Key Summary Points
The aim of study was to identify factors predicting balance in older hip fracture patients undergoing motor rehabilitation.The aim of study was to identify factors predicting balance in older hip fracture patients undergoing motor rehabilitation.
AbstractSection FindingsCognitive function, comorbidity and hip muscles strength are important predictors of balance in hip fracture patients.
AbstractSection MessageKnowledge of specific predictors could be useful for physicians to identify patients needing specific rehabilitation programs for balance.
Abstract
Purpose
Little is known about the factors predicting balance in hip fracture patients. The aim of this retrospective observational study was to assess balance before and after inpatient rehabilitation and, secondarily, to identify factors predicting the balance levels in older hip fracture patients after motor rehabilitation.
Methods
Data were collected in 124 hip fracture patients over a 2-year period. All patients underwent a standard motor rehabilitation program. A modified version of Berg Balance Scale (BBS) score after rehabilitation, daily gain and percentage of improvement in BBS were the outcome measures. Multivariate regression analysis was performed to identify the predictors of balance.
Results
The mean BBS score was 8.33 ± 7.23 at admission and 21.79 ± 12.15 at the end of rehabilitation (p < 0.001). The daily gain in BBS score was 0.39 ± 0.31 and the percent improvement was 32.28 ± 23.04%. Standing with one foot in front and standing on one foot were the BBS items with the lowest score at discharge and the lowest daily gain and percent improvement. The Cognitive-Functional Independence Measure (cognitive-FIM), hip muscles strength, and Katz index at discharge had moderate-to-strong relationships with final score, daily gain and percentage of improvement in BBS. Cognitive-FIM was a predictor of final BBS score (beta 0.49, p < 0.001), daily gain in BBS (beta 0.34, p < 0.001) and percent improvement in BBS (beta 0.44, p < 0.001). Conversely, hip muscles strength was a predictor of final BBS score (beta 0.32, p = 0.001), and Cumulative Illness Rating Scale severity, a predictor of daily gain in BBS (beta -0.29, p = 0.001). The R2 value of the models were, respectively, 0.39, 0.23, and 0.19.
Conclusions
Cognitive function, comorbidities and hip muscles strength are important predictors of balance in hip fracture patients. Knowledge of these specific factors can be useful for physicians to identify patients needing specific rehabilitation programs for balance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most rehabilitation programs after hip fracture mainly focus on postoperative range of motion exercises, standing, gait training with progressive weight bearing, and strengthening exercises of the hip extensor and abductor muscles [1]. These conventional programs have been shown to improve the independence of activities of daily living (ADLs) and gait function after hip fracture [2]. However, after rehabilitation hip fracture patients can show balance deficits for 2–3 years [3,4,5], because the standard rehabilitation programs have little effect on balance [6].
The persistence of balance deficits is a serious problem for hip fracture patients since postural instability and fear of falling affect locomotion and ADLs and can lead to falls with potentially severe consequences including fractures and other injuries [7, 8]. Because of negative effects of balance deficits on mobility and ADLs, it is very important to know the factors influencing balance and to identify hip fracture patients with higher risk of poorer balance recovery. Knowledge of these predictors may help physicians to plan more appropriate rehabilitation programs in patients who have greater difficulty in recovering balance to prevent falls and re-fractures in these patients. Indeed, little is known about the factors influencing the rehabilitation of balance and the factors predicting balance levels in hip fracture patients undergoing rehabilitation. The literature on this topic is scant and the data are conflicting [9,10,11].
The primary aim of this retrospective observational study was to assess balance before and after motor rehabilitation in older hip fracture patients. The secondary aim was to identify what factors can predict the balance performance in these patients.
Materials and methods
This retrospective cohort study was conducted at the Istituti Clinici Scientifici Maugeri. It consists of a secondary analysis on data from an Institutional database evaluating the impact of hip diseases on balance, collected in patients aged ≥ 65 years undergoing hip surgery and admitted to our Rehabilitation Unit as in-hospital patients between January 2016 and December 2017. Exclusion criteria were patients aged < 65 years, or referred from other departments outside our district with concomitant acute events, or patients with post-surgery complications that emerged during rehabilitation, and patients who died or were transferred back to acute care during the course of rehabilitation. Patients who did not give informed consent or were not able to walk prior to the fracture or perform basic activities without assistance, or who were not living at home at the time of the fracture, or who had pathological fractures were also excluded. All patients demonstrated, after administration of cognitive-FIM [12], an adequate language comprehension and gave their written informed consent to participate. The Local Review Board of our Institute approved the study protocol. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Mode of assessment
Clinical evaluation of all patients was performed at admission and at the end of rehabilitation by a qualified team of physiatrists and geriatricians with scales of demonstrated reliability, validity and sensitivity [12,13,14] that have been used in previous studies concerning hip fracture recovery [12, 14,15,16,17,18]. Patient demographic characteristics and comprehensive clinical data including orthopedic surgery (internal fixation, bipolar hemi-arthroplasty, total hip replacement arthroplasty, immobilization), time from fracture to admission for rehabilitation (days), body mass index (BMI), and length of stay in hospital (days) (LOS) were also recorded. The following instruments were used for assessment:
The Berg Balance Scale (BBS) was used to measure balance in our hip fracture patients by assessing the performance of functional tasks [15]. The BBS consists of 14 items that require subjects to maintain positions of varying difficulty and perform specific tasks. Each item is scored on a 5-point ordinal scale ranging from 0 (unable to perform) to 4 (normal performance). In this study, we excluded the item “pick up an object from the floor” to avoid excessive hip flexion which may predispose to hip dislocation in arthroplasty patients; therefore, the aggregate score of BBS ranged from 0 to 52.
The Cumulative Illness Rating Scale (CIRS) was used at admission to evaluate comorbidities [14]. In this study, we considered the average severity of all comorbidities (severity index).
The Katz ADL scale was used to assess patients’ functional status at admission [16]. It is a 6-item scale assessing bathing, dressing, toileting, transferring, continence, and feeding. Katz scores range from 0 (severe functional impairment) to 6 (full function).
The Cognitive-Functional Independence Measure (cognitive-FIM) was used to assess the mental status of patients [12]. The cognitive-FIM is a 5-item ordinal scale assessing comprehension, expression, social interaction, problem solving, and memory, with each item scored from 1 (total dependence) to 7 (total independence). The cognitive-FIM total score ranges from 0 to 35.
Hip pain intensity was measured using an 11-point Visual Numeric Scale (VNS) from 0 (no pain) to 10 (intolerable pain) [17].
The Muscle Strength Grading Scale (Oxford Scale) [18] was used to assess hip muscle strength. Scores ranged from 0 to 5 (where 0 = no movement and 5 = muscle contracts against full resistance). For our study, we considered the sum of the strength of flexor and abductor muscles of the hip and strength of quadriceps.
A manual goniometer was used to measure the range of motion (ROM) of the hip joint. The sum of ROM in flexion (0–120°) and abduction (0–45°) was considered [19].
Rehabilitation program
The rehabilitation program consisted of an average of 330 min/week of standard motor rehabilitation (6 days/week) for the entire duration of in-hospital stay and was supported by 150 min/week of occupational therapy in the final 2 weeks of in-hospital stay.
The rehabilitation program was based on lower limb ROM, strengthening exercises (hip abduction, flexion and extension, knee extension and ankle dorsi-plantar flexion in the supine position), bed to chair mobility (bed to chair, chair to toilet, chair to chair), pre-gait (sit to stand and vice-versa, balance in standing position), gait activities (parallel bars, walker, crutches), and ADL training (climbing stairs, bathroom skills).
Each patient’s needs, specific rehabilitation goals and progress/outcomes were discussed at admission and bi-monthly by the rehabilitation team (composed of physicians, physiotherapists, and an occupational therapist). Rehabilitation commenced the day after admission. Patients were discharged when, in the opinion of the rehabilitation team, no further in-hospital improvement with rehabilitation was expected.
Statistical analysis
All statistical analyses were performed with the software application Statistica Version 6. Statistical analysis was performed using the Shapiro–Wilk test, descriptive statistic tests (mean ± SD, percentage), and Student’s t test to examine differences within the group. Spearman’s rank correlation coefficient was used to assess correlations between variables, and correlations < 0.30 were considered weak, from 0.30 to 0.50 moderate, and > 0.50 strong [20]. Backward stepwise multiple regression analyses were performed to identify predictors of outcome measures. Multiple regression analyses on BBS scores were performed and residual distribution and homoscedasticity were checked. Only admission variables that were significant at univariate analysis underwent multivariate analysis. Age, sex, time from surgery to admission for rehabilitation, CIRS severity index, BMI, cognitive-FIM, pain VNS, hip ROM, and hip muscle strength were independent variables investigated in the univariate analysis.
Final score and effectiveness and efficiency of motor rehabilitation on balance performance, as measured by the BBS, were the outcome measures.
Effectiveness was defined as the proportion of potential improvement achieved during rehabilitation. In this study the Effectiveness of motor training on balance of hip fracture patients was calculated with the following formula: [(admission BBS score − discharge BBS score)/(52 − admission BBS)] × 100 [21]. Efficiency of motor rehabilitation training on balance represents the average increase in BBS per day obtained by therapy [21] and was calculated by dividing the total number of BBS points gained during rehabilitation by the number of in-hospital days of patients.
P values < 0.05 were considered as statistically significant.
Results
The study was carried out on 124 eligible hip fracture patients consecutively admitted to our Rehabilitation Unit during the study period. Table 1 reports demographic and clinical characteristics and the final BBS scores of the study population.
In the whole sample of hip fracture patients, the mean BBS score was 8.33 ± 7.23 at admission and 21.79 ± 12.15 at the end of rehabilitation (p < 0.001). The mean gain in BBS score was 13.46 ± 9.31 and it was significant (p < 0.001). The daily gain in BBS score of hip fracture patients was 0.39 ± 0.31 and percentage of improvement in BBS achieved with rehabilitation was 32.28 ± 23.04%. The final levels, daily gain and percentage of improvement in BBS of male hip fracture patients did not differ from those of female patients (p = 0.246, p = 0.924, and p = 0.389, respectively).
Internal Fixation and Hemi-arthroplasty patients were the most representative groups.
Before rehabilitation Internal fixation patients had a longer time from fracture to admission for rehabilitation (p = 0.015) with respect to Hemi-arthroplasty patients because they required more time to achieve a stable fixation. At the end of rehabilitation there were no differences in final levels, daily gain, and percentage of improvement in BBS score between Internal fixation and Hemi-arthroplasty patients (p = 0.978, p = 0.573, p = 0.691, respectively).
Table 2 reports the BBS item scores for the study population. All the BBS items had a significant improvement at the end of rehabilitation (p < 0.001 for all). Standing with one foot in front (0.59 ± 1.08, 012 ± 0.23, and 13.0 ± 125.3) and standing on one foot (0.83 ± 1.15, 017 ± 0.24, and 18.4 ± 26.2) were the BBS items with the lowest score at discharge and the lowest daily gain and percentage of improvement in BBS (Table 2).
Tables 3 and 4 report the correlations between outcome measures at discharge and clinical and demographic characteristics of the hip fracture patients at admission and at discharge, as assessed by Spearman’s correlation. Table 4 shows that cognitive-FIM (rho 0.57, 0.40 and 0.47, respectively), hip muscles strength (rho 0.62, 0.48 and 0.55, respectively), and Katz index (rho – 0.67, – 0.49 and 0.58, respectively) at discharge had moderate-to-strong relationships with final, daily gain and percentage of improvement in BBS.
Table 5 shows the results of backward regression analysis performed on hip fracture patients. Only variables at admission that were significant at Spearman’s correlation underwent multivariate analysis. The table shows that Cognitive-FIM was a predictor of final BBS score (beta 0.49, p < 0.001), daily gain in BBS (beta 0.34, p < 0.001) and percentage of improvement in BBS (beta 0.44, p < 0.001). Conversely, hip muscles strength was a predictor of final BBS score (beta 0.32, p = 0.001) and CIRS severity of daily gain in BBS (beta – 0.29, p = 0.001). The R2 value of the models were respectively 0.39, 0.23, and 0.19.
Discussion
This study analyzed the factors predicting the balance performance in older hip fracture patients undergoing standard motor rehabilitation.
Differently from other studies in the literature [9,10,11], we analyzed in these patients efficiency and effectiveness in BBS, which respectively represent the daily gain and percentage of improvement in balance achieved with rehabilitation [21]. In our opinion, these two parameters can be considered as indicators of the efficacy and appropriateness of a rehabilitation program.
We found that in hip fracture patients at the end of rehabilitation the mean BBS score was 21.79 ± 12.15, while the BBS gain for each day of stay in the Rehabilitation Department was 0.39 and the rate of improvement in the BBS was 32.28%. Moreover, at the end of rehabilitation there were no differences in the final levels, daily gain, and percentage of improvement in BBS score between Internal fixation and Hemi-arthroplasty patients and between male and female hip fracture patients.
To our knowledge, no previous studies in the literature have analyzed the efficiency and effectiveness of motor rehabilitation on balance performance in hip fracture patients; hence it is not possible to compare our findings with other reports.
We used a back multiple regression analysis to identify the factors predicting the balance performance in hip fracture patients. We found that cognitive-FIM at admission was a predictor of both daily gain and percentage of improvement in BBS, while CIRS was a predictor of daily gain only. The relationships among cognitive-FIM, daily gain and percentage of improvement in BBS were positive, while the relationships between CIRS and daily gain in BBS were negative; this suggests that, after rehabilitation, daily gain and percent improvement in balance may be lower in hip fracture patients with cognitive impairment and/or severe comorbidities.
The cognitive impairment interferes with the processes that involve sensory information and motor response necessary to control balance and postural stability [22, 23], but it can also affect patient's participation in the rehabilitation program thus prolonging its length [24]. Moreover, severe diseases related to neurological and musculoskeletal systems can cause joint and muscle damages slowing down the rehabilitation program and thus reducing balance efficiency [9, 25]. In addition, during the course of rehabilitation, the moderate-to-severe comorbidities may be more frequently complicated by adverse clinical events (as chest infections and heart failure) slowing down the rehabilitation course and inducing the same effect as above [26]. Knowledge that balance recovery may be poorer in hip fracture patients with cognitive impairment and severe comorbidities suggests that in these patients rehabilitation programs should include balance task-specific training.
These programs have been shown in the literature to be superior to conventional motor rehabilitation in improving balance, lower limb strength, ADLs, and the quality of life in older patients after hip fracture [6, 27, 28] and to produce benefits that last for at least 12 months [6].
Moreover, the associations among outcome measures, cognitive impairment and comorbidity suggest: (i) to activate in these patients measures that can prevent the onset and worsening of cognitive impairment [29], and (ii) to promptly treat the adverse clinical events in patients with severe comorbidities [30].
The multivariate analysis also showed that the cognitive-FIM and hip muscles strength of lower limb after surgery were important predictors of final BBS levels. Relationships among final BBS score, cognitive impairment and hip muscle strength were positive, indicating that after rehabilitation the final balance levels may be lower in hip fracture patients with cognitive impairment and/or poor hip muscles strength.
Our findings on cognitive function are in agreement with Ariza-Vega et al. [11], who showed that cognitive impairment is an independent predictor of mobility in hip fracture patients. Conversely, our finding on muscle strength is not confirmed by the literature in hip patients after surgery.
In any case, muscle strength is a factor that influences balance because it enables the motor responses necessary to control balance and postural stability [22, 31].
In this study, we considered the strength of flexor and abductor muscles of the hip and strength of quadriceps. The sum of the strength of all these muscles was an important predictor of final BBS score: this suggests that standard motor rehabilitation programs should be integrated with muscle-strengthening exercises in patients who have poor muscle strength in the lower limb. Indeed, muscle-strengthening programs have been shown to concurrently improve both hip strength and balance [32, 33]. Sylliaas et al. [32] showed that a 3-month high-intensity strength training improved both strength and balance in home-dwelling hip fracture patients [32]. However, balance task-specific training improved both strength and balance as well [6, 27].
The study also analyzed the factors which at the end of rehabilitation were associated with outcome measures. Spearman’s correlation pointed out that cognitive-FIM, hip muscles strength, and Katz index at discharge had moderate-strong relationships with final, daily gain and percent improvement in BBS, while ROM at discharge had a moderate relationship with the outcome measures.
Studies on this issue analyzed only the BBS score at the end of rehabilitation and found that male, sex, increased comorbidity, cognitive impairment, older age and a longer hospitalization were variables associated to a worse balance [9, 11]. Our study confirms the associations between cognitive impairment and worse balance at the end of rehabilitation reported by Ariza-Wega et al. [11] and points out that also poor hip muscles strength and higher ADL disability are associated to worse balance. These associations confirm the need to activate, early after the onset of hip fracture, measures to prevent and counteract cognitive impairment [29], ADL disability, and lower limb muscle strength deficits [29, 31].
Finally, the study assessed the final levels, daily gain and percentage of improvement achieved with rehabilitation in single items of BBS of hip fracture patients and found a significant improvement in all the items of BBS. However, the scores were lower in two items: "on standing with one foot in front" and "standing on one foot". These items assess balance in highly unstable conditions and their correct execution requires higher levels of cognitive function and muscle strength thus explaining their lower daily gain and percentage of improvement in hip fracture patients.
Our study has some limitations. The ROM assessment considered only the hip ROM in flexion and abduction, while muscle assessment considered only the strength of flexor and abductor muscles of the hip and strength of quadriceps, which in other studies were significant determinants of performance on static and dynamic balance tests [34, 35]. Muscle strength assessment was performed with manual and not instrumental tests, which have a higher level of accuracy and reliability [36].
We did not analyze all the possible factors that may have influenced balance [10, 11]. Patients were admitted to a specific rehabilitation program and therefore the results may not apply to other programs with different entry criteria. Finally, the study was not population-based (patients were referred from general hospitals) and therefore it does not represent all hip fracture patients.
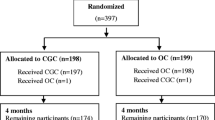
In conclusion, we show that in hip fracture patients, cognitive function, comorbidities and hip strength are important predictors of balance. Knowledge of these findings can be useful for physicians to identify patients needing more specific rehabilitation programs (Fig. 1) and to plan a new tailored treatment approach for balance.
References
Kim IH, Lee SU, Jung SH, Lee SJ, Lee SY (2018) Effectiveness of the computerized balance rehabilitation after hip fracture surgery: A study protocol of a prospective and open-label clinical trial. Medicine (Baltimore) 97:e12199
Chudyk AM, Jutai JW, Petrella RJ, Speechley M (2009) Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil 90:246–262
Archdeacon M, Ford KR, Wyrick J, Paterno MV, Hampton S, Ludwig MB, Hewett TE (2008) A prospective functional outcome and motion analysis evaluation of the hip abductors after femur fracture and antegrade nailing. J Orthop Trauma 22:3–9
Wareńczak A, Lisiński P (2019) Does total hip replacement impact on postural stability? BMC Musculoskelet Disord 20:229
Pop T, Szymczyk D, Majewska J, Bejer A, Baran J, Bielecki A, Rusek W (2018) The Assessment of Static Balance in Patients after Total Hip Replacement in the Period of 2–3 Years after Surgery. Biomed Res Int 2018(4):3707254
Monticone M, Ambrosini E, Brunati R, Capone A, Pagliari G, Secci C, Zatti G, Ferrante S (2018) How balance task-specific training contributes to improving physical function in older subjects undergoing rehabilitation following hip fracture: a randomized controlled trial. Clin Rehabil 32:340–351
Mitani S, Shimizu M, Abo M, Hagino H, Kurozawa Y (2010) Risk factors for second hip fractures among elderly patients. J Orthop Sci 15:192–197
Stenvall M, Olofsson B, Nyberg L, Lundström M, Gustafson Y (2007) Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med 39:232–238
Radosavljevic N, Nikolic D, Lazovic M, Petronic I, Milicevic V, Radosavljevic Z, Potic J, Ilic-Stojanovic O, Jeremic A (2013) Estimation of functional recovery in patients after hip fracture by Berg Balance Scale regarding the sex, age and comorbidity of participants. Geriatr Gerontol Int 13:365–371
Martín-Martín LM, Arroyo-Morales M, Sánchez-Cruz JJ, Valenza-Demet G, Valenza MC, Jiménez-Moleón JJ (2015) Factors Influencing Performance-Oriented Mobility After Hip Fracture. J Aging Health 27:827–842
Ariza-Vega P, Lozano-Lozano M, Olmedo-Requena R, Martín-Martín L, Jiménez-Moleón JJ (2017) Influence of cognitive impairment on mobility recovery of patients with hip fracture. Am J Phys Med Rehabil 96:109–115
Tesio L, Granger CV, Perucca L, Franchignoni FP, Battaglia MA, Russell CF (2002) The FIM instrument in the United States and Italy: a comparative study. Am J Phys Med Rehabil 81:168–176
Ottonello M, Ferriero G, Benevolo E, Sessarego P, Dughi D (2003) Psychometric evaluation of the Italian version of the Berg Balance Scale in rehabilitation inpatients. Europa Medicophysica 39:181–189
Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, Spazzafumo L, Mancinelli L, Espinosa E, Rappelli A, Dessì-Fulgheri P (2008) A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc 56:1926–1931
Berg KO, Wood-Dauphinee SL, Williams JI, Gayton D (1989) Measuring balance in the elderly: preliminary development of an instrument. Physiotherapy Canada 41:304–311
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The Index of ADL: A standardized measure of biological and psychosocial function. JAMA 21(185):914–919
Ritter PL, González VM, Laurent DD, Lorig KR (2006) Measurement of pain using the visual numeric scale. J Rheumatol 33:574–580
Miller DW, Hahn JF (1996) General methods of clinical examination. In: Youmans JR (ed) Neurological Surgery, 4. Saunders, Philapdelphia, W.B, pp 31–32
Cipriano JJ (1997) Photographic Manual of Regional Orthopaedic and Neurological tests, 3rd edn. Williams & Wilkins, Baltimore, MD
Peat J, Barton B, Elliot E (2009) Statistics Workbook for Evidence-Based Health Care. John Wiley & Sons, Hoboken, NJ
Shah S, Vanclay F, Cooper B (1990) Efficiency, effectiveness and duration of stroke rehabilitation. Stroke 21:241–246
Lauretani F, Maggio M, Ticinesi A, Tana C, Prati B, Gionti L, Nouvenne A, Meschi T (2018) Muscle weakness, cognitive impairment and their interaction on altered balance in elderly outpatients: results from the TRIP observational study. Clin Interv Aging 13:1437–1443
Saverino A, Waller D, Rantell K, Parry R, Moriarty A, Playford ED (2016) The role of cognitive factors in predicting balance and fall risk in a neuro-rehabilitation setting. PLoS ONE 11:e0153469
Seitz DP, Adunuri N, Gill SS, Rochon PA (2011) Prevalence of dementia and cognitive impairment among older adults with hip fractures. J Am Med Dir Assoc 12:556–564
Gialanella B, Prometti P, Monguzzi V, Ferlucci C, Baiardi P, Comini L (2018) Determinants of functional outcome in hip fracture: the role of comorbidity. Aging Clin Exp Res 30:643–650
Guerini F, Frisoni GB, Morghen S, Speciale S, Bellelli G, Trabucchi M (2010) Clinical instability as a predictor of negative outcomes among elderly patients admitted to a rehabilitation ward. J Am Med Dir Assoc 11:443–448
Lee SY, Jung SH, Lee SU, Ha YC, Lim JY (2019) Effect of balance training after hip fracture surgery: a systematic review and meta-analysis of randomized controlled studies. J Gerontol A Biol Sci Med Sci 74:1679–1685
Wu JQ, Mao LB, Wu J (2019) Efficacy of balance training for hip fracture patients: a meta-analysis of randomized controlled trials. J Orthop Surg Res 14:83
Siddiqi N, Stockdale R, Britton AM, Holmes J (2007) Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev 18:CD005563
Björkelund KB, Hommel A, Thorngren KG, Gustafson L, Larsson S, Lundberg D (2010) Reducing delirium in elderly patients with hip fracture: a multi-factorial intervention study. Acta Anaesthesiol Scand 54:678–688
Muehlbauer T, Gollhofer A, Granacher U (2015) Associations between measures of balance and lower-extremity muscle strength/power in healthy individuals across the lifespan: a systematic review and meta-analysis. Sports Med 45:1671–1692
Sylliaas H, Brovold T, Wyller TB, Bergland A (2011) Progressive strength training in older patients after hip fracture: a randomised controlled trial. Age Ageing 40:221–227
Lee SY, Yoon BH, Beom J, Ha YC, Lim JY (2017) Effect of lower-limb progressive resistance exercise after hip fracture surgery: a systematic review and meta-analysis of randomized controlled studies. J Am Med Dir Assoc 18:1096.e19–1096.e26
Carter ND, Khan KM, Mallinson A, Janssen PA, Heinonen A, Petit MA, McKay HA (2002) Fall-Free BC Research Group. Knee extension strength is a significant determinant of static and dynamic balance as well as quality of life in older community-dwelling women with osteoporosis. Gerontology. 48:360–368
Wilson BR, Robertson KE, Burnham JM, Yonz MC, Ireland ML, Noehren B (2018) The relationship between hip strength and the Y balance test. J Sport Rehabil 27(5):445–450
Mijnarends DM, Meijers JM, Halfens RJ, ter Borg S, Luiking YC, Verlaan S, Schoberer D, Cruz Jentoft AJ, van Loon LJ, Schols JM (2013) Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc 14:170–178
Acknowledgements
The Authors thank Rosemary Allpress for English revision of the manuscript and Laura Comini for critical revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare. The study was not supported by Pharmaceutical Companies. It was supported by the “Ricerca Corrente” Funding scheme of the Ministry of Health, Italy.
Ethical approval
The Local Review Board of our Institute approved the study protocol. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Informed consent
All patients demonstrated, after administration of cognitive-FIM [12], an adequate language comprehension and gave their written informed consent to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gialanella, B., Santoro, R., Prometti, P. et al. Predictors of balance in older hip fracture patients undergoing standard motor rehabilitation. Eur Geriatr Med 12, 69–77 (2021). https://doi.org/10.1007/s41999-020-00402-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00402-2