Abstract
End-stage hip joint degeneration in the paediatric population is uncommon. Traditionally, arthroplasty has had limited use in this population, owing to fears about wear and early multiple revisions. Advances in implant and bearing surface design, alongside improved surgical technique, are making total hip arthroplasty (THA) in the paediatric population a more viable option. A systematic review of THA in the paediatric population using conventional literature databases and grey literature was undertaken from January 1988 until December 2020 to determine the functional, clinical and radiological outcomes of THA in patients under 18 years old. One hundred and eighty-six studies were initially eligible from the inclusion criteria. Upon screening the papers, ten papers met the inclusion criteria and were included in the review. Heterogeneous data was acquired; therefore, no meta-analysis was performed. Overall implant survival was 96% at 5 years and equivalent to THA in adults. Functional and pain scores were significantly improved at 6 weeks, 6 months and 1-year post-operative follow-up. Complication rate was 3%. Dislocation rate was lower than adult THA at 0.4%. THA is a well-proven treatment in adults. However, this review of the literature demonstrates that THA in the paediatric population has good survival rates, with low dislocation, infection and complication rates. THA can confer significant improvements in pain and function and should be considered as a feasible option for management of end-stage degenerative disease. A prospective controlled trial is required to fully confirm and quantify this further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative hip disease in children can arise following infection, trauma and paediatric hip pathology including developmental dysplasia of the hip (DDH), Perthes disease and slipped capital femoral epiphysis (SCFE) [1,2,3]. Although improvements in national and international screening programmes have reduced the incidence of severe disease, certain factors such as health care accessibility, anatomical variability, low community awareness and initial normal radiographical imaging still result in late presentation associated with more severe pain and deformity [4, 5].
End-stage degenerative hip disease is uncommon in the paediatric population. When it does occur, it can be difficult to treat, with long-term effects on function and often necessitates multiple and potentially complex interventions. Management of this condition was traditionally conservative, with analgesia and protected weight-bearing aiming to delay inevitable joint replacement surgery until middle age [6].
Surgical management options for degenerative joint disease in children include arthroscopy and bone conserving osteotomies. These procedures aim to improve hip morphology, kinematics and stability. Osteotomies of the pelvis or acetabulum typically remove bone from one area to redirect forces through another. While they can be highly effective in delaying the degenerative process, they do not retain the native anatomy and may increase the complexity of any future arthroplasty surgery [7]. Arthroscopy has also been suggested to manage femoroacetabular impingement (FAI) and delay the onset of juvenile degenerative joint disease [8, 9]. The effectiveness of arthroscopy is more limited in those patients whose disease is end stage at presentation. In these patients, options become limited.
After cataract surgery, total hip arthroplasty (THA) is recognised to be the most effective intervention ever established. It is the most commonly performed orthopaedic operation in the United Kingdom (UK), with more than 600,000 performed annually and has a 95% patient satisfaction [10, 11]. Its use in paediatric patients is less popular, owing to higher risk of multiple revision surgery, given the longer time periods in use and the higher functional demands of younger people [12].
Improvements in implant design, bearing surfaces and surgical technique in THA may offer reduced wear and increased implant longevity [13]. Prostheses are now increasingly bone conserving, providing more real estate for potential revisions [14]. Developments in polyethylene processing have reduced wear rates significantly, which mitigate against aseptic loosening, recognised as the main indication for revision surgery in children [15]. Minimally invasive techniques for implantation have been developed, which reduce the physiological and anatomical impact of surgery early in life [16].
Taking into consideration these developments, a systematic review of the current literature was performed to establish the outcomes of THA in the paediatric population and re-consider its role in managing end-stage hip degeneration.
Aim
The primary aim of this review is to establish the functional and radiological outcomes following THA in patients under the age of 18. The secondary aims include the assessment of the nature and frequency of complications occurring, the effect of bearing surface and the effect of the approach used.
Methods
Search Strategy
The reviewers performed a PRISMA compliant search of the electronic databases Embase, MEDLINE, Cochrane, PubMed and CINAHL using the Ovid platform between January 1988 and December 2020. Google Scholar was also utilised. Grey literature was searched using OpenGrey, EThOS, ProQuest and OpenDOAR. The Cochrane database was searched, and no similar systematic reviews were identified.
The search terms adopted included (“Paediatrics” OR “pediatrics” OR “paediatric” OR “pediatric”) AND (“arthroplasty, replacement, hip”) OR (“arthroplasty” OR “replacement” AND “hip”) OR “hip replacement arthroplasty” OR (“total” AND “hip” AND “replacement”) OR “total hip replacement”.
Eligibility Criteria
All papers with a study population mean age of 18 or younger were eligible. Given this is not a commonly performed procedure, case reports were included to increase the amount of eligible data analysed.
Study Selection
Studies identified by the electronic search were screened initially by title to exclude any adult arthroplasty papers or those that did not answer the research question. After initial screening, the remaining abstracts were scrutinised, and any further exclusions were made due to irrelevance to the primary research question. Full-text articles of the remaining studies were assessed, and one final exclusion was made. The remaining articles were included in the systematic review. Articles were assessed by two independent reviewers (GG, GS), and any differences in article inclusion were discussed with the senior author (SR) and resolved by consensus. Reference lists of included articles were also scrutinised for any eligible papers.
Data Collection Process
Outcome measures in the studies identified were validated, but not homogenous. Data were collected in an Excel spreadsheet. The number of patients, duration of follow-up, functional and radiological outcome measures used in each study and their results were identified. Furthermore, any complications or other relevant clinical observations made were identified and included.
Risk of Bias
The data collected is heterogeneous in nature. Registry data were included; we acknowledge that this carries a risk of selection and reporting bias as well as potential discrepancies between statistically significant and clinically significant differences. Many of the studies included are of low evidence level (case reports and small series), and these are likely to show reporting bias and publication bias.
Results
Study Selection
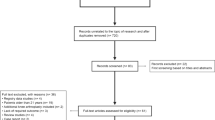
Using the search criteria described, 186 studies were identified. Following initial screening, 164 studies were excluded on the basis that they were concerning adult patients or were irrelevant to the research question. Of the remaining 22 abstracts screened, 12 were excluded (over 18 year old subjects, topic review without relevance to systematic review). Ten full-text articles were evaluated, with one excluded as a general topic review. The nine remaining studies were included in the final review. However, a further article was identified on reviewing the references, resulting in ten papers for inclusion (Fig. 1, PRISMA flow diagram).
Study Characteristics and Results of Individual Studies
The ten studies included in the review have been broadly split into three groups according to their data type: registry data evaluation, case series and case reports. Three studies involve evaluation of large registry datasets, five were case series and two were single patient case studies. Summaries of the papers can be seen in Table 1.
Registry Data Evaluation
The studies were designed to interpret the UK, Australian and Nordic Joint Registry Databases [17,18,19]. The primary aim of all three studies was to ascertain the rate of revision and implant survival. There were no functional or radiological outcome measures used. The three papers included a total of 1747 patients and 1947 THAs. The follow-up time and mean age were comparable, as were the indications for surgery (Table 2). Predominantly these were paediatric hip disorders (SCFE, Perthes, DDH), inflammatory disease and osteoarthritis. Implant survival at 10 years was assessed in the Nordic study and 5 years in the Australian and UK studies. At 5 years, there was mean 95.7% survival, and at 10 years, this was 86%.
Sedrakyan et al. [17] stratified survival by age group and demonstrated higher revision rates in the paediatric population (10% vs. 5% at 5 years). The authors identified that THA performed in the setting of differing and unique paediatric pathology may contribute to this difference.
Havorsen et al. [18] evaluated data in order to ascertain whether there is a difference between cemented and uncemented implants. Seventy-five percent of the THA performed in this registry study were uncemented, with the choice of fixation not affected by surgical indication. The primary outcome identified was revision for any reason at 10 years, and a survivorship of 86% at 10 years was ascertained. With regards to revision rate, it was reported that cups were more commonly revised than stems, but there was no statistically significant difference between cemented and uncemented implants.
Metcalfe et al. [19] scrutinised the UK National Joint Registry (NJR). Again, the primary outcome was the time to first revision, but secondary outcome was to determine any effect of bearing surface on revision rate. The survivorship at 5 years was found to be 96%. Metal on polyethylene (MoP) and metal on metal (MoM) bearings were associated with significantly higher revision rates than ceramic on ceramic (CoC) and ceramic on polyethylene (CoP) bearings.
Case Series
Four papers present data for 212 patients with 261 THAs. The mean age of patients included was 16 [6, 12, 20,21,22].
Indications varied between centres and case series, as shown in Table 3. Van de Velde et al. [22], Luceri et al. [6], Buddhev et al. [12] and Hannouche et al. [21] report predominantly paediatric hip conditions as the surgical indication. Daurka et al. [20] undertook THA purely for inflammatory disease (including rheumatoid arthritis and systemic lupus erythematosus).
A comparison of the surgical techniques used in the five case series are summarised in Table 4. All authors used uncemented implants, therefore, providing no comparison with cemented implants as seen in the registry data. Four out of the five studies used ceramic femoral heads and a combination of polyethylene or ceramic acetabular liners, with only Van de Velde et al., reporting the use of metal femoral heads. In terms of the approach used in each study, the majority of procedures were undertaken through a posterior approach or a modified Hardinge approach.
Functional outcome scores were reported in all five case series but data was heterogeneous. Two studies used the Merle d’Aubigné-Postel score [21, 22], two studies used the Harris Hip Score [6, 20] and one study used the Oxford Hip Score [12]. These scores have all been externally validated in the literature. Time points in each study were similar at 6 weeks, 6 months and 1 year. Regardless of which scoring stem was used, all studies reported significant increases in functional score at all time points post-operatively.
Two papers were assessed for evidence of radiological loosening at follow-up [21, 22]. Van de Velde et al. reported no incidence of loosening on follow-up imaging, whereas Hannouche et al. determined that there was radiological loosening in 16/91 (17.5%) cases.
Van de Velde et al., Buddhev et al., and Daurka et al. assessed pain scores at follow-up. All three studies reported significant improvements [12, 20, 22].
Four of the five studies reported post-operative complications. Luceri et al. reported 3 out of 10 complications: a transient femoral nerve palsy in an anterior approach patient and two dislocations in the posterior approach group [6]. Buddhev et al. reported two of 60 complications, both aseptic loosening requiring revision [12]. Daurka et al. reported a single case of foot drop, which resolved spontaneously [20]. Hannouche et al. reported two complications out of their 113 cases: a haematoma which required no intervention and a partial subluxation in a Marfan’s patient [21].
Case Reports
Two case reports were included in the review. Blake et al. reported the outcomes for staged bilateral THA in cerebral palsy [23]. They reported that at the last follow-up (18 years post-operatively), the patients’ sitting posture remained preserved, and they were pain free.
Ulici et al. (2016) reported the outcome of THA performed for developmental dysplasia of the hip in a 14-year-old girl. They reported excellent post-operative progress, even in the immediate post-operative phase, with rapid return to function and no pain. The patient was reported to have a 2-cm residual leg length discrepancy [24].
These registry data evaluation studies, case series and case reports demonstrate that THA in the paediatric population may provide benefits even in complex or poorly ambulatory patients as a pain relieving procedure.
Discussion
Fortunately, end-stage degenerative hip disease is relatively uncommon in the paediatric population. However, delays to diagnosis and late presentations with severe paediatric hip conditions still occur and present the surgeon with a complex management dilemma [1,2,3, 25].
Traditionally THA has been reserved as an operation for middle and older age patients. However, in the past, early implant designs and bearing surfaces have conferred a finite duration of use, leading to concerns for early and multiple revision operations if performed in younger patients. Early implants were large and bulky and therefore are associated with more bone loss at the first revision, making this more complex [13,14,15, 25]. Improvements in bearing surfaces with advances in polyethylene production provide lower wear profiles and longer potential duration of use. Newer implant designs are also more bone conserving and, therefore, facilitate more straightforward revision options as necessary [14].
The National Joint Registry (NJR) was established in order to document and monitor arthroplasty, in terms of indication for the primary procedure, implant survival, revision rate and indication for revision. In patients over 55, the NJR suggests an average 10-year survival rate of 94% [26]. At present, the NJR do not report the use of arthroplasty in patients under the age of 18 [26].
The current evidence for use of THA in patients aged under 18 is limited and heterogeneous. Due to the low number of operations performed in this patient population, most papers published reviewing functional, radiological and pain-related outcomes are level four evidence case series. Larger papers, such as those of Sedrakyan et al., Havorsen et al. and Metcalfe et al., present registry data [17,18,19]. The primary outcome of registry data evaluation is to identify the revision rate and the indication for revision. Registry and big data depend on the quality of the collected data at the individual surgeon level and can often miss key information, if not collected or entered [27]. Despite these limitations, the registry data from three large registries (the UK, Nordic and Australian) demonstrate implant survival in paediatric patients of 96% at 5 years and 86% at 10 years. These are young, active patients, who place much higher demands on their implants. Given this consideration, the implant survival is excellent [17,18,19].
Case series aiming to establish clinical outcomes demonstrate good pain relief and return to mobility, equivalent to those used in adults. However, the numbers of cases are much lower and would require a prospective controlled trial in order to fully confirm if results in the paediatric population are equivalent to those in the adult population [6, 12, 20,21,22]. Indications for surgery in patients under 18 are different to those in adults; most were performed for consequences of paediatric hip disease or idiopathic osteonecrosis, compared with primary osteoarthritis in the adult group. This could affect overall implant longevity. Also, the case reports included involved patients who have more complex systemic conditions, which may limit the functional outcomes reported [23, 24].
The current literature shows a complication rate of less than 3%, with complications varying from transient nerve palsies to aseptic loosening [6, 12, 17,18,19,20,21,22,23,24]. Dislocation in paediatric literature appears to be less of a concern than in adults with a rate of 0.4% (compared with 1–3% primary THA in adults and 4–6% after the neck of femur fracture) in the case series and less than 1% in registry papers [28]. This is despite the use of varied approaches (lateral, posterior and anterior) which are well recognised to affect this risk in adults [29].
Prosthetic joint infection (PJI) rates in this study are around 2% (44/ 2187 patients); this is higher than the adult literature, which quotes PJI of 0.7 to 1.24%. However, our figure relies on the results of a single joint registry (Nordic) and may overestimate the true incidence [30, 31].
Limitations
This systematic review was designed to have strict inclusion criteria, however, to make the findings more generalisable, the data obtained were heterogeneous and of low evidence. We also acknowledge the small numbers of these procedures performed and included in the review.
Conclusion
End-stage degenerative hip joint disease is an uncommon presentation in the paediatric population, and while it has a significant effect on quality of life, there are only limited options to surgeons for management [1,2,3]. Traditionally non-operative, pain relieving measures were employed in order to postpone surgery until skeletal maturity or such time as arthroplasty could be considered. Over time, temporising measures have been performed to improve patient comfort and satisfaction [8, 9, 32].
THA a highly effective surgical intervention yet is conventionally reserved for middle and older aged patients with osteoarthritis, with fears over multiple revisions and poor outcome in children [25].
In conclusion, with a survival rate demonstrated at 96% at 5 years and 86% at 10 years, as well as significant improvements in function and pain; we suggest that arthroplasty is a feasible option in the paediatric population Additionally, the rate of complications is comparable to that in adults, and dislocation rate is considerably lower.
Research into this field is relatively new and will continue to define our understanding of the role of THA in the paediatric population. More research in the form a prospective randomised controlled trial looking specifically at clinical outcome measures as well as indication and revision rates would be indicated to confirm these findings further.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code Availability
Code availability was not applicable as this manuscript is a systematic review.
References
Solomon L. Patterns of osteoarthritis of the hip. Bone Joint J. 1976;58-B(2):176–83.
Yagdiran A, Zarghooni K, Semler JO, Eysel P. Hip pain in children. Dtsch Arztebl Int. 2020;117(5):72–82.
Rutz E, Spoerri M. Septic arthritis of the paediatric hip - a review of current diagnostic approaches and therapeutic concepts. Acta Orthop Belg. 2013;79(2):123–34 (infection).
Lowry CA, Donoghue VB. Murphy JFAuditing hip ultrasound screening of infants at increased risk of developmental dysplasia of the hip. Arch Dis Child. 2005;90:579–81.
Lindberg AW, Bompadre V, Satchell EK, Larson ACR, White KK. Patient factors associated with delayed diagnosis of developmental dysplasia of the hip. J Child Orthop. 2017;11(3):223–8.
Luceri F, Morelli I, Sinicato CM, et al. Medium-term outcomes of total hip arthroplasty in juvenile patients. J Orthop Surg Res. 2020;15:476. https://doi.org/10.1186/s13018-020-01990-2.
Gillingham BL, Sanchez AA, Wenger DR. Pelvic osteotomies for the treatment of hip dysplasia in children and young adults. J Am Acad Orthop Surg. 1999;7(5):325–37.
Jayakumar P, Ramachandran M, Youm T, Achan P. Arthroscopy of the hip for paediatric and adolescent disorders: current concepts. J Bone Joint Surg Br. 2012;94-B(3):290–6.
Abu Amara S, Leroux J, Lechevallier J. Surgery for slipped capital femoral epiphysis in adolescents. Orthop Traumatol Surg Res. 2014;100(1 Suppl):S157–67.
Crawford RW. Murray, DW Total hip replacement: indications for surgery and risk factors for failure. Ann Rheum Dis. 1997;56:455–7.
Okafor L, Chen AF. Patient satisfaction and total hip arthroplasty: a review. Arthroplasty. 2019;1:6. https://doi.org/10.1186/s42836-019-0007-3.
Buddhdev PK, Vanhegan IS, Khan T, Hashemi-Nejad A. Early to medium-term outcomes of uncemented ceramic-bearing total hip arthroplasty in teenagers for paediatric hip conditions. Bone Joint J. 2020;102-B(11):1491–6.
Zagra L, Gallazzi E. Bearing surfaces in primary total hip arthroplasty. EFORT Open Rev. 2018;3(5):217. https://doi.org/10.1302/2058-5241.3.180300.
Ahmad R, Kerr HL, Spencer RF (2018) Bone conserving mini hip replacement. Orthopaedic Proceedings 94-B(SUPP_XLII)
Gómez-Barrena E, Medel F, Puértolas JA. Polyethylene oxidation in total hip arthroplasty: evolution and new advances. Open Orthop J. 2009;3:115–20. https://doi.org/10.2174/1874325000903010115 (Published 2009 Dec 24).
Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. (2004) Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res (1976-2007). 2004;December 2004(429):239–47.
Sedrakyan A, Romero L, Graves S, Davidson D, de Steiger RN, Lewis PL, Solomon M, Vial R, Lorimer M. Survivorship of hip and knee implants in pediatric and young adult populations. J Bone Joint Surg-Am. 2014;96(Suppl. 1(E)):73–8.
Halvorsen V, Fenstad AM, Engesæter LB, et al. Outcome of 881 total hip arthroplasties in 747 patients 21 years or younger: data from the Nordic Arthroplasty Register Association (NARA) 1995–2016. Acta Orthop. 2019;90(4):331–7.
Metcalfe D, Peterson N, Wilkinson JM, Perry DC. Temporal trends and survivorship of total hip arthroplasty in very young patients: a study using the National Joint Registry data set. Bone Joint J. 2018;100-B(10):1320–9.
Daurka JS, Malik AK, Robin DA, Witt JD. The results of uncemented total hip replacement in children with juvenile idiopathic arthritis at ten years. J Bone Joint Surg Br. 2012;94(12):1618–24.
Hannouche D, Devriese F, Delambre J, et al. Ceramic-on-ceramic THA implants in patients younger than 20 years. Clin Orthop Relat Res. 2016;474(2):520–7.
Van de Velde SK, Loh B, Donnen L. Total hip arthroplasty in patients 16 years of age or younger. J Children’s Orthop. 2017;11(6):428–33.
Blake SM, Kitson J, Howell JR, Gie GA, Cox PJ. Constrained total hip arthroplasty in a paediatric patient with cerebral palsy and painful dislocation of the hip. A case report. J Bone Joint Surg Br. 2006;88(5):655–7.
Ulici A, Dulea AM, Tevanov I, Sterian G, Balanescu R. Total hip replacement in congenital hip dislocation in 14 years female patient. Chirurgia (Bucur). 2016;111(3):279–82.
Learmouth ID, Heywood AW, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. Bone Joint J. 1989;71-B(2):209–12.
NJR Annual Report (2020) Executive Summary. Found at: https://reports.njrcentre.org.uk/AR-Executive-Summary (last acessed 27/12/2020 at 13:36)
Williams WG. Uses and limitations of registry and academic databases. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2010;13(1):66–70.
Dargel J, Oppermann J, Brüggemann GP, Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int. 2014;111(51–52):884–90.
Lu Y, Xiao H, Xue F. Causes of and treatment options for dislocation following total hip arthroplasty. Exp Ther Med. 2019;18(3):1715–22.
Kosola J, Huotari K, Helkamaa T. Prosthetic joint infections after hip fractures. Orthop Proc 100-B(SUPP_17)
Akgün D, Müller M, Perka C, Winkler T. High cure rate of periprosthetic hip joint infection with multidisciplinary team approach using standardized two-stage exchange. J Orthop Surg Res. 2019;14(1):78.
Karlen JW, Skaggs DL, Ramachandran M, Kay RM. The Dega osteotomy: a versatile osteotomy in the treatment of developmental and neuromuscular hip pathology. J Pediatr Orthop. 2009;29(7):676–82.
Author information
Authors and Affiliations
Contributions
Gemma Green: concept, Data analysis, wrote manuscript, and edited manuscript.
Golnoush Seyedzenouzi: Data analysis and wrote manuscript.
James Houston: Data analysis and wrote manuscript.
Irrum Afzal: Wrote manuscript, edited manuscript.
Sarkhell Radha: Concept, data analysis, wrote manuscript, and edited manuscript.
Corresponding author
Ethics declarations
Ethics
This is a review article and Research Ethics Committee has confirmed that no ethical approval is required.
Consent to Participate
Consent to participate was not applicable as this manuscript is a systematic review.
Consent for Publication
Consent to publication was not applicable as this manuscript is a systematic review.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery.
Level of Evidence: Level II.
Rights and permissions
About this article
Cite this article
Green, G., Seyedzenouzi, G., Houston, J. et al. Total Hip Arthroplasty in the Paediatric Population—A Systematic Review of Current Outcomes. SN Compr. Clin. Med. 5, 26 (2023). https://doi.org/10.1007/s42399-022-01324-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01324-9