol Sci. 2014;10(3):278–84. https://doi.org/10.7150/ijbs.6375.
Pauli JM, Repke JT. Preeclampsia: short-term and long-term implications. Obstet Gynecol Clin North Am. 2015;42(2):299–313. https://doi.org/10.1016/j.ogc.2015.01.007.
Saito S, Nakashima A. A review of the mechanism for poor placentation in early-onset preeclampsia: the role of autophagy in trophoblast invasion and vascular remodeling. J Reprod Immunol. 2014;101-102:80–8. https://doi.org/10.1016/j.jri.2013.06.002.
Rajakumar A, Whitelock KA, Weissfeld LA, Daftary AR, Markovic N, Conrad KP. Selective overexpression of the hypoxia-inducible transcription factor, HIF-2alpha, in placentas from women with preeclampsia. Biol Reprod. 2001;64(2):499–506. https://doi.org/10.1093/biolreprod/64.2.499.
Zhou Y, Yuge A, Rajah AM, Unek G, Rinaudo PF, Maltepe E. LIMK1 regulates human trophoblast invasion/differentiation and is down-regulated in preeclampsia. Am J Pathol. 2014;184(12):3321–31. https://doi.org/10.1016/j.ajpath.2014.08.013.
Sasagawa T, Nagamatsu T, Morita K, Mimura N, Iriyama T, Fujii T, et al. HIF-2α, but not HIF-1α, mediates hypoxia-induced up-regulation of Flt-1 gene expression in placental trophoblasts. Sci Rep. 2018;8(1):17375. https://doi.org/10.1038/s41598-018-35745-1.
Highet AR, Khoda SM, Buckberry S, Leemaqz S, Bianco-Miotto T, Harrington E, et al. Hypoxia induced HIF-1/HIF-2 activity alters trophoblast transcriptional regulation and promotes invasion. Eur J Cell Biol. 2015;94(12):589–602. https://doi.org/10.1016/j.ejcb.2015.10.004.
Thilaganathan B. Placental syndromes: getting to the heart of the matter. Ultrasound Obstet Gynecol. 2017;49(1):7–9. https://doi.org/10.1002/uog.17378.
Dubinsky V, Poehlmann TG, Suman P, Gentile T, Markert UR, Gutierrez G. Role of regulatory and angiogenic cytokines in invasion of trophoblastic cells. Am J Reprod Immunol. 2010;63(3):193–9. https://doi.org/10.1111/j.1600-0897.2009.00778.x.
Pervin S, Singh R, Hernandez E, Wu G, Chaudhuri G. Nitric oxide in physiologic concentrations targets the translational machinery to increase the proliferation of human breast cancer cells: involvement of mammalian target of rapamycin/eIF4E pathway. Cancer Res. 2007;67(1):289–99. https://doi.org/10.1158/0008-5472.Can-05-4623.
Orucevic A, Bechberger J, Green AM, Shapiro RA, Billiar TR, Lala PK. Nitric-oxide production by murine mammary adenocarcinoma cells promotes tumor-cell invasiveness. Int J Cancer. 1999;81(6):889–96. https://doi.org/10.1002/(sici)1097-0215(19990611)81:6<889::aid-ijc9>3.0.co;2-2.
Kim PK, Zamora R, Petrosko P, Billiar TR. The regulatory role of nitric oxide in apoptosis. Int Immunopharmacol. 2001;1(8):1421–41. https://doi.org/10.1016/s1567-5769(01)00088-1.
Stepovaya YA, Zhavoronok TV, Starikov YV, Bychkov VA, Chasovskih NY, Starikova YG, et al. Regulatory role of nitric oxide in neutrophil apoptosis. Bull Exp Biol Med. 2008;146(6):737–40. https://doi.org/10.1007/s10517-009-0386-5.
Glynn SA, Boersma BJ, Dorsey TH, Yi M, Yfantis HG, Ridnour LA, et al. Increased NOS2 predicts poor survival in estrogen receptor-negative breast cancer patients. J Clin Invest. 2010;120(11):3843–54. https://doi.org/10.1172/jci42059.
Karmakar S, Dhar R, Das C. Inhibition of cytotrophoblastic (JEG-3) cell invasion by interleukin 12 involves an interferon gamma-mediated pathway. J Biol Chem. 2004;279(53):55297–307. https://doi.org/10.1074/jbc.M407013200.
Cervar M, Puerstner P, Kainer F, Desoye G. Endothelin-1 stimulates the proliferation and invasion of first trimester trophoblastic cells in vitro--a possible role in the etiology of pre-eclampsia? J Investig Med. 1996;44(8):447–53.
Jiang YZ, Li Y, Wang K, Dai CF, Huang SA, Chen DB, et al. Distinct roles of HIF1A in endothelial adaptations to physiological and ambient oxygen. Mol Cell Endocrinol. 2014;391(1-2):60–7. https://doi.org/10.1016/j.mce.2014.04.008.
Funding
This study was supported by National Natural Science Foundation of China (grant number 81760276)
Author information
Authors and Affiliations
Contributions
Yingying Xie contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Pengli Luo, Haining Zhao, Meng Ma, Mengting Xu, and Qin Li. The first draft of the manuscript was written by Zhuojia Yang and Cenying He, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study contains no human participants or tissues. Ethical approval and informed consent are not applicable for this study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xie, Y., Zhao, H., Luo, P. et al. Downregulation of HIF-2α Enhances Apoptosis and Limits Invasion in Human Placental JEG-3 Trophoblast Cells. Reprod. Sci. 28, 2710–2717 (2021). https://doi.org/10.1007/s43032-021-00581-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00581-8