Abstract
Objective
To evaluate short- and long-term outcomes of elderly patients (≥ 65 years) treated at an intermediate care unit (IMCU) and to identify outcome predictors.
Design and setting
Prospective observational study in the IMCU of a university teaching hospital.
Participants
We studied 412 patients over 8 months, classified into three groups: under 65 years (control group, n = 158), 65–80 (n = 186), and > 80 (n = 68).
Measurements
At admission: APACHE II, TISS-28 first day, Charlson Index, diagnosis, and prior Barthel Index. Outcome measures: in-hospital mortality, length of stay, discharge destination, and 2-year mortality and readmissions. Data analysis included multivariate logistic regression and receiver operating characteristics area under the curve (ROC AUC).
Results
No statistically significant differences between groups were observed in hospital mortality (14.1%), discharge to a long-term facility (2.7%), or 2-year readmissions (1.2 ± 2.1). However, hospital stay was longer in patients aged 65–80 years (14 vs.10 days) and 2-year mortality was higher in those 65 or over (34% vs.10.6%). In the overall series in-hospital mortality was predicted by APACHE II, first-day TISS-28, and diagnosis (ROC AUC 0.81), and 2-year mortality by Charlson Index and age (ROC AUC 0.77). In the elderly patients 2-year mortality was predicted by Charlson and Barthel indices (ROC AUC 0.70).
Conclusions
Illness severity and therapeutic intervention at admission to IMCU were predictors of short-term mortality, whereas the strongest predictor of long-term mortality was comorbidity. Our results suggest that comprehensive assessment of elderly patients at admission to IMCUs may improve outcome prediction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intermediate care units (IMCUs), also called step-down units or high-dependency units, attempt to provide appropriate resources to a subset of critically ill patients who do not require all the resources of a full intensive care unit (ICU) but need more care than that available in general wards [1]. An increasing number of elderly patients are being treated in these units [2, 3], but little is known about their previous functional status, comorbidity, severity of illness, and short- and long-term outcomes. This information is important in clinical practice when deciding whether to resuscitate, to initiate major organ support (e.g., mechanical ventilation, renal dialysis), and to transfer the patients to an ICU. Some studies in critical care units suggest that increasing age contributes to poorer outcome [4, 5], whereas others show that severity of the illness at admission is a better prognostic indicator [6, 7]. Nevertheless, studies addressing this subject in IMCUs are scarce. De Silva et al. [8] reported that increased age in a high-dependency unit was associated with poorer outcome in terms of physiological dysfunction measured by the Logistic Organ Dysfunction System score. Brooks [9] found, however, that older and sicker patients reported higher levels of satisfaction with their resulting quality of life. More recently, Ip et al. [10] concluded from their study of 150 unselected critically ill medical patients older than 70 years that high-dependency care for elderly patients is worthwhile.
The primary objective of this study was prospectively to evaluate short- [11] and long-term mortality in elderly patients admitted to an IMCU in comparison with younger patients. We also assessed other outcomes such as length of hospital stay, discharge destination, and hospital readmissions. It was hypothesized that prognosis in elderly patients depends more on severity of illness, comorbidity, previous functional status, and therapeutic intervention than on chronological age.
Methods
Setting
Hospital de la Santa Creu i Sant Pau comprises a 600-bed acute care center, a 30-bed ICU, and a 20-bed IMCU. The multidisciplinary IMCU is adjacent to the ICU. Patients are admitted to the IMCU from the emergency department, acute hospital wards, ICU, or directly from other hospitals. All patients in the sample required high-dependency care that could not be provided in a general ward, including intensive nursing care (e.g., hourly observation, continuous electrocardiographic monitoring), and active intervention (e.g., inotropic agents, noninvasive mechanical ventilation) or invasive monitoring (e.g., arterial or central venous catheter). Organ support such as invasive mechanical ventilation and renal dialysis was performed occasionally, mainly in patients receiving chronic therapy and those awaiting a ICU bed. More complex forms of life support were not usually provided.
Patients
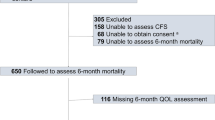
We prospectively studied 412 patients admitted to the IMCU during daytime hours on weekdays between March and October 2000 (mean age 64.6 ± 17.5 years, 158 aged under 65 and 254 aged 65 or over; 65% men). Admissions were from the emergency department in 80.1% of cases, hospital wards in 8%, ICU in 6.6%, and other hospitals in 5.3%. Patients were categorized according to their age as follows: under 65, 65–80, and over 80 years; there were no statistically significant differences between the three age groups in admission source. Table 1 shows patients' baseline characteristics and diagnoses. It was not possible to enroll all patients because of logistic constraints; at nights and on weekends there was only a single staff physician on duty and a high turnover in nursing shifts. Patients admitted several times during the study were followed only on their first admission. Age, sex, in-hospital mortality, and length of stay of the included patients were compared with the other 1,183 patients treated in the IMCU in 2000 who were not included in the study, and we found no statistically significant differences (see Table E1, electronic supplementary material, ESM). The follow-up process is outlined in Fig. 1.
Data collection
Data collected at the time of IMCU admission by the attending physician were: age, sex, origin, Acute Physiology and Chronic Health Evaluation (APACHE) II score [12], ability to perform basic activities of daily living 15 days prior to hospital admission, comorbidity, and diagnosis. The principal diagnosis or main reason for IMCU admission was coded as one of ten diagnostic categories: coronary syndrome, heart failure, gastrointestinal bleeding, trauma, stroke, respiratory disease, sepsis, overdose, postsurgery, or other (see explanation of the diagnostic coding in the ESM). Data about ability to perform basic activities of daily living were self-reported and gathered from information obtained at a structured interview conducted at the IMCU admission between patients, and/or their relatives, and the attending physician. The Therapeutic Intervention Scoring System (TISS-28) [13] was administered by the attending nurse. Evaluation at admission followed predetermined protocols, and all staff involved in the study had been trained in this. A separate group of trained clinician-researchers (O.H.T., E.F. and V.L.) conducted a detailed review of hospital records for IMCU and in-hospital mortality, length of IMCU and hospital stay for survivors, and discharge destination. Two years later readmissions and postdischarge mortality were determined from medical records and/or telephone questionnaire. Thirty-four patients (8.3%) were lost to follow-up.
Measurements
Severity of illness was measured using the APACHE II scoring system [12], which was designed to characterize severity of illness in critical care patients. This includes three types of data collected during the first 24 h after admission: worst value for physiological variables, age, and the presence of severe chronic illness. Scores can range from 0 to 71, with higher scores indicating more severe illness. Therapeutic intervention was determined in the first 24 h after admission using TISS-28 [13]. This scoring system enables quantitative comparisons of patient care and can help in allocating resources. Points are assigned for specific interventions in the critical care unit over a 24-h period and range from 1 to 4. Higher values are given for more specialized, critical or life-sustaining activities. Dependency in basic activities of daily living was scored using the Barthel Index [14], which measures the capacity to perform ten basic activities and gives a quantitative estimation of the patient's level of dependency, scoring from 0 (totally dependent) to 100 (totally independent). This index has been proposed as the standard for clinical and research purposes [15]. The Charlson Index was used as a comorbidity index. It scores from 1 to 6 for 18 specific medical diagnoses, representing increasing levels of illness. Scores have been shown to be correlated with long-term survival following acute medical illness [16].
Analyses
Descriptive statistics for continuous variables were expressed as mean ± standard deviation, 95% confidence interval (CI) for the mean, and median. The Kruskal-Wallis test was used to compare groups, and Fisher's exact test and the χ2 test were used for categorical variables. Spearman rank correlation coefficient was applied to determine significant correlations between parameters. Multiple logistic regression with forwards stepwise selection was used to determine prognostic factors of hospital mortality, length of stay, long-term destination at discharge, and 2-year readmission and mortality, adjusted for patients' characteristics (APACHE II, TISS-28 first day, Charlson score, Barthel Index, diagnosis, age, and sex). Colinearity was examined using a variance inflation factor [17] and condition indexes. Age was centered on its mean to reduce collinearity [17]. The entry criterion for the multivariate model was p ≤ 0.05. We defined cutoff points for the length of stay variables to create a binary dependent variable: 3 days for IMCU stay and 12 days for hospital stay. These cutoff points were chosen because they were the median values for the variables. Furthermore, based on our clinical experience, these levels corresponded to usual stays vs. longer and/or complicated IMCU and hospital stays. The receiver operating characteristics (ROC) area under the curve (AUC) was used to assess models discrimination. Tests were two-tailed, and statistical significance was set at the p ≥ 0.05 level. The SPSS/Win statistical package (version 10.5) was used for all the analyses (SPSS, Chicago, Ill., USA).
Results
Table 2 shows the outcomes in each of the three age groups. No differences between groups were observed in IMCU length of stay (3.6 ± 6.3 days, 95% CI 2.9–4.2, median 3) or number of readmissions 2 years later (1.2 ± 2.1, 95% CI 1–1.4, median 0). There were also no statistically significant differences in outcomes, including IMCU mortality (7.8%), in-hospital mortality (14.1%), and discharge to a long-term care center (2.7%; data not shown). However, differences in hospital length of stay and 2-year mortality did differ significantly. As indicated in Table 2, it is of interest that 2-year mortality clearly differed between younger (< 65) and older patients (≥ 65; (10.6% vs. 34%, p ≤ 0.001), but between the two older age groups (p = 0.302). Hospital stay was longer for patients aged 65–84 years (14 vs.10 days, p = 0.004).
Multivariate logistic regression studies
Results of multivariate logistic regression studies and the ROC AUC are shown in Table 3. For IMCU and in-hospital mortality the logistic regression model showed APACHE II and TISS-28 first day as strong predictors (p ≤ 0.01). Diagnosis was also included in the model, and the diagnosis of stroke was a significant predictor (p ≤ 0.03). The only protective factor for IMCU mortality was the Barthel Index (p = 0.048). Mortality 2 years after discharge was predicted by the Charlson Index and age (p ≤ 0.001). These models showed good discrimination (ROC AUC 0.77–0.88). Good discriminant performance was also shown by the prediction model for discharge to a long-term facility (ROC AUC 0.80). Higher independence in activities of daily living measured by Barthel Index was a protective factor for discharge to a long-term facility (p = 0.003), whereas a higher score in TISS-28 first day was a predictor for discharge to a long-term facility (p = 0.047).
The analyses were repeated in the elderly patients (≥ 65 years), and similar results were found. However, when 2-year mortality was analyzed, age was not significant. We found 2-year mortality after discharge to be predicted by the Charlson Index (p = 0.001) and Barthel Index (p = 0.020; ROC AUC 0.70). Table 4 compares the results of logistic regression analyses in patients aged under 65 and those aged 65 years or older. Models for IMCU and in-hospital length of stay, and 2-year readmissions showed only fair to moderate discrimination (see Tables E2 and E3, ESM).
Discussion
Our results emphasize the importance of comprehensive assessment for IMCU patients to estimate prognosis more accurately and to avoid decisions based on age. Among the variables that we examined the indicators which maximized prognostic sensitivity and specificity were severity of illness and therapeutic intervention at admission for short-term outcomes while the strongest predictor of long-term mortality was comorbidity. The only outcome in which age showed an impact was long-term mortality. This effect was not observed in the elderly subgroup (those 65 years old or over).
IMCU mortality in our study was 7.8% and in-hospital mortality 14.1%. Although mortality was higher in older patients, the differences were not statistically significant. The mortality rate during hospitalization is comparable to the 17.6% reported by Porath et al. [18] in a medical IMCU with similar mean disease severity as measured by APACHE II (12.9 vs. 12.6 in our study). However, to our knowledge, mortality rates in elderly patients in IMCUs have not been reported previously, with the exception of the unselected group of critical patients 70 years old or over reported by Ip et al. [10] in a medical geriatric high-dependency unit. They found mortality 1 month after discharge from the hospital to be 48%.
Severity of illness scoring systems have been established to predict outcomes, specifically in ICU patients [12]. Ip et al. [10] reported a close correlation between APACHE II and short-term mortality in elderly patients treated in a medical high-dependency unit. In accordance with this finding, our study confirms APACHE II as an independent predictor for short-term mortality in adults.
Originally designed as a measure of illness severity, TISS has proven a reliable measurement of resource use in ICU patients. It has been used in IMCUs to differentiate between intensive care and high-dependency patients and to identify nursing skill requirements [19]. Wakefield et al. [20] reported that higher intervention TISS scores were significantly associated with 30-day mortality in a surgical high-dependency unit. In our study TISS-28 first day was also a predictor of short-term mortality.
The 2-year cumulative mortality rate in our series was 33.5% (20.9% in patients < 65 years and 45.6% in those ≥ 65 years). The only study to date on long-term outcomes in a high-dependency unit reported a 6-month cumulative mortality of 49.6% in medical patients of a similar age, but severity was higher than in our population (mean age 65 ± 16 years, mean APACHE II score 17.8 ± 8). Age was suggested as an important predictor, but only univariate analysis was performed [21]. Previous multivariate analyses of long-term mortality after ICU discharge have identified predictors such as age [5, 6, 7, 20], severity of illness [5, 7, 22, 23, 24], diagnosis [5, 7], prior functional status [6, 23, 24, 25], comorbidity [25], and immunocompromised state [23]. However, the value of chronological age as a predictor is controversial because some authors have found no association with long-term mortality in adults [24] or very elderly patients [22], and others have stated that the contribution of age in predicting survival is relatively low compared with the contribution of acute physiology or diagnosis [7]. In our study there were significant differences between younger and elderly (≥ 65 years) IMCU patients regarding long-term survival after discharge, but not between the two elderly groups (65–84 vs. ≥ 85 years). Thus in the overall series comorbidity and age were independent predictors for long-term mortality after discharge; however, age was not a significant predictor among elderly patients. In this population 2-year mortality was predicted by comorbidity and a lower Barthel Index. The importance of functional status for long-term survival in the elderly population has already been clearly established [6, 23, 24, 25].
Higher independence in activities of daily living measured by the Barthel Index was a protective factor not only for 2-year mortality but also for discharge to a long-term facility. To our knowledge, there are no studies in IMCU addressing the value of preadmission functional status as an outcome measure. However, in critical care units poor functional status has been reported to be related to poor short-term [4, 23, 26] and long-term [6, 24, 25] outcome and to lower chance of being discharged home [26]. In contrast in the very elderly population, Kass et al. [22] reported that preadmission functional status was not correlated with ICU or with 1-year mortality rates.
Our study has certain limitations. First, the study population was limited to a single community hospital with a relatively small number of patients. Multicentric studies in IMCUs are difficult because of the marked variations in the roles and capabilities of IMCUs internationally and even within individual hospitals. Second, our study population was heterogeneous, including postoperative and posttraumatic groups who carry a better prognosis [12]. For this reason we entered the possible confusing variable “diagnosis” in our analyses. From a practical viewpoint we were interested in the prognosis of the elderly patients as a group and in the conditions in which they were attended at IMCUs rather than the prognosis of the different subgroups of elderly patients. Third, because of logistic constraints it was not possible to enroll all the patients during the study period, and this may introduce a bias. Nevertheless, we compared our patients with the nonstudy patients admitted to the IMCU throughout 2000 (Table E1, ESM) and observed no statistically significant differences. Thus we consider our sample representative of the patients admitted to the IMCU. Furthermore, the observational study design could have introduced a preadmission bias: perhaps only the elderly patients with suspected good-prognosis were admitted to IMCU. To avoid this bias we adjusted outcomes not only for severity of illness, therapeutic intervention, and diagnosis but also for comorbidity and functional status. Finally, decisions such as admission to the ICU or initiation of organ support depended on the decision of the attending physician, thus having an impact on patient outcome. Moreover, information on the aggressiveness of treatment delivered after hospital discharge was not available; the oldest patients and those with higher dependency in activities of daily living may have received less aggressive treatment.
The strengths of our study, on the other hand, include its prospective design, the attempt to standardize a complete evaluation of patients admitted to IMCU, the detailed characterization of our patients in the different age groups, and, especially, the long-term follow-up of patients admitted to IMCU with a high degree of completeness (91.7%).
In conclusion, the contribution of age in predicting prognosis in elderly patients is relatively small compared with that of the four indices analyzed (APACHE II, first-day TISS-28, Charlson Index, Barthel Index). Such information may aid physicians in clinical decision making without overestimating risk related to chronological age. Future studies are required to evaluate prognosis in IMCUs, to examine how older age affects outcomes, and to provide objective analysis in this complex group of patients.
References
Cheng DC, Byrick RJ, Knobel E (1999) Structural models for intermediate care areas. Crit Care Med 27:2266–2271
Dhond G, Ridley S, Palmer M (1998) The impact of a high-dependency unit on the workload of an intensive care unit. Anaesthesia 53:841
Havill JH, Cranston D (1998) The place of the high dependency unit in a modern New Zealand hospital. N Z Med J 111:203–205
Quality of life after mechanical ventilation in the aged study investigators (2002) 2-month mortality and functional status of critically ill adult patients receiving mechanical ventilation. Chest 121:549–558
Djaiani G, Ridley S (1997) Outcome of intensive care in the elderly. Anaesthesia 52:1130–1136
Somme D, Maillet JM, Gisselbrecht M, Novara A, Ract C, Fagon JY (2003) Critically ill old and the oldest-old patients in intensive care: short- and long-term outcomes. Intensive Care Med 29:2137–2143
Hamel MB, Davis RB, Teno JM, Knaus WA, Lynn J, Harrel FJr, Galanos A, Wu AW, Phillips RS (1999) Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. Ann Intern Med 131:721–728
De Silva RJ, Anderson A, Tempest H, Ridley S (2001) Sequential organ scoring as a measure of effectiveness of care in the high-dependency unit. Anaesthesia 56:850–854
Brooks N (2000) Quality of life and the high-dependency unit. Intensive Crit Care Nurs 16:18–32
Ip S, Leung YF, Ip CY, Mak WP (1999) Outcomes of critically ill elderly patients: Is high-dependency care for geriatric patients worthwhile? Crit Care Med 27:2351–2357
Torres OH, Benito S, Ruiz D, Montiel JA, Francia E, Vázquez G (2003) Outcome of elderly patients in an Intermediate Care Area. Sixteenth Annual Congress from the European Society of Intensive Care Medicine; 2003 Oct 5–8; Amsterdam, Netherlands. Intensive Care Med 29 [Suppl 1]:115
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Miranda DR, de Rijk A, Schaufeli W (1996) Simplified Therapeutic Intervention Scoring System: the TISS-28 items-results from a multicenter study. Crit Care Med 24:64–73
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Maryland State Med J 14:61–65
Wade DT, Collin C (1988) The Barthel ADL Index: a standard measure of physical disability? Int Disabil Studies 10:64–67
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Kleinbaum DG, Kupper LL, Muller KE (1988) Applied regression analysis and other multivariables methods. PWS-Kent, Boston
Porath A, Reuveni H, Grinberg G, Lieberman D (1995) The intermediate care unit as a cost-effective option for the treatment of medical patients in critical condition. Isr J Med Sci 31:674–680
Pirret AM (2002) Utilizing TISS to differentiate between intensive care and high-dependency patients and to identify nursing skill requirements. Intensive Crit Care Nurs 18:19–26
Wakefield CH, Corry R, Dodds R, Park L Lee A, Fearon KCH (2000) Activities and outcome in the surgical high-dependency setting. Br J Surg 87 [Suppl 1]:54
Ching CK, Yam LY, Lee CH (1997) 6-month survival of patients admitted to a medical high dependency unit. Chest 112 [Suppl 3]:85S
Kass JE, Castriotta RJ, Malakoff F (1992) Intensive care unit outcome in the very elderly. Crit Care Med 20:1666–1971
Mayer-Oakes SA, Oye RK, Leake B (1991) Predictors of mortality in older patients following medical intensive care: the importance of functional status. J Am Geriatr Soc 39:862–868
Roche VML, Kramer A, Hester E, Welsh CH (1999) Long-term functional outcome after intensive care. J Am Geriatr Soc 47:18–24
Boumendil A, Maury E, Reinhard I, Luquel L, Offenstadt G, Guidet B (2004) Prognosis of patients aged 80 years and over admitted in medical intensive care unit. Intensive Care Med 30:647–654
Nierman DM, Schechter CB, Cannon LM, Meier DE (2001) Outcome prediction model for very elderly critically ill patients. Crit Care Med 29:1853–1859
Acknowledgements
We thank Carolyn Newey for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0172-z
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Torres, O.H., Francia, E., Longobardi, V. et al. Short- and long-term outcomes of older patients in intermediate care units. Intensive Care Med 32, 1052–1059 (2006). https://doi.org/10.1007/s00134-006-0170-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0170-1