Abstract
The primary lymphoma of the skull is very rare. We describe a case of a 48-year-old woman with a palpable, soft, painless swelling of the soft tissues of the right frontal region, in absence of neurological symptoms. The ultrasonography showed the presence of solid, very vascularized, subcutaneous, and intra-thecal tissue and bone erosion of the internal and external cranial theca. A CT scan of the skull, thorax, and abdomen was performed to exclude further manifestations of the disease and an MRI examination of the brain to exclude involvement of the intracranial structures. CT and MRI confirmed the presence of the intra-thecal and extra-thecal mass that infiltrated the external and internal cranial theca, the scalp, and the epidural region without infiltration of the cerebral cortex. The patient underwent mass removal surgery and histological analysis, which allowed the diagnosis of non-Hodgkin B cell lymphoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-Hodgkin lymphomas of the skull are infrequent and generally secondary. A primary bone localization is rare [1, 2], especially in the skull [3]; only 37 cases have been reported in the literature [4, 5].
The word primary refers to a lymphoma which has not spread from other locations; it must not be detectable in the bone marrow biopsy; in the end, it must not be found elsewhere in the body within 6 months from the time of initial diagnosis [6].
Clinical Symptoms
Generally, the onset is asymptomatic, and the patient only shows the appearance of a soft and painless swelling of the scalp. The symptomatology is linked to the intracranial extension of the mass which can infiltrate the epidural and subdural region and rarely the cerebral cortex, causing neurological symptoms.
Methods of Imaging Examination
Ultrasonography is the first imaging examination to be performed. It allows to assess the subcutaneous soft tissues and to detect bony erosions. CT allows us to study the tumor mass, focusing the bone erosion, and can also exclude the spreading of the disease. MRI is performed to study the neoplastic mass and its relationship with intracranial structures. The integration between the aforementioned methods guarantees a complete diagnostic framework of the disease.
Differential Diagnosis
The differential diagnosis includes other skull tumors such as metastatic carcinoma [7], osteomyelitis [8], granuloma [9], plasmacytoma [10], meningioma [11], anaplastic meningioma [12], meningeal sarcoma [13], sarcomatoid carcinoma [14], etc.
Therapy
The therapy is generally surgical and consists of a circumferential craniotomy with a safety margin of at least 1 cm. Subsequently, patients undergo sequential cycles of chemotherapy and radiotherapy [15].
Case Report
Written informed consent was obtained from the patient for publication of this case report and any accompanying images and clips. A copy of the written consent is available for review by the editor of this journal.
History and Clinical Findings
We describe the case of a 48-year-old woman, immunocompetent, with progressive growth (a few months) of a cranial swelling in the soft tissues of the right frontal region without further symptoms. The clinical examination showed a soft painless swelling, overlaid by an unaltered smooth skin. The laboratory tests revealed no abnormalities.
Ultrasound Imaging
The patient underwent ultrasound examination with an Aplio XG Toshiba device with a 7.5 Mhz linear probe. Transverse, oblique, and longitudinal scans of the frontoparietal skull region were performed with the patient in supine position. Scans were performed with B-Mode, color Doppler, power Doppler, and duplex Doppler. The B-Mode and the color Doppler examination showed a hypoechoic, inhomogeneous, highly vascularized, subcutaneous mass with intralesional anechoic areas and bone erosion of the cranial vault (Fig. 1a, b). The power Doppler highlighted an unusual aspect of the intralesional arterial vessels, with a “herringbone” pattern that is large central vessel and minor branches perpendicular with low peak velocity at the duplex Doppler (Fig. 2). The ultrasound examination was performed by an operator with 20-year experience in the field.
Ultrasound scan of the right frontoparietal region. a The color Doppler shows the presence of a very vascularized mass extending from the internal boarding (long arrows) to the subcutaneous region; the ultrasound shows bone erosion of the external plank (short arrows). b The power Doppler shows a “herringbone” morphology of the intralesional arterial vascularization (arrows). There are hypoechoic areas meaning intralesional necrosis (heads of arrow)
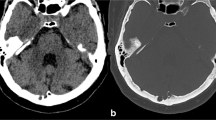
CT Imaging
The patient underwent a CT scan of the skull, neck, thorax, and abdomen with a multi-detector CT (Optima 64 slices, GE Healthcare). The CT of the skull showed an inhomogeneous mass in the right frontoparietal region extending intra- and extra-cranially from the subcutaneous region with bone erosion. The body CT showed absence of disease.
MR Imaging
The MRI examination showed a bulky, intra-, and extra-axial mass, which was located in the frontoparietal region. It was hypointense on both T1- and T2-weighted images, and pronounced and inhomogeneous enhancement was detected after administration of 5 mmol (0.1 mmol/Kg) paramagnetic contrast agent (Dotarem, Guerbet, Roissy, France). This mass compressed the cerebral parenchyma causing smoothing of the frontoparietal cerebral gyri. It also caused bone erosion of the internal and external theca with involvement of subcutaneous tissue (Fig. 3a, b).
a The CT of the skull with coronal reconstruction demonstrates the presence of a right frontoparietal hypodense mass (heads of arrow) and bone erosion of the internal (short arrows) and external plank (long arrows). b The MRI study of the skull (T1 sequence with contrast medium), with coronal reconstruction, shows an inhomogeneous, hypointense mass presenting some areas of intralesional enhancement (long arrow) and extending from the subcutaneous tissue up to the intracranial region with compression of the cerebral cortex (heads of arrow)
Therapy
The surgical exploration has revealed a mass very vascularized and infiltrated the internal and external theca, the scalp, and the epidural and subdural space with minimal compression of the cerebral cortex. The mass was surgically excised, and histological examination was performed (Fig. 4). Following surgery, radio-, and chemotherapy were performed with CHOP regimen (cyclophosphamide, doxorubicin, vincristine, and prednisone) and radiotherapy in the operating field.
After 6 months and 1 year, the patient showed no local recurrence or systemic spread of the disease.
Discussion
The diagnosis of lymphoma can be straightforward when the typical clinical manifestations or laboratory alterations are present; in our case, with an immunocompetent and asymptomatic patient, one of the risks consists of underestimating the disease. Ultrasonography can rapidly provide an accurate evaluation of subcutaneous masses. Moreover, the presence of bone infiltration allows us to exclude more common subcutaneous benign masses such as lipomas, osteomas, fibrous dysplasia, and hemangioma. Meningioma is a benign mass which can simulate a primary lymphoma of the cranial vault [16, 17]. One of the main differences is that meningioma often shows intralesional calcifications and adjacent bone hyperplasia, which were both absent in our case. Moreover, meningioma does not show bone infiltration. The differential diagnosis in our case was limited to lesions that result in infiltration of the bone, such as anaplastic meningiomas, osteomyelitis, sarcomas, metastases, and myeloma. The ultrasound study therefore has been focused on the characteristics of the intralesional vascularization which, in the case of lymphomas, can provide valuable elements for the differential diagnosis [18]. The duplex Doppler did not provide relevant elements for the differential diagnosis since the sampling of the intralesional arterial vessels did not show high systolic peak velocities, present instead in many other malignant neoplasms. The most important data emerged from the arterial vascularization and above all from the unusual morphology of the “herringbone” of the intralesional arterial vessels found in our case, which could represent, if confirmed on a larger series, a pathognomonic pattern of skull lymphomas. Up to now, about 37 cases of primary skull lymphoma have been described in literature. Hence, only a few reports about imaging findings have been published so that no clear criteria for differential diagnosis are available and percutaneous or excisional biopsy is mandatory.
Conclusion
Primary lymphomas of the cranial theca are very rare but must be considered in the differential diagnosis of subcutaneous masses of the cranial vault. Ultrasound examination represents the first-line imaging modality and is useful for diagnosis.
It allows to detect bone erosion. The primary localization in the cranial vault, the lack of symptoms, and the “herringbone sign” as visualized with power Doppler ultrasound are hallmarks of this disease.
References
Kosugi S, Kume M, Sato J, Sakuma I, Moroi J, Izumi K, et al. Diffuse large B-cell lymphoma with mass lesions of skull vault and ileocecum. J Clin Exp Hematop. 2013;53:215–9.
Fadoukhair Z, Lalya I, Amzerin M, et al. Successful management of primary non Hodgkin lymphoma of the cranial vault. Pan Afr Med J. 2011;8:50.
El Asri AC, Akhaddar A, Baallal H, et al. Primary lymphoma of the cranial vault: case report and a systematic review of the literature. Acta Neurochir. 2012;154:257–65.
Salvo V, Brogna B, Sampirisi L, et al. Diffuse-primary-B-cell lymphoma of the cranial vault presenting as stroke. Radiol Case Rep. 2018;13(3):658–62.
Kanaya M, Endo T, Hashimoto D, et al. Diffuse large B-cell lymphoma with a bulky mass in the cranial vault. Int J Hematol. 2017;106(2):147–8.
Dürr HR, Müller PE, Hiller E, Maier M, Baur A, Jansson V, et al. Malignant lymphoma of bone. Arch Orthop Trauma Surg. 2002;122:10–6.
Mitsuya K, Nakasu Y, Horiguchi S, Harada H, Nishimura T, Yuen S, et al. Metastatic skull tumors: MRI features and a new conventional classification. J Neuro-Oncol. 2011;104:239–45.
Pincus DJ, Armstrong MB, Thaller SR. Osteomyelitis of the craniofacial skeleton. Semin Plast Surg. 2009;23(2):73–9.
Shah SR, Keshri A, Behari S, et al. Giant cell granuloma of the anterior skull base: need for early, maximal surgical excision: a short series of 3 cases with review of literature. Indian J Otolaryngol Head Neck Surg. 2015;67(4):347–52.
Gürbüz MS, Akmil MU, Akar E et al. Solitary plasmocytoma of the skull. BMJ Case Rep. 2013. https://doi.org/10.1136/bcr-2013-200379.
Kwon SY, Shin HS, Kim TH, et al. Primary intraosseous osteolytic meningioma of the skull mimicking scalp mass: a case report and review of literature. Brain Tumor Res Treat. 2015;3(2):151–5.
Kessler RA, Garzon-Muvdi T, Yang W, et al. Metastatic atypical and anaplastic meningioma: a case series and review of the literature. World Neurosurg. 2017;101:47–56.
Wu G, Liang Q, Liu Y. Primary osteosarcoma of frontal bone: a case report and review of literature. Medicine (Baltimore). 2017;96(51):e9392.
Sadashiva N, Nandeesh BN, Devi BI. Primary cranial sarcomatoid carcinoma. J Neuro-Oncol. 2017;133(1):207–9.
Fadoukhair Z, Lalya I, Amzerin M, et al. Successful management of primary non Hodgkins lymphoma of the cranial vault. Pan Afr Med J. 2011;8:50.
Johnson MD, Powell SZ, Boyer PJ, Weil RJ, Moots PL. Dural lesions mimicking meningiomas. Hum Pathol. 2002;33:1211–26.
Agrawal A, Makannavar JH, Shetty JP, Shetty RK, Shetty L. Frontal convexity primary lymphoma masquerading meningioma: a case report and review of literature. Indian J Cancer. 2007;44:36–7.
Mandava A, Koppula V, Wortsman X, et al. The clinical value of imaging in primary cutaneous lymphomas: role of high resolution ultrasound and PET-CT. Br J Radiol. 2019;92(1095):20180904.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
Statement of human rights.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Electronic Supplementary Material
Clip The power Doppler shows a “herringbone” morphology of the arterial intralesional vascularization. (MP4 12903 kb)
Rights and permissions
About this article
Cite this article
Farina, R., Iannace, F.A., Conti, A. et al. Role of Ultrasound in a Rare Case of Primary Lymphoma of the Cranial Vault. SN Compr. Clin. Med. 2, 2438–2441 (2020). https://doi.org/10.1007/s42399-020-00577-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00577-6