Abstract
The aim of this work was to study the prevalence of hypocalcemia in cancer patients based on ionized calcium and, as a secondary aim, the influence that hypocalcemia may have on survival. For this retrospective study, a representative sample of all the records of low and normal ionized calcium measured in 2014 was studied. Patients under 18 years and patients from the bone marrow transplantation service were excluded. The number of patients included in this study was 471. The median patient age was 63 years (18 to 91), and 247 (52%) were female. The most represented cancers were thyroid, colorectal, and breast. Ionized calcium was in the normal range in 331 (70%) patients and low in 140 (30%). In a univariable analysis, there were no significant differences in survival at 4 years between normal (47%) and low-level (42%) ionized calcium (p = 0.192), but there were differences in gender, age, the primary site, the number of metastatic sites, and the level of albumin. In the multivariable analysis, only the primary cancer, the number of metastatic sites, and the albumin levels were associated with survival. In a multivariable analysis excluding thyroid cancer, hypocalcemia remained not associated with survival. Hypocalcemia occurs in a variety of cancer types, and it does not have an influence on survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of hypocalcemia in cancer patients is a topic which is not often addressed in the medical literature, unlike hypercalcemia. Most data on hypocalcemia in cancer comes from case reports, case series, or reviews of specific syndromes involving hypocalcemia [1]. We found only 3 articles on the prevalence of hypocalcemia in cancer patients; 2 of them were published in 1986 [2] and 1991 [3]; the third was carried out by the lead author of this article and was published in 2019 [4].
In the last article, hypocalcemia measured by the total calcium corrected for serum albumin was not a negative prognostic factor. Other factors, such as age, primary cancer, and serum albumin were significantly associated with survival, but corrected calcium was not. However, the correction of total calcium for serum albumin is not a very accurate method for determining the level of calcium. Particularly, in some clinical situations, such as patients receiving transfusions with citrated blood, in critically ill patients, in late stages of chronic kidney disease, in hyperparathyroidism, and in hypercalcemia of malignancy, the direct measurement of ionized calcium is clearly more accurate than the total calcium corrected for the albumin level [5]. For example, in a study carried out in a surgical intensive care unit, the sensitivity and specificity of the corrected serum calcium for evaluating hypocalcemia were 53% and 85%, respectively; corrected calcium underestimated the prevalence of hypocalcemia and overestimated the prevalence of normocalcemia, and no factors were able to distinguish which patients could be evaluated by corrected calcium levels [6]. Another study, carried out on adult patients admitted to a trauma intensive care unit who received specialized nutrition support, also concluded that predictive methods for estimating ionized or corrected serum concentrations should not be used. Therefore, direct measurement of serum ionized calcium concentration is indicated for assessing calcium status for this population [7].
Thus, the preferred method for assessing the calcium level is ionized calcium, as it is not influenced by the albumin level and it is the functioning part of calcium.
However, the direct measurement of ionized calcium is costly and technically challenging, but especially in patients with complex illnesses, it is a more accurate method relative to the corrected total calcium level. Our previous study was based on the level of calcium corrected for albumin. This time, we tried to confirm, or not, the results obtained with this study based on ionized calcium.
Methods
This study was carried out in a comprehensive oncology center. The primary aim of this study was the prevalence of hypocalcemia in cancer patients. The secondary aim was to study the possible influence of hypocalcemia on survival. For this retrospective study, a representative sample of the patients with all the records of ionized calcium measured in 2014 was used, excluding patients under 18 years and patients in the bone marrow transplantation service. Patients in this service were excluded because they constitute a special group of patients who undergo particularly aggressive treatments and therefore are not comparable with other patients.
The sample included 471 patients, roughly one-third, randomly selected. This sample was representative of the full cohort since there were no significant differences in the mean of ages (p = 0.963), gender (p = 0.312), primary cancer (p = 0.058), or mean calcium level (p = 0.054).
For the secondary aim of this study, survival of patients with hypocalcemia was compared with patients with normal calcium levels; patients with hypercalcemia were excluded. When more than one measurement was available, as frequently occurred, the first one was chosen.
The factors included for analysis in this study were the same as in the previous one (age, gender, primary site, metastases, serum calcium level, and serum albumin), except for the addition of the number of metastatic sites.
To verify if the prevalence of hypocalcemia in the sample studied was similarly distributed among all types of cancer, a comparison with the mean of cancer diagnoses made in 2013 and 2014 was made.
Descriptive statistics methods were used for analyzing the data. To evaluate the existence or not of associations between variables, the chi-squared test was used. Survival curves were calculated using the Kaplan–Meier estimator and compared using the log-rank test. For multivariable analysis, Cox regression was used. The level of significance was deemed to be 0.05. Data were analyzed using the software IBM SPSS version 26.
This study was approved by the ethics committee of the hospital.
Results
The median patient age was 63 years (18 to 91) and 247 (52%) were female. The most represented cancers were: thyroid—90 (19%), colorectal—71 (15%), and breast—60 (13%), and the most frequent metastasized sites were lymph nodes and bone (Table 1).
Compared with the mean number of the diagnoses of patients admitted in 2013 and 2014, the proportion of cases of hypocalcemia was significantly higher in patients with thyroid cancer and significantly lower in patients with breast and prostate cancers (Table 2).
Several drugs are associated with hypocalcemia. In this study, patients taking two or more of such drugs had more frequently hypocalcemia than patients taking one or none (p = 0.016). The most frequently used drugs, which may lower the calcium level were proton pump inhibitors—192 (41%) and corticosteroids—93 (20%). Patients on bisphosphonates, 29 (6%), were not more likely to have hypocalcemia than the other patients (p = 0.873). Denosumab was not used in any patient.
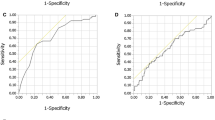
Ionized calcium was in the normal range in 331 (70%) patients and low in 140 (30%). The overall 4-year survival rate was 46%. In a univariable analysis, there were no significant differences in survival at 4 years between normal (47%) and low-level (42%) ionized calcium (p = 0.192), even when calcium is divided in quartiles (p = 0.050), but there were differences in gender, with 36% of males alive vs. 55% of females (p < 0.001), in age with 58% of under 64 s alive vs. 33% of older patients (p < 0.001), in the primary site (p < 0.001), number of metastatic sites with lower survival related with the increase in that number (p < 0.001), and the level of albumin, with lower survival associated with lower levels of albumin (p < 0.001). In the multivariable analysis only the primary cancer, the number of metastatic sites and the albumin levels were associated with survival (Table 3).
As the percentage of thyroid neoplasm was relatively high and hypocalcemia related to them may result from surgery and not from advanced cancer, an analysis excluding thyroid neoplasms was performed. In the multivariable analysis, the level of calcium remained without prognostic value. The main difference was the exclusion of the primary cancer as a significant factor, remaining the number of metastatic sites and the albumin levels associated with survival (Table 4).
Discussion
Hypocalcemia is a frequent occurrence in many diseases and in many settings, particularly cancer. In our previous study, the median age was the same (63 years) with a similar range (18 to 93). There was a small difference between genders, and there was also a bigger difference in the primary sites. However, the lack of influence of low serum calcium on survival was confirmed [4]. That observation was also made in one of the older studies [2].
Age did not influence survival as it did in the previous study. Concerning the primary sites, the composition of the sample was different from the former one, and the selection of patients was different. The former study was based on total low calcium level, and the present study was based on all patients with an ionized calcium measured in 2014 with normal or low calcium. These results are also different from the results of older studies on hypocalcemia [2, 3], making the studies hard to compare.
Concerning the mean number of diagnoses made in 2013 and 2014 [4], patients with thyroid cancer had a significantly higher incidence of hypocalcemia relative to the patients admitted with that cancer type, whereas breast and prostate cancers had a lower incidence. This finding was also observed in the former study. Differences between the two studies were seen in lung cancer, which was marginally significantly lower in the previous study, but not in the current one, and hematological cancer, which was significantly higher in the previous study but not in this one.
The association of thyroid cancer with hypocalcemia is well-known, due to postsurgical hypoparathyroidism [8], and not necessarily to advanced disease. In fact, in the analysis excluding thyroid cancer, the primary site has no longer influence on survival, what seems to support that fact. Hypocalcemia is also associated with prostate cancer, which often metastasizes to bone, usually as osteoblastic metastases that cause increased deposition of calcium and phosphate in bone, tending to decrease the serum concentrations [9]. This may be aggravated by treatment with bisphosphonates or denosumab [1]. However, in the patients studied, we observed that the percentage of patients with prostate cancer is significantly lower than the population of patients diagnosed in 2013 and 2014. Breast cancer is more frequently associated with hypercalcemia [10] and therefore, naturally, is not often associated with hypocalcemia.
The prevalence of hypocalcemia in cancer patients is unknown, but it seems not to be rare. Even the few studies carried out so far, including this study, cannot shed light on this point because it would be necessary to systematically assess serum calcium in oncology patients to reach a conclusion on the prevalence of hypocalcemia in these patients.
Hypocalcemia in cancer patients may have several mechanisms. Mild transient hypocalcemia may be due to multiple transfusions, as ionized calcium binds to citrate. Hypocalcemia may be caused by tumor lysis syndrome due to acute hyperphosphatemia; deficiency of parathyroid hormone due to surgery for thyroid or laryngeal cancer or neck radiotherapy; magnesium depletion due to chemotherapy or antibiotics; malabsorption due, for example, to surgery or radiotherapy involving the bowel; osteoblastic metastases which uptake calcium and may cause hungry bone syndrome; acute or chronic renal failure; and patients in critically ill situations, such as overwhelming infection. There are other possible causes, and hypocalcemia is often multifactorial [1]. Hypocalcemia may be false, due to hypoalbuminemia or recent MRI with gadolinium, which cause interference with assay [1]. However, ionized calcium is not affected by hypoalbuminemia.
Hypocalcemia in cancer patients is usually mild and asymptomatic [11]. There are, however, some cases of severe and heavily symptomatic hypocalcemia, but in the few studies carried out on this topic, hypocalcemia seems to have no influence on survival, at least in most cases.
Conclusion
Hypocalcemia seems not to be a rare occurrence in cancer patients. However, the data suggests that it does not influence survival, as the few studies on this topic have shown.
Data Availability
Data are available from the correspondent author if requested.
Code Availability
IBM SPSS version 26.
References
Schattner A, Dubin I, Huber R, et al. Hypocalcaemia of malignancy. Neth J Med. 2016;74:231–9.
Blomqvist CP. A hospital survey of hypocalcemia in patients with malignant disease. Acta Med Scand. 1986;220:167–73.
D’Erasmo E, Acca M, Celi FS, et al. A hospital survey of hypocalcemia and hyperphosphatemia in malignancy. Tumori. 1991;77:311–4.
Ferraz Gonçalves JA, Costa T, Rema J, et al. Hypocalcemia in cancer patients: an exploratory study. Porto Biomed J. 2019;4:e45.
Calvi LM, Bushinsky DA. When Is It Appropriate to order an ionized calcium? J Am Soc Nephrol. 2008;19:1257–60.
Byrnes MC, Huynh K, Helmer SD, Stevens C, Dort JM, Smith RS. A comparison of corrected serum calcium levels to ionized calcium levels among critically ill surgical patients. Am J Surg. 2005;189:310–4.
Dickerson RN, Alexander KH, Minard G, et al. Accuracy of methods to estimate ionized and “corrected” serum calcium concentrations in critically ill multiple trauma patients receiving specialized nutrition support. J Parenter Enteral Nutr. 2004;28:133–41.
Iglesias P, Díez JJ. Endocrine complications of surgical treatment of thyroid cancer: an update. Exp Clin Endocrinol Diabetes. 2017;125:497–505.
Murray RML, Grill V, Crinis N, Ho PWM, Davison J, Pitt P. Hypocalcemic and normocalcemic hyperparathyroidism in patients with advanced prostatic cancer. J Clin Endocrinol Metab. 2001;86:4133–8.
Riancho JA, Arjona R, Valle R, et al. The clinical spectrum of hypocalcaemia associated with bone metastases. J Intern Med. 1989;226:449–52.
Kassi E, Kapsali I, Kokkinos M, Gogas H. Treatment of severe hypocalcaemia due to osteoblastic metastases in a patient with post thyroidectomy hypoparathyroidism with 153Sm-EDTMP. BMJ Case Reports May 2017, 2017 bcr-2017–219354.
Funding
This work was supported in part by the North Section of the Portuguese League against Cancer.
Author information
Authors and Affiliations
Contributions
Corresponding author: idea, initial conception, first draft of the protocol, first draft of the manuscript and final approval of the manuscript. All other authors: review of the different versions and final approval of the protocol, data collection, review of the different versions, and final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Approved by the Ethics Committee meeting on 09 November 2017, Ref. 327/2017.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Ferraz-Gonçalves, J.A., Monteiro, A.R., Patrão, A.S. et al. Hypocalcemia in Cancer Patients: a Study Based on Ionized Calcium. SN Compr. Clin. Med. 3, 2520–2524 (2021). https://doi.org/10.1007/s42399-021-01053-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-01053-5