Abstract
Objective
To determine the relationship between adverse pregnancy outcomes and maternal serum alpha-fetoprotein (MSAFP) levels.
Materials and methods
A retrospective cohort study was conducted on consecutive singleton pregnancies, screened for fetal Down syndrome, in the northern part of Thailand. The prospective database of our fetal Down screening program was assessed to recruit all consecutive records. Pregnancies with medical complication and fetal abnormality were excluded. The recruited women were categorized into three groups: normal (≥0.76 to ≤2.0 MoM), low (<0.76 MoM) and high (>2.0 MoM) MSAFP levels.
Results
Of 7,110 screened women, 5,486 met inclusion criteria, including 240; 5,016 and 230 in the group of high, normal and low MSAFP levels, respectively. The rates of preterm birth, pregnancy-induced hypertension (PIH), fetal growth restriction (FGR), fetal death, low birth weight (LBW) and low APGAR scores were significantly higher in women with high MSAFP levels (11.7 vs. 6.6 %, 7.5 vs. 3.3 %, 7.5 vs. 3.3 %, 2.1 vs. 0.3 %, 15.8 vs. 6.7 %, and 2.9 vs. 0.5 % respectively), with relative risk of 1.76, 2.28, 2.27, 7.46, 2.35 and 6.09, respectively. The rates of preterm birth, FGR and LBW were significantly lower in low MSAFP levels with relative risk of 0.39, 0.26 and 0.26, respectively, whereas the rates of PIH and fetal death and low Apgar scores were not significantly different.
Conclusions
Pregnant women with high MSAFP levels had an increased risk of poor pregnancy outcomes, while those with low MSAFP levels had a significantly lower risk of such outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perinatal mortality is one of the most common causes of public health problems and several attempts have been made to prevent or decrease this serious event [1]. Pregnancy complications such as preterm birth, PIH, and FGR etc., are common causes associated with an increased perinatal mortality. This study attempted to find the way to facilitate early detection of these pregnancy complications.
Currently, maternal serum biochemical markers have been used for many years as a screening test for fetal open neural tube defects and chromosomal abnormalities, in particular trisomy 21 and trisomy 18. Based on extensive experience of such a screening, abnormal values of the different analytes used in these screening tests have been linked to a variety of other adverse pregnancy outcomes including preterm birth, growth restriction and preeclampsia [2].
Maternal serum alpha-fetal protein (MSAFP), one component of the triple screen for Down syndrome, is a glycoprotein that is normally produced in early pregnancy by the fetal yolk sac, liver, and gastrointestinal tract as well as choroid plexuses [3]. Decreased MSAFP levels increase risk of fetal Down syndrome, whereas increased MSAFP levels are associated with fetal defects including open neural tube defects or exomphalos and increased transfer from the fetal to maternal circulation as a consequence of placental damage and increased production in the mother [4].
Unexplained high levels of maternal serum alpha-fetoprotein (MSAFP) have been associated with an increased risk of adverse pregnancy outcomes, such as fetal death before 28 weeks of gestation, perinatal death, low birth weight (LBW), preterm birth, and other obstetric complications. However, the association between unexplained low levels of MSAFP and poor pregnancy outcomes is controversial. Some studies suggest that low MSAFP levels be associated with an increased risk of fetal death, including spontaneous abortions and stillbirths [5, 6], while some study showed a tendency to have favorable outcomes among pregnancies with unexplained low levels of MSAFP [7, 8].
Therefore, it is possible that MSAFP levels may help identify pregnant women at a higher risk of adverse pregnancy outcomes. As already known, MSAFP concentrations in maternal serum are varied with several factors, including racial factor. Therefore, we conducted this study to determine the strength of relationship between MSAFP concentrations using our own reference range, and rates of preterm birth (primary objective) and other adverse pregnancy outcomes, such as PIH, FGR, Fetal death, LBW and low Apgar scores.
Materials and methods
A retrospective cohort study was conducted on consecutive low-risk pregnancies, undergoing second trimester screening for fetal Down syndrome between January 2010 and July 2013, at Department of Obstetrics and Gynecology, Chiang Mai University and our 32 network hospitals in the northern part of Thailand, under our established project for prenatal Down screening. The study was ethically approved by the institute review boards. The inclusion criteria consisted of: (1) singleton pregnancies and (2) reliable gestational age based on certain last menstrual period and ultrasound examination for crown-rump length in the first trimester or biparietal diameter in the first half of pregnancy. The exclusion criteria included: (1) fetal anomalies such as neural tube defect, etc., (2) fetal chromosomal abnormalities and (3) incomplete data, loss to follow-up or unavailability of the final outcomes. Baseline demographic data of the women, including maternal age, parity, maternal body weight, ethnic origin and illicit drug use as well as medical history were identified and recorded in the database at the time of blood sample collection. The collected blood samples were immediately transferred to the laboratory and were centrifuged for serum separation. The clinical assays for MSAFP were performed in batches to eliminate inter-assay variations, using DELFIA® Xpress system (Perkin Elmer, Waltham, MA, USA). The absolute concentrations of serum AFP were converted to MoM based on Thai gestation-specific medians and weight correction [9]. A combined risk of 1:250 or greater was considered positive, and karyotyping would be offered.
The recruited pregnant women from the prospective database were assigned to one of the following three groups; (1) women with elevated MSAFP levels (>2.0 MoM), (2) women with normal MSAFP levels (≥0.76 and ≤2.0 MoM) and (3) women with low MSAFP levels (<0.76 MoM). All were followed-up until delivery. The pregnancy outcomes were evaluated by our obstetric team and neonatal outcomes were evaluated by the pediatricians in the project. The primary outcomes were the rate of preterm births and the secondary outcomes were the rate of pregnancy-induced hypertension (PIH), fetal growth restriction (FGR), fetal death in utero, low birth weight (LBW) and low Apgar scores.
Definitions of pregnancy outcomes were as follows: (1) preterm birth: live birth before 37 weeks of gestation; (2) PIH (pregnancy-induced hypertension): systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg plus proteinuria ≥1+ on urinary dipstick or or 24-h urinary total protein ≥300 mg after GA 20 weeks; (3) FGR (fetal growth restriction): birth weight of below the 10th percentile of the normal growth curve; (4) fetal death: death of the fetus in utero after 20 weeks of gestation; (5) low birth weight: birth weight of less than 2,500 g; (6) low Apgar scores: the scores of <7 at 5 min after birth and (7) overall poor outcomes: any outcomes mentioned above.
Statistical analysis
The statistical analysis was performed using SPSS version 21.0 (IBM Corp. Released 2012; IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp). Descriptive statistics were used to compare baseline characteristics between the two groups, using Student t test for continuous variables and Chi-square or Fisher’s exact tests for categorical variables. P < 0.05 was considered statistically significant. Relative risk for preterm birth, PIH, FGR, fetal death, LBW and low APGAR scores among pregnancies with elevated or low MSAFP levels compared to the normal group was calculated, as well as 95 % CI.
Results
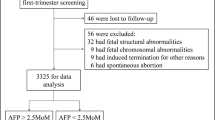
Of 7,110 pregnant women screened for fetal Down syndrome in the second trimester, 1,624 were excluded for various reasons including medical disease (342), fetal anomalies (245), fetal chromosomal abnormalities (75), loss to follow-up (482) and incomplete data (480). The remaining 5,486 women were available for analysis, including the three groups of high (240; 4.4 %), normal (5,016; 91.4 %) and low (230; 4.2 %) MSAFP levels, as presented in Fig. 1.
The epidemiological characteristics of the each study group were as follows: means maternal age (±SD) of the pregnancies in the group of high, normal and low MSAFP levels were 28.7 ± 5.3, 28.3 ± 5.7, and 27.7 ± 6.0 years, respectively, not significantly different (P = 0.362), and gestational ages in days at the time of sample collection were also not significantly different (111 ± 8, 110 ± 8, and 110 ± 9 days, respectively, P = 0.152). However, mean baseline maternal weight (kg) in the group of high MSAFP levels was significantly lower (54.4 + 8.4 kg) than the normal group (55.8 ± 10.1 kg), whereas that in the group of low MSAFP levels was significantly higher (58.1 ± 10.4); P < 0.001. The percentage of nulliparity among the group of high, normal and low MSAFP levels was not significantly different (40.8, 41.0, and 41.1 % respectively, P = 0.663).
Of the 5,486 pregnant women, 6.6 % (366) were preterm birth, 3.3 % (185) were PIH, 3.3 % (186) were FGR, 0.3 % (19) were fetal death, 6.9 % (380) were LBW and 0.5 % (32) were Low APGAR scores (APGAR score <7 at 5 min).
The mean gestational age of the group of high MSAFP levels was significantly lower than that in the normal group (37.8 ± 2.1 vs. 38.2 ± 1.6; P < 0.001) whereas the mean in the group of low MSAFP levels was significantly higher than that in the normal group (38.5 ± 1.2 vs. 38.2 ± 1.6; P < 0.001). Similarly, the mean birth weight in the group of high MSAFP was significantly lower than that in the normal group (2,921 ± 538 vs. 3,081 ± 451 g, P < 0.001), while the mean birth weight in the group of low MSAFP was significantly higher (3,137 ± 431 g, P < 0.001).
In comparison of pregnancy outcomes between the group of high MSAFP levels and the normal group, the rates of preterm birth, PIH, FGR, fetal death, LBW and low APGAR scores were significantly higher in women with elevated MSAFP levels (11.7 vs. 6.6 %, 7.5 vs. 3.3 %, 7.5 vs. 3.3 %, 2.1 vs. 0.3 %, 15.8 vs. 6.7 %, and 2.9 vs. 0.5 % respectively), with relative risk of 1.76, 2.28, 2.27, 7.46, 2.35 and 6.09, respectively, as presented in Table 1.
In comparison of pregnancy outcomes between the group of low MSAFP levels and the normal group as presented in Table 2, the rates of preterm birth, FGR and LBW were significantly lower in the low MSAFP group (2.6 vs. 6.6 %, 0.9 vs. 3.3 %, and 1.7 vs. 6.7 %, respectively), with relative risk of 0.39, 0.26 and 0.26, respectively, whereas the rates of PIH and fetal death and low Apgar scores were not significantly different between the two groups.
Discussion
The results of this study demonstrated that a high MSAFP level, as a component of second trimester serum marker screening, was an independent predictor of preterm birth, PIH, FGR, fetal death, LBW and low Apgar scores, consistent with previous western reports [10–20]. Though these findings are not new, this study confirmed that such a relation could also be reproducible among southeast Asian population like our pregnant women. This information may be clinically useful, especially in the area of high prevalence of preterm birth similar to our population, as high as 15 %. Pregnancies with high MSAFP levels are at a higher risk of preterm birth and other poor outcomes. Though, in the current guideline, preterm prevention in cases of high MSAFP levels is not recommended for progesterone prophylaxis as indicated in cases of prior preterm birth or short cervical length measured on transvaginal ultrasound [21], close monitoring for early detection or cervical length measurement at mid-pregnancy may be indicated in cases of unexplained high MSAFP levels. Nevertheless, clinical use of MSAFP measurement as a marker of an increased risk of poor pregnancy outcomes should be further explored. For examples, the relationship between cervical length and MSAFP levels should be studied. It is possible that pregnant women with high MSAFP levels and short cervix may be beneficial for progesterone prophylaxis as in pregnancies with prior preterm birth. Our results may serve as evidence for further studies in risk identification and prevention of spontaneous preterm delivery.
The association between low MSAFP levels and low risk for poor pregnancy outcomes has yet to be fully elucidated. Some studies showed the relationship between poor pregnancy outcomes and low MSAFP levels [22, 23], while some did not [8, 17]. Women who have low levels MSAFP in the second trimester of pregnancy are often informed that they have an increased risk of fetal Down syndrome. However, based on this study most euploid pregnancies with unexplained low MSAFP levels have a lower risk for poor pregnancy outcomes in terms of preterm birth, FGR, PIH and low birth weight. Therefore, MSAFP levels may be useful in identifying women with a low risk of common adverse pregnancy outcomes, consistent with the suggestion by Waller et al. [7].
Notably, the prevalence of low birth weight among pregnancies with low MSAFP levels was only 1.5 % compared to 15.8 %. Likewise the mean birth weight of newborns with low MSAFP levels was significantly higher than that among those with normal or elevated MSAFP levels. We may probably conclude that birth weight is inversely related to MSAFP levels. This observation may be consistent with the finding reported by Baschat et al. [24], who noted that very low levels of MSAFP in the second trimester were strongly associated with fetal macrosomia (fetal weight >90th centiles).
A low MSAFP level as a predictor of pregnancy outcomes has rarely been evaluated [7]. Spencer et al. [8] demonstrated that a low MSAFP level of less than 0.5 MoM had a significantly lower risk of preterm birth whereas it has a tendency to decrease risk of FGR and stillbirths but such associations did not reach a significant level. Most previous studies did not show a significant relationship between more favorable outcomes and low MSAFP levels. On the contrary, several reports demonstrated an increased risk of poor pregnancy outcomes with low MSAFP levels. Nevertheless, the important finding in this study is that low MSAFP level is significantly associated with better outcomes, including lower rates of preterm birth, PIH, FGR and low birth weight.
The strength of this study may include: (1) large sample size, (2) all laboratory tests were performed using the same machine/settings, (3) high homogeneity of the ethnic groups, northern Thai people and (4) exclusion of known potential pre-existing confounders of poor pregnancy outcome, resulting in high reliability of the conclusion. Limitations of this study may include a large number of losses to follow-up and cases with incomplete data. Additionally, other adverse outcomes like placental abruption, placenta previa, postpartum hemorrhage etc., which might possibly be associated with MSAFP levels were not evaluated.
In conclusion, pregnant women with elevated MSAFP levels (>2.0 MoM) in the second trimester had an increased risk of preterm birth, PIH, FGR, fetal death, LBW and low Apgar scores, while those with low MSAFP levels (<0.76 MoM) had a significantly lower risk of such outcomes. Further prospective studies are needed to determine whether intensive management based on MSAFP levels can improve the outcomes or not.
Abbreviations
- MSAFP:
-
Maternal serum alpha-fetoprotein
- PIH:
-
Pregnancy-induced hypertension
- FGR:
-
Fetal growth restriction
- LBW:
-
Low birth weight
References
Mizejewski GJ (2007) Physiology of alpha-fetoprotein as a biomarker for perinatal distress: relevance to adverse pregnancy outcome. Exp Biol Med (Maywood) 232:993–1004
Morris RK, Cnossen JS, Langejans M et al (2008) Serum screening with Down’s syndrome markers to predict pre-eclampsia and small for gestational age: systematic review and meta-analysis. BMC Pregnancy Childbirth 8:33
Mizejewski GJ (2004) Biological roles of alpha-fetoprotein during pregnancy and perinatal development. Exp Biol Med (Maywood) 229:439–463
Hay DM, Forrester PI, Hancock RL, Lorscheider FL (1976) Maternal serum alpha-fetoprotein in normal pregnancy. Br J Obstet Gynaecol 83:534–538
Merkatz IR, Nitowsky HM, Macri JN, Johnson WE (1984) An association between low maternal serum alpha-fetoprotein and fetal chromosomal abnormalities. Am J Obstet Gynecol 148:886–894
Simpson JL, Palomaki GE, Mercer B et al (1995) Associations between adverse perinatal outcome and serially obtained second- and third-trimester maternal serum alpha-fetoprotein measurements. Am J Obstet Gynecol 173:1742–1748
Waller DK, Lustig LS, Cunningham GC, Feuchtbaum LB, Hook EB (1996) The association between maternal serum alpha-fetoprotein and preterm birth, small for gestational age infants, preeclampsia, and placental complications. Obstet Gynecol 88:816–822
Spencer K (2000) Second-trimester prenatal screening for down syndrome and the relationship of maternal serum biochemical markers to pregnancy complications with adverse outcome. Prenat Diagn 20:652–656
Wanapirak C, Sirichotiyakul S, Luewan S et al (2012) Different median levels of serum triple markers in the second trimester of pregnancy in a Thai Ethnic Group. J Obstet Gynaecol Res 38:686–691
Jauniaux E, Gulbis B, Tunkel S, Ramsay B, Campbell S, Meuris S (1996) Maternal serum testing for alpha-fetoprotein and human chorionic gonadotropin in high-risk pregnancies. Prenat Diagn 16:1129–1135
Milunsky A, Jick SS, Bruell CL et al (1989) Predictive values, relative risks, and overall benefits of high and low maternal serum alpha-fetoprotein screening in singleton pregnancies: new epidemiologic data. Am J Obstet Gynecol 161:291–297
Raty R, Koskinen P, Alanen A, Irjala K, Matinlauri I, Ekblad U (1999) Prediction of pre-eclampsia with maternal mid-trimester total renin, inhibin A, AFP and free beta-hCG levels. Prenat Diagn 19:122–127
Wald NJ, Morris JK, Ibison J, Wu T, George LM (2006) Screening in early pregnancy for pre-eclampsia using Down syndrome quadruple test markers. Prenat Diagn 26:559–564
Dugoff L, Hobbins JC, Malone FD et al (2005) Quad screen as a predictor of adverse pregnancy outcome. Obstet Gynecol 106:260–267
Capeless EL, Kelleher PC, Walters CP (1992) Elevated maternal serum alpha-fetoprotein levels and maternal risk factors. Their association with pregnancy complications. J Reprod Med 37:257–260
Morssink LP, Heringa MP, Beekhuis JR, De Wolf BT, Mantingh A (1997) The association between hypertensive disorders of pregnancy and abnormal second-trimester maternal serum levels of hCG and alpha-fetoprotein. Obstet Gynecol 89:666–670
Cho S, Durfee KK, Keel BA, Parks LH (1997) Perinatal outcomes in a prospective matched pair study of pregnancy and unexplained elevated or low AFP screening. J Perinat Med 25:476–483
Pouta AM, Hartikainen AL, Vuolteenaho OJ, Ruokonen AO, Laatikainen TJ (1998) Midtrimester N-terminal proatrial natriuretic peptide, free beta hCG, and alpha-fetoprotein in predicting preeclampsia. Obstet Gynecol 91:940–944
Hershkovitz R, de Swiet M, Kingdom J (2005) Mid-trimester placentation assessment in high-risk pregnancies using maternal serum screening and uterine artery Doppler. Hypertens Pregnancy 24:273–280
Brazerol WF, Grover S, Donnenfeld AE (1994) Unexplained elevated maternal serum alpha-fetoprotein levels and perinatal outcome in an urban clinic population. Am J Obstet Gynecol 171:1030–1035
Society for Maternal-Fetal Medicine Publications Committee (2012) Progesterone and preterm birth prevention: translating clinical trials data into clinical practice. Am J Obstet Gynecol 206:376–386
Burton BK (1988) Outcome of pregnancy in patients with unexplained elevated or low levels of maternal serum alpha-fetoprotein. Obstet Gynecol 72:709–713
Krause TG, Christens P, Wohlfahrt J, Lei U, Westergaard T, Norgaard-Pedersen B et al (2001) Second-trimester maternal serum alpha-fetoprotein and risk of adverse pregnancy outcome. Obstet Gynecol 97:277–282
Baschat AA, Harman CR, Farid G, Chodirker BN, Evans JA (2002) Very low second-trimester maternal serum alpha-fetoprotein: association with high birth weight. Obstet Gynecol 99:531–536
Acknowledgments
The Faculty of Medicine Research Fund of Chiang Mai University, and the National Research University Project under Thailand’s Office of the Higher Education Commission.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puntachai, P., Wanapirak, C., Sirichotiyakul, S. et al. Associations between pregnancy outcomes and unexplained high and low maternal serum alpha-fetoprotein levels. Arch Gynecol Obstet 292, 81–85 (2015). https://doi.org/10.1007/s00404-014-3606-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3606-9