Abstract
To evaluate the relationship between the actual maternal serum alpha-fetoprotein (MSAFP) levels and maternal, fetal, and neonatal outcomes in patients diagnosed with placental abruption. This prospective case-control study included 40 patients who presented at the Perinatology Department between December 15, 2018, and September 01, 2019, were diagnosed with placental abruption and underwent cesarean section delivery at ≥ 34 weeks, and 41 healthy individuals without any additional systemic pathologies, who had a cesarean section under elective conditions. The patient demographic data, MSAFP levels, and maternal, fetal, and neonatal results were compared. Correlation analyses were applied between the MSAFP levels and demographic characteristics, birthweight, Apgar scores, and transfusion requirement in the group with placental abruption. MSAFP levels (ng/ml) were significantly higher in the group with placental abruption than in the healthy control group (299.1 ± 214 and 156.2 ± 52.3, p = 0.012). In the neonatal results, birthweight and 1st and 5th minutes Apgar scores were lower in the group with placental abruption than in the control group (p = 0.025 and p < 0.001). The neonatal intensive care unit admission rate was higher in the group with placental abruption than in the healthy control group (p = 0.017 and p = 0.002). A statistically significant, negative correlation was found between MSAFP and 1st and 5th minutes Apgar scores (r = − 0.526, r = − 0.522 and p < 0.001, p = 0.001, respectively). The data obtained in this study suggest that MSAFP, which is a simple test, can be used in the clinical management of suspicious placental abruption or antepartum hemorrhage of unknown origin and the prediction of neonatal prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Placental abruption is defined as the complete or partial separation of the placenta from the area where it is implanted in the uterus as a result of bleeding into the decidua basalis. It is one of the most important causes of third-trimester bleeding and a serious complication of pregnancy-related maternal and perinatal mortality and morbidity [1]. The incidence is 2–10/1000 births [2]. Although the etiopathogenesis has not been fully clarified, predisposing risk factors have been defined. The most important risk factor is the history of placental abruption in a previous pregnancy, and other risk factors include advanced maternal age, pre-eclampsia, chronic hypertension, preterm early membrane rupture, chorioamnionitis, fetal growth restriction, multiple pregnancies, polyhydramnios, uterine anomalies, trauma, smoking, and cocaine use [3, 4]. It is clinically diagnosed after the 20th gestational week in general, and the clinical findings are vaginal bleeding, uterine tension, sensitivity, and painful tetanic contractions [5]. The diagnosis of placental abruption is mostly clinical [6]. The criteria for the diagnosis of placental abruption on ultrasonography (US) consist of observing intra-amniotic, subchorionic or marginal hematoma, increase in placenta thickness (> 5 cm) and heterogeneity, preplacental and retroplacental collections, and “jello-like” movements on the chorionic surface when the fetus moves [6]. In diagnosis, the sensitivity of US findings is 25–60%. However, more than 50% of placental abruption cases cannot be diagnosed sonographically, and, even if normal US findings are observed, the diagnosis of placental abruption cannot be excluded [7]. Therefore, clinical and sonographic evaluation can be insufficient for the diagnosis of placenta abruption, particularly in the early stage.
Alpha-fetoprotein (AFP) is the major glycoprotein in the fetal serum secreted by the fetal yolk sac and liver. From the early stage of pregnancy onwards, maternal serum AFP (MSAFP) levels increase, and serum screening has been optimized to distinguish the normal and abnormal MSAFP results during the 15–18-week period of the second trimester of pregnancy [8]. Unexplained elevated MSAFP levels in the second trimester have been associated with adverse pregnancy outcomes such as fetal growth restriction (FGR), pre-eclampsia, preterm labor, fetal demise, and stillbirth [9]. However, these data have been accessed via retrospective records. MSAFP levels at 20–24-week gestation are elevated in women who developed placental abruption later during the pregnancy [10]. Bartha et al. reported that elevated actual MSAFP levels in preterm labor cases can be used as a biomarker for the diagnosis of placental abruption in clinical practice [11]. Furthermore, Ngai et al. stated that when actual MSAFP levels exceed 280 μg/l in the third trimester, they have a predictive value with the specificity of 89% for placental abruption, and therefore, MSAFP can be used as a simple, cheap, and quick test for the clinical management of placental abruption [12]. There are few studies in the literature that have investigated the relationship between the actual MSAFP in the third trimester and placental abruption.
The aim of this study was to compare MSAFP levels between pregnant women with placental abruption and a healthy control group. The association of maternal, fetal, and neonatal outcomes with MSAFP was also investigated.
Materials and Methods
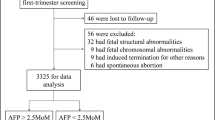
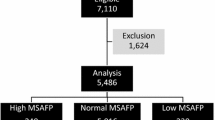
This prospective, case-control study was approved by the Ethics Committee of the University of Health Sciences, Zekai Tahir Burak Women’s Health Training and Research Hospital. Pregnant women who presented at the Department of Perinatology between December 15, 2018, and September 01, 2019, were included. The required data were collected after obtaining informed written consent from all participants. Power analysis was performed based on previous study results [11]. Target alpha (α) and 1-beta (β) error levels were taken as 0.05 and 0.95, respectively, and the minimum number of patients required to obtain 95% power in each group was calculated as 40 (total 80). G*Power 3.1.9.4 statistical software was used to perform these analyses [13]. The study included 40 patients who underwent cesarean section with the pre-diagnosis of ≥ 34-week placental abruption and 41 healthy individuals without any additional systemic pathologies, who had a cesarean section under elective conditions [14]. Multiple pregnancies and pregnant women with chromosomal and structural anomalies were excluded from the study.
The pre-diagnosis of placental abruption was established with clinical findings (vaginal bleeding, uterine sensitivity, and pain) and US findings (subchorionic or retroplacental hematoma, placenta heterogeneity, and increased thickness) [6]. Blood samples were taken from all the patients upon admission to the clinic for evaluating the MSAFP levels. It took 30 min for MSAFP results to become available approximately. Cesarean section was planned as the birth method for the patients. During the operation, the placenta was examined macroscopically. Placental abruption was confirmed upon observing retroplacental bleeding or clotting in the placenta. The percentage of abruption was recorded. The diagnosis of fetal growth restriction (FGR) was determined according to the international Delphi consensus [15, 16].
In this study, pregnant women with placental abruption and healthy control subjects were compared in terms of demographic characteristics, MSAFP levels, maternal, fetal, and neonatal outcomes. Maternal age, body mass index (BMI) (kg/m2), gestational age, gravidity, parity, living children, abortion, MSAFP level (ng/ml), birthweight, 1st and 5th minutes Apgar scores, neonatal intensive care unit (NICU) admission rate (n, %), and size of placental abruption (%) were compared between the groups. Correlation analyses were applied between the MSAFP levels and demographic characteristics, birthweight, APGAR scores, and transfusion requirement in the group with placental abruption. MSAFP was measured by enzyme immunoassay (ELISA) using the Enzymuntest AFP kit (Boehringer Mannheim).
Statistical Analysis
Data were analyzed using SPSS vn.20.0 statistical software. Conformity of the continuous variables to normal distribution was assessed using the Kolmogorov-Smirnov/Shapiro-Wilk tests. The Mann-Whitney U test was applied for non-parametric numerical data and Student’s t-test for parametric numerical data. To compare the categorical data, the Pearson chi-square (χ2) or Fisher’s χ2 tests were performed. The Pearson correlation test was applied to examine the relationships between the variables. A value of p < 0.05 was considered statistically significant.
Results
The comparisons of the demographic characteristics and MSAFP levels of the pregnant women with placental abruption and the healthy control group are presented in Table 1. Both groups were similar except for MSAFP levels (p > 0.05). The MSAFP levels (ng/ml) were statistically significantly higher in the group with placental abruption than in the healthy control group (299.1 ± 214 and 156.2 ± 52.3, respectively, p = 0.012). The comorbidity rates in pregnant women with placental abruption are shown in Table 2.
The comparisons of birthweights, Apgar scores, NICU admission rates (n, %), and size of abruption (%) of the pregnant women with placental abruption and the healthy control group are shown in Table 3. In the group with placental abruption, the 1st and 5th minutes Apgar scores were significantly low (p = 0.025 and p < 0.001, respectively), and the NICU admission rate (n, %) and percentage of placental abruption (%) were significantly high (p = 0.017, p = 0.002, p < 0.001, respectively).
In the group with placental abruption, the correlations of the MSAFP levels with demographic characteristics, birthweight, 1st and 5th minutes Apgar scores, and transfusion requirement are presented in Table 4. A statistically significant, negative correlation was found between MSAFP and the 1st and 5th minutes Apgar scores (r = − 0.526, r = − 0.522 and p < 0.001, p = 0.001, respectively). No other significant correlation was determined for the remaining parameters. Scatter plots of the 1st and 5th minutes APGAR scores and MSAFP levels are shown in Fig. 1.
Discussion
Placental abruption refers to the partial or complete separation of the placenta before the birth of the fetus. It is defined for pregnancies exceeding the 20th week. The main clinical findings are vaginal bleeding and abdominal pain, which are often accompanied by hypertonic uterus contractions, uterine sensitivity, and unreliable fetal heart rate [6]. However, there may be no symptoms observed in an early-stage or self-limited subacute and chronic abruption [11]. Cases complicated with disseminated intravascular coagulation (DIC), hypovolemic shock, blood transfusion, hysterectomy requirement, renal failure, unreliable fetal status, preterm labor, fetal growth restriction, maternal-fetal, and neonatal death are defined as severe abruption. Two-thirds of cases is classified as severe abruption [17]. Therefore, placental abruption is a significant cause of maternal, fetal, neonatal morbidity, and mortality [4]. In the diagnosis of placental abruption, US is useful, and retroplacental hematoma is a classical finding. Compared to the placenta, it might have a solid, complex, hyperechoic, or hypo-isoechoic (due to resolution rather than acute hematoma) appearance. However, the diagnostic sensitivity of US is approximately 25–60%. If US findings of placental abruption are seen in a symptomatic patient, the positive predictive value will be high (88%) [7]. Mild separation/hemostasis in hemorrhage tests is generally normal. In severe abruption, DIC may develop, and initial fibrinogen levels of ≤ 200 mg/dl indicate severe postpartum hemorrhage (positive predictive value = 100%) [18]. Furthermore, in severe abruption, the frequency of serious maternal complications has been stated to be 142/10,000 [17].
As previously mentioned, placental abruption is correlated with fetal-neonatal complications such as hypoxemia, asphyxia, low birthweight, preterm labor, and fetal growth restriction (with chronic abruption) [19, 20]. Preterm labor can be iatrogenic due to preterm pre-labor rupture of membranes (PPROM) or unreliable fetal/maternal status [6]. In a series of more than 500 placental abruptions that resulted in live birth, the birth rate between the 32nd and 36th weeks was reported to be 25.3%, and before the 32nd week, 14.3% [3]. In the current study, the preterm labor rate was 22.5%. Although the etiopathogenesis of placental abruption has not been fully clarified, multifactorial causes such as impaired placentation, placental insufficiency, oxidative stress, intrauterine hypoxia, thrombosis and necrosis in decidual veins, immunological reaction, and acute or chronic inflammation have been researched [21]. In the last decade, novel terms like “placenta mediated pregnancy complications” and “placental inflammation” have come to practice. In this concept, pathologies affecting the placental structures are considered to be the main etiological factors behind poor obstetric outcomes and pregnancy complications including miscarriage, intrauterine fetal demise, fetal growth restriction, preterm labor, pre-eclampsia, and placental abruption [22, 23].
Alpha-fetoprotein (AFP) is a plasma protein produced by the embryonic yolk sac and fetal liver. The AFP levels in serum, amniotic fluid, and urine are used as a screening test for congenital disabilities, where physical integrity is impaired, such as neural tube defects, omphalocele and gastroschisis, chromosomal anomalies, and some pathologies seen in adults (e.g., hepatocellular carcinoma, germ cell tumors, liver cirrhosis). In the prenatal period of embryonic development, the levels increase after the end of the first trimester and decrease after the 32nd gestational week. MSAFP is a parameter of the triple or quad fetal aneuploidy screening tests [9, 24]. MSAFP levels increase in placental pathologies such as chorioangioma and intervillous thrombosis [25, 26]. Moreover, elevated MSAFP levels have been reported to be possibly correlated with the impairment of the maternal-fetal-placental barrier and gestational complications [9].
Mid-trimester human gonadotropic (hCG), inhibin A, or MSAFP elevations have been reported to be correlated with obstetric complications such as intrauterine growth restriction (IUGR), pre-eclampsia, preterm labor, fetal loss, and stillbirth [27]. Elevated AFP levels (> 2 multiples of median = MoM) could determine 17% of subsequent placental abruptions [28]. The correlation of the levels of pregnancy-associated plasma protein-A (PAPP-A), which is a protease for the insulin-like growth factor binding protein-4, below the fifth centile in the first trimester with placental abruption has been reported [29]. Florio et al. found the mid-trimester levels of dimeric glycoprotein activin A secreted from placental trophoblasts to be higher in placental abruption cases [30]. In a study of 24 cases that developed gestational complications, Sharony et al. determined a statistically significant correlation between the MSAFP/AFAFP (AFP reservoir in the amniotic fluid) ratio, IUGR, and gestational week in the cases that underwent amniocentesis after MSAFP and therefore stated that the MSAFP/AFAFP ratio could be a predictor of gestational complications [9]. It can be seen in the literature that evaluations have been made more as a result of retrospective analyses, that is, on the parameters of the first- and second-trimester screening tests in the prediction of placental abruption.
The diagnosis of severe placental abruption is clinical and, usually easy to make, these women should be delivered as soon as possible before fetal distress or coagulation complications could develop. Precious time could therefore be waisted by waiting for the results of special investigations. However, in uncertain or suspicious cases, the use of MSAFP could be of value.
Bartha et al. evaluated the correlation of the actual MSAFP levels (in IU/ml and MoM) with placental abruption in 58 pregnant women who presented due to preterm labor between the 24th and 36th gestational weeks and reported that MSAFP levels (IU/ml) and MoM values (247.70 ± 88.82 [280.89], 1.97 ± 0.68 [2.08] MoM, p = 0.054, p = 0.033, respectively) were higher in 9 cases (15.5%) that developed placental abruption [11]. Similarly, Ngai et al. demonstrated that the actual MSAFP levels (μg/l) in the third trimester increased in pregnant women with placental abruption compared to a healthy control group (221 ± 139 and 128 ± 67, p < 0.01, respectively). It was also stated that when MSAFP levels exceeded 280 μg/l (= ng/ml), they had a predictive value with the specificity of 89% for placental abruption. Therefore, MSAFP could be used as a simple test for the clinical management of placental abruption, although the need for further, more extensive studies was also emphasized [12]. Consistent with both of the abovementioned studies, the MSAFP levels (ng/ml) were also higher in the group with placental abruption than the healthy control group in the current study (299.1 ± 214 and 156.2 ± 52.3, respectively, p = 0.012). Furthermore, a statistically significant negative correlation was determined between the elevated MSAFP levels and the 1st and 5th minutes Apgar scores (p < 0.001 and p = 0.001, respectively). The data obtained in this study support that MSAFP can be an auxiliary biomarker to be used in practice especially in suspicious, early-stage, subacute, or chronic placental abruption cases without typical clinical symptoms.
The strength of the present study was that it was the first such study to have a prospective design together with the evaluation of the third trimester and maternal-fetal and neonatal outcomes. However, the limitations could be said to be the lack of actual MSAFP MoM values, placental abruption was not confirmed pathologically, and the number of severe cases was low.
Conclusion
Placental abruption is one of the most important causes of the third-trimester bleeding and a serious complication of pregnancy-related maternal and perinatal mortality and morbidity. More than 50% of cases cannot be diagnosed with US, and even if normal US findings are observed, the diagnosis cannot be excluded. The usefulness of MSAFP in cases where the diagnosis of placental abruption is certain could be questioned but it may be of value in cases where the diagnosis is uncertain. The data obtained in this study support that MSAFP, which is a simple test, can be used as a biomarker in the clinical management of especially suspicious, early-stage, subacute, or chronic placental abruption cases without typical clinical symptoms and in the prediction of neonatal prognosis.
References
Ruiter L, Ravelli AC, de Graaf IM, Mol BW, Pajkrt E. Incidence and recurrence rate of placental abruption: a longitudinal linked national cohort study in the Netherlands. Am J Obstet Gynecol. 2015;213(4):573.e1-8.
Ananth CV, Keyes KM, Hamilton A, Gissler M, Wu C, Liu S, et al. An international contrast of rates of placental abruption: an age-period-cohort analysis. PLoS One. 2015;10(5):e0125246.
Tikkanen M. Placental abruption: epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand. 2011;90(2):140–9.
Anderson E, Raja EA, Shetty A, Gissler M, Gatt M, Bhattacharya S, et al. Changing risk factors for placental abruption: a case crossover study using routinely collected data from Finland. Malta and Aberdeen. PLoS One. 2020;15(6):e0233641.
Mei Y, Lin Y. Clinical significance of primary symptoms in women with placental abruption. J Matern Fetal Neonatal Med. 2018;31(18):2446–9.
Oyelese Y, Ananth CV. Placental abruption. Obstetrics and gynecology. 2006;108(4):1005–16.
Shinde GR, Vaswani BP, Patange RP, Laddad MM, Bhosale RB. Diagnostic performance of ultrasonography for detection of abruption and its clinical correlation and maternal and foetal outcome. J Clin Diagn Res. 2016;10(8):Qc04-7.
Practice Bulletin No. 187. Neural tube defects. Obstet Gynecol. 2017;130(6):e279–e90.
Sharony R, Dayan D, Kidron D, Manor M, Berkovitz A, Biron-Shental T, et al. Is the ratio of maternal serum to amniotic fluid AFP superior to serum levels as a predictor of pregnancy complications? Arch Gynecol Obstet. 2016;293(4):767–70.
Odendaal HJ, Geerts L, Nel DG, Brink LT, Hitchcock E, Groenewald CA. Effects of alcohol, cigarettes, methamphetamine and marijuana exposure during pregnancy on maternal serum alpha-fetoprotein levels at 20-24 weeks’ gestation. Journal of pediatrics & neonatal care. 2018;8(1).
Bartha JL, Comino-Delgado R, Arce F. Maternal serum alpha-fetoprotein in placental abruption associated with preterm labor. Int J Gynaecol Obstet. 1997;56(3):231–6.
Ngai I BP, Chazotte C, Merkatz I, Garry D. Maternal serum alpha-fetoprotein (MSAFP) and placental abruption poster session number 122 American Journal of Obstetrics and Gynecology January 2012 S67.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60.
Wilmink FA, Pham CT, Edge N, Hukkelhoven C, Steegers EAP, Mol BW. Timing of elective pre-labour caesarean section: a decision analysis. The Australian & New Zealand journal of obstetrics & gynaecology. 2019;59(2):221–7.
Lees CC, Stampalija T, Baschat A, da Silva CF, Ferrazzi E, Figueras F, et al. ISUOG Practice Guidelines: diagnosis and management of small-for-gestational-age fetus and fetal growth restriction. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2020;56(2):298–312.
Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, et al. Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2016;48(3):333–9.
Ananth CV, Lavery JA, Vintzileos AM, Skupski DW, Varner M, Saade G, et al. Severe placental abruption: clinical definition and associations with maternal complications. Am J Obstet Gynecol. 2016;214(2):272.e1-.e9.
Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H, et al. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007;5(2):266–73.
Ananth CV, Smulian JC, Srinivas N, Getahun D, Salihu HM. Risk of infant mortality among twins in relation to placental abruption: contributions of preterm birth and restricted fetal growth. Twin Res Hum Genet. 2005;8(5):524–31.
Sheiner E, Shoham-Vardi I, Hadar A, Hallak M, Hackmon R, Mazor M. Incidence, obstetric risk factors and pregnancy outcome of preterm placental abruption: a retrospective analysis. J Matern Fetal Neonatal Med. 2002;11(1):34–9.
Tikkanen M. Etiology, clinical manifestations, and prediction of placental abruption. Acta Obstet Gynecol Scand. 2010;89(6):732–40.
Tanacan A, Beksac MS, Orgul G, Duru S, Sener B, Karaagaoglu E. Impact of extractable nuclear antigen, anti-double stranded DNA, antiphospholipid antibody, and anticardiolipin antibody positivity on obstetrical complications and pregnancy outcomes. Human antibodies. 2019;27(2):135–41.
Beksac MS, Tanacan A, Ozten G, Cakar AN. Low-dose low-molecular-weight heparin prophylaxis against obstetrical complications in pregnancies with metabolic and immunological disorder-associated placental inflammation. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2020:1–8.
Rood K, Stiller R. Hereditary persistence of alpha-fetoprotein: a rare cause for unexplained alpha-fetoprotein elevations in pregnancy. Conn Med. 2013;77(1):43–5.
Kofinas A, Kofinas G, Sutija V. The role of second trimester ultrasound in the diagnosis of placental hypoechoic lesions leading to poor pregnancy outcome. J Matern Fetal Neonatal Med. 2007;20(12):859–66.
Abdalla N, Bachanek M, Trojanowski S, Cendrowski K, Sawicki W. Placental tumor (chorioangioma) as a cause of polyhydramnios: a case report. Int J Womens Health. 2014;6:955–9.
Huang T, Hoffman B, Meschino W, Kingdom J, Okun N. Prediction of adverse pregnancy outcomes by combinations of first and second trimester biochemistry markers used in the routine prenatal screening of Down syndrome. Prenatal diagnosis. 2010;30(5):471–7.
Toivonen S, Heinonen S, Anttila M, Kosma VM, Saarikoski S. Reproductive risk factors, Doppler findings, and outcome of affected births in placental abruption: a population-based analysis. Am J Perinatol. 2002;19(8):451–60.
Dugoff L, Hobbins JC, Malone FD, Porter TF, Luthy D, Comstock CH, et al. First-trimester maternal serum PAPP-A and free-beta subunit human chorionic gonadotropin concentrations and nuchal translucency are associated with obstetric complications: a population-based screening study (the FASTER Trial). Am J Obstet Gynecol. 2004;191(4):1446–51.
Florio P, Severi FM, Bocchi C, Luisi S, Petraglia F. Abruptio placentae and highest maternal serum activin A levels at mid-gestation: a two cases report. Placenta. 2003;24(2-3):279–80.
Author information
Authors and Affiliations
Contributions
Seyit Ahmet EROL: Original draft preparation, literature search, writing, data collection.
Orhan ALTINBOGA: Analysis/interpretation, reviewing, and editing.
Betul YAKISTIRAN: Data collection.
Filiz HALICI OZTURK: Data collection.
Emre BASER: Analysis/interpretation.
Ali Turhan CAGLAR: Conceptualization, methodology, visualization, reviewing, and editing.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of the University of Health Sciences, Zekai Tahir Burak Women’s Health Training and Research Hospital.
Informed Consent
The participants included in the study were informed of the study and their consent were obtained.
Competing Interest
The authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Erol, S.A., Altinboga, O., Yakistiran, B. et al. Evaluation of Actual Maternal Serum Alpha-Fetoprotein (MSAFP) Levels in Placental Abruption and Associations with Adverse Outcomes. SN Compr. Clin. Med. 3, 611–617 (2021). https://doi.org/10.1007/s42399-021-00794-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00794-7