Abstract
Ofatumumab is a fully humanized monoclonal antibody against CD20. It has been initially used against hematological malignancies but now has been reported widely for autoimmune or rheumatological (e.g., rheumatoid arthritis, multiple sclerosis) and renal conditions. Over the past decade, since the first report on its use in rituximab-resistant nephrotic syndrome, there have been many more centers describing their experience with ofatumumab. Due to it being relatively new, the optimal dosing of ofatumumab for renal conditions has not been established, especially in children, and studies so far have been mainly case reports or case series. Large-scale, multi-center prospective studies are required to establish the appropriate dosing and investigate adverse reactions of ofatumumab. Reported studies on the use of ofatumumab in renal conditions and reported or potential adverse reactions are discussed in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ofatumumab (OFA) is a fully humanized monoclonal antibody against CD20 antigen. CD20 is situated on the surface of pre-B cells maturing to memory B cells; therefore, all B cell subsets, except precursors and plasma cells, express the CD20 antigen [1]. CD20 is involved in B cell maturation and calcium signaling. OFA depletes B cells by directly activating signaling pathways resulting in apoptosis or by means of host immune system components, such as complement system or cells bearing Fc receptor, resulting in cytotoxic response (antibody-dependent cellular cytotoxicity). In primary focal segmental glomerulosclerosis (FSGS), it has been hypothesized that the activity and/or secretion of a circulating permeability factor is B cell related, hence the role of anti-CD20 antibodies. CD20 is a good target because of its high content, limited shedding compared with other pan-B markers and the lack of soluble form which would compete for antibody binding. In addition, OFA exerts cytotoxic effect on peripheral B cells without affecting the regeneration from stem cells because it is not on the immature B cells residing in the bone marrow [2].
How Ofatumumab Is Different from Rituximab and Indications for Ofatumumab After the Use of Rituximab
OFA recognizes an epitope located more proximally to the cell membrane [3], has greater binding avidity, and dissociates slower than rituximab (RTX). In vitro studies have suggested that OFA is a better inducer of antibody-dependent cellular cytotoxicity (ADCC) [4] and complement-dependent cytotoxicity (CDC) [5, 6] than RTX.
RTX is a chimeric mouse/human monoclonal antibody against CD20, whereas OFA is fully humanized. Thus, it is possible that there might be less allergic reaction or hypersensitivity to OFA. It has been demonstrated that it is safe to administer OFA despite infusion-related reactions to RTX [7].
OFA has also been used when anti-chimeric antibodies have developed against RTX, as demonstrated by time to B cell repopulation shortened after each RTX cycle [8].
It has also been proposed that in an adult, OFA may even be more cost effective than RTX because 300 mg of OFA for a 70-kg patient costs €1193 compared with €3206 for 700 mg of RTX [3].
Use of Ofatumumab in Conditions Affecting the Kidneys
-
1.
Nephrotic syndrome
-
2.
Membranous nephropathy
-
3.
Systemic lupus erythematosus
-
4.
IgA vasculitis with nephropathy
-
5.
Thrombotic thrombocytopenic purpura
-
6.
ANCA-associated vasculitis
-
7.
ABO-incompatible kidney transplantation
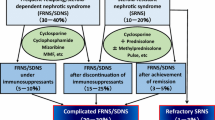
Nephrotic Syndrome
Table 1 shows the details of the case reports and case series of ofatumumab (OFA) therapy for patients with nephrotic syndrome. The use of OFA in renal condition was first described by Basu et al. and results were promising [9]. OFA was given to five patients as a single infusion of 300 mg/1.73 m2, then subsequently 2000 mg/1.73 m2 weekly for 5 weeks. These were patients between the ages 5 and 19 years and had rituximab-resistant idiopathic steroid-resistant nephrotic syndrome (SRNS). The first patient who brought OFA to attention was a 19-year-old girl who had SRNS secondary to FSGS and had received cyclophosphamide (CYC)/tacrolimus(TAC)/RTX. She then had a 2-year history of chronic lymphocytic leukemia (CLL), for which she was receiving OFA. After the first dose, proteinuria improved, and the serum albumin normalized after the third dose. Complete remission (urine protein to creatinine ratio (u-PCR) < 0.2 g/g) was achieved after the sixth dose of OFA. Of the subsequent four patients who were treated with OFA (two with minimal change disease (MCD) and the other two with FSGS), complete remission was achieved in three patients and partial remission in one.
Another case series describes the use of OFA in 4 children [10] who had persistence of proteinuria for ≥ 1 year despite being treated with steroids/cyclosporine (CSA)/TAC/mycophenolate mofetil (MMF)/RTX/angiotensin-converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB). Genetic testing for all was negative. Renal function was affected in two cases with estimated glomerular filtration rate (eGFR) 30–60 ml/min/1.73 m2. The effect of OFA varied amongst the patients. After infusion of the second dose of OFA, two patients (the ones who already had abnormal renal function) did not respond, one had partial response, and one had complete remission.
In a case report of 2 pediatric patients successfully treated with OFA after developing severe allergic reaction to RTX [11], OFA was given as a single infusion at a lower dose (750 mg/1.73 m2). Both patients (one with steroid-dependent nephrotic syndrome (SDNS) and the other with SRNS) achieved complete remission. Another case report [14] described the successful treatment with OFA in a boy with SDNS, who developed serum anti-RTX antibody and RTX infusion reactions. A single dose of OFA (300 mg/m2) was given during a proteinuria-free period and prednisolone was weaned off without relapse at 3 months after OFA infusion. Five months after OFA, he remained in complete remission under only CSA and CD19-positive cells returned.
Using the same OFA regime as Basu et al. [9], five patients with SDNS or SRNS were treated with varying success [12]. Two patients had complete remission, two had partial remission, and one did not receive the full dose of OFA due to infusion reaction. Of note, one of the patients with SDNS (FSGS) had recurrence of disease within 24 h of deceased-donor renal transplantation. He was treated with plasmapheresis, starting on postoperative day (POD) 1 (daily for 3 weeks then 4 days/week). He was also treated with RTX/IV methylprednisolone/TAC/MMF/CSA/CYC. Eight months later, he was given OFA. Proteinuria decreased to non-nephrotic range 12 weeks after the first OFA dose. Similarly, reporting on recurrence of FSGS post-transplantation, Bernard et al. [13] described a patient, with SRNS due to FSGS, with no mutations in podocin or WT1 genes. She underwent living donor transplantation but NS relapsed during the first-year post-transplantation resulting in loss of graft. For her second renal transplantation (deceased donor), disease recurrence occurred 8 days after the transplantation. She was treated with corticosteroids/IAds (immunoadsorption sessions)/enalapril/losartan/CSA (then changed to TAC)/RTX/abatacept. However, proteinuria recurred whenever IAds were stopped. OFA, 300 mg/1.73 m2 then five infusions of 2000 mg/1.73 m2 (2–3 weeks apart), was started two and a half years after the second transplantation. u-PCR improved from nephrotic to subnephrotic range (0.2–1.0 g/g). When B lymphocytes increased with the recurrence of NS, another infusion of OFA (2000 mg/1.73 m2) was given. Even though u-PCR remained at 3–6 g/g, IAds were not reinitiated and creatinine remained stable at 100–110 umol/l with serum albumin > 30 g/l. Further reports on the use of OFA in the recurrence of FSGS post-renal transplant [15,16,17] demonstrated that patients were able to achieve partial or full remission. The details of these case reports can be found in Table 1.
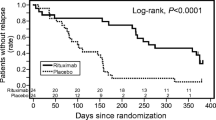
An exciting first double-blind randomized placebo-controlled trial has reported its initial results involving 13 patients [18]. Patients had a median age of 12 (control group) and 16 years (OFA group). These patients with NS had documented multi-drug resistance; i.e., NS was resistant to steroid, CSA/TAC, and MMF. The control group received normal saline infusion and the OFA group received a single infusion of 1500 mg/1.73 m2. The study was stopped as all 13 children remained nephrotic and renal function worsened in 5 children (2 in OFA group, 3 in control group) who required renal replacement therapy during the study period. Despite the trial ending early, it paves the way for future studies—(1) higher OFA doses may be considered (2) instead of normal saline, one may consider RTX or other steroid-sparing immunosuppressants in the other group, to compare efficacy of OFA with other immunosuppressants in SRNS or SDNS. Demonstrating non-inferiority to other immunosuppressants may encourage clinicians to use OFA earlier, rather than after resistance to multiple drugs.
Membranous Nephropathy
Table 2 shows case reports and case series of OFA therapy for patients with membranous nephropathy. In a review article on membranous nephropathy (MN), two patients successfully treated with OFA were reported [3]. Both achieved complete remission after OFA. In another case series, amongst 44 patients with MN treated with ACEI/ARB and RTX [19], 10 patients developed anti-RTX antibodies, of which 3 were treated with OFA and partial remission was achieved.
Podesta et al. also described their experience with OFA in three adult patients with [20] high anti-PLA2R titers. Two patients had persistent nephrotic-range proteinuria while one had partial remission. In a more recent case report [21] on an 18-year-old boy with PLA2R-related MN refractory to steroids/CSA, remissions were achieved with RTX. The seventh dose of RTX was complicated by infusion-related reaction then delayed serum-sickness, which resolved with steroids. On subsequent relapse, OFA 300 mg resulted in partial remission and serum albumin and glomerular filtration rate normalized. For the eighth relapse, OFA (100 mg) failed to induce remission but repeat OFA (300 mg) 5 months later resulted in remission. One year later, the patient relapsed and OFA (300 mg) induced partial remission of proteinuria 1 month after treatment. On the most recent follow-up, the patient is not edematous and has normal GFR.
Systemic Lupus Erythematosus
Table 3 shows case reports and case series of OFA therapy for patients with systemic lupus erythematosus (SLE). A case report [22] described a 22-year-old woman who developed SLE at 11 years old, treated with azathioprine (AZA)/MMF/steroids/RTX. She responded but developed anaphylaxis to RTX requiring IM adrenaline. She relapsed in 2011 requiring steroids/CYC/MTX/CSA/belimumab/IVIG. In 2013, she was given OFA 300 mg then 700 mg 1 week and 3 weeks later. SLEDAI score decreased from 15 to 2, 5 months after the OFA regime. Haarhaus et al. reported on 4 SLE patients receiving OFA after developing RTX infusion reactions, of which 1 achieved urine albumin to creatinine ratio (u-ACR) 3 mg/mmol and the rest had higher u-ACR. Md Yusof et al. reported on 125 patients with SLE treated with RTX over 12 years [8]. Three were given ocrelizumab and two given OFA (two doses of 700 mg). All 5 patients who received ocrelizumab/OFA responded clinically (improvement of BILAG score).
A very interesting case report described three siblings with protein kinase C δ deficiency who presented with SLE before 3 years of age [26]. Two of them developed infusion-related reactions when receiving RTX. They received OFA 300 mg/1.73 m2 then 700 mg/1.73 m2 2 weeks apart without adverse events and showed marked clinical improvement—cutaneous lesions resolved; anti-dsDNA decreased; and hemoglobin, white cells, and platelets improved.
A retrospective case series of sixteen patients (19 to 55 years old) treated with OFA for SLE was reported [25]. Twelve patients were treated for LN and half of these patients achieved renal remission by 6 months. Progressive disease that was unresponsive to increased immunosuppression with CYC was seen in 5 patients.
Another 2 case reports on patients with SLE [24, 27] described improvement in immunological and hematological markers after OFA.
IgA Vasculitis with Nephropathy
A case series describes four patients [28], one of which received OFA. The patient is a 19-year-old obese woman with a history of purpura in childhood. She presented with purpura, abdominal pain, arthralgia with blood pressure of 135/85 mmHg, creatinine 61 umol/l, and urinary dipstick positive for hematuria and proteinuria, and skin biopsy showed necrotizing leukocytoclastic vasculitis. Two days later, creatinine increased to 99 umol/l, serum albumin 34 g/l, urine red blood cells 4–10/hpf, urine granular casts 2–5/hpf, and u-ACR 538 mg/mmol. Another 3 days later, serum albumin decreased to 28 g/l and she developed severe edema. IV methylprednisolone/PO prednisolone was given. Renal biopsy on day 7 from admission demonstrated immunoglobulin A vasculitis with nephritis (IgAVN), no crescents/necrosis, and MEST score M1S0E1T0 (Oxford classification of IgAN). Immunofluorescence staining was positive in the mesangium for IgA, C3, and some IgG. RTX was given on day 9 in view of worsening proteinuria (u-ACR 1633 mg/mmol), and the high-dose steroids were weaned off because of severe obesity. However, she had recurrent bronchospasm during RTX infusion, and thus this was changed to OFA (300 mg first dose, then 500 mg weekly for 3 doses). Albuminuria has since then been < 200 mg/day and creatinine has been normal.
Thrombotic Thrombocytopenic Purpura
Two case reports described the use of OFA in patients with thrombotic thrombocytopenic purpura (TTP) (Table 4). Both patients had RTX transfusion reactions and both patients’ ADAMTS13 responded to OFA.
ANCA-Associated Vasculitis
In a case series, eight patients with ANCA-associated vasculitis (AAV) received OFA two doses, each 700 mg, and 2 weeks apart [31]. The patients were between 21 and 77 years old. Other induction meds include IV CYC/oral prednisone/AZA/MMF. The AAV phenotypes include granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis (EGPA). Five of the six patients with renal involvement had confirmatory renal biopsies demonstrating necrotizing or crescentic glomerulonephritis. Two patients presented with dialysis-dependent renal failure and received plasma exchange in addition to medical therapy with anti-CD20/CYC/steroids. All patients experienced B cell depletion by 1 month and this was sustained until at least 6 months in all patients. All achieved clinical remission by 3 months (BVAS of zero or BVAS < 5 if all scores were due to persistent hematuria or proteinuria in the presence of stable or improving renal function as measured by serum creatinine).
ABO-Incompatible Kidney Transplantation
OFA was used in a desensitization protocol for ABO-incompatible kidney transplantation [32]. A 41-year-old man, with ESRD due to nephroangiosclerosis, on PD for 18 months, had ischemic heart disease treated with dual stent placement. The donor’s blood type was B and the recipient’s was O. Cross-matches, DSA, and match-HLA were all negative and anti-B IgG titer was 1:128. Desensitization protocol for ABO-incompatible recipients included RTX for 4 weeks before the transplant, then plasmapheresis 2 weeks before transplant. Most recipients received plasmapheresis 4 to 5 times until the isoagglutinin anti-ABO antibody ratio was ≤ 1:8. However, this patient developed adverse reaction to RTX and this was thus changed to OFA (300 mg 35 days before the transplant and 2000 mg 28 days before the transplant). He also had six sessions of apheresis and a low-dose intravenous immunoglobulin (0.5 g/kg). Tac/MMF/prednisone was started on the first day of the plasmapheresis. Basiliximab was given on the day of renal transplantation and POD4. Levels of IgG isoagglutinin anti-B were rechecked periodically after transplantation and were at 1:2.
Adverse Reactions of Ofatumumab
Although OFA has been used in patients with RTX-associated anaphylaxis, possible cross-reactions may still occur. This has been described in an adult patient with TTP [33]. She previously had chills and hyperthermia associated with RTX, despite having been given steroids. She also developed generalized rash with hypotension 15 min into the OFA infusion. In a case series describing the use of OFA to treat five patients with SDNS/SRNS [14], three patients developed reactions during OFA infusion but two of these patients eventually tolerated OFA after a desensitization protocol.
Dyspnea, throat irritation, and pharyngolaryngeal pain may also occur with OFA and these appear to be dose-correlated. Thirty-two patients, aged 4–18 years, who are on prednisone and CSA or TAC for NS were given OFA 1500 mg/1.73 m2 (absolute dose 550 to 1900 mg), diluted in 1 l saline and infused at constant rates (12 to 96 ml/h) [34]. Nineteen patients received a pre-treatment with intravenous methylprednisolone (2 mg/kg), oral cetirizine 0.2 mg/kg, and paracetamol 15 mg/kg and sixteen developed dyspnea, throat irritation, and pharyngolaryngeal pain that required repeat steroids and cetirizine. Subsequently, another thirteen patients were pre-treated with salbutamol (0.1 mg/kg up to a maximum of 3.75 mg) administered by a nebulizer at the start of OFA infusion and this resulted in less respiratory reactions.
In another study, spanning over 9 years, reporting adverse reactions to anti-CD20 antibodies [35] in children, 3 to 14 years of age, 130 received RTX and 37 received OFA. These pediatric patients had SDNS or steroid and CNI-dependent NS. The adverse reactions were grouped into infusion, early, and late events, with regard to infusion reactions, only one case of hypotension and one case of dyspnea following RTX infusion in the steroid-dependent group. Patients who were on multiple drugs for their NS developed more symptoms, 5% and 18% following RTX and OFA infusion respectively. These symptoms include skin rash, dyspnea, fever, cough, and itchy throat. Gastrointestinal symptoms, including nausea and abdominal pain, were observed only during OFA infusion. In only two cases (one receiving RTX and one receiving OFA), allergic symptoms required the discontinuation of the infusion. In all other cases, infusion reactions resolved following the reduction in the infusion rate, the administration of antihistamines or steroids, or the addition of salbutamol before OFA infusion. Early adverse reactions (within 3 months of infusion) include infections (2% after RTX, 6% after OFA), bacterial pneumonia (one case after RTX, one case after OFA), and anti-CD20-associated lung injury (three cases after RTX, one case after OFA). Late adverse reactions manifest as infections (two cases after RTX, four cases after OFA). One patient in the OFA group had sacral fistula. With regard to infections, during long-term follow-up (median 28 months) of 14 SLE patients who receive OFA [25], five severe infections (lower respiratory tract infection, dialysis access infections, and gastroenteritis) requiring hospital admission or treatment with intravenous antibiotics occurred in three patients. Three patients from the case series reporting the use of OFA in patients with ANCA-associated vasculitis [31] had infectious complications (urinary tract infections, upper and lower respiratory tract infections). One patient had a transient episode of neutropenia not associated with infection.
Conclusions
The main indications for the use of ofatumumab include failure to achieve B cell depletion with rituximab, failure to achieve clinical response with rituximab, or infusion reaction with rituximab (with or without the presence of anti-RTX antibodies). However, the success of OFA in the treatment of the abovementioned renal conditions has been variable. OFA treatment protocols, as well as concurrent and preceding treatments, differed amongst these studies. Adverse effects known so far include infections and infusion reactions, and the latter may be reduced with pre-medications. Of interest, salbutamol (given via metered dose inhaler or nebulization prior to ofatumumab infusion) may decrease respiratory side effects. The long-term effects remain unknown. Currently, the most frequently reported use of ofatumumab for renal conditions is in patients with nephrotic syndrome. Future studies are needed to (1) compare the efficacy of OFA with other immunosuppressants in different renal conditions, (2) to discover the lowest effective dose, and (3) to observe for long-term adverse effects.
Abbreviations
- ACEI:
-
angiotensin-converting enzyme inhibitor
- ARB:
-
angiotensin receptor blocker
- ATG:
-
anti-thymocyte globulin
- AZA:
-
azathioprine
- CLL:
-
chronic lymphocytic leukemia
- CNI:
-
calcineurin inhibitor
- CSA:
-
cyclosporine
- CYC:
-
cyclophosphamide
- eGFR:
-
estimated glomerular filtration rate
- ESRD:
-
end-stage renal disease
- FSGS:
-
focal segmental glomerulosclerosis
- Hb:
-
hemoglobin
- HCQ:
-
hydroxychloroquine
- IAds:
-
immunoadsorption sessions
- LN:
-
lupus nephritis
- MCD:
-
minimal change disease
- MMF:
-
mycophenolate mofetil
- MN:
-
membranous nephropathy
- NS:
-
nephrotic syndrome
- OFA:
-
ofatumumab
- POD:
-
post-op day
- RTX:
-
rituximab
- SDNS:
-
steroid-dependent nephrotic syndrome
- SLE:
-
systemic lupus erythematosus
- SRNS:
-
steroid-resistant nephrotic syndrome
- TAC:
-
tacrolimus
- u-ACR:
-
urine albumin to creatinine ratio
- u-PCR:
-
urine protein to creatinine ratio
References
Colucci M, Corperri G, Emma F, Vivarelli M. Immunology of idiopathic nephrotic syndrome. Pediatr Nephrol. 2018;33(4):573–84.
Stasiłojć G, Felberg A, Okrój M. Parameters critical for the effector mechanism of anti-CD20 antibodies revisited. Br J Haematol. 2018;180(6):777–9.
Ruggenenti P, Fervenza FC, Remuzzi G. Treatment of membranous nephropathy: time for a paradigm shift. Nat Rev Nephrol. 2017;13(9):563–79.
VanDerMeid KR, Elliott MR, Baran AM, Barr PM, Chu CC, Zent CS. Cellular cytotoxicity of next-generation CD20 monoclonal antibodies. Cancer Immunol Res. 2018;6(10):1150–60.
Teeling JL, French RR, Cragg MS, van den Brakel J, Pluyter M, Huang H, et al. Characterization of new human CD20 monoclonal antibodies with potent cytolytic activity against non-Hodgkin lymphomas. Blood. 2004;104(6):1793–800.
Du J, Yang H, Guo Y, Ding J. Structure of the Fab fragment of therapeutic antibody ofatumumab provides insights into the recognition mechanism with CD20. Mol Immunol. 2009;46(11–12):2419–23.
Chen LY, Shah R, Cwynarski K, et al. Ofatumumab is a feasible alternative anti-CD20 therapy in patients intolerant of rituximab. Br J Haematol. 2018.
Md Yusof MY, Shaw D, El-Sherbiny YM, et al. Predicting and managing primary and secondary non-response to rituximab using B-cell biomarkers in systemic lupus erythematosus. Ann Rheum Dis. 2017;76(11):1829–36.
Basu B. Ofatumumab for rituximab-resistant nephrotic syndrome. N Engl J Med. 2014;370(13):1268–70.
Bonanni A, Rossi R, Murtas C, Ghiggeri GM. Low-dose ofatumumab for rituximab-resistant nephrotic syndrome. BMJ Case Rep. 2015;2015.
Vivarelli M, Colucci M, Bonanni A, Verzani M, Serafinelli J, Emma F, et al. Ofatumumab in two pediatric nephrotic syndrome patients allergic to rituximab. Pediatr Nephrol. 2017;32(1):181–4.
Wang CS, Liverman RS, Garro R, George RP, Glumova A, Karp A, et al. Ofatumumab for the treatment of childhood nephrotic syndrome. Pediatr Nephrol. 2017;32(5):835–41.
Bernard J, Bruel A, Allain-Launay E, Dantal J, Roussey G. Ofatumumab in post-transplantation recurrence of a pediatric steroid-resistant idiopathic nephrotic syndrome. Pediatr Transplant. 2018;22(4):e13175.
Fujinaga S, Sakuraya K. Single infusion of low-dose ofatumumab in a child with complicated nephrotic syndrome with anti-rituximab antibodies. Pediatr Nephrol. 2018;33(3):527–8.
Kienzl-Wagner K, Rosales A, Scheidl S, Giner T, Bösmüller C, Rudnicki M, et al. Successful management of recurrent focal segmental glomerulosclerosis. Am J Transplant. 2018;18(11):2818–22.
Solomon S, Zolotnitskaya A, Del Rio M. Ofatumumab in post-transplantation recurrence of focal segmental glomerulosclerosis in a child. Pediatr Transplant. 2019;23(4):e13413.
Colucci M, Labbadia R, Vivarelli M, Camassei FD, Emma F, Dello Strologo L. Ofatumumab rescue treatment in post-transplant recurrence of focal segmental glomerulosclerosis. Pediatr Nephrol. 2020;35(2):341–5.
Ravani P, Pisani I, Bodria M, Caridi G, Degl’Innocenti ML, Ghiggeri GM. Low-dose ofatumumab for multidrug-resistant nephrotic syndrome in children: a randomized placebo-controlled trial. Pediatr Nephrol. 2020;35:997–1003. https://doi.org/10.1007/s00467-020-04481-y.
Boyer-Suavet S, Andreani M, Lateb M, Savenkoff B, Brglez V, Benzaken S, et al. Neutralizing anti-rituximab antibodies and relapse in membranous nephropathy treated with rituximab. Front Immunol. 2020 Jan 13;10:3069 eCollection 2019.
Podestà MA, Gennarini A, Portalupi V, et al. Accelerating the depletion of circulating anti-phospholipase A2 receptor antibodies in patients with severe membranous nephropathy: preliminary findings with double filtration plasmapheresis and ofatumumab. Nephron. 2019:1–6.
Podestà MA, Ruggiero B, Remuzzi G, Ruggenenti P. Ofatumumab for multirelapsing membranous nephropathy complicated by rituximab-induced serum-sickness. BMJ Case Rep. 2020;13(1).
Thornton CC, Ambrose N, Ioannou Y. Ofatumumab: a novel treatment for severe systemic lupus erythematosus. Rheumatology (Oxford). 2015;54(3):559–60.
Haarhaus ML, Svenungsson E, Gunnarsson I. Ofatumumab treatment in lupus nephritis patients. Clin Kidney J. 2016;9(4):552–5.
Speth F, Hinze C, Häfner R. Combination of ofatumumab and fresh frozen plasma in hypocomplementemic systemic lupus erythematosus: a case report. Lupus. 2018;27(8):1395–6.
Masoud S, McAdoo SP, Bedi R, Cairns TD, Lightstone L. Ofatumumab for B cell depletion in patients with systemic lupus erythematosus who are allergic to rituximab. Rheumatology (Oxford). 2018.
Lei L, Muhammad S, Al-Obaidi M, et al. Successful use of ofatumumab in two cases of early-onset juvenile SLE with thrombocytopenia caused by a mutation in protein kinase C delta. Pediatr Rheumatol Online J. 2018;16(1):61.
Poulet A, Jarrot PA, Mazodier K, Jean R, Kaplanski G. Successful treatment of systemic lupus erythematosus-related refractory autoimmune hemolytic anemia with ofatumumab. Lupus. 2019;28(14):1735–6.
Lundberg S, Westergren E, Smolander J, Bruchfeld A. B cell-depleting therapy with rituximab or ofatumumab in immunoglobulin A nephropathy or vasculitis with nephritis. Clin Kidney J. 2017;10(1):20–6.
Crowley MP, McDonald V, Scully M. Ofatumumab for TTP in a patient with anaphylaxis associated with rituximab. N Engl J Med. 2018;378(1):92–3.
Al-Samkari H, Grace RF, Connors JM. Ofatumumab for acute treatment and prophylaxis of a patient with multiple relapses of acquired thrombotic thrombocytopenic purpura. J Thromb Thrombolysis. 2018;46(1):81–3.
McAdoo SP, Bedi R, Tarzi R, Griffith M. Pusey CD4 Cairns TD. Ofatumumab for B cell depletion therapy in ANCA-associated vasculitis: a single-centre case series. Rheumatology (Oxford). 2016;55(8):1437–42.
Mancianti N, Monaci G, Rollo F, et al. First case report of using ofatumumab in kidney transplantation AB0 incompatible. G Ital Nefrol. 2017;34.
Cohen Aubart F, Haroche J, Amoura Z. More on ofatumumab for TTP. N Engl J Med. 2018;378(14):1364–5.
Bonanni A, Bertelli E, Moscatelli A, Lampugnani E, Bodria M, Ravani P, et al. Ofatumumab-associated acute respiratory manifestations: clinical characteristics and treatment. Br J Clin Pharmacol. 2016;82(4):1146–8.
Bonanni A, Calatroni M, D’Alessandro M, Signa S, Bertelli E, Cioni M, et al. Adverse events linked with the use of chimeric and humanized anti-CD20 antibodies in children with idiopathic nephrotic syndrome. Br J Clin Pharmacol. 2018;84(6):1238–49.
Acknowledgments
I thank Dr. Eugene Kin Mun Wuan for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
Dr. Esther Huimin Leow contributed to the research, drafting, and approval of the final version.
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Leow, E.H. The Use of Ofatumumab in Renal Conditions. SN Compr. Clin. Med. 2, 2300–2309 (2020). https://doi.org/10.1007/s42399-020-00507-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00507-6