Abstract
High-acuity patients occasionally require advanced resources and monitoring, but do not qualify for intensive care admission in large intensive care unit (ICU). For these patients, intermediate care units (IMCUs) can provide adequate care. IMCUs lessen the patient burden for both the general ward and the ICU, allowing for more free beds in the ICU and ward. The main purpose of this study was to explore typical patient characteristics/demographics of patients admitted to an IMCU from the emergency room (ER) and mortality rate. This study is a retrospective cross-sectional study of a medical surveillance unit (MSU), which is an IMCU located in Pasqua Hospital, Regina. All patients admitted to the MSU from the ER in 2017 and 2018 were included in the study. This study retrospectively reviewed 715 patients in total. Patients’ age, sex, discharge disposition, comorbidities, primary and secondary diagnoses, admission and discharge date to/from the MSU, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, early assessment and response system (EARS) score, and acuity score were recorded. A total of 715 patient charts were reviewed for this study, with 323 patients in 2017 and 392 patients in 2018. Approximately a third of the study participants were diabetic, and half were hypertensive. Male sex had higher comorbidities including asthma or cerebrovascular accidents, and women had been diagnosed with coronary heart disease or liver disease. Both male and female were equally affected by substance use. 25.6% of the study population were smokers, 15.5% were intravenous drugs, and 16.8% were suffering with alcohol use disorder. Respiratory diseases account for a quarter of all primary diagnoses made in the MSU. Overall mortality rate was 5.9%. The APACHE II, EARS, and acuity scores were significantly different between deceased and alive patients (p < 0.001, p < 0.007, and p < 0.001, respectively). Half of the patients were discharged to home and a quarter were transferred to the ward. Nearly two-third of the study population was not readmitted to hospital within 30 days. This is one of the first studies to describe IMCU patients characteristics transferred from the ER in Canada. The APACHE II, EARS, and acuity scores were found significantly different between deceased and alive patients. These scores could therefore be used to develop tools that can identify high-risk patients for equitable allocation of healthcare resources to reduce mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Certain patients require high-acuity care but do not qualify for intensive care unit (ICU) admission. For these patients, intermediate care units (IMCUs) can provide adequate care. IMCUs are dedicated wards for patients that are too high of an acuity for a general ward, but not acute enough for an ICU [1, 2]. IMCUs are growing in popularity among North American hospitals; however, there is very little information published about them [3]. Most of the information regarding IMCUs comes from Europe and to a lesser extent in the USA [4].
IMCUs lessen the patient’s burden for both the general ward and the ICU, allowing for more free beds in the ICU and ward. This ensures that patients are more likely to receive appropriate care upon admission to the hospital [5,6,7]. Additionally, IMCUs can shorten emergency room (ER) waiting time by facilitating faster transfers to inpatient beds [8].
The MSU located in Pasqua Hospital, Regina, Saskatchewan, functions as an IMCU and acted as the source of information for this study. This IMCU has been operational since January 15, 2016. The MSU uses a modified early warning score (MEWS) called the EARS score. Additionally, to help triage patients to appropriate nursing teams, the MSU also utilizes an acuity score for all incoming and discharged patients. While these scores aid in triaging patients, their predictive value for mortality has not been studied. While other MEWS scores have been validated for predicting mortality [9], the early assessment and response system (EARS) and acuity scores have not.
An additional score studied was the Acute Physiology and Chronic Health Evaluation II (APACHE II) score. While this score has been validated in the ICU setting, there is minimal information published validating APACHE II scores in IMCUs [10]. A previous study was conducted at the MSU to explore typical IMCU patient demographics and where most of the patients admitted to the MSU were transferred from. That study found that most patients admitted to the MSU were transferred from the ER, and therefore, the MSU was being used primarily as a step-up in care from the ER/ward as opposed to a step-down in care from the ICU as previous studies have suggested [8].
The purpose of this study is to explore typical patient characteristics/demographics of patients admitted to/from the MSU from the ER. This study also assesses the EARS, acuity, and APACHE II scores and mortality in an IMCU. Additionally, the results of this study can guide resource management and staff training and can potentially inform guidelines for new and existing IMCUs.
Methods
This is a retrospective cross-sectional study of a MSU, located in Pasqua Hospital, Regina. In January 2016, MSU launched an intermediate care model within the Pasqua Hospital which is one of the two tertiary care hospitals in Regina. About 50% of MSU patient volume has been from the ER, 22% through intensive care transfers, and 28% has been from other inpatient medical areas including postoperative patients who require a higher level of care or monitoring. All patients are admitted to the hospitalist, and all are consulted to general internal medicine. Assessing real-time patient condition using the newly adopted Early Assessment Response System (EARS) has been very useful in allowing staff to not only intervene in a timely fashion to changes in the status of patient vital signs but to quantify patient acuity and manage the requirements of appropriate staffing models related to patient needs.
All patients admitted to the MSU from the ER in 2017 and 2018 were included in the study. Using convenience sampling technique, 715 patients’ charts were reviewed. All data extracted from the patient charts was recorded in an anonymous manner in a password-protected USB drive in encrypted files. Each patient was assigned a unique study identification number. No unique patient identifiers such as medical record numbers were entered into the database, and the database was anonymous. Data analysis was performed on an anonymous dataset in order to protect patient confidentiality.
Information was gathered by a medical student who was not involved in the assessment or treatment of the patients studied. Patients’ age, gender, discharge disposition, comorbidities, primary and secondary diagnoses, admission and discharge date to the MSU, EARS score, acuity score (ranges from 1 to 5, where more critical the patient’s condition, the higher the level of acuity, level 1 being the highest and level 5 the lowest), and APACHE II score [11] are recorded (Table 1). The patients’ primary and secondary diagnoses were further sorted into categories for analysis.
This study has been reviewed and approved on ethical grounds by the research ethics board of the former Regina Qu’Appelle Health Region, Regina, SK, Canada (REB/19-58). Waiver of informed consent was approved by research ethics board as this study meets criteria a-f of Article 5.5 in the Tri-Council Policy Statement-2 (TCPS). In this retrospective chart review, our estimated sample size was 715 patients admitted in the medical surveillance unit at the Pasqua Hospital.
Statistical analysis was performed using SPSS Statistics software (Version 22.0. Armonk, NY: IBM Corp.). Data was expressed in frequencies, mean, and percentages. Chi-square test was used as a test of significance to compare differences between groups for categorical data, and t test/Mann Whitney U test was used for continuous data. Significance will be set at p < 0.05 level. Kaplan-Meier survival curve was developed for both males and females to illustrate which gender survived most.
Results
A total of 715 patient charts were reviewed for this study, with 323 patients in 2017 and 392 patients in 2018. A summary of the patient characteristics and comorbidities is presented in Table 2. Of the patients studied, 342 were female and 373 were male. The mean age of participants is 62.72 ± 20.84 years ranged from 16 to 101 years. Approximately a third of participants had diabetes, and half had hypertension. 11.4% of participants had renal disease. 11.5% of participants had asthma, and men were almost twice as likely to had a diagnosis of asthma compared to women (p < 0.008). A quarter of participants had chronic obstructive pulmonary disease (COPD), and men and women were equally had this diagnosis. Coronary heart disease had a prevalence of 16.8%, and liver disease had a prevalence of 16.4%. Approximately one-tenth of participants had a diagnosis of dementia, with no significant difference between women or men. 15.3% of participants had had a cerebrovascular accident (CVA) in the past. Interestingly, many participants either smoked or had substance use disorders including intravenous drugs and alcohol. 25.6% of participants smoke, 15.5% use intravenous drugs, and 16.8% had an alcohol use disorder. No significant association was observed between gender and smoke, use intravenous drugs, or had an alcohol use disorder (p < 0.44, p < 0.29, p < 0.08, respectively).
Patients’ reason for hospitalization, primary diagnosis, and secondary diagnosis are presented in Table 3. The most common hospital reason and primary diagnosis accounting for about a quarter of all primary diagnoses are respiratory diseases. Infections were the next most common reason for hospitalization and primary diagnosis, accounting for about a fifth of all primary diagnoses. Gastrointestinal and cardiovascular diagnoses account for 14% and 12.6% of primary diagnoses, respectively. Other diagnoses such as diabetes and cancer were less than 10% of the total primary diagnoses studied.
Table 4 describes the APACHE II, EARS, and acuity scores on admission and discharge to the MSU. The average APACHE II score among patients that were discharged from hospital is 9.81 ± 4.99, and the score for patients that died in hospital is 16.86 ± 5.27. This difference in scores is statistically significant (p < 0.001). A similar trend is seen with admitting EARS, disposition EARS, and admitting acuity scores (p < 0.007, p < 0.001, and p < 0.001, respectively). The disposition acuity score did not reach significance between the alive and deceased population.
Majority of APACHE II scores were between 6 and 10, with 41.8% of participants falling in this range of scores. Approximately a quarter of participates (26.6%) were between APACHE II scores of 11 and 15. Less than one-fifth, 13.8% and 17.8% of study participants were in the highest (> 15) and lowest (0–5) score ranges, respectively. Half of study participants (50.3%) were discharged home from the MSU, and about one-quarter (26.6%) were transferred to the ward. Twelve percent of participants were transferred to alternative level of care (ALC); 5.2% were transferred to the ICU of which 43.2% had primarily diagnosed with respiratory, 18.9% gastrointestinal, 16.2% with infection, and 21.7% with other disease. Out of 715, MSU admitted patients 42 (5.9%) had a fatal outcome, of which 26.2% had a primary diagnosis of respiratory illness, 23.8% infection, 14.3% cardiovascular, 14.3% gastrointestinal, and 21.4% with other illnesses.
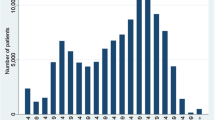
A total of 4.3% of participants were readmitted to hospital in less than 7 days, 3.6% in 7–14 days, and 6.2% 15–30 days. Nearly two-third of participants (male 74.3% and female 69%) were not readmitted to hospital within 30 days. Approximately one-eighth of participants (male 12.9% and female 15.5%) were deceased within 30 days of discharge from hospital. Kaplan-Meier curves (Fig. 1) reveal that the estimated mean survival time for a month was 24.54 (95% confidence interval (CI): 20.49–28.59) days in females and 24.49 (95% CI: 23.21–25.77) days in their males (p − 0.509). The survival curve horizontal axis shows the time to event. In this plot, drops in the survival curve occur whenever the event occurs. The vertical axis shows the probability of survival (probability of not experience the event).
Discussion
Canadian studies on IMCUs and their patients are lacking, and this study is one of the few that addresses this topic. There had been similar studies in the USA and Europe, but these studies did not had the same level of data on patients’ demographics and comorbidities [5, 7, 12]. This study conducted an in-depth analysis on 715 patients admitted to an IMCU from the ER in 2017 and 2018 in Central Canada.
This study analyzed a large variety of comorbidities among MSU patients such as diabetes and hypertension. Over half the patients had hypertension and over a third had diabetes, which is similar to our previous study as well as other published research [7, 13]. Interestingly, the rates of diabetes and hypertension in this study (33.8% and 54.8%, respectively) are higher than the reported prevalence in Canada [14]. This finding was likely due to single-center patient’s data and different ethnic proportion of study population. Previous research also suggests that prevalence rates in hypertension and diabetes are higher among south Asian and Black Canadians than White Canadians [15, 16]. Another study highlights the complexity of the unequal distribution of hypertension and diabetes, which includes inordinately high risks of both outcomes for poor Black women and an absence of associations between income and both outcomes for Black men in Canada [17].
Our APACHE II scores for patients that survived or died in hospital were 9.81 ± 4.99 and 16.86 ± 5.27 (p < 0.001), respectively. Fernandes et al.’s study also measured APACHE II scores and found that survivors had a mean score of 13.66 ± 6.52 and non-survivors had a mean score of 20.04 ± 5.84 (p < 0.001) [13]. While both our study and Fernandes et al.’s study found that the APACHE II score is an independent predictor of mortality in their respective IMCUs, the Fernandes et al. study’s scores were consistently higher than those in our study. This is most likely because their study included all patients admitted to their IMCU, whereas our study included only those admitted from the ER, who are generally of a lower acuity than those from other units.
Interestingly, the EARS score was significantly different between alive and deceased MSU patients. Other MEWS had been validated as prognostic indicators in various other wards [9], but the EARS score had not been rigorously studied. On general medical wards, MEWS had been shown to be excellent prognostic indicators by mostly using information from triage [18]. The acuity score uses similar criteria for scores but also includes factors that affect nursing workload such as the number of intravenous medications that the patient needs. Because both the EARS and acuity scores used similar variables to other MEWS [18], it is likely this was the reason they were both significantly different in alive and deceased patient.
Most patients admitted from the ER were either discharged home or transferred to the ward. Because almost half of the patients admitted to the MSU were discharged home, there were implications for staffing to offer services such as home care. The mortality rate was found to be 5.9%, which was about 4% less than our previous study and other studies of intermediate care units [13]. This was likely because our previous study population was all transfers to the MSU, and the current study looked only at transfers from the ER (which is lower acuity). A readmission rate within 30 days was approximately 15%. While readmission rates vary by location, staffing, and acuity of patients, this was typical for higher acuity wards [19].
A main limitation of this study was that data collection was limited to electronic health records. Some data may had been missed as the data may not had been transcribed or easily found within the record. Another limitation was that it is limited, as 2 years may not be enough time to see long-term trends in the data. While this study did not address cost or resource use for this cohort of patients, other studies had found that IMCUs are cost-effective overall [20, 21]. While these studies are based out of Europe and were based on individual hospitals, they indicate that the cost savings were between 500,000 and 1,500,000 euros per year. Thus, while a cost analysis of each individual IMCU is required due to the varying nature of their implementation, most IMCUs studied do show a reduction in total costs.
This study results found significant difference between alive and deceased patients EARS score, acuity score, and APACHE II scores, and that the patient demographics in a Canadian IMCU was similar to those in the USA and Europe. Additionally, this study’s findings can provide information for staffing IMCUs and resource allocation moving forward.
Conclusion
This was one of the first studies to describe IMCU patients transferred from the ER in Canada. Characterization of this subpopulation of the MSU should act to inform investigations and care plans for optimal patient care. The APACHE II, EARS, and acuity scores were found significantly different between deceased and alive patients. Future research is needed to develop a predictive model and an algorithm to utilize EARS, acuity, and APACHE II cut-off values to predict patient’s outcomes in IMCU.
Abbreviations
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- COPD:
-
Chronic obstructive pulmonary disease
- EARS:
-
Early Assessment and Response System
- ER:
-
Emergency room
- IMCU:
-
Intermediate care units
- ICU:
-
Intensive care unit
- MEWS:
-
Modified early warning score
- MSU:
-
Medical surveillance unit
- TCPS:
-
Tri-Council Policy Statement
References
Melis RJF, Rikkert MGMO, Parker SG, van Eijken MIJ. What is intermediate care? BMJ. 2004;329(7462):360–1.
Nasraway SA, Cohen IL, Dennis RC, Howenstein MA, Nikas DK, Warren J, et al. Guidelines on admission and discharge for adult intermediate care units. American College of Critical Care Medicine of the Society of Critical Care Medicine. Crit Care Med. 1998;26(3):607–10.
Sjoding MW, Valley TS, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR. Rising billing for intermediate intensive care among hospitalized Medicare beneficiaries between 1996 and 2010. Am J Respir Crit Care Med. 2016;193(2):163–70. https://doi.org/10.1164/rccm.201506-1252OC.
Prin M, Wunsch H. The role of Stepdown beds in hospital care. Am J Respir Crit Care Med. 2014;190(11):1210–6. https://doi.org/10.1164/rccm.201406-1117PP.
Capuzzo M, Volta C, Tassinati T, Moreno R, Valentin A, Guidet B, et al. Hospital mortality of adults admitted to intensive care units in hospitals with and without intermediate care units: a multicentre European cohort study. Crit Care (London, England). 2014;18(5):551. https://doi.org/10.1186/s13054-014-0551-8.
Hall AM, Stelfox HT, Wang X, Chen G, Zuege DJ, Dodek P, et al. Association between afterhours admission to the intensive care unit, strained capacity, and mortality: a retrospective cohort study. Crit Care (London, England). 2018;22(1):97. https://doi.org/10.1186/s13054-018-2027-8.
Simpson CE, Sahetya SK, Bradsher RW 3rd, Scholten EL, Bain W, Siddique SM, et al. Outcomes of emergency medical patients admitted to an intermediate care unit with detailed admission guidelines. Am J Crit Care. 2017;26(1):e1–e10. https://doi.org/10.4037/ajcc2017253.
Gershengorn HB, Chan CW, Xu Y, Sun H, Levy R, Armony M, et al. The impact of opening a medical step-down unit on medically critically ill patient outcomes and throughput: a difference-in-differences analysis. J Intensive Care Med. 2018;885066618761810:425–37. https://doi.org/10.1177/0885066618761810.
Cuthbertson BH, Boroujerdi M, McKie L, Aucott L, Prescott G. Can physiological variables and early warning scoring systems allow early recognition of the deteriorating surgical patient? Crit Care Med. 2007;35(2):402–9. https://doi.org/10.1097/01.Ccm.0000254826.10520.87.
Torres OH, Francia E, Longobardi V, Gich I, Benito S, Ruiz D. Short- and long-term outcomes of older patients in intermediate care units. Intensive Care Med. 2006;32(7):1052–9. https://doi.org/10.1007/s00134-006-0170-1.
Akavipat P, Thinkhamrop J, Thinkhamrop B, Sriraj W. Acute physiology and chronic health evaluation (APACHE) II score - the clinical predictor in neurosurgical intensive care unit. Acta Clin Croat. 2019;58(1):50–6. https://doi.org/10.20471/acc.2019.58.01.07.
Lu L, Chan C, Green L, Escobar GJ. The impact of step-down unit care on patient outcomes. Columbia Business School Research Paper No. 16–74. 2014. Available at SSRN: https://ssrn.com/abstract=2859231 or https://doi.org/10.2139/ssrn.2859231. Accessed 20 June 2020.
Fernandes L, Duque S, Silvestre J, Freitas P, Pinto M, Sousa A, et al. Prognostic factors of patients admitted in a medical intermediate care unit: a prospective observational study. Int Arch Med. 2015;8. https://doi.org/10.3823/1762.
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–49. https://doi.org/10.1016/j.diabres.2013.11.002.
Chiu M, Austin PC, Manuel DG, Tu JV. Comparison of cardiovascular risk profiles among ethnic groups using population health surveys between 1996 and 2007. CMAJ. 2010;182(8):E301–10. https://doi.org/10.1503/cmaj.091676.
Chiu M, Maclagan LC, Tu JV, Shah BR. Temporal trends in cardiovascular disease risk factors among white, South Asian, Chinese and black groups in Ontario, Canada, 2001 to 2012: a population-based study. BMJ Open. 2015;5(8):e007232. https://doi.org/10.1136/bmjopen-2014-007232.
Gagné T, Veenstra G. Inequalities in hypertension and diabetes in Canada: intersections between racial identity, gender, and income. Ethn Dis. 2017;27(4):371–8. https://doi.org/10.18865/ed.27.4.371.
Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified early warning score in medical admissions. Qjm. 2001;94(10):521–6. https://doi.org/10.1093/qjmed/94.10.521.
Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care. 2009;21(6):397–407. https://doi.org/10.1093/intqhc/mzp045.
Heili Frades Zimmermann SB, Carballosa De Miguel MDP, Galdeano Lozano M, Mate García X, Mahillo Fernández I, Fernández Ormaechea I, et al. Cost analysis of an intermediate respiratory care unit. Is it really efficient and safe? Eur Respir J. 2019;54(suppl 63):PA1972. https://doi.org/10.1183/13993003.congress-2019.PA1972.
Plate JDJ, Peelen LM, Leenen LPH, Hietbrink F. The intermediate care unit as a cost-reducing critical care facility in tertiary referral hospitals: a single-centre observational study. BMJ Open. 2019;9(6):e026359-e. https://doi.org/10.1136/bmjopen-2018-026359.
Acknowledgments
Thank you to the University of Saskatchewan, College of Medicine, Dean’s Project for supporting this research.
Author information
Authors and Affiliations
Contributions
KL and MAS conceived the study. KV has collected the data and MAS analyzed the data. KV and MAS drafted the manuscript, while MC, KL, KV, and MAS revised and reviewed the whole manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
The study protocol was approved by the former Regina Research Ethics Board (REB/19-58), Saskatchewan Health Authority, Regina, SK, Canada.
Consent for Publication
Not applicable.
Availability of Data and Materials
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Vantomme, K., Siddiqui, M., Cossette, M. et al. Outcomes of Emergency Medical Patients Admitted to a Medical Surveillance Unit: a Retrospective Cross-Sectional Study. SN Compr. Clin. Med. 2, 2771–2777 (2020). https://doi.org/10.1007/s42399-020-00622-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00622-4